Abstract
PURPOSE:
The aim of this study is to compare two different methods of analysis of preoperative reference marking for toric intraocular lens (IOL) after marking with an electronic marker.
SETTING/VENUE:
Cataract and IOL Implantation Service, Shroff Eye Centre, New Delhi, India.
PATIENTS AND METHODS:
Fifty-two eyes of thirty patients planned for toric IOL implantation were included in the study. All patients had preoperative marking performed with an electronic preoperative two-step toric IOL reference marker (ASICO AE-2929). Reference marks were placed at 3-and 9-o'clock positions. Marks were analyzed with two systems. First, slit-lamp photographs taken and analyzed using Adobe Photoshop (version 7.0). Second, Tracey iTrace Visual Function Analyzer (version 5.1.1) was used for capturing corneal topograph examination and position of marks noted. Amount of alignment error was calculated.
RESULTS:
Mean absolute rotation error was 2.38 ± 1.78° by Photoshop and 2.87 ± 2.03° by iTrace which was not statistically significant (P = 0.215). Nearly 72.7% of eyes by Photoshop and 61.4% by iTrace had rotation error ≤3° (P = 0.359); and 90.9% of eyes by Photoshop and 81.8% by iTrace had rotation error ≤5° (P = 0.344). No significant difference in absolute amount of rotation between eyes when analyzed by either method.
CONCLUSIONS:
Difference in reference mark positions when analyzed by two systems suggests the presence of varying cyclotorsion at different points of time. Both analysis methods showed an approximately 3° of alignment error, which could contribute to 10% loss of astigmatic correction of toric IOL. This can be further compounded by intra-operative marking errors and final placement of IOL in the bag.
Keywords: Electronic reference marker, iTrace, toric IOL
Introduction
It has been estimated that 15%–29% of patients with cataract have more than 1.5 diopters (D) of preexisting astigmatism.[1,2] Apart from correcting corneal astigmatism with spectacles and contact lenses, treatment options include excimer laser refractive procedures such as photorefractive keratectomy, laser in situ keratomileusis, and laser-assisted subepithelial keratomileusis; astigmatic keratotomy using limbal or corneal relaxing incisions; opposite clear corneal incisions; and toric phakic or pseudophakic intraocular lens (IOL).[3]
In today's modern age, toric IOL and are an integral part of cataract and refractive surgery. Toric IOLs were developed to neutralize preexisting corneal astigmatism in cataract patients.[4] They provide the opportunity to correct preexisting astigmatism, offering patients optimum distance vision without the use of spectacles or contact lenses.[5] Alignment of the toric IOL at the calculated alignment axis is necessary to achieve effective astigmatism correction. Misalignment of the IOL can be caused by inaccurate placement of the IOL, rotation of the IOL, or both.[5] There are various methods to align the toric IOL at the intended axis.[6] However, most methods follow a 3-step procedure. First, the horizontal axis (0–180°) of the eye is marked preoperatively with patient sitting upright to correct for cyclotorsion. This is usually carried out using a reference marker or a slit lamp along with a rotating slit. Next, intra operatively, the desired alignment axis for the toric IOL is marked with an angular graduation instrument. Finally, the toric IOL is implanted and rotated until the IOL markings agree with the alignment marks.[5]
In our series, all patients had preoperative marking of the eye done with an electronic preoperative toric IOL reference marker. The reference marks were analyzed by two different methods using Tracey iTrace Visual Function Analyser, version 5.1.1 (Tracey™ Technologies, Houston, Tx). The amount of alignment error (in degrees) from the horizontal, by both methods was calculated.
The purpose of this study was to compare two different methods of analysis of preoperative reference marking for toric IOL after marking with an electronic marker (e-marker) and also the accuracy of the electronic marker as a means of establishing the reference point for the final alignment of the toric IOL. This was done to achieve an outcome as close as possible to emetropia.
Patients and Methods
Study design and patient population
This prospective study comprised recruitment of 52 eyes of thirty patients presenting to the outpatient department of Shroff Eye Centre, New Delhi from October 2012 to March 2013.
Materials and methods
Fifty-two eyes of thirty patients planned for toric IOL implantation were included in the study. All patients had preoperative marking carried out using electronic two step toric IOL reference marker (ASICO AE-2929) designed by Dr. Akahoshi. Before the marking, the eye is anesthetized with 0.5% proparacaine drops. The patient is seated in the upright position and made to fixate at a distant target.
Electronic toric IOL marker (ASICO AE-2929), two-step reference marker, was used for marking the reference marks for identifying the 3- and 9-o'clock positions on the limbus [Figure 1a]. The electronic head was fitted on the body and the marker was gradually advanced toward the eye whereas the examiner ensured a central green light without any beep was present when the wedges made contact with the limbus [Figure 1b]. The green light ensured that the horizontal wedges of the marker were truly horizontal. An orange light with a slow beep indicated slight tilt and a red light with fast beep indicated severe tilt. A special ultrafine Gentian Violet Pen was used to ink the wedges. The advantage of this marker was that the surgeon could concentrate on patient's eye as green light and audio tone confirmed horizontal axis. Furthermore, pressing the two buttons on the electronic marker simultaneously calibrated the device. All marking procedures were performed by the same observer, AK.
Figure 1.
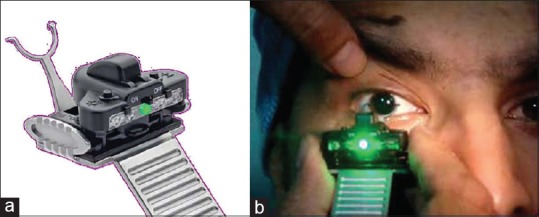
(a) The Electronic Marker (ASICO AE-2929). (b) Being used for preoperative marking
Image analysis
Slit lamp photographs were analyzed using tools in Adobe Photoshop (version 7.0) and were taken by a single masked observer, RD. Amount of alignment error of each eye was calculated. A preoperative photograph with the reference marks was imported in the Adobe Photoshop. Using the “single row marquee tool” a straight line was placed on the image adjacent to the limbal reference marks [Figure 2]. Using the “transform tool,” straight line was rotated in such a manner so as to align through the reference marks on the limbus. The amount of rotation (clockwise or anti-clockwise) was noted from the “set rotation” dialog box. Similarly, iTrace Visual Function Analyzer (Tracey version 5.1.1) was used to analyze the reference marks. A color photograph showing the gentian violet marks on the limbus was captured using iTrace Visual Function Analyzer. The Toric Planner program in the iTrace was used to calculate the amount of alignment error (in degrees) of the gentian violet marks from the horizontal axis of 0° and 180° [Figure 3]. The Toric Planner display is a comprehensive display designed to assist with selection and placement of toric IOL implants. The display utilized data from iTrace wavefront and corneal topography measurements and user-entered data to help the surgeon select the best toric lens power and determine the best axis placement for that lens. The Toric Planner also analyses the exact location of the axis of placement in relation to gentian violet marks which are placed presurgically. The software displayed two arcs, one from 0° to the closest end of the axis of placement, and one from 180° to the opposite end of the axis of placement. The angular measurements initially displayed, provide the location of the axis of placement if the limbal markings were placed exactly at 0° and 180°. The caliper arcs were moved into position by clicking and holding the reference line at 180° between the angular scale and the beginning of the arc and then dragging it to the gentian violet mark. Same step was repeated for the 0° reference mark. The actual position of the marks was read off from the radial scale.
Figure 2.
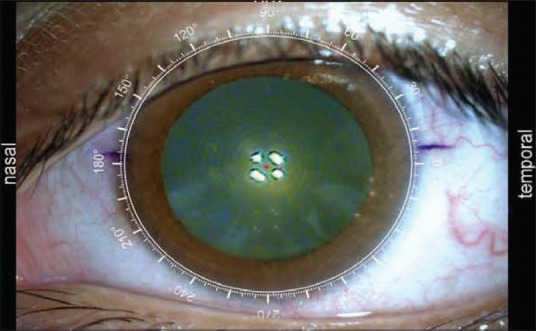
Toric Planner Program in iTrace Visual Function Analyzer (Tracey version 5.1.1)
Figure 3.
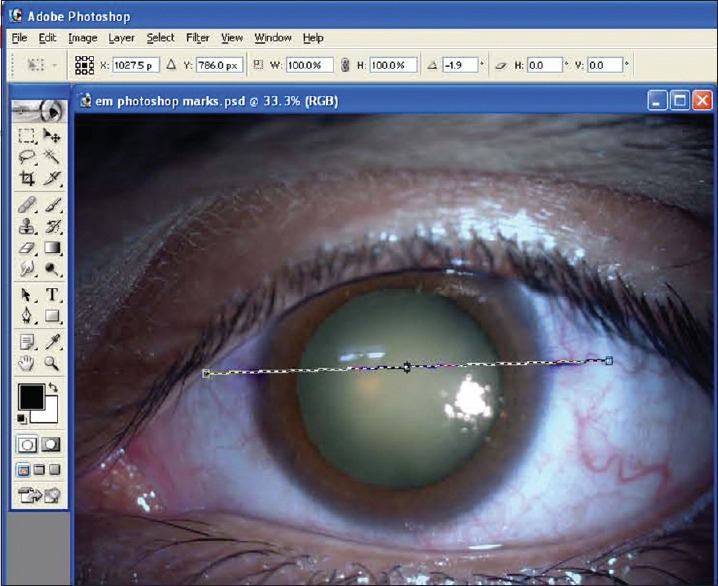
Preoperative photograph with reference marks imported in Adobe Photoshop (Version 7)
Results
The study enrolled 52 eyes of thirty patients. The mean age was 65 years (range from 45 to 80 years). The mean absolute rotation of reference marks in the horizontal axis by iTrace method was 2.44° +1.36° and by Photoshop method was 2.38° ±1.78° (P = 0.193).
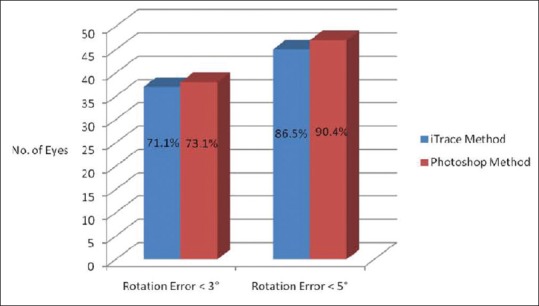
We also analyzed the percentage of eyes showing absolute rotation of reference marks <3° and <5° by both iTrace method and by Photoshop method [Figure 4]. 71.1% (37 eyes) by iTrace method and 73.1% (38 eyes) by Photoshop method showed absolute rotation of reference marks <3° (P = 0.562). Furthermore, an absolute rotation of reference marks <5° was seen in 86.5% (45 eyes) of patients analyzed by iTrace method and 90.4% (47 eyes) of patients analyzed by Photoshop method (P = 0.298).
Figure 4.
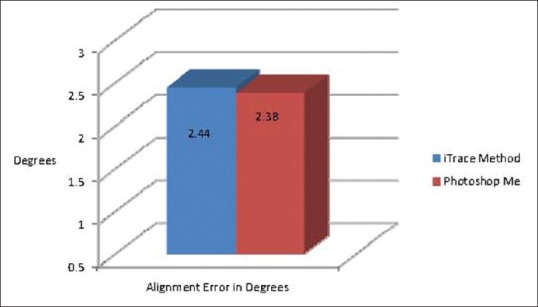
Mean absolute rotation of reference marks in the horizontal axis
Discussion
We performed all our preoperative markings in sitting position to avoid cyclotorsion [Figure 5].
Figure 5.
Eyes showing absolute rotation of reference marks ≤° and <5°
Cyclotorsion of the eye from the upright to supine position is approximately 2–4° on average, but can be up to 15° in individual patients.[7,8,9]
During this study, there was no statistical difference between the two image analyzing techniques and both of them showed that the electronic marker was fairly accurate as evaluated by the two imaging techniques.
Furthermore, there were a few observations that we made. In the electronic toric IOL marker, we found that the device gave both audio and visual confirmation of the correct position of the reference marks without diverting attention from the patient's eye. However, there was no external calibration tool provided to verify horizontal level. Furthermore, third wedge for marking the limbus at 6 o'clock was not present (as in cases of Bubble Markers and Pendulum Markers). In a comparative study done by Popps et al.[10] in Vienna, the pendulum-marking device showed the least rotational deviation to the reference meridian (mean 1.8°). However, they did not use an electronic two step toric IOL reference marker in their study for comparison. Furthermore, to the best of our knowledge, we could not find any other study carried out on Asian eyes where an electronic marker was used for preoperative marking techniques.
In our study, the electronic toric IOL marker showed approximately 3° of alignment error. It can be attributed to the “menace reflex” causing the patient to blink due to an approaching object. It may also be due to spread of the preoperative gentian violet marks.
Conclusions
Accuracy of corneal marking before surgery is critical to achieving good surgical-astigmatism correction outcomes, and electronic toric IOL marker gave good results. Errors in intra-operative marking and final alignment of the IOL in the bag could possibly add on to this error. We believe that slit-lamp based methods are cumbersome to perform and require greater patient co-operation; the YAG laser method requires additional instrumentation. Furthermore, sophisticated methods such as iris fingerprinting and intra-operative wavefront aberrometry, although highly accurate, cannot be routinely incorporated in the average ophthalmologist's practice.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Hoffer KJ. Biometry of 7,500 cataractous eyes. Am J Ophthalmol. 1980;90:360–8. doi: 10.1016/s0002-9394(14)74917-7. [DOI] [PubMed] [Google Scholar]
- 2.Ninn-Pedersen K, Stenevi U, Ehinger B. Cataract patients in a defined Swedish population 1986-1990. II. Preoperative observations. Acta Ophthalmol (Copenh) 1994;72:10–5. doi: 10.1111/j.1755-3768.1994.tb02729.x. [DOI] [PubMed] [Google Scholar]
- 3.Bauer NJ, de Vries NE, Webers CA, Hendrikse F, Nuijts RM. Astigmatism management in cataract surgery with the AcrySof toric intraocular lens. J Cataract Refract Surg. 2008;34:1483–8. doi: 10.1016/j.jcrs.2008.05.031. [DOI] [PubMed] [Google Scholar]
- 4.Shimizu K, Misawa A, Suzuki Y. Toric intraocular lenses: Correcting astigmatism while controlling axis shift. J Cataract Refract Surg. 1994;20:523–6. doi: 10.1016/s0886-3350(13)80232-5. [DOI] [PubMed] [Google Scholar]
- 5.Visser N, Berendschot TT, Bauer NJ, Jurich J, Kersting O, Nuijts RM. Accuracy of toric intraocular lens implantation in cataract and refractive surgery. J Cataract Refract Surg. 2011;37:1394–402. doi: 10.1016/j.jcrs.2011.02.024. [DOI] [PubMed] [Google Scholar]
- 6.Visser N, Ruíz-Mesa R, Pastor F, Bauer NJ, Nuijts RM, Montés-Micó R. Cataract surgery with toric intraocular lens implantation in patients with high corneal astigmatism. J Cataract Refract Surg. 2011;37:1403–10. doi: 10.1016/j.jcrs.2011.03.034. [DOI] [PubMed] [Google Scholar]
- 7.Arba-Mosquera S, Merayo-Lloves J, de Ortueta D. Clinical effects of pure cyclotorsional errors during refractive surgery. Invest Ophthalmol Vis Sci. 2008;49:4828–36. doi: 10.1167/iovs.08-1766. [DOI] [PubMed] [Google Scholar]
- 8.Chernyak DA. Cyclotorsional eye motion occurring between wavefront measurement and refractive surgery. J Cataract Refract Surg. 2004;30:633–8. doi: 10.1016/j.jcrs.2003.08.022. [DOI] [PubMed] [Google Scholar]
- 9.Swami AU, Steinert RF, Osborne WE, White AA. Rotational malposition during laser in situ keratomileusis. Am J Ophthalmol. 2002;133:561–2. doi: 10.1016/s0002-9394(01)01401-5. [DOI] [PubMed] [Google Scholar]
- 10.Popp N, Hirnschall N, Maedel S, Findl O. Evaluation of 4 corneal astigmatic marking methods. J Cataract Refract Surg. 2012;38:2094–9. doi: 10.1016/j.jcrs.2012.07.039. [DOI] [PubMed] [Google Scholar]


