Abstract
Study Design
Retrospective review of a prospective cohort
Objective
To determine the patient characteristics and surgical procedure factors related to increased rates of 30-day unplanned readmission and major perioperative complications after spinal fusion surgery, as well as the association between unplanned readmission and major complications.
Summary of Background Data
Reducing unplanned readmissions can reduce the cost of healthcare. Payers are implementing penalties for 30-day readmissions following discharge. There is limited data regarding the current rates and risk factors for unplanned readmission and major complications related to spinal fusion surgery.
Methods
Spine fusion patients were identified using the 2012 and 2013 American College of Surgeons National Surgical Quality Improvement Program Participant User File. Rates of readmissions within 30 days following spine fusion surgery were calculated using the person-years method. Cox proportional hazards models were used to assess the independent associations of spine surgical procedure types, diagnoses, patient profiles and major perioperative complications with unplanned related readmissions. Independent risk factors for major complications were assessed by multivariable logistic regression.
Results
Of 18,602 identified patients, there was a 5.2% overall major perioperative complication rate. There was a rate of 4.4% per 30 person-days for unplanned readmissions related to index surgery. Independent risk factors for both readmissions and major perioperative complications included combined anterior and posterior surgery, diagnosis of solitary tumor, older age, and higher American Society of Anesthesiologists class. Patients with deep/organ surgical site infection carried higher risk of having unplanned readmission, followed by pulmonary embolism, acute renal failure and stroke/CVA with neurological deficit.
Conclusions
This study provides benchmark rates of 30-day readmission based on diagnosis and procedure codes from a high-quality database for adult spinal fusion patients and showed increased rates of 30-day unplanned readmission and major perioperative complications for patients with specific risk factors. Targeted preoperative planning on modifiable risk factors with proportional reimbursement may promote higher quality healthcare.
Keywords: readmissions, complications, adult spine fusion, risk factors, NSQIP, outcome, bundled payment
Introduction
Complex reconstruction and fusion techniques are frequently performed for the treatment of spine disorders1,2, resulting in relief of neurologic compression, correction of spinal deformity, increased mechanical stability, and improved function. Despite these potential contributions, spine fusion surgery has been associated with high perioperative complication rates3.
Readmission within 30 days after discharge is one important measure to assess patient outcomes and the quality of care for individual institutions. Recent healthcare reform strategies have focused on bundled payments to incentivize cost saving from the payers’ perspective4. Centers for Medicare and Medicaid Services has implemented financial penalties targeting high readmission frequencies5–7, while other payers and authorities also have instituted adverse consequences for unplanned rehospitalizations6,8. With this ongoing trend, it is imperative for practicing spine surgeons and hospitals to understand risk factors associated with hospital readmissions and to identify those who are at high-risk of major complications and readmissions. Clarifying the risk factors for major surgical complications after spine fusion can help identify high-risk patients and facilitate informed decision-making. Further, targeted interventions and programs fueled by improved reimbursement can be implemented for high-risk patients to reduce readmission and complications.
Patient characteristics9–11, surgical procedure types9,12 and various perioperative complications10,13 have been associated with readmission after index spine surgery in a variety of patient cohorts. However, many of these studies primarily address Medicare populations. The American College of Surgeons National Surgical Quality Improvement Program (ACS-NSQIP, referred to as “NSQIP”) is a multi-center, prospective high quality database that provides detailed patient profiles, preoperative patient characteristics and examination results, procedures performed, other surgical patient information, and 30-day postoperative outcomes. It encompasses a balanced population in terms of age and socioeconomic status compared to the Medicare database, and has been used to identify the risk factors for 30-day readmission after elective primary total joint arthroplasty surgeries14 as well as a variety of lumbar spine surgeries15.
We hypothesized that patient profile and surgical procedure factors are related to increased rates of 30-day unplanned readmission after spinal fusion surgery as well as major perioperative complications and may be modifiable, and that major perioperative complications can predict the likelihood of unplanned readmission. Thus, the specific aims of the current study were: (1) to identify the independent risk factors associated with 30-day unplanned readmission and major perioperative complications, and (2) to determine the association of major perioperative complications and unplanned readmission.
Materials and Methods
Study Design
The present study analyzed a cohort of 18,602 spine fusion patients who were enrolled in the NSQIP database in 2012 or 2013, from 435 hospitals. The spine fusion surgeries included in the present study were based on the Current Procedural Terminology (CPT) codes. (Table 1) NSQIP was founded in 2005 and has been collecting detailed readmission data since 2012. Data is abstracted from the medical record by trained surgical clinical reviewers. Further information regarding the NSQIP database, including the participating institutions and models of the database, can be found on the official website16. Data is collected for 30-days following the index surgery. As information beyond 30-days is not available, our study focuses on short-term postoperative outcomes. Further, the Center for Medicare and Medicaid Services (CMS) quality metric is 30-day readmission from the time of discharge; while NSQIP only collects data for 30-days following the index surgery, not the time of discharge. Collected NSQIP parameters included: (A) surgical procedure type, (B) postoperative diagnosis, (C) patient characteristics, (D) medical profiles and (E) preoperative lab data (Appendix I–V). The surgical procedure types were categorized using the CPT codes (Table 1). The diagnoses were categorized using the International Classification of Diseases, 9th Revision (ICD-9, Appendix VI). Only patients undergoing spinal fusion procedures were included in the present study. Due to potential coding differences among centers, we did not take into account whether a decompression procedure had been performed in addition to the fusion procedure. Similarly, the CPT procedure codes did not provide reliable information regarding which spinal levels or areas of the spine (cervical, thoracic, lumbar) were fused.
Table 1. Current Procedural Terminology (CPT) codes.
that were used to include spine fusion patients as well as categorize the surgical procedure types for the present study.
| CPT | Description |
|---|---|
| 22800 | Arthrodesis, posterior, for spinal deformity, with or without cast; up to 6 vertebral segments |
| 22842 | Posterior segmental instrumentation (eg, pedicle fixation, dual rods with multiple hooks and sublaminar wires); 3 to 6 vertebral segments (List separately in addition to code for primary procedure) |
| 22802 | Arthrodesis, posterior, for spinal deformity, with or without cast; 7 to 12 vertebral segments |
| 22843 | Posterior segmental instrumentation (eg, pedicle fixation, dual rods with multiple hooks and sublaminar wires); 7 to 12 vertebral segments (List separately in addition to code for primary procedure) |
| 22804 | Arthrodesis, posterior, for spinal deformity, with or without cast; 13 or more vertebral segments |
| 22844 | Posterior segmental instrumentation (eg, pedicle fixation, dual rods with multiple hooks and sublaminar wires); 13 or more vertebral segments (List separately in addition to code for primary procedure) |
| 22808 | Arthrodesis, anterior, for spinal deformity, with or without cast; 2 to 3 vertebral segments |
| 22845 | Anterior instrumentation; 2 to 3 vertebral segments (List separately in addition to code for primary procedure) |
| 22810 | Arthrodesis, anterior, for spinal deformity, with or without cast; 4 to 7 vertebral segments |
| 22846 | Anterior instrumentation; 4 to 7 vertebral segments (List separately in addition to code for primary procedure) |
| 22812 | Arthrodesis, anterior, for spinal deformity, with or without cast; 8 or more vertebral segments |
| 22847 | Anterior instrumentation; 8 or more vertebral segments (List separately in addition to code for primary procedure) |
Two main outcome measures were determined within 30 days of index spine surgery: (i) unplanned readmission that was related to the index surgery and (ii) any record of perioperative major complications, per NSQIP record. Each readmission was determined either related or not related to the index surgery based on NSQIP record. NSQIP trained surgical clinical reviewers abstract the medical records to capture minor and major complications as defined by NSQIP and as previously described17,18. Major complications are pulmonary embolism, ventilation support > 48 hours, re-intubation, renal failure, cardiac arrest, myocardial infarction, stroke or cerebral vascular accident (CVA), deep incisional or organ space surgical site infection (SSI), and return to the operating room (OR). Return to OR (operation room) and ventilation support > 48 hours were not included as independent variables in the multivariable analysis with the outcome of unplanned readmission related to the index surgery since these were found to be highly collinear with other independent variables. Minor complications include superficial surgical site infection, pneumonia, urinary tract infection, deep venous thrombosis/thrombophlebitis, blood transfusions, and progressive renal insufficiency.
NSQIP collects thirty-day readmission data starting with the day of the index surgery rather than the day of discharge. CMS defines readmission as readmission to the hospital within 30 days of discharge. 19 Many spine fusion patients may spend up to a week in the hospital after surgery, when they are not a risk for readmission. Similarly, deceased patients are not eligible for readmission. Because length of stay during the index hospitalization varies, patients do not have the same number of days at risk of readmission up to 30 days post index surgery; therefore, we used the person-years method to calculate the unplanned readmission rate per 30 person-days to account for varying days at risk of readmission. Using this method, patients contributed to the time factor in the denominator only after they were out of hospital and were still alive up to 30 days post index surgery, excluding the time spent in the hospital as part of a readmission. Because NSQIP does not capture length of readmissions, we assumed that each patient was in the hospital for an average of 5 days per readmission. We conducted a sensitivity analysis to test this assumption and found that varying this assumption from 2 to 7 days did not significantly affect our results.
All statistical analysis was performed using SAS (SAS Institute Inc. Cary, NC) Version 9.3. Significance was set at α=0.05 for all statistical analysis.
Univariate Analysis
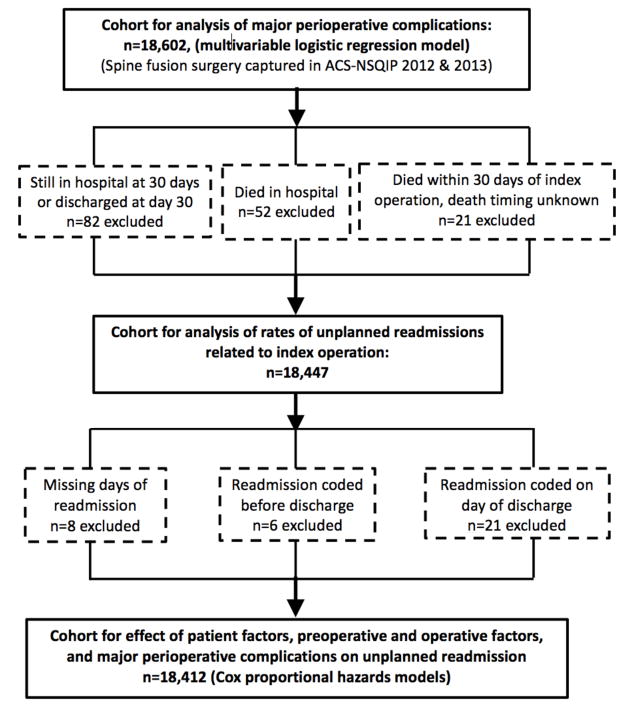
The association between (A) surgical procedure type, (B) postoperative diagnosis, (C) patient characteristics, (D) medical profiles and (E) preoperative lab data on readmission and major perioperative complications was first assessed with univariate analysis by Chi-square tests, or Fisher’s exact tests when low expected counts were observed. The following patients were excluded from the univariate analysis assessing unplanned related readmission: those who (i) died in-hospital (n=52), (ii) were still in hospital 30 days following the index operation (n=82), (iii) died within 30-days following the index operation with the timing of death unknown (n=21). There were a total of 155 patients excluded from the original 18,602 patient cohort based on these criteria (Fig. 1).
Figure 1.
Flowchart for patient inclusion/exclusion for the two major outcome analyses: (a) major perioperative complications (b) unplanned readmission related to index surgery.
Multivariable Analysis: Independent Risk Factors
Independent risk factors for unplanned readmission were identified using Cox proportional hazards models to account for the varying lengths of time that patients were eligible for readmission in the period between discharge from their index hospitalization and thirty days following their index surgery; risk factors for perioperative major complications were identified using multivariable logistic regression. Models for both outcomes included variables that were statistically significant in univariate analysis. Two covariates (“Current smoker within one year” and “Gender”) that did not show significance in univariate analysis were still included in the multivariable models because they were considered clinically relevant. 20–22 On univariate analysis, length of stay was associated with increased complications and readmissions, but length of stay also was significantly associated with procedure type and diagnosis group, and thus not included in the multivariable analysis as an independent variable.
The following patients were excluded from the Cox proportional hazards models assessing independent risk factors of unplanned readmission: those who (i) were excluded from the univariate analysis of readmissions rates as described above (n=155), (ii) were readmitted but were missing the timing of readmission (n=8), (iii) had a readmission coded before discharge (n=6), (iv) had a readmission coded on the day of discharge (n=21). There were a total of 190 patients excluded from the original 18,602 patient cohort based on these criteria (Fig. 1).
Association of Postoperative Major Complications with Unplanned Readmission
In addition to including patient characteristics and preoperative factors in our Cox proportional hazards models, we included postoperative major complications in order to assess the effect of complications on unplanned readmission. Complications were included as time-dependent covariates in the first Cox proportional hazards model to account for the timing of the postoperative complication compared to the timing of the unplanned readmission. In order to identify complications that may be risk factors for readmission when they occurred during the index hospitalization, we created a second multivariable Cox proportional hazards model that included the in-hospital postoperative complications as binary covariates. This second model followed the same exclusion criteria as the first model described above (Fig. 1).
Source of Funding
No funding was used for the present study.
Results
Overall Readmission Rates, Discharge Destination, and Complication Rates
The unplanned readmission rate recorded as related to the index surgery was 4.4% per 30 person-days. The most common causes of unplanned related readmission included deep/organ space surgical site infection (14.1%), superficial surgical site infection/wound disruption (10.0%), hematoma/seroma (8.5%), DVT/PE requiring treatment (7.7%), pneumonia (5.4%), and postoperative pain (4.0%). The overall rate of unplanned readmission including both related and unrelated readmissions was 6.1% per 30 person-days. Thus, 27.9% of readmissions were found to be unrelated to the index surgery, which was calculated by (6.1% – 4.4%) / (6.1%).
Median length of stay (LOS) for index hospitalization was 3 days (interquartile range, 1 to 4). The median length of stay on the index admission was significantly shorter for patients who did not have a later related readmission within 30 days of the index spine fusion surgery, with a median of 2 days (1–4, interquartile range) for those who were not readmitted compared to 4 days (2–6, interquartile range) for those who were readmitted (p<0.001). Overall, 81.8% of patients discharged to home, 17.4% to skilled care or rehabilitation, and 0.8% other. The overall percentage of major perioperative complications was 5.2%, including a 3.2% unplanned return to surgery. The percentage of minor complications was 17%.
Univariate Analysis
Unplanned readmission was more frequent in anterior-posterior combined procedures and posterior fusion greater than 6 levels (Appendix I-A), postoperative diagnoses of solitary tumor and infection (Appendix II-A), older age (Appendix III-A), and history of certain medical comorbidities (Appendix IV-A). Perioperative lab data that deviated from normal values were associated with higher probabilities of readmission (Appenfix V-A).
Higher risks of major perioperative complication were associated with anterior-posterior combined procedures and posterior fusion greater than 6 levels (Appendix I-B), postoperative diagnoses of infection, solitary tumor and cervical fractures/dislocations (Appendix II-B), older age, higher body mass index (BMI) (Appendix III-B), and history of certain medical comorbidities (Appendix IV-B). Perioperative lab data that deviated from normal values were associated with higher risks of major perioperative complications (Appendix V-B).
Multivariable Analysis: Independent Risk Factors for Unplanned Readmission
Independent risk factors for unplanned readmission related to index surgery included: surgical procedure type (highest hazard ratio: anterior and posterior together), postoperative diagnosis (highest hazard ratio: solitary tumor), age (highest hazard ratio: more than 70 years), history of chronic obstructive pulmonary disease (COPD), preoperative dialysis, The American Society of Anesthesiologists Physical Status classification (ASA class, highest hazard ratio: ASA 4–5) (Table 2). Other diagnoses associated with increased hazard ratio for readmission included cervical fracture/dislocation and thoracolumbar spondylosis/stenosis/disc disease.
Table 2. Independent risk factors for unplanned readmission related to index surgery assessed by multivariable Cox proportional hazards model.
REF: reference group for comparison. CVA: cerebral vascular accident; SSI: surgical site infection.
| Independent risk factors for unplanned readmission (I): surgical procedure type, postoperative diagnosis, patient characteristics, medical profiles, preoperative labs | |||||
|---|---|---|---|---|---|
| Category | Variable | p value | Hazard Ratio (HR) | 95% HR Confidence Interval (low, high) | |
| Surgical procedure type | Anterior surgery only - 2–3 levels or fewer | (REF) | |||
| Anterior and posterior together | 0.010 | 1.8 | 1.1 | 2.7 | |
| Anterior surgery only - more than 3 levels | 0.057 | 1.4 | 1.0 | 1.9 | |
| Posterior only - up to 6 levels | 0.32 | 1.1 | 0.9 | 1.4 | |
| Posterior only - greater than 6 levels | 0.10 | 1.3 | 0.9 | 1.8 | |
| Diagnosis group | Cervical Spondylosis/Stenosis/Disc | (REF) | |||
| Solitary tumor (malignant or benign) | <0.001 | 3.0 | 1.8 | 4.8 | |
| Cervical Fractures/Dislocations | 0.026 | 1.9 | 1.1 | 3.5 | |
| Thoracolumbar Spondylosis/Stenosis/Disc | <0.001 | 1.7 | 1.3 | 2.1 | |
| Spondylolisthesis | 0.054 | 1.4 | 1.0 | 2.0 | |
| Disseminated tumor | 0.094 | 1.6 | 0.9 | 2.9 | |
| Thoracolumbar Fractures/Dislocations | 0.71 | 1.1 | 0.6 | 2.2 | |
| Spinal Fractures/Dislocations, Others, Unspecified | 0.37 | 1.3 | 0.7 | 2.4 | |
| Infection | 0.76 | 0.9 | 0.4 | 1.8 | |
| Scoliosis | 0.48 | 1.2 | 0.8 | 1.7 | |
| Other | 0.28 | 0.8 | 0.6 | 1.2 | |
| Age | 18–40 | 0.96 | 1.0 | 0.7 | 1.5 |
| 41–50 | (REF) | ||||
| 51–60 | 0.013 | 1.4 | 1.1 | 1.9 | |
| 61–70 | 0.006 | 1.5 | 1.1 | 2.0 | |
| > 70 | 0.002 | 1.6 | 1.2 | 2.2 | |
| History of severe COPD | Yes vs. No | <0.001 | 1.9 | 1.5 | 2.6 |
| ASA class | 1–2 (No/Mild Disturb) | (REF) | |||
| 3 (Severe Disturb) | <0.001 | 1.4 | 1.1 | 1.6 | |
| 4–5 (Life Threat/Moribund) | 0.016 | 1.6 | 1.1 | 2.2 | |
| Unknown | <0.001 | 5.2 | 2.1 | 12.8 | |
| Preoperative serum creatinine (mg/dL) | < 1.5 | (REF) | |||
| ≥ 1.5 | 0.040 | 1.5 | 1.0 | 2.3 | |
| Unknown | 0.88 | 1.1 | 0.5 | 2.2 | |
| Preoperative INR | < 1.5 | (REF) | |||
| ≥ 1.5 | 0.001 | 2.6 | 1.5 | 4.7 | |
| Unknown | 0.25 | 0.9 | 0.7 | 1.1 | |
| Currently on dialysis (preop) | Yes vs. No | 0.035 | 2.5 | 1.1 | 5.7 |
| Independent risk factors for unplanned readmission (II): major perioperative complications during or after index hospitalization as risk factors | |||||
|---|---|---|---|---|---|
| Category | Variable | p value | Hazard Ratio (HR) | 95% HR Confidence Interval (low, high) | |
| Deep/Organ Space SSI | Yes vs. No | <0.001 | 78.7 | 59.5 | 104.2 |
| Pulmonary Embolism | Yes vs. No | <0.001 | 10.0 | 6.6 | 15.1 |
| Acute renal failure | Yes vs. No | 0.001 | 6.8 | 2.1 | 22.2 |
| Stroke/CVA with neurological deficit | Yes vs. No | 0.015 | 2.8 | 1.2 | 6.2 |
| Risk factors that were also adjusted for, but were considered “non-significant” with the p value less than 0.05: | |||||
|---|---|---|---|---|---|
| Category | Variable | p value | Hazard Ratio (HR) | 95% HR Confidence Interval (low, high) | |
| Gender | Male vs. Female | 0.42 | 0.9 | 0.8 | 1.1 |
| Current smoker within one year | Yes vs. No | 0.95 | 1.0 | 0.8 | 1.2 |
| >10% loss body weight in last 6 months | Yes vs. No | 0.73 | 1.2 | 0.5 | 2.7 |
| Dyspnea | At rest/Moderate exertion vs. No | 0.99 | 1.0 | 0.8 | 1.3 |
| Congestive heart failure in 30 days before surgery | Yes vs. No | 0.93 | 1.0 | 0.4 | 2.6 |
| Hypertension requiring medication | Yes vs. No | 0.97 | 1.0 | 0.8 | 1.2 |
| Insulin-dependent Diabetes | Yes vs. No | 0.097 | 1.3 | 1.0 | 1.7 |
| Steroid use for chronic condition | Yes vs. No | 0.060 | 1.3 | 1.0 | 1.8 |
| Bleeding disorders | Yes vs. No | 0.58 | 1.2 | 0.7 | 1.9 |
| Preoperative serum sodium (mmol/L) | ≤ 130 | 0.89 | 1.0 | 0.5 | 2.1 |
| > 130 | (REF) | ||||
| Unknown | 0.99 | 1.0 | 0.5 | 1.9 | |
| Preoperative BUN (mg/dL) | ≤ 40 | (REF) | |||
| > 40 | 0.17 | 0.6 | 0.3 | 1.3 | |
| Unknown | 0.59 | 0.9 | 0.5 | 1.5 | |
| Preoperative WBC count (/mL) | < 12,000 | (REF) | |||
| ≥ 12,000 | 0.76 | 1.1 | 0.8 | 1.5 | |
| Unknown | 0.093 | 0.3 | 0.1 | 1.2 | |
| Preoperative hematocrit (%) | ≤ 24 | 0.93 | 1.0 | 0.4 | 2.7 |
| > 24 to ≤ 35 | (REF) | ||||
| > 35 | 0.91 | 1.0 | 0.8 | 1.3 | |
| Unknown | 0.85 | 0.9 | 0.3 | 2.8 | |
| Preoperative platelet count (/mL) | ≤ 50,000 | 0.15 | 2.3 | 0.7 | 7.4 |
| > 50,000 | (REF) | ||||
| Unknown | 0.11 | 2.5 | 0.8 | 7.6 | |
| Unplanned intubation | Yes vs. No | 0.86 | 0.9 | 0.5 | 1.8 |
| Cardiac arrest requiring CPR | Yes vs. No | 0.70 | 1.3 | 0.3 | 5.6 |
| Myocardial infarction | Yes vs. No | 0.094 | 2.2 | 0.9 | 5.5 |
Multivariable analysis: Associations of Postoperative Major and Minor Complications with Unplanned Readmission
The following postoperative complications occurring during or after discharge from the index hospitalization were closely associated with unplanned readmission, from highest to lowest hazard ratio: deep/organ space SSI, pulmonary embolism, acute renal failure, and stroke/CVA with neurological deficit (Table 2).
In a second model that assessed postoperative complications that occurred during the index hospitalization as binary covariates, postoperative complications that were independently associated with increased risk of unplanned related readmission were acute renal failure as well as deep/organ space SSI; other complications assessed were not associated with readmission when the complication occurred during the index hospitalization (Table 3).
Table 3.
Association of complications during index hospitalization with unplanned readmission related to index surgery assessed by a second Cox proportional hazard model that considered complications as binary covariates.* REF: control group for comparison.
| Category | p value | Hazard Ratio (HR) | 95% HR Confidence Interval (low, high) | |
|---|---|---|---|---|
| Acute renal failure complication at index hospitalization | 0.003 | 6.0 | 1.8 | 19.6 |
| Deep/OrganSpace SSI at Index Hospitalization | 0.034 | 3.5 | 1.1 | 11.3 |
Also adjusted for the following factors, surgical procedure type, diagnosis group, gender, age, current smoker, >10% loss body weight in last 6 months, dyspnea, history of severe COPD, congestive heart failure in 30 days before surgery, hypertension requiring medication, insulin-dependent diabetes, steroid use for chronic condition, bleeding disorders, preoperative dialysis, ASA class, preoperative serum sodium, preoperative BUN, preoperative serum creatinine, preoperative WBC count, preoperative hematocrit, preoperative platelet count, preoperative INR, pulmonary embolism, unplanned intubation, cardiac arrest requiring CPR, myocardial infarction, and stroke/CVA with neurological deficit.
The presence of any minor complication during index admission was associated with increased risk of readmission (hazard ratio 1.3, 95% CI 1.1 to 1.6, p=0.017).
Multivariable Analysis: Independent Risk Factors for Major Perioperative Complications
Independent risk factors for major perioperative complication included: surgical procedure type (highest odds ratio: anterior and posterior together), postoperative diagnosis (highest odds ratio: solitary tumor), age (highest odds ratio: more than 70 years), BMI (highest odds ratio: BMI ≥ 40), race (highest odds ratio: black), current smoker within one year, more than 10% body weight loss in last 6 months, preoperatively on dialysis, and ASA class (highest odds ratio: ASA 4–5) (Table 4).
Table 4.
Independent risk factors for major perioperative complications assessed by multivariable logistic regression. REF: control group for comparison.
| (I) Independent risk factors for major perioperative complications: | |||||
|---|---|---|---|---|---|
| Category | Variable | p value | Odds Ratio (OR) | 95% Confidence Intervalfor OR (low, high) | |
| Surgical procedure type | Anterior surgery only - 2–3 levels or fewer | (REF) | |||
| Anterior surgery only - more than 3 levels | 0.017 | 1.4 | 1.1 | 2.0 | |
| Anterior and posterior together | <0.001 | 2.6 | 1.8 | 3.8 | |
| Posterior only - up to 6 levels | <0.001 | 1.5 | 1.2 | 1.8 | |
| Posterior only - greater than 6 levels | <0.001 | 2.3 | 1.8 | 3.0 | |
| Diagnosis group | Cervical Spondylosis/Stenosis/Disc | (REF) | |||
| Disseminated tumor | 0.037 | 1.6 | 1.0 | 2.5 | |
| Solitary tumor (malignant or benign) | <0.001 | 4.0 | 2.6 | 6.0 | |
| Cervical Fractures/Dislocations | <0.001 | 3.4 | 2.2 | 5.1 | |
| Thoracolumbar Spondylosis/Stenosis/Disc | <0.001 | 1.4 | 1.2 | 1.8 | |
| Spinal Fractures/Dislocations, Others, Unspecified | 0.018 | 1.7 | 1.1 | 2.6 | |
| Infection | <0.001 | 3.2 | 1.9 | 5.3 | |
| Scoliosis | <0.001 | 1.8 | 1.4 | 2.5 | |
| Others | 0.014 | 1.4 | 1.1 | 1.9 | |
| Thoracolumbar Fractures/Dislocations | 0.059 | 1.7 | 1.0 | 2.8 | |
| Spondylolisthesis | 0.085 | 1.3 | 1.0 | 1.8 | |
| Age | 18–40 | 0.85 | 1.0 | 0.7 | 1.5 |
| 41–50 | (REF) | ||||
| 51–60 | <0.001 | 1.7 | 1.3 | 2.3 | |
| 61–70 | <0.001 | 2.0 | 1.5 | 2.6 | |
| >70 | <0.001 | 2.4 | 1.8 | 3.2 | |
| BMI | <18.5 | 0.44 | 0.8 | 0.4 | 1.4 |
| 18.5–24.9 | (REF) | ||||
| 25.0–29.9 | 0.60 | 1.0 | 0.8 | 1.1 | |
| 30.0–34.9 | 0.18 | 0.9 | 0.7 | 1.1 | |
| 35.0–39.9 | 0.80 | 1.0 | 0.8 | 1.2 | |
| ≥40 | 0.019 | 1.4 | 1.1 | 1.8 | |
| Race | White | (REF) | |||
| Black | <0.001 | 1.6 | 1.3 | 2.0 | |
| Other or Unknown | 0.49 | 0.9 | 0.7 | 1.2 | |
| Current smoker within one year | Yes vs. No | 0.028 | 1.2 | 1.0 | 1.4 |
| >10% body weight loss in last 6 months | Yes vs. No | 0.002 | 2.3 | 1.4 | 3.9 |
| Steroid use for chronic condition | Yes vs No | 0.004 | 1.5 | 1.1 | 1.9 |
| Currently on dialysis (preop) | Yes vs No | 0.002 | 2.7 | 1.4 | 5.2 |
| ASA class | 1–2 (No/Mild Disturb) | (REF) | |||
| 3 (Severe Disturb) | <0.001 | 1.5 | 1.3 | 1.7 | |
| 4–5 (Life Threat/Moribund) | <0.001 | 2.6 | 2.0 | 3.5 | |
| Unknown | 0.64 | 0.6 | 0.1 | 4.6 | |
| Preoperative WBC count (/mL) | < 12,000 | (REF) | |||
| ≥ 12,000 | 0.012 | 1.4 | 1.1 | 1.8 | |
| Unknown | 0.45 | 0.6 | 0.2 | 2.2 | |
| Preoperative hematocrit (%) | ≤ 24 | 0.31 | 0.6 | 0.2 | 1.6 |
| > 24 to ≤ 35 | (REF) | ||||
| > 35 | 0.007 | 0.8 | 0.6 | 0.9 | |
| Unknown | 0.59 | 0.8 | 0.3 | 1.9 | |
| Preoperative platelet count (/mL) | > 50,000 | (REF) | |||
| ≤ 50,000 | 0.035 | 3.2 | 1.1 | 9.5 | |
| Unknown | 0.48 | 1.5 | 0.5 | 5.0 | |
| (II) Risk factors that were also adjusted for, but were considered “non-significant” with the p value less than 0.05: | |||||
|---|---|---|---|---|---|
| Category | Variable | p value | Hazard Ratio (HR) | 95% HR Confidence Interval (low, high) | |
| Gender | Male vs. Female | 0.17 | 1.1 | 1.0 | 1.3 |
| Dyspnea | Yes vs. No | 0.074 | 1.2 | 1.0 | 1.6 |
| History of severe COPD | Yes vs. No | 0.69 | 0.9 | 0.7 | 1.3 |
| Congestive heart failure in 30 days before surgery | Yes vs. No | 0.28 | 1.5 | 0.7 | 3.0 |
| Hypertension requiring medication | Yes vs. No | 0.91 | 1.0 | 0.8 | 1.2 |
| Insulin-dependent Diabetes | Yes vs. No | 0.68 | 1.1 | 0.8 | 1.4 |
| Bleeding disorders | Yes vs. No | 0.094 | 1.4 | 0.9 | 2.0 |
| Preoperative serum sodium (mmol/L) | ≤ 130 | 0.98 | 1.0 | 0.6 | 1.7 |
| > 130 | (REF) | ||||
| Unknown | 0.58 | 1.2 | 0.7 | 2.0 | |
| Preoperative BUN (mg/dL) | ≤ 40 | (REF) | |||
| > 40 | 0.72 | 0.9 | 0.5 | 1.6 | |
| Unknown | 0.17 | 1.3 | 0.9 | 2.0 | |
| Preoperative serum creatinine (mg/dL) | < 1.5 | (REF) | |||
| ≥ 1.5 | 0.17 | 1.3 | 0.9 | 1.8 | |
| Unknown | 0.20 | 0.7 | 0.4 | 1.2 | |
| Preoperative INR | < 1.5 | (REF) | |||
| ≥ 1.5 | 0.14 | 1.6 | 0.9 | 2.8 | |
| Unknown | 0.37 | 0.9 | 0.8 | 1.1 | |
Discussion
The present study provides benchmark data regarding the risks of unplanned readmission and perioperative major complications based on a large, prospective high-quality database with 30-day follow-up after index surgery. Complications and unplanned readmissions were closely associated with surgeries performed for solitary tumor, cervical fractures/dislocations, and thoracolumbar spondylosis/stenosis/disc. These data document reliable percentages of complications and readmissions from a large multicenter database. Our analysis focused on unplanned readmissions related to the index surgery captured in the NSQIP database from year 2012 through 2013. This facilitated exclusion of planned and unrelated readmission events that could confound the readmission rates23. The high case volume from multiple institutions, prospective-enrollment nature and detailed demographic and medical profile information still provided meaningful information regarding readmission rates.
Our methodology had several limitations. The database only includes 30-day post-operative follow-up. Patients may have had readmissions or complications after the 30-day window, which are not captured in the follow-up period. Accordingly, this is not a suitable database to evaluate fusion rates or durability of the surgical construct, as implant problems, delayed infection, and pseudarthrosis may present up to several years after the index surgery. Further, the nature of the present study precluded us from looking for strict cause-consequence relationship and rather only at associations. The stratification of diagnoses and laboratory values and certain continuous variables were a simplification of the patient’s true physiological state and underlying medical condition. For instance, radiographic review and detailed data regarding fracture type, tumor diagnoses, and associated comorbidities were not available. Accuracy of coding and inclusion of all procedures performed may vary from one institution to the next24–26. For this reason, we sought to capture only fusion procedures. We did not subcategorize whether decompression or an osteotomy had been performed in addition to the fusion.
Other limitations of the NSQIP database include a lack of data on perioperative pain control. Similarly, NSQIP provides no data regarding the cause of death or whether prolonged hospitalization is related to the index surgery. For this reason, we were not able to include patient mortality as a primary outcome measure. Last but not least, the progression of underlying medical diseases can alter the risk for perioperative major complications, as shown by the association of renal impairment with lumbar spine surgeries27 as well as liver diseases with a variety of surgical procedures28. Accounting for such associations is out of the scope of the present study both because it warrants a distinct set of analysis methodologies and because NSQIP does not provide longitudinal progression of the patients’ medical comorbidities.
The present study found an overall rate of unplanned readmissions related to the index surgery of 4.4% per 30 person-days. This is on par with the overall unplanned readmission rate reported for lumbar spine surgery15, which was based on a variety of lumbar spinal procedures and included data only from year 2012 in the NSQIP database. Of note, our analysis focused on spinal fusion surgery of the cervical, thoracic and lumbar spines and included NSQIP data from both years 2012 and 2013. Our findings also provided novel information regarding how major complication interacts with unplanned readmission. In addition, we utilized the person-year method rather than raw unplanned readmission percentages. This more accurately assessed independent risk factors of unplanned readmission within thirty days of the index surgery.
In addition, the readmission rate of 4.4% per 30 person-days is similar to that of approximately 3.8%13 to 8.4%10 reported by various authors for readmission within 30 days following adult spine surgery, 4.6% for total knee arthroplasty and 4.2% for total hip arthroplasty found in another study using the NSQIP database14. A NSQIP pediatric cohort undergoing spine deformity surgery had a 3.96% readmission rate29. Using the NSQIP patient cohort in year 2011, similar risk factors for 30-day readmission have been reported, such as older age and high ASA class for primary total knee arthroplasty, and obesity as well as steroid use for primary total hip arthroplasty14.
Targeted preoperative planning for these patients may improve the underlying medical conditions and thus possibly decrease the risk of unplanned readmission and complications during the first 30 days after index surgery. Compared to ASA classification 1–2 patients, ASA 4–5 patients were 1.6 times higher risk for unplanned readmission and 2.6 times higher risk for major complications compared to ASA 1–2, while ASA 3 patients presented 1.4 times and 1.5 times higher risk, respectively. Improved control of heart disease, hypertension, diabetes, COPD and asthma could potentially decrease ASA classification and lower perioperative risk. Likewise, weight reduction may decrease the likelihood of major perioperative complications. Patients with a BMI more than 40 resulted in a 1.4 times increased risk of complications relative to patients with a BMI 18.5 to less than 25, while patients with a BMI of 25.0–39.9 did not have an increased major perioperative complication rate. Furthermore, appropriate medical management to bring preoperative serum creatinine to lower than 1.5 mg/dL or INR to less than 1.5 could possibly remediate the risk for unplanned readmission. Interventions may not cure the underlying diseases, but may fine tune the patients’ perioperative parameters and lower the risk of perioperative complications30,31. Some interventions likely need to be planned well ahead of time and require a “total care” approach with multiple specialties involved and are only suited for elective procedures.
For patients with risk factors that are not modifiable, our results provide relevant information for patient counseling and shared surgeon-patient decision-making. In certain scenarios, less aggressive management may be considered for patients 1,32. For example, decompression alone or a shorter fusion may be an alternative for select high risk patients who wish to decrease their risk of readmission or perioperative complications1.
Identification of patients at higher risk of readmission and complications is the first step towards minimizing 30-day unplanned readmission and major complications to improve the quality of care and optimize medical resource use from the payers’ perspective. Previous reports focused on Medicare beneficiaries found the overall readmissions are prevalent and costly up to $17 billion annually33. Our results inform future studies and work in quality improvement, necessary in the context of more common financial penalties for readmissions, bundled payments and the implementation of the Affordable Care Act.4
These policies aim to improve the quality of care and accessibility. Nevertheless, they can also lead to unexpected financial problems, repercussions in delivered quality of care and physician-patient relationship as well as potential undue influence on the surgeon’s decision-making on treatment strategies. Such issues have been observed in another developed country, Taiwan, where similar policies have been on track since 199534–37. Further cost-efficiency and cost-effectiveness studies on adult spine surgery can hopefully lead to the point where the goals of the patient, provider and the payer are well balanced and potentially provide fair reimbursement for high quality care for the most complex patients.
In conclusion, we found increased complications rates and readmission rates in patients with more extensive surgical procedures, older age, and specific diagnoses such as solitary tumor. Patients with deep/organ space SSI had around 79 times the odds of unplanned readmission. Patients and surgical procedures that carry the highest risk of readmission and 30-day complications should be targeted for special interventions as well as proportional reimbursement to assure high quality care. Our results provide new information from a high quality database to provide benchmarks for surgeons and payers and to assist in planning targeted perioperative interventions to aimed to reduce complications and readmissions.
Supplementary Material
Footnotes
The manuscript submitted does not contain information about medical device(s)/drug(s).
No relevant financial activities outside the submitted work.
No funds were received in support of this work.
References
- 1.Deyo RA, Mirza SK, Martin BI, et al. Trends, major medical complications, and charges associated with surgery for lumbar spinal stenosis in older adults. JAMA. 2010;303:1259–65. doi: 10.1001/jama.2010.338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Carragee EJ. The increasing morbidity of elective spinal stenosis surgery: is it necessary? JAMA. 2010;303:1309–10. doi: 10.1001/jama.2010.402. [DOI] [PubMed] [Google Scholar]
- 3.Smith JS, Fu KM, Polly DW, Jr, et al. Complication rates of three common spine procedures and rates of thromboembolism following spine surgery based on 108,419 procedures: a report from the Scoliosis Research Society Morbidity and Mortality Committee. Spine. 2010;35:2140–9. doi: 10.1097/BRS.0b013e3181cbc8e7. [DOI] [PubMed] [Google Scholar]
- 4.Epstein AM. Revisiting readmissions--changing the incentives for shared accountability. New England Journal of Medicine. 2009;360:1457–9. doi: 10.1056/NEJMe0901006. [DOI] [PubMed] [Google Scholar]
- 5.Foster DHG. Healthcare Reform: Pending Changes to Reimbursement for 30-Day Readmissions. Research Brief. 2010
- 6.Medicare-Payment-Advisory-Comission. Report to the Congress. 2014. Medicare Payment Policy. [Google Scholar]
- 7. [Accessed Apr 20, 2015];Readmissions Reduction Program. 2014 Aug 04; Available at: http://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/Readmissions-Reduction-Program.html.
- 8. [Accessed Apr 11, 2015];Patient Protection and Affordable Care Act, HR3590, 111th Congress (2009–2010) Available at: http://www.gpo.gov/fdsys/pkg/BILLS-111hr3590eas/pdf/BILLS-111hr3590eas.pdf.
- 9.Wang S, Zhang J, Qiu G, et al. Dual growing rods technique for congenital scoliosis: more than 2 years outcomes: preliminary results of a single center. Spine. 2012;37:E1639–44. doi: 10.1097/BRS.0b013e318273d6bf. [DOI] [PubMed] [Google Scholar]
- 10.Schairer WW, Carrer A, Deviren V, et al. Hospital Readmission After Spine Fusion for AdultSpinal Deformity. Spine. 2013;38:1681–9. doi: 10.1097/BRS.0b013e31829c08c9. [DOI] [PubMed] [Google Scholar]
- 11.Lovecchio F, Hsu WK, Smith TR, et al. Predictors of Thirty-Day Readmission After Anterior Cervical Fusion. Spine. 2014;39:127–33. doi: 10.1097/BRS.0000000000000051. [DOI] [PubMed] [Google Scholar]
- 12.Modhia U, Takemoto S, Braid-Forbes MJ, et al. Readmission Rates After Decompression Surgery in Patients With Lumbar Spinal Stenosis Among Medicare Beneficiaries. Spine. 2013;38:591–6. doi: 10.1097/BRS.0b013e31828628f5. [DOI] [PubMed] [Google Scholar]
- 13.McCormack RA, Hunter T, Ramos N, et al. An Analysis of Causes of Readmission After Spine Surgery. Spine. 2012;37:1260–6. doi: 10.1097/BRS.0b013e318245f561. [DOI] [PubMed] [Google Scholar]
- 14.Pugely AJ, Callaghan JJ, Martin CT, et al. Incidence of and risk factors for 30-day readmission following elective primary total joint arthroplasty: analysis from the ACS-NSQIP. The Journal of arthroplasty. 2013;28:1499–504. doi: 10.1016/j.arth.2013.06.032. [DOI] [PubMed] [Google Scholar]
- 15.Pugely AJ, Martin CT, Gao Y, et al. Causes and risk factors for 30-day unplanned readmissions after lumbar spine surgery. Spine. 2014;39:761–8. doi: 10.1097/BRS.0000000000000270. [DOI] [PubMed] [Google Scholar]
- 16. [Accessed Apr 2015, 2015];Program ACoSNSQI. 2015 Available at: http://www.facs.org/quality-programs/acs-nsqip.
- 17.Shubert CR, Habermann EB, Truty MJ, et al. Defining perioperative risk after hepatectomy based on diagnosis and extent of resection. J Gastrointest Surg. 2014;18:1917–28. doi: 10.1007/s11605-014-2634-x. [DOI] [PubMed] [Google Scholar]
- 18.Shubert CR, Habermann EB, Bergquist JR, et al. A NSQIP Review of Major Morbidity and Mortality of Synchronous Liver Resection for Colorectal Metastasis Stratified by Extent of Liver Resection and Type of Colorectal Resection. J Gastrointest Surg. 2015;19:1982–94. doi: 10.1007/s11605-015-2895-z. [DOI] [PubMed] [Google Scholar]
- 19. [Accessed Apr 04, 2015];30-day unplanned readmission and death measures. Available at: http://www.medicare.gov/hospitalcompare/Data/30-day-measures.html.
- 20.Tang H, Zhu J, Ji F, et al. Risk factors for postoperative complication after spinal fusion and instrumentation in degenerative lumbar scoliosis patients. J Orthop Surg Res. 2014;9:15. doi: 10.1186/1749-799X-9-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Veeravagu A, Patil CG, Lad SP, et al. Risk factors for postoperative spinal wound infections after spinal decompression and fusion surgeries. Spine. 2009;34:1869–72. doi: 10.1097/BRS.0b013e3181adc989. [DOI] [PubMed] [Google Scholar]
- 22.McCunniff PT, Young ES, Ahmadinia K, et al. Smoking is Associated with Increased Blood Loss and Transfusion Use After Lumbar Spinal Surgery. Clin Orthop Relat R. 2015 doi: 10.1007/s11999-015-4650-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Amin BYTT, Schairer WW, Na L, Takemoto S, Berven S, Deviren V, Ames C, Chou D, Mummaneni PV. Pitfalls of calculating hospital readmission rates based on nonvalidated administrative data sets. J Neurosurg Spine. 2013;18:134–8. doi: 10.3171/2012.10.SPINE12559. [DOI] [PubMed] [Google Scholar]
- 24.Faciszewski T, Broste SK, Fardon D. Quality of data regarding diagnoses of spinal disorders in administrative databases. A multicenter study. The Journal of bone and joint surgery American volume. 1997;79:1481–8. doi: 10.2106/00004623-199710000-00004. [DOI] [PubMed] [Google Scholar]
- 25.Romano PS, Chan BK, Schembri ME, et al. Can administrative data be used to compare postoperative complication rates across hospitals? Med Care. 2002;40:856–67. doi: 10.1097/00005650-200210000-00004. [DOI] [PubMed] [Google Scholar]
- 26.Deyo RA, Taylor VM, Diehr P, et al. Analysis of automated administrative and survey databases to study patterns and outcomes of care. Spine. 1994;19:2083S–91S. doi: 10.1097/00007632-199409151-00011. [DOI] [PubMed] [Google Scholar]
- 27.Martin CT, Pugely AJ, Gao Y, et al. The Impact of Renal Impairment on Short-term Morbidity Risk Following Lumbar Spine Surgeries. Spine. 2015;40:909–16. doi: 10.1097/BRS.0000000000000890. [DOI] [PubMed] [Google Scholar]
- 28.Friedman LS. The risk of surgery in patients with liver disease. Hepatology. 1999;29:1617–23. doi: 10.1002/hep.510290639. [DOI] [PubMed] [Google Scholar]
- 29.Martin CT, Pugely AJ, Gao Y, et al. Causes and Risk Factors for 30-Day Unplanned Readmissions After Pediatric Spinal Deformity Surgery. Spine. 2015;40:238–46. doi: 10.1097/BRS.0000000000000730. [DOI] [PubMed] [Google Scholar]
- 30.Guzman JZ, Iatridis JC, Skovrlj B, et al. Outcomes and complications of diabetes mellitus on patients undergoing degenerative lumbar spine surgery. Spine. 2014;39:1596–604. doi: 10.1097/BRS.0000000000000482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Guzman JZ, Skovrlj B, Shin J, et al. The impact of diabetes mellitus on patients undergoing degenerative cervical spine surgery. Spine. 2014;39:1656–65. doi: 10.1097/BRS.0000000000000498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Weinstein JN, Lurie JD, Tosteson TD, et al. Surgical versus nonoperative treatment for lumbar disc herniation: four-year results for the Spine Patient Outcomes Research Trial (SPORT) Spine (Phila Pa 1976) 2008;33:2789–800. doi: 10.1097/BRS.0b013e31818ed8f4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the Medicare fee-for-service program. New England Journal of Medicine. 2009;360:1418–28. doi: 10.1056/NEJMsa0803563. [DOI] [PubMed] [Google Scholar]
- 34.Tsai Y-W, Hu T-W. National health insurance, physician financial incentives, and primary cesarean deliveries in Taiwan. American journal of public health. 2002;92:1514–7. doi: 10.2105/ajph.92.9.1514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Lin H-C, Xirasagar S, Tang C-H. Costs per discharge and hospital ownership under prospective payment and cost-based reimbursement systems in Taiwan. Health policy and planning. 2004;19:166–76. doi: 10.1093/heapol/czh020. [DOI] [PubMed] [Google Scholar]
- 36.Cheng S-H, Chen C-C, Chang W-L. Hospital response to a global budget program under universal health insurance in Taiwan. Health Policy. 2009;92:158–64. doi: 10.1016/j.healthpol.2009.03.008. [DOI] [PubMed] [Google Scholar]
- 37.Xirasagar S, Lin H-C. Cost convergence between public and for-profit hospitals under prospective payment and high competition in Taiwan. Health services research. 2004;39:2101–16. doi: 10.1111/j.1475-6773.2004.00334.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.