Abstract
Background and Objectives
In a previous conducted study functional outcome of young patients with bone sarcoma located around the knee was longitudinally evaluated during the first 2 years postoperatively. Functional outcome improved significantly over the first 2 years. The purpose of this descriptive study was to evaluate the functional outcome of these patients at long‐term follow‐up of 7 years.
Methods
Functional outcome was assessed with the TESS, MSTS, Baecke questionnaire, and three functional performance tests: time up and down stairs (TUDS), various walking activities (VWA), and the 6‐min walking test (6MWT). Linear Mixed Model has been employed for the repeated measurements.
Results
Twenty patients of the original study (n = 44) participated in the current study. Fifteen limb‐salvage and five ablative surgery patients, median follow‐up 7.4 years (6.8‐8.0) (CI 95%), mean age 22.3 years (18.2‐31.6). Between 2 and 7 years after surgery, 8 limb‐salvage patients (53%) encountered surgery related complications. Questionnaires and functional performance tests showed no significant difference in functional outcome between 2 years and 7 years after surgery (P < 0.05).
Conclusions
Between 2 years and follow‐up at average 7 years after surgery no further improvements were noticed at young patients with a bone sarcoma located around the knee.
Keywords: follow‐up, functional outcome, knee, malignant bone sarcoma, young patients
1. INTRODUCTION
The most common bone sarcomas in children younger than 20 years old are osteosarcoma (OSA) (60%) and Ewing sarcoma (ESA) (34%), about 5% of all pediatric cancers.1, 2 The most common localization of these sarcomas is for the lower extremity the region around the knee.2, 3 In general bone sarcoma are treated in a standard strategy, namely neoadjuvant chemotherapy, local excision, followed by adjuvant chemotherapy. Currently the 5‐year overall survival rate is approximately 70% for patients diagnosed with primary non‐metastatic extremity OSA and ESA.4, 5, 6 However, the prognosis for patients with metastatic OSA or ESA at presentation is poor with a 5‐year event‐free survival (EFS) of less than 30%.6, 7, 8
Since there are no differences in survival rates between limb‐salvage (LS) and ablative surgery (AS), long‐term functional outcome studies have become increasingly important to make a patient specific surgical decision.9, 10 However, comparability of these studies is complicated because of the use of different research design, different kind of functional tests and questionnaires, various anatomic sites, a wide range of ages and follow‐up.10, 11, 12, 13, 14, 15, 16, 17, 18
In a previous multicenter study by Bekkering et al, functional ability and physical activity levels were prospectively evaluated at six time points during 2 years after surgery for malignant bone tumors around the knee in a cohort of young patients. Surgery consists of endoprosthesis or allograft reconstruction (LS), rotationplasty, or amputation (AS). After significant improvement of functional outcome over the 1st year, it stabilizes over the 2nd year.19
Aim of this long‐term follow‐up study was to reassess patients of the original cohort in order to evaluate functional outcome at average 7 years after surgery.
2. PATIENTS AND METHODS
This long‐term follow‐up study was an extension of a prospective multi‐center follow‐up study conducted between January 2004 and January 2008.19 Patients who underwent a surgical intervention due to a bone sarcoma around the knee joint were evaluated in one of three appointed university medical hospitals in the Netherlands (34 at Leiden University Medical Centre, 8 at Academic Medical Center University of Amsterdam and 2 at Erasmus MC University Medical Center—Sophia Children's Hospital Rotterdam). All patients (n = 44, 17 female, mean age 15.2 [range 7.8‐24.1]) were treated conforming to EURAMOS‐, EORTC/EOI‐80931, or Euro‐EWING protocol. None of the patients with an Ewing sarcoma received radiation.
All survivors of the original study were invited once for the follow‐up study at average 7 years after surgery. Inclusion criteria for the initial and follow‐up study were: (1) age between 8 and 25 years at the time of surgery, (2) bone sarcoma (osteosarcoma or Ewing sarcoma) located around the knee, (3) limb‐salvage or ablative surgery. Patients were excluded if medical conditions other than bone tumor (related) surgery limited their physical activities.
Measurements at 2 years after surgery were used as comparison values for the current follow‐up study. Two years after surgery, at the end of the initial study, 24 patients (15 LS and 9 AS) continued to be monitored.
The Medical Ethics Committee of all three centers approved the extension of the initial study and all patients gave informed consent.
Patients’ baseline socio‐demographic and clinical characteristics, orthopedic and oncological complications during this long‐term follow‐up were derived from the medical record.
Twenty‐one patients (48%) had died of disease (DOD). At diagnosis of the primary bone tumor of the leg 1 patient had also a bone metastasis and 8 patients had lung metastases. Five years after surgery the survival rate of all patients was 52.3%. Twenty patients, out of the 44 patients at the initial study, were eligible to evaluate functional ability and physical activity (Fig. 1).
Figure 1.
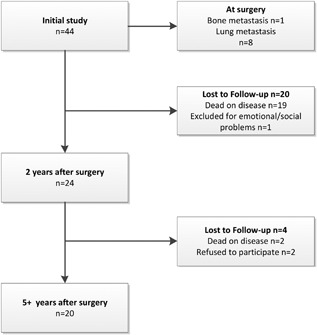
Flow chart showing the number of patients in the original study and the follow‐up study
One surviving patient was excluded in the initial study due to social and emotional problems, two patients refused to participate in the follow‐up study without a reason. Mean age at evaluation in the current study was 22.3 years (range 18.2‐31.6) and median follow‐up was 7.4 years (range 6.8‐8.0) (CI 95%). None of the patients had at the index surgery (severe) obesity (BMI ≥ 30) or neuro‐motor development disabilities.
Physical therapy consists of muscle function training, optimizing joint mobility, and performing daily activities such as walking and climbing stairs independently. Subsequently, after 2 years, rehabilitation was mainly dependent on sport and daily activities.
Table 1 presents patients disease characteristics at 2 years after surgery and at the follow‐up study (Table1). In the current study 75% had an osteosarcoma (15/20) and 25% an Ewing's sarcoma (5/20).
Table 1.
Disease characteristics at 2 years postoperatively (n = 24) and at current follow‐up study (n = 20)
| At 2 years FU | At 7 years FU | |
|---|---|---|
| All patients; n = 24 | All patients; n = 20 | |
| Surgery | ||
| Allograft | 6 | 6 |
| Prosthesis | 12 | 9 |
| Amputation | 5 | 5 |
| Rotationplasty | 1 | 0 |
| Pathology | ||
| Osteosarcoma | 19 | 15 |
| Ewing's sarcoma | 5 | 5 |
| Localization | ||
| Distal femur | 14 | 11 |
| Proximal tibia | 10 | 9 |
At last follow‐up 15 patients with a limb‐salvage procedure (six intercalary allografts and nine endoprostheses) were reviewed and five patients with an ablative procedure (five amputations). All patients with a rotationplasty of the initial study died of disease.
Functional ability was assessed with the Toronto Extremity Salvage Score (TESS), functional performance tests and the Musculoskeletal Tumor Society score (MSTS). The MSTS score was only measured at the long‐term follow‐up.
The functional tests consist of three different activities: (1) the timed up and down stairs (TUDS) test, measuring the time a patient takes to walk up and down 10 stairs (seconds), (2) a combination of three various walking activities (VWA) consisting of 10 m walking at normal speed, slalom, and obstacle walking, and (3) the 6 min walking test (6MWT); patients were informed to walk during 6 min to cover the largest distance (meters). Physical activity was assessed with the Baecke questionnaire, measuring physical activity during sport, leisure time, and work. The total activity score is the summation of these items, ranging from 3 (inactive) to 9 (very active).20 Information about daily living concerning study, work and sportive limitations were derived from a subject interview. Complications were classified according to Henderson (H type I‐V).21, 22
All analyses have been performed with SPSS statistics 20.0 for Windows (SPSS Inc., Chicago, IL). Level of statistical significance was set at P < 0.05. A linear mixed model for the repeated measures with subjects as random effects has been employed to assess the effect for all patients on functionality measured by all the functional ability tests.
3. RESULTS
Between 2 years and the current follow‐up nine patients encountered surgery related complications (45%), 3/6 allograft patients, 5/9 prostheses patients, and 1/5 amputation patients. The allograft complications consisted of a delayed union (H type II, n = 1), a fracture (H type III, n = 1), and an infection (H type IV, n = 1). The fracture resulted in a non‐union of more than 1 year and was completely healed after two operations. The infection was healed after two operations.
The prosthesis complications consisted of aseptic loosening (H type II, n = 2) and structural failure (H type III, n = 3) and resulting to seven re‐operations (two patients twice). One of the five amputation patients had an infection after osseo‐integration surgery. None of the included patients of the follow‐up study had local recurrences (H type V).
Functional ability assessed with TESS, MSTS, and functional performance tests are displayed in Table 2. The TESS scores at 2 years and 7 years after surgery; 88.1‐93.2, TUDS; 11.3‐10.9 s, VWA; 25.4‐25.2 s and the 6MWT; 495‐514 m. The Baecke outcome score reached a plateau phase after 2 years (7.8‐7.8). All changes based on adjusted estimated marginal means between 2 years and 7 years study were not significant (Table 2).
Table 2.
Adjusted estimated marginal means (95% confidence intervals [CI]) at 2 and 7 years after surgery and mean difference (95% confidence intervals [CI]) between 2 and 7 years after surgery
| Estimated means (CI) | Mean differences (CI) | |||
|---|---|---|---|---|
| 2 years | 7 years | 2‐7 years | P‐value | |
| TESS | 88.1 (83.1‐93.1) | 93.2 (88.0‐98.6) | −5.2 (−10.9‐0.5) | 0.08 |
| 6MWT | 494.6 (456.2‐533.0) | 513.5 (470.9‐556.1) | −18.9 (−68‐30.2) | 0.45 |
| TUDS | 11.3 (7.1‐15.5) | 10.9 (6.2‐15.6) | 0.4 (−5.2‐6.0) | 0.89 |
| VWA | 25.4 (22.0‐28.7) | 25.2 (21.6‐28.8) | 0.2 (−3.6‐4.0) | 0.94 |
| BAECKE | 7.8 (7.3‐8.4) | 7.8 (7.3‐8.4) | 0,0 (−0.6‐0.6) | 0.96 |
| MSTS | 83 (37‐100) | |||
TESS, Toronto Extremity Salvage Score; 6 MWT, 6 min walking test; TUDS, timed up and down stairs; VWA, various walking activity; MSTS, Musculo‐Skeletal Tumor Society score.
The MSTS score was 83% (range 37‐100%) at 7 years postoperatively. The lowest score concerns the domain “walking pattern” (mean 3.8, range 0‐5 points) and the highest score at the domain “use of supports” (mean 4.4, range 0‐5 points).
Based on the interviews; 19 patients were active with study, work, or both. Ten patients were involved in a relationship and four of them became parent. Four patients (3 LS and 1 AS) encountered limitations of the operated limb during work and/or study. Eleven patients were active in sports, mainly individual and all low intensive sports, such as fitness, swimming, or biking. Seven of them changed their sport and nine of them suffered limitations compared to their peers.
4. DISCUSSION
The improvements in functional outcome, after surgery due to bone sarcoma around the knee, between 2 and 7 years follow‐up study are insignificant.
The current study with a 7 years follow‐up is an extension of a previous conducted study of young patients (between 8 and 25 years old) and in contrast to other longitudinal studies, concerning functional outcome, without exclusion of patients with local recurrences or metastasis, using the same outcome measures.19
The small number of reviewed patients has limited the results and conclusion of the current study. Unfortunately half of the patients at initial study enrolment deceased on disease.
Physical therapy consists of muscle function training, optimizing joint mobility, and performing daily activities such as walking and climbing stairs independently. Subsequently, after 2 years, rehabilitation was mainly dependent on the individual daily activities and sport activities.
In literature long‐term bone sarcoma studies, especially longitudinal prospective studies concerning the functional outcome after limb surgery for bone sarcoma are scarce. In the prospective study of Marchese et al a comparable cohort of patients was assessed at 6, 12, and 18 months after surgery but with different outcome measures (Functional Mobility Assessment [FMA]), no long‐term follow‐up and not comparable to the current study.23
Most studies on this topic have a cross sectional design. Furthermore, comparability of these long‐term studies is hampered because of different research design (most commonly retrospective design), use of different outcome measures, widely ranged ages of included patients and widely ranged follow‐up moments.10, 11, 12, 14, 15, 16, 17, 18
In general, studies focusing on functional outcome after bone sarcoma surgery of the lower limb, report outcome scores of TESS and MSTS most commonly.12, 14, 15, 18
The prospective study of Ginsberg et al which is most comparable to the present study concerning age and follow‐up time points, reported similar TESS scores at 5 years post‐surgery: a median follow‐up duration of 5.6 years, mean age at surgery of 14.5 years (sd = 4.06) and mean age at study enrollment of 20.1 years (sd = 5.7). TESS scores of amputations above the knee 84.4 (sd = 10.8), amputations below the knee 94.5 (sd = 5.1), LS femur 94.5 (sd = 9.9), and LS tibia 88.1 (sd = 9.3) are comparable to the current study.14 The MSTS scores in the study of Ginsberg of amputation above‐below knee; 65‐77% and LS femur‐LS tibia; 73‐77%; however, are below the scores of the current study (83%).14
According Pakulis et al the MSTS do not meet any of the components for sensibility for the pediatric bone tumor population, despite the popularity of the MSTS scales.24
Unfortunately a number of studies concerning bone sarcoma surgery of the lower extremity reporting scores of TESS and MSTS are not comparable to the current study. The studies by Hopyan et al and Aksnes et al report on older patients, respectively mean 26 years (range 10‐39 years) and 31 years (range 15‐57 years) and a longer median follow‐up duration respectively mean 13,9 (range 5‐26 years) and 13 years (range 6‐22 years).12, 15
Additionally, in the study by Akahane et al lacked allograft patients and in the study by Saraiva et al only endoprosthesis and amputation patients were included.11, 17
In the end comparison of all these studies with the current follow‐up study at 7 years postoperatively is laborious because of the difference in age, difference in timeframe and distribution in respect of surgery of the included patients.
Physical activity as part of the functional outcome was measured by the Baecke questionnaire. Van Dam et al, using the Baecke questionnaire, reported outcome scores of 7.0 (range 4.2‐8.6) for patients after bone sarcoma surgery 2 years post‐surgery.18 Although these comparable scores, the high median age of the included patients (49 years, range 18‐69) and the wide range in follow‐up (range 1‐13 years) limited the comparability to our results.18
Functional outcome scores in longitudinal studies of patients after malignant bone surgery are mostly derived from measurements such as TESS, Baecke, and MSTS. These questionnaires report on the individual perception and satisfaction of physical activity and functional ability after an operation and especially after surviving a life‐threatening event.
Scores derived from functional tests, consisting of daily life activities, are more objective compared to questionnaires. Short‐ and long‐term functional test scores, could be helpful to more accurately predict functionality after limb surgery. However, despite their objectivity, patients with the same functional outcome could have different perception and satisfaction after the same surgery according questionnaires concerning functional outcome.
Only a few studies regarding functional outcome after bone sarcoma surgery, report about objective functional tests.23, 25 In contrast, the current study contains both kind of data collection and additionally we also measured functional outcome at short‐ and long‐term with the same research design and the same measure instruments.
Unfortunately, nearly half of the patients dead of disease and the survival of 23 patients (52,3%) in the current follow‐up study is lower than the described 70% survival rate in the literature.4, 26 This could be due to the fact that at initial study enrolment 9 of the 44 patients had bone or lung metastases at first surgery.
The functional outcome stabilizes after 2 years, which was remarkable given the number of complications in the follow‐up. The high complication and revision rate of the endoprostheses (5/9 patients, 55%), between 2 years after surgery and current study are not in line with the result of studies of Capanna et al, reporting an overall implant survival rate of and 75,9 % at 5 years and 66,2% at 10 years. However, in the study of Capanna et al age of the included patients varied widely (mean 43 years, range 12‐90 years).27 A higher activity level of the younger patients in the current follow‐up study induces probably this higher complication rate.
Remarkable, between 2 and 7 years after surgery there is no deterioration in performance despite the fact that half of the patients had one or more complications. It would be interesting to evaluate whether age, chemotherapy and/or type of reconstruction influence functional outcome scores in a subsequent larger cohort study.
Despite these surgical complications, all patients covered a longer walking distance in the current study. However, outcome scores at the current follow‐up study of 514 meter (range 471‐556) are still lower compared to outcome score of 593 meters ± 57 at healthy subjects between 20 and 50 years old.28
There were no significantly changes concerning the TUDS between the original study and the current study. However, it is not possible to compare these values with normal values, since there is no standard design for the TUDS and normal values are missing as a result.29
Despite the encountered complications and stabilization of the improvement in functional outcome in the first 2 years after surgery, these constraints are not limiting for age‐appropriate social participation at work, sport, and school. All patients in the current study at 7 years postoperatively are working and/or studying and participating in sports.
Based on our results we postulate that 2 years after surgery patients reach a stable phase and cope with their minor disabilities. They are able to integrate them well into normal life despite functional impairments.
Concerning the small cohort size, we recommend a prospective study with a larger cohort to confirm our conclusion regarding functional outcome and surgical treatment.
5. CONCLUSION
We found no significant difference in functional outcome concerning TESS, Baecke, 6 min walking distance test and functional tests (TUDS, VWA) between 2 years and 7 years after surgery in patients treated for bone sarcoma around the knee.
After a significant improvement in functional outcome during the first year after resection of the bone sarcoma, the functional outcome stabilizes and no improvement was found 7 years after surgery.
ETHICAL REVIEW COMMITTEE STATEMENT
The Medical Ethics Committee of all medical centers approved this study, and all patients and their parents (in case of children under the age of 18 years) gave their informed consent.
SYNOPSIS
In a multi‐center extension study, no significant difference was found in functional outcome concerning TESS, Baecke, 6 min walking distance test and functional tests between 2 years and 7 years after surgery in patients treated for bone sarcoma around the knee.
ACKNOWLEDGMENTS
This study was supported by grants from the Johanna Children Fund (project nr. 2003/0111‐161), Children Fund Adrian Foundation (project nr. 2003/0111) and BIO‐Children Rehabilitation Fund (2003/0131‐161).
van Egmond‐van Dam JC, Bekkering WP, Bramer JA, Beishuizen A, Fiocco M, Dijkstra PS. Functional outcome after surgery in patients with bone sarcoma around the knee; results from a long‐term prospective study. J Surg Oncol. 2017; 115: 1028–1032. https://doi.org/10.1002/jso.24618
REFERENCES
- 1. Gurney J, Swensen A, Bulterys M, et al Ries LAG, Smith MA, Gurney JG, Linet M, Tamra T, Young JL, Bunin GR (eds). Malignant bone tumors Cancer Incidence and Survival Among Children and Adolescents: United States SEER Program 1975–1995, Bethesda, MD: National Cancer Institute, SEER Program, NIH; 1999: Pub No 99–4649. [Google Scholar]
- 2. Williams RF, Fernandez‐Pineda I, Gosain A. Pediatric sarcomas. Surg Clin North Am. 2016; 96:1107–1125. [DOI] [PubMed] [Google Scholar]
- 3. Damron TA, Ward WG, Stewart A. Osteosarcoma, chondrosarcoma, and ewing's sarcoma: national cancer data base report. Clin Orthop Relat Res. 2007; 459:40–47. [DOI] [PubMed] [Google Scholar]
- 4. Smeland S, Muller C, Alvegard TA, et al. Scandinavian Sarcoma Group Osteosarcoma Study SSG VIII: prognostic factors for outcome and the role of replacement salvage chemotherapy for poor histological responders. Eur J Cancer. 2003; 39:488–494. [DOI] [PubMed] [Google Scholar]
- 5. Potratz J, Dirksen U, Jurgens H, Craft A. Ewing sarcoma: clinical state‐of‐the‐art. Pediatr Hematol Oncol. 2012; 29:1–11. [DOI] [PubMed] [Google Scholar]
- 6. Friebele JC, Peck J, Pan X, et al. Osteosarcoma: a meta‐Analysis and review of the literature. Am J Orthop (Belle Mead NJ). 2015; 44:547–553. [PubMed] [Google Scholar]
- 7. Mialou V, Philip T, Kalifa C, et al. Metastatic osteosarcoma at diagnosis: prognostic factors and long‐term outcome‐the French pediatric experience. Cancer. 2005; 104:1100–1109. [DOI] [PubMed] [Google Scholar]
- 8. Durfee RA, Mohammed M, Luu HH. Review of osteosarcoma and current management. Rheumatol Ther. 2016; 3:221–243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Bielack SS, Kempf‐Bielack B, Delling G, et al. Prognostic factors in high‐grade osteosarcoma of the extremities or trunk: an analysis of 1,702 patients treated on neoadjuvant cooperative osteosarcoma study group protocols. J Clin Oncol. 2002; 20:776–790. [DOI] [PubMed] [Google Scholar]
- 10. Nagarajan R, Clohisy DR, Neglia JP, et al. Function and quality‐of‐life of survivors of pelvic and lower extremity osteosarcoma and Ewing's sarcoma: the Childhood Cancer Survivor Study. Br J Cancer. 2004; 91:1858–1865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Akahane T, Shimizu T, Isobe K, et al. Evaluation of postoperative general quality of life for patients with osteosarcoma around the knee joint. J Pediatr Orthop B. 2007; 16:269–272. [DOI] [PubMed] [Google Scholar]
- 12. Aksnes LH, Bauer HC, Jebsen NL, et al. Limb‐sparing surgery preserves more function than amputation: a Scandinavian sarcoma group study of 118 patients. J Bone Joint Surg Br. 2008; 90:786–794. [DOI] [PubMed] [Google Scholar]
- 13. Bekkering WP, Vliet Vlieland TP, Koopman HM, et al. Functional ability and physical activity in children and young adults after limb‐salvage or ablative surgery for lower extremity bone tumors. J Surg Oncol. 2011; 103:276–282. [DOI] [PubMed] [Google Scholar]
- 14. Ginsberg JP, Rai SN, Carlson CA, et al. A comparative analysis of functional outcomes in adolescents and young adults with lower‐extremity bone sarcoma. Pediatr Blood Cancer. 2007; 49:964–969. [DOI] [PubMed] [Google Scholar]
- 15. Hopyan S, Tan JW, Graham HK, Torode IP. Function and upright time following limb salvage, amputation, and rotationplasty for pediatric sarcoma of bone. J Pediatr Orthop. 2006; 26:405–408. [DOI] [PubMed] [Google Scholar]
- 16. Malek F, Somerson JS, Mitchel S, Williams RP. Does limb‐salvage surgery offer patients better quality of life and functional capacity than amputation?. Clin Orthop Relat Res. 2012; 470:2000–2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Saraiva D, de CB, Davis AM. Cultural adaptation, translation and validation of a functional outcome questionnaire (TESS) to Portuguese with application to patients with lower extremity osteosarcoma. Pediatr Blood Cancer. 2008; 50:1039–1042. [DOI] [PubMed] [Google Scholar]
- 18. van Dam MS, Kok GJ, Munneke M, et al. Measuring physical activity in patients after surgery for a malignant tumour in the leg. The reliability and validity of a continuous ambulatory activity monitor. J Bone Joint Surg Br. 2001; 83:1015–1019. [DOI] [PubMed] [Google Scholar]
- 19. Bekkering WP, Vliet Vlieland TP, Koopman HM, et al. A prospective study on quality of life and functional outcome in children and adolescents after malignant bone tumor surgery. Pediatr Blood Cancer. 2012; 58:978–985. [DOI] [PubMed] [Google Scholar]
- 20. Baecke JA, Burema J, Frijters JE. A short questionnaire for the measurement of habitual physical activity in epidemiological studies. Am J Clin Nutr. 1982; 36:936–942. [DOI] [PubMed] [Google Scholar]
- 21. Henderson ER, Groundland JS, Pala E, et al. Failure mode classification for tumor endoprostheses: retrospective review of five institutions and a literature review. J Bone Joint Surg Am. 2011; 93:418–429. [DOI] [PubMed] [Google Scholar]
- 22. Henderson ER, O'Connor MI, Ruggieri P, et al. Classification of failure of limb salvage after reconstructive surgery for bone tumours: a modified system Including biological and expandable reconstructions. Bone Joint J. 2014; 96‐B:1436–1440. [DOI] [PubMed] [Google Scholar]
- 23. Marchese VG, Rai SN, Carlson CA, et al. Assessing functional mobility in survivors of lower‐extremity sarcoma: reliability and validity of a new assessment tool. Pediatr Blood Cancer. 2007; 49:183–189. [DOI] [PubMed] [Google Scholar]
- 24. Pakulis PJ, Young NL, Davis AM. Evaluating physical function in an adolescent bone tumor population. Pediatr Blood Cancer. 2005; 45:635–643. [DOI] [PubMed] [Google Scholar]
- 25. Sugiura H, Katagiri H, Yonekawa M, et al. Walking ability and activities of daily living after limb salvage operations for malignant bone and soft‐tissue tumors of the lower limbs. Arch Orthop Trauma Surg. 2001; 121:131–134. [DOI] [PubMed] [Google Scholar]
- 26. Ferrari A, De Salvo GL, Brennan B, et al. Synovial sarcoma in children and adolescents: the european pediatric soft tissue sarcoma study group prospective trial (EpSSG NRSTS 2005). Ann Oncol. 2015; 26:567–572. [DOI] [PubMed] [Google Scholar]
- 27. Capanna R, Scoccianti G, Frenos F, et al. What was the survival of megaprostheses in lower limb reconstructions after tumor resections?. Clin Orthop Relat Res. 2015; 473:820–830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Chetta A, Zanini A, Pisi G, et al. Reference values for the 6‐min walk test in healthy subjects 20‐50 years old. Respir Med. 2006; 100:1573–1578. [DOI] [PubMed] [Google Scholar]
- 29. Nightingale EJ, Pourkazemi F, Hiller CE. Systematic review of timed stair tests. J Rehabil Res Dev. 2014; 51:335–350. [DOI] [PubMed] [Google Scholar]


