Abstract
Introduction and Aims
Disadvantaged men suffer substantial harm from heavy drinking. This feasibility study developed and evaluated the methods for a trial of a brief intervention delivered by text messages to disadvantaged men. It aimed to test the methods for recruitment and retention, to monitor engagement with the intervention and assess the overall acceptability of study methods.
Design and Methods
Disadvantaged men aged 25–44 years who had ≥2 episodes of binge drinking (≥8 units in one session) in the preceding month were recruited. Two recruitment strategies were assessed: recruitment from general practice registers and by a community outreach strategy. Theoretically and empirically based text messages were tailored to the target group.
Results
The study recruited 67 disadvantaged men at high risk of alcohol‐related harm, exceeding the target of 60. Evaluation showed that 95% of text messages were delivered, and the men engaged enthusiastically with the intervention. Retention at follow up was 96%. Outcomes were successfully measured on all men followed up. This provided data for the sample size calculation for the full trial. Post‐study evaluation showed high levels of satisfaction with the study.
Discussion and Conclusions
This study has shown that disadvantaged men can be recruited and follow‐up data obtained in an alcohol intervention study. The study methods were acceptable to the participants. The men recruited were at high risk of alcohol‐related harms. It also clarified ways in which the recruitment strategy, the baseline questionnaire and the intervention could be improved. The full trial is currently underway. [Crombie IK, Irvine L, Falconer DW, Williams B, Ricketts IW, Jones C, Humphris G, Norrie J, Slane P, Rice P. Alcohol and disadvantaged men: A feasibility trial of an intervention delivered by mobile phone. Drug Alcohol Rev 2017;36:468‐476]
Keywords: text messaging, binge drinking, vulnerable population, man, feasibility study
Introduction
Alcohol misuse is a major cause of death and disease across the world 1. Alcohol also causes substantial costs to society through lost productivity, increased health care and other public sector costs as well as crime and social disruption 2, making it a priority for intervention internationally 1.
People who are socially disadvantaged are at a substantially higher risk of suffering alcohol‐related diseases 3. This may be related to binge drinking that is more prevalent among disadvantaged men 4, 5. Although there is extensive evidence showing that brief interventions are effective in reducing alcohol consumption 6, 7, 8, 9, no studies have specifically addressed disadvantaged groups. Brief interventions may need to be tailored for disadvantaged people, because they are less likely to engage in health promotion programs 10. For example, there is good evidence that smoking cessation interventions are less effective in disadvantaged groups 11, 12.
The mobile phone is an attractive method to deliver behaviour change interventions to large numbers of people at very low cost. Text messaging has been used to modify adverse health behaviours and to increase health‐care uptake and improve adherence to treatment. Systematic reviews 13, 14 suggest that brief interventions by mobile phone may be effective, although there is a concern that many of the existing trials have serious methodological weaknesses 15.
Several recent studies have shown that mobile phone‐delivered interventions have the potential to influence drinking behaviour in emergency department attendees 16, 17, 18, college students 19, 20, young people 21, adults 22 and alcohol‐dependent patients 23. Delivering an alcohol brief intervention by mobile phone would be ideal for targeting disadvantaged groups who may be reluctant to participate in research. It avoids barriers such as attending clinic appointments. Further, a mobile phone intervention makes little demand on participants, as behaviour change is facilitated through a series of short text messages.
One challenge for mobile phone studies is the design of the text messages. An emerging literature is beginning to provide a solid theoretical and empirical basis for intervention design 24. A variety of techniques have been used: tailoring of text messages to the target group, making texts interactive, information giving, individually tailored advice, self‐monitoring of the behaviour to be changed and goal setting 13, 25, 26, 27, 28. An important recommendation is to vary the number and timing of text messages to fit the target behaviour. For example, in smoking cessation studies, a higher frequency of texts can be sent around the date that a smoker has set for quitting 29. This is also important for interventions on alcohol use where the text messages can be targeted at heavy drinking occasions 30.
This paper describes the feasibility study that was undertaken prior to a full trial of a mobile phone intervention delivered to disadvantaged men. Feasibility/pilot studies are essential when planning a full trial, providing the opportunity to test and improve all study procedures 31, 32. The aim is to ensure that design weaknesses, technical problems and methodological flaws do not compromise the full trial 33. Challenges were expected because disadvantaged groups are more difficult to recruit to research studies 34, 35, 36, and they are less likely to engage with the intervention. Thus, three specific questions were identified for this study:
Do the component parts of a randomised controlled trial work successfully (recruitment, informed consent, randomisation, intervention delivery, retention, outcome assessment)?
Do study participants successfully engage with key components of the behaviour change intervention?
Is the intervention likely to be an acceptable way to influence the frequency of heavy drinking?
Materials and Methods
Ethical approval for the study was obtained from the East of Scotland Research Ethics Service (ref no. 09/S1401/78). The study is registered as ISRCTN10515845.
Recruitment
The recruitment strategy used evidence‐based techniques for hard to reach and minority groups: culturally sensitive study materials, multiple recruitment strategies and incentives 37, 38, 39, 40, 41, 42, 43. Two recruitment strategies were assessed: recruitment from general practice registers and by a community outreach strategy. The details of the methods are described elsewhere 44. Briefly, strategy 1 identified men in the two most disadvantaged deciles of the patient lists of three general practices in the city of Dundee, Scotland. The Scottish Index of Multiple Deprivation 45 was used to assign postcodes a deprivation score. The general practitioners sent a personally addressed letter inviting men to take part, after which the research assistant recruited men by telephone. Strategy 2, respondent‐driven sampling, is a form of community outreach in which men were recruited from a variety of venues (e.g. sports centres, bars, community centres, the criminal justice system, training centres for the unemployed). Participants recruited in this way were also asked to identify friends (people from their social networks) suitable for inclusion in the study.
Screening, inclusion and exclusion criteria
Individuals identified by the recruitment strategies were screened by a phone call from a researcher to establish current drinking levels. Men were included in the study if they had two or more episodes of binge drinking (≥8 units in a single session) in the preceding month. Exclusion criteria were men currently attending care at an Alcohol Problem Service and men who would not be contactable by mobile phone for any part of the intervention period.
Informed consent
Informed consent was obtained by telephone and text message. Initially, the men were given the participant information sheet. In a subsequent phone call, the participant information sheet was explained and verbal consent was sought. Eligible men who agreed to participate were sent a text message to which they responded if they wanted to participate. This positive action was taken to indicate consent. The date and time of obtaining consent was recorded, and the consenting text was retained as proof of consent.
Randomisation
Participants were randomised to the intervention or control group using a web‐based randomisation system provided by the Glasgow Clinical Trials Unit. Randomisation was stratified by recruitment strategy and restricted with a block size of four. On completion of the baseline questionnaire, participants were sent an initial £10 gift voucher, a £5 gift voucher every week of the text message delivery period and a £10 voucher for completing the outcome assessment.
Intervention design
A series of interactive text messages and images were designed (by DWF) using messaging theory 46, 47, 48, social cognition models 49, systematic reviews of interventions to tackle alcohol problems 7, 8, 9 and systematic reviews of text message intervention studies 26, 27, 29. The intervention adopted a motivational interviewing approach of helping individuals to decide for themselves that they wish to change, rather than advising them to change 50. It also highlighted the discrepancy between what the individual wants from a behaviour (e.g. fun and socialising) and the adverse outcomes that sometimes occur to the drinker and to his family and close friends. The Theory of Planned Behaviour was chosen because it is the most widely used model that identifies the cognitive antecedents of health behaviours 51. Thus, text messages sought to increase motivation to change by addressing attitudes, subjective norms and perceived behavioural control. They incorporated behaviour change techniques identified by Michie and colleagues 52, 53, 54. Text messages were tailored by using language, alcohol‐related experiences and attitudes to cutting down that were familiar to disadvantaged men. The style was informal, using many colloquial expressions that were obtained from focus groups conducted prior to intervention development. The text messages were also tailored to take advantage of the predominant pattern of alcohol consumption, binge drinking at weekends.
In total, 36 short message service (SMS) and multimedia messaging service (MMS) messages were sent. These were intended to increase perceived susceptibility to harms, to alter positive alcohol expectancies (the perceived benefits of heavy drinking) and to increase drinking refusal self‐efficacy. They emphasised the benefits of reduced drinking, encouraged the men to identify opportunities to drink less, to set goals for reduced drinking and to seek social support for these goals.
The text messages presented the credibility of the source (University of Dundee), used the informal style and abbreviations of everyday text messages and made frequent use of humour. Several techniques were employed to increase message effectiveness: tailoring of messages, use of gain‐framed texts, pairing of messages and inclusion of questions to promote interactivity. The messages were constructed to take advantage of the conventional pattern of heavy weekend drinking, tapping into three windows of opportunity: before weekend drinking (to encourage moderate drinking), after a heavy drinking weekend (to gain commitment to change) and midweek sobriety (goal setting). The approach is illustrated by a few example texts, together with the intended behavioural impact, in Appendix 1.
The control group received 34 SMS and MMS messages over 28 days. These were on general health promotion topics (food, physical activity, mental health and sexual health). They were primarily fact‐giving and did not incorporate behaviour change techniques. Examples are given in Appendix 1. These texts ensured that the control group received a similar amount of attention as the intervention group. They were intended to promote retention of participants in the study.
Baseline data
Interviews were conducted by phone, with the interviewer blind to treatment status. Questions on alcohol consumption were taken from the US Behavioural Risk Factor Surveillance System 55. The binge drinking threshold of ≥8 units is twice the recommended UK daily maximum consumption of 4 units per day. This threshold is used in UK government health surveys 56 and corresponds to the Alcohol Use Disorders Identification Test question 57 that elicits the frequency of consuming six standard drinks (i.e. 60 g of alcohol, in the UK, 8 units is 64 g of alcohol). In addition, the frequency of drinking substantially in excess of the conventional binge drinking level (≥16 units in a session) was recorded. Alcohol consumption was measured over the 30 days prior to interview to capture patterns of drinking that could vary from week to week. Questions on refusal skills were taken from the Drinking Refusal Self‐Efficacy Questionnaire 58.
Retention
Techniques to increase retention in follow‐up studies 59, 60, 61 emphasise cultural and person‐sensitive approaches, the importance of creating a project identity and building and maintaining rapport. The specific action taken included the use incentives, sending reminders about follow‐up interviews and multiple attempts at follow up with flexible scheduling of interview times.
Outcome assessment
Follow‐up interviews were conducted by phone, with the interviewer blind to treatment status. The primary outcome measure (for a full trial) was the frequency of binge drinking (consumption of ≥8 units in a single session). It was measured at 3 months after the baseline assessment. Secondary outcomes for the feasibility study were the extent to which the intervention influenced perceptions of harms of alcohol and benefits of moderated drinking. In addition, questions were asked about receipt of the text messages, whether these messages were shared with others and whether involvement in the study had been worthwhile.
Results
The flow of participants through the study is shown in Figure 1. Overall, the number of men recruited, 67, exceeded the target of 60. Each of the recruitment methods met its target of 30 men, with 37 recruited from general practice registers and 30 recruited by community outreach. The participants were spread across the age range 25–44 years; almost four–fifths were in the lowest two deprivation deciles and over half only had school level qualifications (Table 1). Twice as many participants were employed as unemployed and most lived with a partner. The intervention and control groups were similar on all demographic factors.
Figure 1.
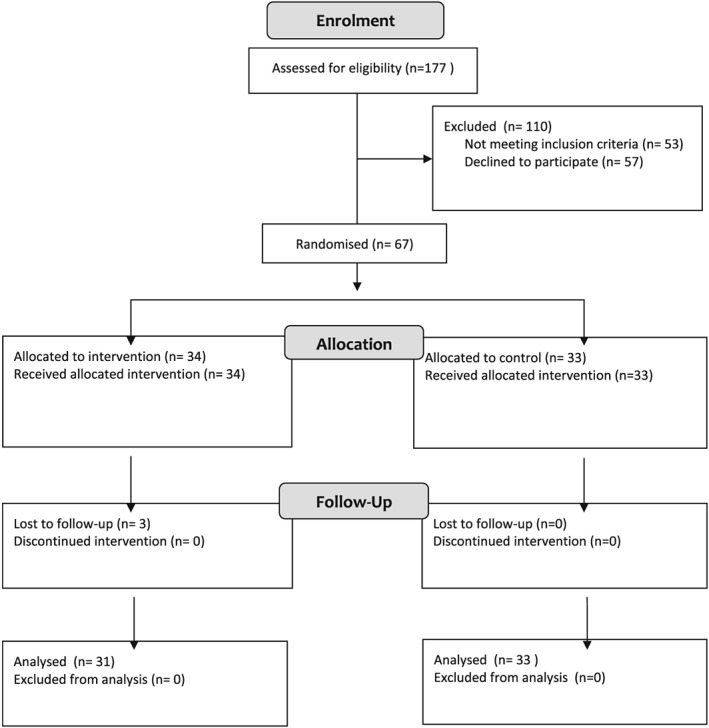
CONSORT 2010 flow diagram.
Table 1.
Demographic characteristics at baseline
| Factor | Control group, N = 33, n (%) | Intervention group, N = 31, n (%) | Total, N = 64, n (%) |
|---|---|---|---|
| Participants' age | |||
| 25–29 years | 13 (39) | 7 (23) | 20 (31) |
| 30–34 years | 6 (18) | 5 (16) | 11 (17) |
| 35–39 years | 9 (27) | 9 (29) | 18 (28) |
| 40–44 years | 5 (15) | 10 (32) | 15 (23) |
| Marital status | |||
| Married/lives with a partner | 21 (64) | 16 (52) | 37 (58) |
| Single | 12 (36) | 15 (48) | 27 (42) |
| Scottish Index of Multiple Deprivation decile | |||
| 1 (most deprived) | 14 (42) | 13 (42) | 27 (42) |
| 2 | 11 (33) | 12 (39) | 23 (36) |
| 3 | 5 (15) | 1 (3) | 6 (9) |
| >4 | 3 (9) | 5 (16) | 8 (13) |
| Employment status | |||
| Employed | 25 (76) | 18 (58) | 43 (67) |
| Unemployed | 8 (24) | 13 (42) | 21 (33) |
| Highest educational attainment | |||
| University degree | 6 (18) | 4 (13) | 10 (16) |
| Vocational qualification/further training | 9 (27) | 11 (36) | 20 (31) |
| High school | 18 (55) | 16 (52) | 34 (53) |
Intervention delivery was monitored electronically. A total of 1108 SMS messages were sent to the 67 participants during the intervention period. Of these, 1053 messages (95%) were delivered to the participants' telephones. Of the remaining 55 messages, 45 were recorded as undelivered (the phone was switched off or it had no signal for 24 h), and no delivery status was recorded for the remaining 10 messages. Fifty‐six men received all of the messages. Of the 11 men who did not receive the complete set of texts, the numbers missed ranged from 1 to 13 with a median of 5 messages missed.
The men were followed up 3 months after the baseline assessment to measure the outcomes. Overall, 96% of those randomised were followed up at 3 months, with high retention in both intervention (91%) and control groups (100%). The main purpose of the follow up was to determine whether the outcomes could be assessed, and complete data was obtained on those followed up. Following guidance for feasibility studies 31, 32, 62, 63, 64, no formal statistical testing for effectiveness was carried out. Inspection of the data (Table 2) shows that men in the intervention group reduced the frequency of their binge drinking (8 or more units in a session) by slightly more than men in the control group. A similar result was seen for heavy binge drinking (16 or more units in a session), but again, the differences were small. The total amount of alcohol consumed by the intervention and control groups fell by similar amounts.
Table 2.
Changes in drinking history between baseline and follow up
| Factor | Baseline | Follow up |
|---|---|---|
| Mean number of binge drinking days in previous 30 days (>8 units in one session) | ||
| Control group | 5.42 | 5.36 |
| Intervention group | 6.32 | 5.77 |
| Mean number of units usually consumed during a binge drinking session | ||
| Control group | 16.29 | 12.85 |
| Intervention group | 14.72 | 13.80 |
| Mean number of heavy binge drinking days in previous 30 days (>16 units in one session) | ||
| Control group | 2.64 | 2.52 |
| Intervention group | 3.68 | 2.77 |
| Mean alcohol consumption in past 30 days (units) | ||
| Control group | 89.54 | 82.92 |
| Intervention group | 103.28 | 96.32 |
| Mean number of moderate drinking days in previous 30 days (<8 units in one session) | ||
| Control group | 2.30 | 2.48 |
| Intervention group | 1.35 | 2.06 |
| Mean number of alcohol free days in previous 30 days | ||
| Control group | 22.27 | 22.15 |
| Intervention group | 22.32 | 22.16 |
The intervention had mixed effects on the intermediate steps to moderated drinking (Table 3). Outcome expectancies were influenced, such that fewer people in the intervention group thought the benefits of drinking outweighed its harms. Slightly more men in the intervention group reported making a plan to reduce their drinking, and more said that they were taking action to achieve this. However, the intervention had less impact on awareness of the definition of binge drinking in the intervention group. Self‐efficacy to refuse a drink was not influenced in the intervention group.
Table 3.
Changes in knowledge and beliefs about alcohol
| Statement which participants assess | Agree at baseline, n (%) | Agree at follow up, n (%) |
|---|---|---|
| The benefits from my drinking outweigh the harms it causes | ||
| Control group | 9 (27) | 10 (30) |
| Intervention group | 13 (42) | 7 (23) |
| I have made a plan to reduce my drinking | ||
| Control group | 5 (15) | 11 (33) |
| Intervention group | 3 (10) | 12 (39) |
| I am taking action to reduce my drinking | ||
| Control group | 5 (15) | 8 (24) |
| Intervention group | 4 (13) | 11 (35) |
| Binge drinking is consuming ≥8 units of alcohol | ||
| Control group | 2 (6) | 12 (36) |
| Intervention group | 1 (3) | 7 (23) |
| I could resist alcohol if someone offered me a drink | ||
| Control group | 25 (76) | 24 (73) |
| Intervention group | 21 (68) | 23 (74) |
| I could resist alcohol when my friends are drinking | ||
| Control group | 16 (48) | 21 (64) |
| Intervention group | 18 (58) | 18 (58) |
The follow‐up interviews also revealed that almost all the men found participation worthwhile and that the timing of the texts was acceptable (Table 4). More telling is that almost all the men mentioned the study to other people and would recommend it to others. Slightly more men in the intervention group thought that they had been helped by the study to reduce their drinking.
Table 4.
Views on acceptability of the study
| Control N = 33 n (%) | Intervention N = 31 n (%) | Total N = 64 n (%) | |
|---|---|---|---|
| Do you think it was worthwhile taking part in the study? | |||
| Yes | 31 (94) | 29 (94) | 60 (94) |
| No | 2 (6) | 2 (6) | 4 (6) |
| Did you receive any text messages at inconvenient times? | |||
| Yes | 1 (3) | 0 | 1 (2) |
| No | 32 (97) | 31 (100) | 63 (98) |
| Do you think the number of text received was appropriate? | |||
| Appropriate | 21 (64) | 21 (68) | 42 (66) |
| Wanted more | 12 (36) | 10 (32) | 22 (34) |
| Wanted fewer | 0 | 0 | 0 |
| How many people did you mention the study to? | |||
| None | 1 (3) | 2 (7) | 3 (5) |
| 1–5 | 18 (55) | 16 (52) | 34 (53) |
| 6–10 | 8 (24) | 10 (32) | 18 (28) |
| >10 | 6 (18) | 3 (10) | 9 (14) |
| Would you recommend the study to anyone? | |||
| Yes | 33 (100) | 27 (87) | 60 (94) |
| No | 0 | 1 (3) | 1 (2) |
| Maybe | 0 | 3 (10) | 3 (5) |
| Do you think taking part in this study helped to reduce the amount you drink? | |||
| Yes | 14 (42) | 18 (58) | 32 (50) |
| No | 11 (33) | 9 (29) | 20 (31) |
| Maybe | 8 (24) | 4 (13) | 12 (19) |
The level of engagement with the intervention can be measured by the extent to which men responded to text messages. Thirty of the 34 study participants (88%) in the intervention group responded to the text messages that asked questions. More than half (18 men) replied to seven or more of the nine questions with two replying to all nine questions and a further nine men answering eight questions. Of the four men who did not respond to any of the questions, two were also lost to follow up. Further details are given elsewhere 65.
Discussion
This feasibility study showed that all the stages of a randomised controlled trial were successfully completed: disadvantaged men were recruited; a non‐contact method of obtaining informed consent worked well; baseline data were obtained by telephone; a brief alcohol intervention was delivered by text messages; the men were followed up; blinded outcome measure were recorded and the men expressed satisfaction with the study. Thus, a full trial could be successfully conducted.
A key finding is the retention rate of 96%. This was achieved with disadvantaged men, who commonly have lower engagement in research 10 and are more likely to be lost to follow up 66, 67. Mobile phone‐delivered interventions that tackle adverse health behaviours typically have retention rates of 70–90% 26, 27, 29, so the present study ranks among the highest. This may have been because of the use of evidence‐based retention techniques, particularly the use of financial incentives 61, 68, 69.
Following the guidance of methodologists 31, 62, 63, 64, this feasibility study did not attempt to estimate the effectiveness of the intervention. Feasibility studies are underpowered to detect intervention effects. They are also vulnerable to imbalance between treatment groups at baseline, which could bias estimates of effectiveness. However, the feasibility study is able to shed some light on whether the intervention has the potential to influence binge drinking. Inspection of the data showed a possible effect on the primary outcome measure, frequency of binge drinking. However, this was small, and no effect was seen on overall alcohol consumption. These results suggest that this feasibility study intervention, comprising 36 messages delivered over 28 days, may need to be strengthened to ensure that the intervention for a full trial has the potential to change drinking behaviour.
The intervention was designed to moderate drinking by modifying alcohol expectancies, alter cognitions about drinking, to increase intentions to reduce consumption and to promote action in drinking less. The follow‐up interviews indicated that it had some success in achieving this. Moreover, the differences between intervention and control groups were modest, in keeping with the limited impact on alcohol consumption. This suggested that these constructs should be given additional attention in a full trial. In addition, there was little change in self‐efficacy to refuse a drink, indicating that additional texts should be created to address this.
One of the major benefits of a feasibility study is that it provides data for the calculation of the sample size for a full trial. This will be based on the difference in the proportion of frequent binge drinking between intervention and control groups at the 12‐month follow‐up assessment. The baseline interviews from the feasibility study showed that 57% of men consumed >8 units on at least three occasions in the previous 30 days. A recent systematic review of conventional brief interventions 8 found an 11% difference in the frequency of binge drinking between intervention and control. Thus, the proposed effect size is that the intervention will reduce the frequency of binge drinking from 57 to 46%, a net reduction of 11%. To detect a reduction in the frequency of binge drinking in this way from 57 to 46% (at the 5% significance level with a power of 80%) would require a sample size of 319 per group or 638 in total. To allow for potential loss to follow up of 20%, the total sample size would be 798.
A possible weakness of the study is that the questions on the harms of alcohol and the benefits of reducing consumption were also asked at baseline. The intention was to measure change in these factors over time. However, it is possible that these questions could motivate the control group to modify their drinking. This possibility is supported by recent systematic reviews 70, 71 that confirm that baseline questions can lead participants to re‐evaluate drinking behaviour. The use of these baseline questions could partly explain why the intervention effect appears so modest, as they may bias intervention effects to the null. In the full trial, the number of these questions would need to be substantially reduced to avoid changes in drinking behaviour in the control group.
Another possible weakness of the intervention is that it did not place emphasis on closing the intention behaviour gap 72, 73. The psychological theory underpinning the intervention, the Theory of Planned Behaviour, addresses intention to change behaviour, but not action planning and maintenance of modified behaviour. A more recent model, the Health Action Process Approach 73, goes beyond intention to seek commitment to action and to the promotion of sustained change. Thus, for the full trial, the intervention will be extended with new texts created to promote goal setting, to gain commitment to action, to overcome barriers to action and to promote maintenance of the reduced frequency of binge drinking. Goal planning may also enhance self‐efficacy 51.
The high level of acceptability of the study, such as whether men found participation worthwhile, could have been influenced by the use of incentives. Whatever the explanation, the fact is that the participants were more than comfortable with the methods used. The high frequency with which men told their friends about the study could have a beneficial consequence for roll out. Sharing messages will spread awareness of the intervention and could increase uptake. Further, conversation about the shared messages could increase the effectiveness of the intervention by promoting reflection on the content of the messages.
Overall, the components of the study worked well. However, this feasibility study has identified aspects of the baseline questionnaire and the intervention that need to be modified. This demonstrates the value of feasibility studies: not to provide estimates of treatment effect but to improve the design for a full trial. That trial, amended following the findings of this feasibility study, is currently underway.
Acknowledgements
This project was funded by the UK National Institute for Health Research Public Health Research programme (09/3001/09). The views and opinions expressed herein are those of the authors and do not necessarily reflect those of the NIHR PHR programme or the Department of Health. The study is registered as ISRCTN 10515845.
Appendix 1.
Examples of intervention and control group text messages
| Message type | Message content |
|---|---|
| Intervention group | |
| Risk awareness | Did you know heavy drinking can give you man boobs or male breasts? Stay moob free |
| Alcohol expectancies | John from Dundee says – I've woke up a few times in the cells [at police station] because of drink. If I was sober it would never have happened |
| Subjective norm | Can U think of someone who'd be happy if you made a change! What would you hear them say? Please txt me your answer! |
| Goal setting | Set yourself a goal & try to avoid alcohol on Weekdays (Monday to Thursday). Give it a go |
| Planning | Can U think of any obstacles or barriers that stop U drinking a bit less each week? Text me your answer! |
| Relapse recovery | If U aim to drink a little less on a night out but end up pissed, don't give up, it happens. Just try your best next time. Take care! |
| Control group | |
| Diet | Eating the wrong kinds of food or over‐eating leads to weight gain. Eating well is crucial if U are to have a healthy weight and a smaller waist. |
| Sexual health | Some STDs have very few symptoms but can lead to serious damage. STDs are a major cause of infertility in men! |
| If you have had unprotected sex in the past & think U may have caught something, put your mind at rest & go for a check‐up with your GP. | |
| Mental health | Physical activity is great for your mental health. Exercising will help U cope with stress, anxiety & depression & will improve your self‐confidence. |
| Close relationships affect how we feel – so nurture them. If a problem arises within a relationship, try to resolve it as quickly as U can. | |
GP, general practitioner; STD, sexually transmitted disease.
Crombie, I. K. , Irvine, L. , Falconer, D. W. , Williams, B. , Ricketts, I. W. , Jones, C. , Humphris, G. , Norrie, J. , Slane, P. , and Rice, P. (2017) Alcohol and disadvantaged men: A feasibility trial of an intervention delivered by mobile phone. Drug and Alcohol Review, 36: 468–476. doi: 10.1111/dar.12455.
Iain K Crombie PhD, Professor of Public Health, Linda Irvine PhD, Trial Manager, Donald W. Falconer PhD, Research Fellow, Brian Williams PhD, Professor of Health Services Research, and Director of Health & Wellbeing Research, Ian W. Ricketts PhD, Professor (Emeritus) of Computing, Claire Jones PhD, Senior Software Engineer, Gerry Humphris PhD, Professor of Psychology, John Norrie MSc, Professor of Medical Statistics and Trial Methodology/Director of the Edinburgh Clinical Trials Unit, Peter Slane MB ChB, General Practitioner, Peter Rice MB ChB, Addiction Psychiatrist.
References
- 1. WHO . Global status report on alcohol and health. Geneva: World Health Organization, 2014. [Google Scholar]
- 2. Rehm J, Mathers C, Popova S, Thavorncharoensap M, Teerawattananon Y, Patra J. Alcohol and Global Health 1 Global burden of disease and injury and economic cost attributable to alcohol use and alcohol‐use disorders. Lancet 2009;373:2223–2233. [DOI] [PubMed] [Google Scholar]
- 3. Mackenbach JP, Stirbu I, Roskam A‐JR, et al Socioeconomic inequalities in health in 22 European countries. N Engl J Med 2008;358:2468–+2481. [DOI] [PubMed] [Google Scholar]
- 4. Fone DL, Farewell DM, White J, Lyons RA, Dunstan FD. Socioeconomic patterning of excess alcohol consumption and binge drinking: a cross‐sectional study of multilevel associations with neighbourhood deprivation. BMJ Open 2013;3(4):e002337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Grittner U, Kuntsche S, Gmel G, et al Alcohol consumption and social inequality at the individual and country levels‐results from an international study. Eur J Public Health 2013;23:332–339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Raistrick D, Heather N, Godfrey C. Review of the effectiveness of treatment for alcohol problems. London: The National Treatment Agency for Substance Misuse, 2006. [Google Scholar]
- 7. Bertholet N, Daeppen JB, Wietlisbach V, Fleming M, Burnand B. Reduction of alcohol consumption by brief alcohol intervention in primary care: systematic review and meta‐analysis. Arch Intern Med 2005;165:986–995. [DOI] [PubMed] [Google Scholar]
- 8. Kaner EF, Dickinson HO, Beyer F, et al The effectiveness of brief alcohol interventions in primary care settings: A systematic review. Drug Alcohol Rev 2009;28:301–323. [DOI] [PubMed] [Google Scholar]
- 9. Moyer A, Finney JW, Swearingen CE, Vergun P. Brief interventions for alcohol problems: a meta‐analytic review of controlled investigations in treatment‐seeking and non‐treatment‐seeking populations. Addiction 2002;97:279–292. [DOI] [PubMed] [Google Scholar]
- 10. Blaxter M. Evidence for the effect on inequalities in health of interventions designed to change behaviour. Evidence Paper for NICE 2007. Available at: https://www.nice.org.uk/guidance/ph6/documents/evidence-for-the-effect-on-inequalities-designed-to-change-behaviour2 [Google Scholar]
- 11. Murray RL, Bauld L, Hackshaw LE, McNeill A. Improving access to smoking cessation services for disadvantaged groups: a systematic review. J Public Health (Oxf) 2009;31:258–277. [DOI] [PubMed] [Google Scholar]
- 12. Bryant J, Bonevski B, Paul C, McElduff P, Attia J. A systematic review and meta‐analysis of the effectiveness of behavioural smoking cessation interventions in selected disadvantaged groups. Addiction 2011;106:1568–1585. [DOI] [PubMed] [Google Scholar]
- 13. Heron KE, Smyth JM. Ecological momentary interventions: incorporating mobile technology into psychosocial and health behaviour treatments. Br J Health Psychol 2010;15:1–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Head KJ, Noar SM, Iannarino NT, Grant HN. Efficacy of text messaging‐based interventions for health promotion: A meta‐analysis. Soc Sci Med 2013;97:41–48. [DOI] [PubMed] [Google Scholar]
- 15. Free C, Phillips G, Galli L, et al The effectiveness of mobile‐health technology‐based health behaviour change or disease management interventions for health care consumers: a systematic review. PLoS Med 2013;10:e1001362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Suffoletto B, Callaway C, Kristan J, Kraemer K, Clark DB. Text‐message‐based drinking assessments and brief interventions for young adults discharged from the emergency department. Alcohol Clin Exp Res 2012;36:552–560. [DOI] [PubMed] [Google Scholar]
- 17. Suffoletto B, Kristan J, Callaway C, et al A text message alcohol intervention for young adult emergency department patients: a randomized clinical trial. Ann Emerg Med 2014;64:664–672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Suffoletto B, Kristan J, Chung T, et al An interactive text message intervention to reduce binge drinking in young adults: a randomized controlled trial with 9‐month outcomes. PLoS One 2015;10:e0142877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Mason M, Benotsch EG, Way T, Kim H, Snipes D. Text messaging to increase readiness to change alcohol use in college students. J Prim Prev 2014;35:47–52. [DOI] [PubMed] [Google Scholar]
- 20. Berman AH. Mobile interventions targeting risky drinking among university students: a review. Curr Addict Rep 2016;3:166–174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Wright CJC, Dietze PM, Crockett B, Lim MSC. Participatory development of MIDY (Mobile Intervention for Drinking in Young people). BMC Public Health 2016;16:184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Haug S, Schaub MP, Venzin V, Meyer C, John U, Gmel G. A pre‐post study on the appropriateness and effectiveness of a web‐ and text messaging‐based intervention to reduce problem drinking in emerging adults. J Med Internet Res 2013;15:126–137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Lucht MJ, Hoffman L, Haug S, et al A surveillance tool using mobile phone short message service to reduce alcohol consumption among alcohol‐dependent patients. Alcohol Clin Exp Res 2014;38:1728–1736. [DOI] [PubMed] [Google Scholar]
- 24. Riley WT, Rivera DE, Atienza AA, Nilsen W, Allison SM, Mermelstein R. Health behavior models in the age of mobile interventions: are our theories up to the task? Transl Behav Med 2011;1:53–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Weitzel JA, Bernhardt JM, Usdan S, Mays D, Glanz K. Using wireless handheld computers and tailored text messaging to reduce negative consequences of drinking alcohol. J Stud Alcohol Drugs 2007;68:534–537. [DOI] [PubMed] [Google Scholar]
- 26. Fjeldsoe BS, Marshall AL, Miller YD. Behavior change interventions delivered by mobile telephone short‐message service. Am J Prev Med 2009;36:165–173. [DOI] [PubMed] [Google Scholar]
- 27. Cole‐Lewis H, Kershaw T. Text messaging as a tool for behavior change in disease prevention and management. Epidemiol Rev 2010;32:56–69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Wei J, Hollin I, Kachnowski S. A review of the use of mobile phone text messaging in clinical and healthy behaviour interventions. J Telemed Telecare 2011;17:41–48. [DOI] [PubMed] [Google Scholar]
- 29. Whittaker R, Borland R, Bullen C, et al Mobile phone‐based interventions for smoking cessation. Cochrane Database Syst Rev 2009;4:CD006611. DOI: 10.1002/14651858.CD006611.pub2. [DOI] [PubMed] [Google Scholar]
- 30. Gajecki M, Berman AH, Sinadinovic K, Rosendahl I, Andersson C. Mobile phone brief intervention applications for risky alcohol use among university students: a randomized controlled study. Addict Sci Clin Pract 2014;9(1):11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Lancaster GA, Dodd S, Williamson PR. Design and analysis of pilot studies: recommendations for good practice. J Eval Clin Pract 2004;10:307–312. [DOI] [PubMed] [Google Scholar]
- 32. Arain M, Campbell MJ, Cooper CL, Lancaster GA. What is a pilot or feasibility study? A review of current practice and editorial policy. BMC Med Res Methodol 2010;10:67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Bowen DJ, Kreuter M, Spring B, et al How we design feasibility studies. Am J Prev Med 2009;36:452–457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Lorant V, Demarest S, Miermans PJ, Van Oyen H. Survey error in measuring socio‐economic risk factors of health status: a comparison of a survey and a census. Int J Epidemiol 2007;36:1292–1299. [DOI] [PubMed] [Google Scholar]
- 35. Goodman A, Gatward R. Who are we missing? Area deprivation and survey participation. Eur J Epidemiol 2008;23:379–387. [DOI] [PubMed] [Google Scholar]
- 36. Turrell G, Patterson C, Oldenburg B, Gould T, Roy MA. The socio‐economic patterning of survey participation and non‐response error in a multilevel study of food purchasing behaviour: area‐ and individual‐level characteristics. Public Health Nutr 2003;6:181–189. [DOI] [PubMed] [Google Scholar]
- 37. Gilliss CL, Lee KA, Gutierrez Y, et al Recruitment and retention of healthy minority women into community‐based longitudinal research. J Womens Health Gend Based Med 2001;10:77–85. [DOI] [PubMed] [Google Scholar]
- 38. Yancey AK, Ortega AN, Kumanyika SK. Effective recruitment and retention of minority research participants. Annu Rev Public Health 2006;27:1–28. [DOI] [PubMed] [Google Scholar]
- 39. Southern DA, Lewis S, Maxwell CJ, et al Sampling 'hard‐to‐reach' populations in health research: yield from a study targeting Americans living in Canada. BMC Med Res Methodol 2008;8:57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Schoenfeld ER, Greene JM, Wu SY, O'Leary E, Forte F, Leske MC. Recruiting participants for community‐based research: the Diabetic Retinopathy Awareness Program. Ann Epidemiol 2000;10:432–440. [DOI] [PubMed] [Google Scholar]
- 41. Harkins C, Shaw R, Gillies M, et al Overcoming barriers to engaging socio‐economically disadvantaged populations in CHD primary prevention: a qualitative study. BMC Public Health 2010;10:391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Mapstone J, Elbourne D, Roberts I. Strategies to improve recruitment to research studies. Cochrane Database Syst Rev 2007:MR000013 DOI: 10.1002/14651858.MR000013.pub3 2007. [DOI] [PubMed] [Google Scholar]
- 43. Caldwell PH, Hamilton S, Tan A, Craig JC. Strategies for increasing recruitment to randomised controlled trials: systematic review. PLoS Med 2010;7:e1000368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Crombie IK, Falconer DW, Irvine L, Norrie J, Williams B, Slane PW. Risky single occasion drinking and disadvantaged men: will recruitment through primary care miss hazardous drinkers? Alcohol Clin Exp Res 2013;37:1577–1581. [DOI] [PubMed] [Google Scholar]
- 45. Office of the Chief Statistician , Scottish Index of Multiple Deprivation 2004. Technical Report 2004, Scottish Executive.
- 46. Rothman AJ, Bartels RD, Wlaschin J, et al The strategic use of gain‐ and loss‐framed messages to promote healthy behavior: how theory can inform practice. J Commun 2006;56:S202–S220. [Google Scholar]
- 47. Fishbein M, Cappella JN. The role of theory in developing effective health communications. J Commun 2006;56:S1–S17. [Google Scholar]
- 48. Viswanath K, Emmons KM. Message effects and social determinants of health: its application to cancer disparities. J Commun 2006;56:238–S264. [Google Scholar]
- 49. Conner M, Norman P. Predicting Health Behaviour, 2nd edn. Maidenhead, Berkshire, England: Open University Press, 2005. [Google Scholar]
- 50. Rollnick S, Miller WR. What is motivational interviewing? Behav Cogn Psychother 1995;23:325–334. [DOI] [PubMed] [Google Scholar]
- 51. Abraham C, Southby L, Quandte S, et al What's in a leaflet? Identifying research‐based persuasive messages in European alcohol‐education leaflets. Psychol Health 2007;22:31–60. [Google Scholar]
- 52. Abraham C, Michie S. A taxonomy of behavior change techniques used in interventions. Health Psychol 2008;27:379–387. [DOI] [PubMed] [Google Scholar]
- 53. Michie S, Johnston M, Francis J, et al From theory to intervention: mapping theoretically derived behavioural determinants to behaviour change techniques. Appl Psychol 2008;57:660–663. [Google Scholar]
- 54. Michie S, Johnston M, Abraham C, et al Making psychological theory useful for implementing evidence based practice: a consensus approach. Qual Saf Health Care 2005;14:26–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Stahre M, Naimi T, Brewer R, Holt J. Measuring average alcohol consumption: the impact of including binge drinks in quantity‐frequency calculations. Addiction 2006;101:1711–1718. [DOI] [PubMed] [Google Scholar]
- 56. Craig R, Shelton N, and editors, Health Survey for Engand 2007. Volume 1. Healthy lifestyles: knowledge, attitudes and behaviour. London: The NHS Information Centre for Health and Social Care, 2008. [Google Scholar]
- 57. Babor TF, Higgins‐Biddle JC, Saunders JB, et al AUDIT The Alcohol Use Disorders Identification Test. Guidelines for Use in Primary Care, 2nd edn. Geneva: World Health Organization. Department of Mental Health and Substance Dependence, 2001. [Google Scholar]
- 58. Oei TP, Young RS. Drinking refusal self‐efficacy questionnaire, in assessing alcohol problems In: Allen JP, Wilson VB, eds. A guide for clinicians and researchers. Bethesda: National Institute on Alcohol Abuse and Alcoholism, 2003. [Google Scholar]
- 59. McKenzie M, Tulsky JP, Long HL, Chesney M, Moss A. Tracking and follow‐up of marginalized populations: a review. J Health Care Poor Underserved 1999;10:409–429. [DOI] [PubMed] [Google Scholar]
- 60. Fowler HS, Aubry T. Conducting evaluation research with hard‐to‐follow populations: adopting a participant‐centred approach to maximize participant retention. Can J Prog Eval 2004;19:89–108. [Google Scholar]
- 61. Robinson KA, Dennison CR, Wayman DM, Pronovost PJ, Needham DM. Systematic review identifies number of strategies important for retaining study participants. J Clin Epidemiol 2007;60:757–765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Thabane L, Ma J, Chu R, et al A tutorial on pilot studies: the what, why and how. BMC Med Res Methodol 2010;10:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Arnold DM, Burns KEA, Adhikari NKJ, et al The design and interpretation of pilot trials in clinical research in critical care. Crit Care Med 2009;37:S69–S74. [DOI] [PubMed] [Google Scholar]
- 64. Leon AC, Davis LL, Kraemer HC. The role and interpretation of pilot studies in clinical research. J Psychiatr Res 2011;45:626–629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Irvine L, Falconer DW, Jones C, Ricketts IW, Williams B, Crombie IK. Can text messages reach the parts other process measures cannot reach: an evaluation of a behavior change intervention delivered by mobile phone? PLoS One 2012;7:e52621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Chang M‐W, Brown R, Nitzke S. Participant recruitment and retention in a pilot program to prevent weight gain in low‐income overweight and obese mothers. BMC Public Health 2009;9:424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. El‐Khorazaty MN, Johnson AA, Kiely M, et al Recruitment and retention of low‐income minority women in a behavioral intervention to reduce smoking, depression, and intimate partner violence during pregnancy. BMC Public Health 2007;7:233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Booker CL, Harding S, Benzeval M. A systematic review of the effect of retention methods in population‐based cohort studies. BMC Public Health 2011;11:249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Brueton VC, Tierney JF, Stenning S, et al Strategies to improve retention in randomised trials: a Cochrane systematic review and meta‐analysis. BMJ Open 2014;4(2):e003821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. McCambridge J, Kypri K. Can simply answering research questions change behaviour? systematic review and meta analyses of brief alcohol intervention trials. Plos One 2011;6(10):e23748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Bernstein JA, Bernstein E, Heeren TC. Mechanisms of change in control group drinking in clinical trials of brief alcohol intervention: implications for bias toward the null. Drug Alcohol Rev 2010;29:498–507. [DOI] [PubMed] [Google Scholar]
- 72. Sniehotta FF. Towards a theory of intentional behaviour change: plans, planning, and self‐regulation. Br J Health Psychol 2009;14:261–273. [DOI] [PubMed] [Google Scholar]
- 73. Schwarzer R. Modeling health behaviour change: how to predict and modify the adoption and maintenance of health behaviours. Appl Psychol: Int Rev 2008;57:1–29. [Google Scholar]


