Abstract
Background:
Diabetic retinopathy and its consequence, diabetic macular edema, are leading causes of vision loss in diabetics and can develop even in the first years after onset of diabetes. Being asymptomatic in primary phase and having compensatory effect of bilateral vision delay the necessity of eye care utilization. We conducted this study to determine diabetic individuals’ level of awareness about the importance of regular eye examinations.
Methods:
As part of the cross-sectional, population-based, Yazd Eye Study on people aged 40–80 years, diabetic participants were identified for enrollment in this research. Participants underwent thorough ophthalmic examinations as well as detailed interview. Well-trained interviewers asked participants about their awareness of screening eye examinations and their necessity. Fasting blood sugar, glycated hemoglobin, and complete lipid profile were assessed. All descriptive and analytic tests were done in survey mode. Logistic regression was applied to assess related risk factors.
Results:
Among 497 diabetic persons out of 2098 participants, 364 respondents (73.4%; 95% confidence interval: 68.6-78.2) were not aware of the necessity of regular eye examinations. Among 133 aware respondents, 21 (16%) respondents had no eye examination over the past year. Educational level significantly correlated with awareness (P = 0.004), and physicians were the most frequent source of awareness (79.7%).
Conclusions:
This study showed that a significant proportion of Yazd diabetic population (about 73%) needs to be informed about the necessity of regular eye examinations. The remaining respondents, who had this information, mainly had undergone regular ophthalmologist visits, which imply that educational interventions could improve the situation.
Keywords: Awareness, diabetes mellitus, diabetic retinopathy
Introduction
Vision problems are understood to have imposed an estimated cost of $3 trillion in 2010, which figures up to $3.6 trillion in 2020, on individuals, health-care systems, and world economy directly and indirectly.[1] Based on the last updated data from the World Health Organization (WHO), the greatest burden of visual impairment throughout the world (65%) belongs to people aged over 50 years, and this figure is up to 82% for blindness;[2] nevertheless, eye care resources are underutilized and not well known.[3,4,5] A previous population-based report from Iran demonstrated that 50% of visually impaired people had no eye examination in the last 5 years.[6] This is confirmed by other studies reporting that only 22% of diabetic individuals in Tehran Province have regular eye examinations.[7]
Diabetes mellitus has become a growing health problem globally[8,9] and 75% of cases with more than 20 years of diabetes are expected to develop diabetic retinopathy (DR) and diabetic macular edema (DME) which are considered as the main causes of visual impairment among people aged 15–64 years[10] and in diabetic population, respectively.[11] According to the Iranian Health Profile Survey, Yazd Province has the highest prevalence rate of diabetes mellitus in Iran,[12] with an estimated prevalence of 16.3% in over 30 years of age group.[13] The reported prevalence of DR in the Yazd diabetic population is 29.6%.[14]
Although it is assumed that unaffordable costs or lack of insurance coverage are the main barriers to eye care utilization even in developed countries,[15] unawareness of the necessity of periodic eye examinations, especially in elder people, is also responsible. Screening diabetic individuals for retinopathy signs through regular eye examinations is the most feasible action, which relies on their active cooperation.[16] Community awareness is a key element to succeed in any screening program like screening for DR. This investigation aimed to determine the proportion of diabetic people who are aware of the necessity of having regular eye examinations and those who had at least one comprehensive eye examination during the 12 months before the study.
Methods
This research is a part of the Yazd Eye, cross-sectional, population-based study on people aged 40–80 years in a central district of Iran during 2010–2011. Multi-stage random cluster sampling was applied to invite 2320 persons of urban and rural dwellers of Yazd district. Details of the Yazd Eye Study design and methodology have already been published.[17] Ethical approval was obtained from the Ethics Committee of Shahid Beheshti University of Medical Sciences. All participants were asked to sign a written informed consent before data collection and clinical examination.
For this study, we enrolled diabetic participants of the Yazd Eye Study who were identified through fasting blood sugar (FBS) ≥126 mg/dl tests on 2 separate days or self-reports of a physician diagnosis of diabetes. In addition to their eye examination results, we used data collected from the last part of the 8-section questionnaire which concerned subjects’ knowledge and practice regarding eye care. In this section, participants were asked if they had regular eye examinations (at least once a year), whether they were aware of the necessity of screening eye examinations, and what their source of awareness was (physicians, family, media, or publications).
Using WHO definitions, we defined moderate to severe visual impairment or low vision as a best-corrected visual acuity (BCVA) >0.48 LogMAR (20/60) and ≤1.30 LogMAR (20/400) and blindness as BCVA >1.30 LogMAR.[2] DR was defined by masked grading of stereoscopic fundus photographs based on the early treatment DR Study testing protocol.[18]
Levels of blood glycosylated hemoglobin (HbA1c) and FBS were determined, and a lipid profile including triglycerides, low-density lipoprotein (LDL), high-density lipoprotein (HDL), and cholesterol was assessed. HbA1c values ≥7% were considered as uncontrolled blood sugar.[19] Uncontrolled dyslipidemia was defined as fasting blood level of triglyceride >150 mg/dL (1.7 mmol/L), cholesterol >150 mg/dL (3.9 mmol/L), LDL >130 mg/dL (3.4 mmol/L), or HDL <35 mg/dL (0.9 mmol/L). Blood pressure was measured twice at the same session, after 5 min of rest in sitting posture, and the average of these two was recorded. Data on smoking, diet, and exercise were collected too. To enter education as a binary variable, we combined illiterate and primary education for one value against secondary and higher levels. Diet data were categorized into specific diabetic diet, nonspecific diet, and no diet plan. Exercising at least 3 times per week or having physically active occupations such as working in factories and farms qualified as having regular physical activities.
Cluster design was considered in presenting confidence intervals (CI) and P values. All prevalence rates are reported based on standardized data. Direct standardization was applied for age and gender according to Yazd population that was derived from the 2006 National Census. Studied parameters were examined separately through logistic models. The final logistic regression model was fitted to determine the simultaneous effects of best predictors of participants’ awareness and their related practice.
Results
Of the 2320 eligible participants of the Yazd Eye Study, 2098 individuals (90.4%) entered the study, and 539 were diagnosed with diabetes mellitus (24.5%, 95% CI: 22.5, 26.8).
Awareness
As shown at Figure 1, four hundred ninety-seven diabetic participants answered related questions (response rate: 92.2%). Of these, 364 (73.4%, 95% CI: 68.6, 78.2) were unaware of the necessity of regular eye examinations. Awareness was not statistically associated with age or sex (P = 0.413 and P = 0.451, respectively).
Figure 1.
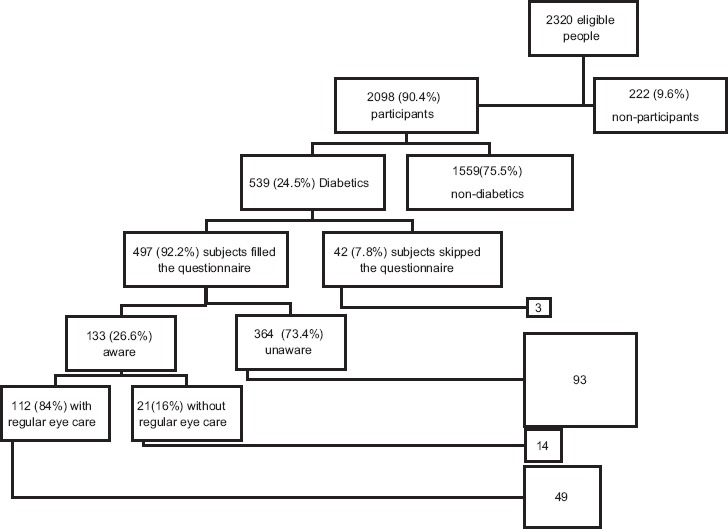
Study enrollment and the proportion of aware subject in the Yazd Eye Study
Awareness and education level
Among all diabetic participants of Yazd Eye Study, 152 (29.2%; 95% CI: 24.6, 33.8) were illiterate. Diabetic individuals were less educated compared to other participants of the Study (P < 0.001), and their awareness showed significant association with education level (P = 0.004). Urban dwellers had higher education level (P = 0.004), and they were more aware (29%) than rural inhabitants (11%) (P = 0.048).
Awareness and diabetes-related factors
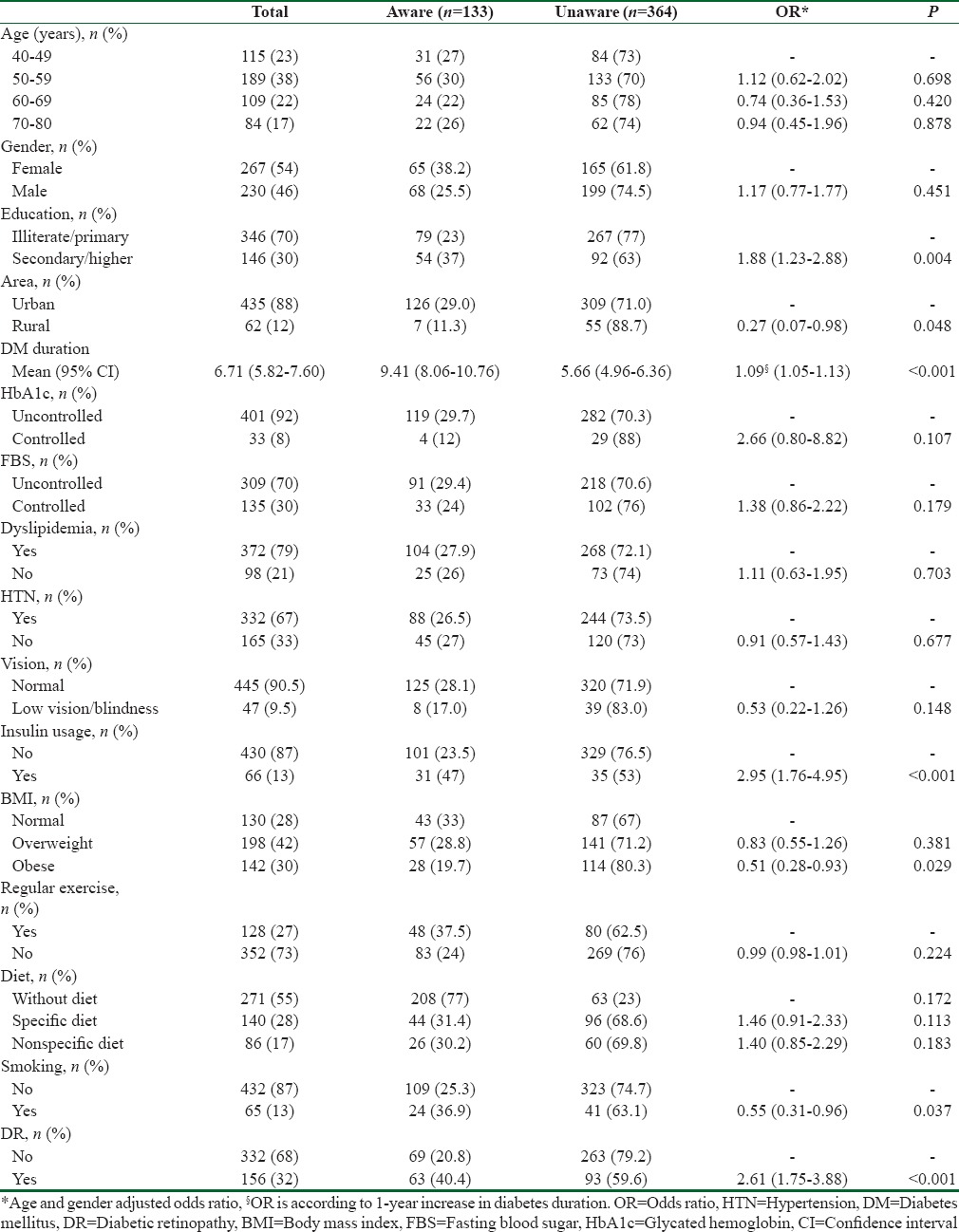
As shown in Table 1, aware participants had longer diabetes duration (9.41 vs. 5.66 years, P < 0.001). Smoking, insulin usage, body mass index (BMI), and HbA1c had significant association with awareness as well [Table 1]. No significant association was observed between awareness and the variables of FBS, hypertension, lipidemia, exercise, or diet (P > 0.05).
Table 1.
Association of awareness of the necessity of regular eye examinations in diabetic participants with some explanatory factors, Yazd Eye Study
Awareness and visual impairment
In terms of BCVA, 42 cases (8.6%; 95% CI: 5.9, 11.3) of the respondents were visually impaired and 7 (1.1%; 95% CI: 0.3, 1.9) were blind. No significant association was observed between awareness and visual impairment (P = 0.148).
Awareness in diabetic retinopathy cases
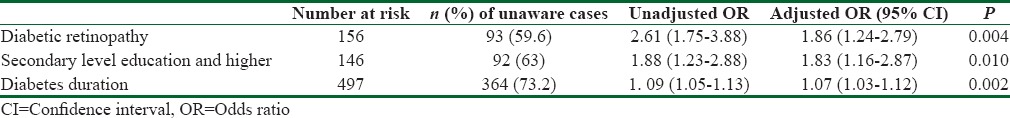
Of all diabetic individuals, DR was confirmed in 159 participants (29.6%; 95% CI: 25.0, 34.3) including 63 (41.5%; 95% CI: 31.8, 51.2) aware participants. Individuals with DR were more likely to be aware of the necessity of regular eye examinations than other diabetic subjects (odds ratio: 2.61; P < 0.001). Based on the best-fitted regression model, more prolonged diabetes, DR, and education level correlated with awareness [Table 2].
Table 2.
Factors associated with awareness of the necessity of regular eye examinations in diabetic participants 40-80 years, Yazd Eye Study
Practice
Among 133 aware participants (26.6%; 95% CI: 21.8, 31.4), 84% (112 of 133) participants declared they had regular eye examinations. Having an eye examination in the last year had no association with age or sex (P = 0.937 and P = 0.555, respectively). In participants with DR, 78% of aware participants (49 of 63) had had an eye examination during the last year.
None of the studied parameters indicated a significant association with having regular eye examinations [Figure 2]. The proportion of people visited by an ophthalmologist was almost the same over all studied categories, and the P value was >0.05 in all comparisons.
Figure 2.
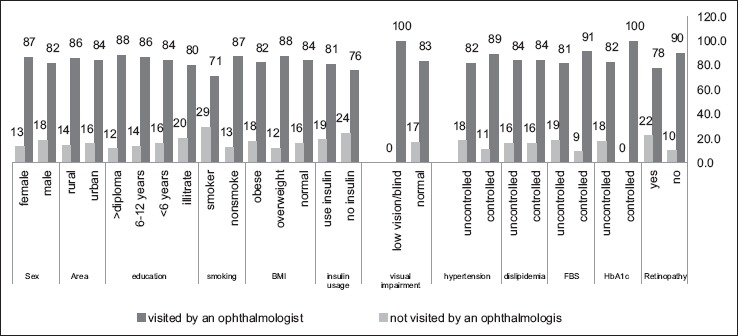
Proportion of adherence to regular eye examination among aware diabetic individuals by some explanatory factors
Source of awareness
For 106 (79.7%) of the 133 aware participants, physicians were mentioned as the main source of awareness; other sources were media for 4 subjects (3%), and family for 2 others (1.5%). For the remaining 21 (15.8%) individuals, the source of information was not clear.
Discussion
Community awareness is a key component of health management programs, and lack of this component cannot be compensated with service coverage or facility improvements. This study showed that a significant proportion of Yazd diabetic population (about 73%) needs to be informed about the necessity of regular eye examinations and would benefit from informative programs. On the other hand, 84% of aware diabetic participants declared they had had at least one ophthalmology visit during the last year. This positive adherence to healthy behavior supports the success of educational programs, as discussed in other studies in Iran.,[20,21] Such programs can be even more beneficial in Yazd Province as the prevalence of diabetes in this region is among the highest in the country.[12] Naturally, the educational level of the target population should be considered to have an effective intervention.
While some studies in Asia[22] illustrated poor healthy behavior in spite of proper knowledge, our data revealed that the majority of subjects with regular eye examinations (112 out of 133 diabetic individuals) acknowledge the importance of regular eye care. However, low literacy level, especially in rural participants, is a drastic barrier for educational interventions. The significant association of educational level with awareness highlighted this fact. To guarantee best achievements, awareness programs can be accompanied by motivational campaigns, as emphasized by Addoor et al.[23] Providing diabetic participants with a free annual ophthalmic visit through the primary health-care services may be beneficial. Furthermore, efficient collaboration between the health sector and educational organizations provides the proper foundation for future actions.
We found that awareness was higher in patients with longer duration of diabetes [Table 1]; this was consistent with previous studies,[24] and implies that individuals with diabetes may not be informed about proper ocular care till the late stages of the disease. Significantly, better awareness among insulin users provides more evidence for this argument. Similarly, previous studies indicated that the shorter the duration of diabetes, the lower the adherence to ophthalmic examinations.[25] This is while DR can develop even during the first 5 years of the disease, and it is not just a long-term complication.[26] The average duration of disease in the aware diabetic participants in our study (27%) was about 5 years longer compared to unaware subjects. Generally, being asymptomatic in early stages and compensation of the unaffected eye for the unilateral vision are two factors that hinder the perception of eye conditions. Huang et al. found this the main cause of unawareness too.[27] Due to the importance of early diagnosis of DR, educational campaigns and screening programs in the first 5 years of the disease are recommended.[28]
Our results regarding the healthy practice of 84% of aware diabetic participants assure the efficiency of educational strategies. Individuals from urban areas were more alert than villagers. Although higher access to specialists and more equipped eye care centers may play an active role, the educational status should not be overlooked. One of the barriers to timely diagnosis of slowly progressing DR and its control in the population is illiteracy. Another barrier is the fact that early symptoms of eye diseases are often considered a normal part of aging, which is a more common misconception among the less educated.
Regarding the source of awareness, physicians were the main source (80%) in our study. Hence, Yazd community is the right place to apply what Huang et al. suggested.[29] They pointed out that the revival of doctor–patient communication, considering the participant's educational level, is the main key. The media including television, magazines, and newspapers provided 3% of the respondents with the needed information. The huge gap between the role of media and other sources in our study should be considered more carefully. Although Saikumar et al.[30] found media as the main source in Southern India; they separated ophthalmologists and general physicians, which provided 62% with information collectively. Our previous study also showed positive evidence for the role of media and acquaintances in publicizing health information in Iran.[31] Among aware DR patients in Tehran, the capital of Iran, family and acquaintances were the main sources of information (59.6%), followed by media (29.8%). These interesting findings highlight the potential power of media in broadcasting health messages on a widespread scale. It may be useful especially for simple and public translation of health information.
A noticeable proportion of aware respondents (84%) had regular eye examinations as they declared. Accessing care centers and ophthalmologists does not seem to be a problem; eye care is simply not a high health priority among people. However, they do seek care when symptoms reach a critical stage. This could explain the association between awareness and the severity of diabetes. In this regard, Muecke et al. found that 43% of participants understood they needed to seek eye care in case of a problem with eyesight.[22] Plain language should be used by health workers or through media while informing diabetic participants about their eye care needs, especially for elder participants and ones with lower literacy.
Conclusions
Seventy-three percent of diabetic respondents were unaware of the necessity of regular eye examinations and the average duration of diabetes was nearly 6 years longer in aware subjects. Since DR and DME are complications of diabetes mellitus, any accomplishment in screening and treatment efforts is inevitably tied to diabetes care and control programs in the primary health care system. Therefore, consolidating diabetes care and the referral system can provide proper grounds for further specific actions. Routine follow-ups need organized reminders, and this role is best fitted with primary health-care workers in the referral system although it seems that physicians play the main role to provoke community members.
Financial support and sponsorship
This study was funded by the Iran Research and Technology Office.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
We thank all the staff who helped to complete the Yazd Eye Study and also participants in this study for their valuable contribution. Finally, our acknowledgments go to the Yazd University of Medical Science for field supports.
References
- 1.Gordois A, Cutler H, Pezzullo L, Gordon K, Cruess A, Winyard S, et al. An estimation of the worldwide economic and health burden of visual impairment. Glob Public Health. 2012;7:465–81. doi: 10.1080/17441692.2011.634815. [DOI] [PubMed] [Google Scholar]
- 2.Pascolini D, Mariotti SP. Global estimates of visual impairment: 2010. Br J Ophthalmol. 2012;96:614–8. doi: 10.1136/bjophthalmol-2011-300539. [DOI] [PubMed] [Google Scholar]
- 3.Palagyi A, Ramke J, du Toit R, Brian G. Eye care in Timor-Leste: A population-based study of utilization and barriers. Clin Exp Ophthalmol. 2008;36:47–53. doi: 10.1111/j.1442-9071.2007.01645.x. [DOI] [PubMed] [Google Scholar]
- 4.Chou CF, Barker LE, Crews JE, Primo SA, Zhang X, Elliott AF, et al. Disparities in eye care utilization among the United States adults with visual impairment: Findings from the behavioral risk factor surveillance system 2006-2009. Am J Ophthalmol. 2012;154(6 Suppl):S45–52.e1. doi: 10.1016/j.ajo.2011.09.025. [DOI] [PubMed] [Google Scholar]
- 5.Eye-care utilization among women aged > or=40 years with eye diseases, 19 states, 2006-2008. MMWR Morb Mortal Wkly Rep. 2010. [Last accessed on 2017 Feb 28]. Available from: http://www.cdc.gov/mmwr/preview/mmwrhtml/mm5919a3.htm . [PubMed]
- 6.Fotouhi A, Hashemi H, Mohammad K. Eye care utilization patterns in Tehran population: A population based cross-sectional study. BMC Ophthalmol. 2006;6:4. doi: 10.1186/1471-2415-6-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Javadi MA, Katibeh M, Rafati N, Dehghan MH, Zayeri F, Yaseri M, et al. Prevalence of diabetic retinopathy in Tehran province: A population-based study. BMC Ophthalmol. 2009;9:12. doi: 10.1186/1471-2415-9-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Shaw JE, Sicree RA, Zimmet PZ. Global estimates of the prevalence of diabetes for 2010 and 2030. Diabetes Res Clin Pract. 2010;87:4–14. doi: 10.1016/j.diabres.2009.10.007. [DOI] [PubMed] [Google Scholar]
- 9.Schwandt P. On the occasion of the world diabetes day: Diabetes mellitus - A globally increasing health problem. Int J Prev Med. 2012;3:747–8. [PMC free article] [PubMed] [Google Scholar]
- 10.Klein BE. Overview of epidemiologic studies of diabetic retinopathy. Ophthalmic Epidemiol. 2007;14:179–83. doi: 10.1080/09286580701396720. [DOI] [PubMed] [Google Scholar]
- 11.Romero-Aroca P. Managing diabetic macular edema: The leading cause of diabetes blindness. World J Diabetes. 2011;2:98–104. doi: 10.4239/wjd.v2.i6.98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Haghdoost AA, Rezazadeh-Kermani M, Sadghirad B, Baradaran HR. Prevalence of type 2 diabetes in the Islamic Republic of Iran: Systematic review and meta-analysis. East Mediterr Health J. 2009;15:591–9. [PubMed] [Google Scholar]
- 13.Lotfi MH, Saadati H, Afzali M. Prevalence of diabetes in people aged = 30 years: The results of screen-ing program of Yazd Province, Iran, in 2012. J Res Health Sci. 2014;14:87–91. [PubMed] [Google Scholar]
- 14.Dehghan MH, Katibeh M, Ahmadieh H, Nourinia R, Yaseri M. Prevalence and risk factors for diabetic retinopathy in the 40 to 80 year-old population in Yazd, Iran: The Yazd Eye Study. J Diabetes. 2015;7:139–41. doi: 10.1111/1753-0407.12205. [DOI] [PubMed] [Google Scholar]
- 15.Reasons for not seeking eye care among adults aged >=40 years with moderate to severe visual impairment-21 States, 2006-2009. Morb Mortal Wkly Rep. 2011. [Last accessed on 2017 Feb 28]. Available from: http://www.cdc.gov/mmwr/preview/mmwrhtml/mm6019a3.htm . [PubMed]
- 16.Spurling G, Askew D, Jackson C. Retinopathy – Screening recommendations. Aust Fam Physician. 2009;38:780–3. [PubMed] [Google Scholar]
- 17.Katibeh M, Ziaei H, Pakravan M, Dehghan MH, Ramezani A, Amini H, et al. The Yazd Eye Study-a population-based survey of adults aged 40-80 years: Rationale, study design and baseline population data. Ophthalmic Epidemiol. 2013;20:61–9. doi: 10.3109/09286586.2012.744844. [DOI] [PubMed] [Google Scholar]
- 18.Grading diabetic retinopathy from stereoscopic color fundus photographs – an extension of the modified Airlie House classification. ETDRS report number. Early Treatment Diabetic Retinopathy Study Research Group. Ophthalmology. 1991;98(5 Suppl):786–806. [PubMed] [Google Scholar]
- 19.Fauci A. Harrison's Principles of Internal Medicine. New York: Mcgraw-Hill Publ. Comp; 2008. [Google Scholar]
- 20.Sharifirad G, Hazavehi M, Baghianimoghadam M, Mohebi S. The effect of a health belief model based education program for foot care in diabetic patients Type II in Kermanshah, Iran (2005) Int J Endocrinol Metab. 2007;5:82–90. [Google Scholar]
- 21.Hazavehei M, Khani Jyhouni A, Hasanzadeh A, Rashidi M. The effect of educational program based on BASNEF model on diabetic (Type II) eyes care in Kazemi's Clinic, (Shiraz) Iran J Endocrinol Metab. 2008;10:145–54. [Google Scholar]
- 22.Muecke JS, Newland HS, Ryan P, Ramsay E, Aung M, Myint S, et al. Awareness of diabetic eye disease among general practitioners and diabetic patients in Yangon, Myanmar. Clin Exp Ophthalmol. 2008;36:265–73. doi: 10.1111/j.1442-9071.2008.01724.x. [DOI] [PubMed] [Google Scholar]
- 23.Addoor KR, Bhandary SV, Khanna R, Rao LG, Lingam KD, V S B, et al. Assessment of awareness of diabetic retinopathy among the diabetics attending the peripheral diabetic clinics in Melaka, Malaysia. Med J Malaysia. 2011;66:48–52. [PubMed] [Google Scholar]
- 24.Tapp RJ, Shaw JE, Harper CA, de Courten MP, Balkau B, McCarty DJ, et al. The prevalence of and factors associated with diabetic retinopathy in the Australian population. Diabetes Care. 2003;26:1731–7. doi: 10.2337/diacare.26.6.1731. [DOI] [PubMed] [Google Scholar]
- 25.Schoenfeld ER, Greene JM, Wu SY, Leske MC. Patterns of adherence to diabetes vision care guidelines: Baseline findings from the diabetic retinopathy awareness program. Ophthalmology. 2001;108:563–71. doi: 10.1016/s0161-6420(00)00600-x. [DOI] [PubMed] [Google Scholar]
- 26.Wong TY, Cheung N, Tay WT, Wang JJ, Aung T, Saw SM, et al. Prevalence and risk factors for diabetic retinopathy: The Singapore Malay eye study. Ophthalmology. 2008;115:1869–75. doi: 10.1016/j.ophtha.2008.05.014. [DOI] [PubMed] [Google Scholar]
- 27.Huang OS, Tay WT, Tai ES, Wang JJ, Saw SM, Jeganathan VS, et al. Lack of awareness amongst community patients with diabetes and diabetic retinopathy: The Singapore Malay eye study. Ann Acad Med Singapore. 2009;38:1048–55. [PubMed] [Google Scholar]
- 28.Soto-Pedre E, Hernaez-Ortega MC, Piniés JA. Duration of diabetes and screening coverage for retinopathy among patients with type 2 diabetes. Ophthalmic Epidemiol. 2007;14:76–9. doi: 10.1080/09286580600879032. [DOI] [PubMed] [Google Scholar]
- 29.Huang OS, Zheng Y, Tay WT, Chiang PP, Lamoureux EL, Wong TY. Lack of awareness of common eye conditions in the community. Ophthalmic Epidemiol. 2013;20:52–60. doi: 10.3109/09286586.2012.751429. [DOI] [PubMed] [Google Scholar]
- 30.Saikumar S, Giridhar A, Mahesh G, Elias A, Bhat S. Awareness about eye diseases among diabetic patients: A survey in South India. Community Eye Health. 2007;20:16–7. [PMC free article] [PubMed] [Google Scholar]
- 31.Katibeh M, Ziaei H, Panah E, Moein HR, Hosseini S, Kalantarion M, et al. Knowledge and awareness of age related eye diseases: A population-based survey. J Ophthalmic Vis Res. 2014;9:223–31. [PMC free article] [PubMed] [Google Scholar]


