Sir,
Postdural puncture headache (PDPH) is a well-known complication after puncture of the dura mater. The typical localization of the headache is usually frontal and/or occipital. It is described as severe, nonpulsatile, debilitating pain that is increasing on sitting up position while decreasing in the supine position.[1] The conservative treatment of PDPH usually consists of fluid therapy, analgesics, and caffeine. Epidural blood patch (EBP) is gold standard therapy but it is an invasive method that carries the same risks as other epidural procedures, including dural puncture, infection, and neurologic complications.
The sphenopalatine ganglion (SPG) is one in all four tiny parasympathetic ganglia found within the head. Transnasal SPG block (SPGB) has been frequently used to treat chronic conditions such as migraine, cluster headache, and atypical facial pain[2,3] and has also been used with good results in a recent case series to treat acute PDPH.[4] The parasympathetic fibers, from SPG, which innervate the cerebral and meningeal blood vessels cause vasodilation and activation of nociceptor fibers in the meninges which is perceived as referred pain from the head by the sensory cortex.
We report a case of a 42-year-old, 55 kg female patient who underwent total abdominal hysterectomy which was planned under combined spinal-epidural anesthesia. In the operation theater, standard monitors were applied, and intravenous access was secured. After preloading with 500 ml of Ringer lactate, an 18-gauge Tuohy needle was used to place a 20-gauge epidural catheter in L2–L3 intervertebral space. Spinal anesthesia was given in L2–L3 intervertebral space using 25-gauge Quincke needle with 3 ml of 0.5% bupivacaine and 25 mcg dexmedetomidine. Anesthesia of sensory level up to T6 was achieved, and intraoperative period was uneventful.
On the 4th postoperative day, the patient complained of bifrontal, nonpulsatile, and worsened headache when the patient was sitting up. Signs of neurologic cause were not observed. She also did not complain nausea, visual impairment, neck rigidity, or fatigue. Physical examination was normal.
We suspected of PDPH and the patient was treated with nonsteroidal anti-inflammatory drugs (NSAIDs), oral caffeine, hydration, and bed rest; as headache did not subside with conventional treatment, on the 6th postoperative day, bilateral transnasal SPGB was performed. A 5 mL syringe preloaded with 0.5% ropivacaine was attached to cotton-tipped 23-gauge spinal needle, the spinal needle was introduced into the naris and advanced through nasal cavity posteriosuperior to medial turbinate till the resistance encountered, and 1.5 ml of ropivacaine was injected on each side [Figure 1]. Following a single SPGB, the patient experienced instantaneous and sustained pain relief. The patient was discharged from the hospital 24 h later without headache. After 3 weeks, during follow-up visit, she was free of pain.
Figure 1.
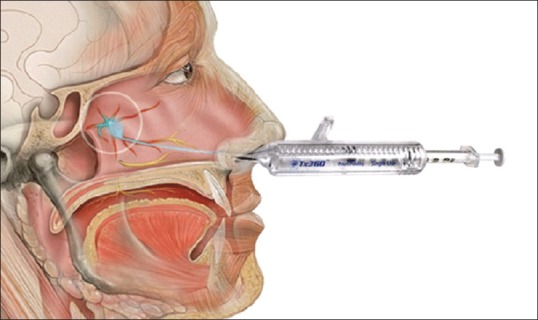
Schematic diagram showing location and procedure of transnasal sphenopalatine ganglion block (image courtesy: TIAN MEDICAL, Illinois, USA)
Leakage of cerebrospinal fluid (CSF) through dural rent results in decreased intracranial pressure. Due to decrease in intracranial pressure and CSF, volume may cause traction on the pain-sensitive intracranial vessels, meninges, and cranial nerves.[5] The conservative treatment of PDPH consists of bed rest, NSAIDs, caffeine, and hydration. Sprigge, and Harper concluded that bed rest and analgesics did not give effective pain relief for more than 14% of patients suffered from PDPH.[5]
The most effective treatment for PDPH is (EBP) Epidural Blood Patch, which involves the injection of autologous blood into the epidural space. EBP is an invasive method and has many side effects. It may cause back pain, radiculopathy, bradycardia, inadvertent dural puncture, and rarely meningitis.[6]
SPGB is minimally invasive and carried out at the bedside without using imaging and has apparently rapid onset than EBP with better safety profile. Despite obvious contraindication in patients with basilar skull fractures, SPGB can be done in cases where EBP Epidural Blood Patch is contraindicated. In addition, being a noninvasive technique, it can be given in the case of infection anywhere else than the nasopharynx.[4]
In conclusion, we suggest that patients presenting with PDPH should be considered primarily for SPGB due to safety of the procedure, immediate and sustained pain relief. Patients may have a rescue EBP if necessary.
Financial support and sponsorship
This study was financially supported by Maax Super Speciality Hospital, Shimoga, Karnataka, India.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Turnbull DK, Shepherd DB. Post-dural puncture headache: Pathogenesis, prevention and treatment. Br J Anaesth. 2003;91:718–29. doi: 10.1093/bja/aeg231. [DOI] [PubMed] [Google Scholar]
- 2.Láinez MJ, Puche M, Garcia A, Gascón F. Sphenopalatine ganglion stimulation for the treatment of cluster headache. Ther Adv Neurol Disord. 2014;7:162–8. doi: 10.1177/1756285613510961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Narouze S. Neurostimulation at pterygopalatine fossa for cluster headaches and cerebrovascular disorders. Curr Pain Headache Rep. 2014;18:432. doi: 10.1007/s11916-014-0432-5. [DOI] [PubMed] [Google Scholar]
- 4.Kent S, Mehaffey G. Transnasal sphenopalatine ganglion block for the treatment of postdural puncture headache in obstetric patients. J Clin Anesth. 2016;34:194–6. doi: 10.1016/j.jclinane.2016.04.009. [DOI] [PubMed] [Google Scholar]
- 5.Sprigge JS, Harper SJ. Accidental dural puncture and post dural puncture headache in obstetric anaesthesia: Presentation and management: A 23-year survey in a district general hospital. Anaesthesia. 2008;63:36–43. doi: 10.1111/j.1365-2044.2007.05285.x. [DOI] [PubMed] [Google Scholar]
- 6.Oh J, Camann W. Severe, acute meningeal irritative reaction after epidural blood patch. Anesth Analg. 1998;87:1139–40. [PubMed] [Google Scholar]


