Abstract
Objective
Akathisia is a neuropsychiatric syndrome characterized by subjective and objective restlessness. It is a common side effect in patients taking antipsychotics and other psychotropics. Patients with delirium are frequently treated with antipsychotic medications that are well known to induce akathisia as a side effect. However, the prevalence, phenomenology, and management of akathisia in patients with delirium remain largely unknown. The purpose of this review was to examine the medical literature in order to establish the current state of knowledge regarding the prevalence of antipsychotic-induced akathisia in patients with delirium.
Method
A systematic review of the literature was conducted using the EMBASE, MEDLINE, PsycINFO, and CINAHL databases. Some 10 studies addressing the incidence of akathisia in patients taking antipsychotic medication for delirium were identified and included in our review.
Results
The included studies reported a variable prevalence of antipsychotic-induced akathisia. A higher prevalence was found in patients taking haloperidol. Among atypical antipsychotics, paliperidone and ziprasidone were associated with a higher risk of akathisia. The risk for akathisia appeared to be a dose-related phenomenon.
Significance of results
Studies using specific scales for evaluation of akathisia in delirium are lacking. Some populations, such as patients with cancer or terminally ill patients in palliative care settings taking antipsychotics for the treatment of delirium, could be at higher risk for development of akathisia as a side effect.
Keywords: Akathisia, Delirium, Antipsychotics
BACKGROUND
Akathisia
Akathisia (from the Greek καθῑζειν: inability to sit) is a neuropsychiatric syndrome consisting of a combination of subjective and objective psychomotor restlessness. Akathisia was first described by Czech physician Ladislav Haskovec, who, after graduating from medical school at Charles University in Prague, won a scholarship to study at La Salpêtrière in Paris with renowned neurologist Jean Martin Charcot. Together they presented two patients with akathisia at the Paris Neurological Society in 1901 (Berrios, 1995). Though these patients were thought to suffer from a neurotic form of akathisia, the term akathisia is nowadays usually employed to refer to the side effects induced by such medications as antipsychotics.
Clinically, akathisia syndrome implies a wide range of subjective and objective symptoms. Subjectively, akathisia may present with an inner restlessness that involves mainly the legs but can also involve the arms or trunk, a compulsion to move, dysphoria, anxiety, inner tension, and other less common symptoms such as rage, fear, nausea, or worsening of psychotic symptoms. Objectively, akathisia may present with fidgetiness of the hands, arms, and limbs, complex repetitive movements, persistent swinging and crossing and uncrossing of the legs, moving from foot to foot, walking, and pacing (Sachdev & Loneragan, 1991; Sachdev, 1995).
The DSM–V establishes a distinction between medication-induced akathisia and tardive akathisia. In the former, the individual has subjective complaints of restlessness, often accompanied by excessive movements, developed within a few weeks of starting or raising the dosage of a medication or after reducing the dosage of a medication used to treat extrapyramidal symptoms. In contrast, tardive akathisia is classified together with tardive dystonia under tardive syndrome. According to the DSM–V, tardive syndrome is distinguished by the late emergence of movement disorders such as akathisia or dystonia in the course of treatment and their potential persistence for months to years, even in the face of antipsychotic discontinuation or dosage reduction (APA, 2013).
Several hypotheses have been postulated to explain the pathophysiology of akathisia. Initially, a postsynaptic dopamine blockade was proposed, in part due to the fact that dopamine-blocking agents and lesions in the ventral tegmental area could result in akathisia. Acetylcholine, GABA, and norepinephrine have also been proposed to play a role in the pathogenesis of akathisia based on observations that the use of anticholinergics, benzodiazepines and beta blockers may alleviate symptoms of akathisia (Sachdev & Loneragan, 1991; Sachdev, 1995). Recently, Loonen and Stahl (2011) proposed a new model for medication-induced akathisia, one that emphasizes the role of the nucleus accumbens (part of the ventral striatum) in the pathogenesis of akathisia. According to this model, the shell of the nucleus accumbens plays a role in promoting unconditioned defensive behavior. Antipsychotics decrease activity in the ventral striatum, resulting in a compensatory enhancement of activity in the locus coeruleus. The locus coeruleus selectively stimulates the shell portion of the nucleus accumbens. This results in overstimulation of the shell when compared to the core of the nucleus accumbens. Relative over-stimulation of the shell of nucleus accumbens results in the typical urge to display curious or defensive behavior accompanied by dysphoric feelings. This model provides an explanation for relief of akathisia with beta blockers, which block norepinephrine-firing neurons in the locus coeruleus (Loonen & Stahl, 2011). In addition, certain genetic polymorphisms have been associated with an increased likelihood for development of akathisia (Jung et al., 2014). Furthermore, Kim and colleagues (2011) published a study in which patients using antipsychotics matched with a control group completed high-resolution positron emission tomography (PET) with [11C]raclopride. A positive correlation was demonstrated between higher scores on the Liverpool University Neuroleptic Side Effects Scale and D2/D3 receptor occupancy in the ventral striatum (nucleus accumbens and olfactory tubercle) among patients using antipsychotics. This study further supports the hypothesis that akathisia stems from a central nervous system pathology (Kim et al., 2011).
Clinical evaluation is essential in detection of akathisia. Nevertheless, several validated scales are available for diagnosis and assessment of the severity of akathisia: the Barnes Akathisia Rating Scale (Barnes & Braude, 1985), the Hillside Akathisia Scale (Fleischhacker et al., 1991), and the Prince Henry Akathisia Scale (Sachdev, 1994). The Barnes Akathisia Rating Scale (BAS) is the most commonly used assessment tool in clinical practice (Barnes & Braude, 1985).
Antipsychotics
Antipsychotics are thought to be the most common cause of akathisia in clinical settings. While akathisia occurs more frequently with the use of high-potency first-generation antipsychotics (such as haloperidol and fluphenazine) (Sachdev & Loneragan, 1991; Sachdev, 1995; Ossowska, 2002), the prevalence of akathisia with intermediate (e.g., perphenazine) and low-potency (e.g., chlorpromazine) first-generation antipsychotics is not necessarily higher than that seen with second-generation antipsychotics (e.g., quetiapine and olanzapine) (Lieberman & Stroup, 2011). In fact, recent studies propose a higher prevalence with certain second-generation antipsychotics such as ziprasidone, asenapine, and aripiprazole (Frazier et al., 2007; Kumar & Sachdev, 2009). Even clozapine, despite having a different mechanism of action, has been associated with akathisia (Gogtay & Rapoport, 2008). The SSRIs have also been associated with akathisia. Enhancement of serotonergic activity has been postulated to result in a decrease in dopamine and subsequent akathisia. Buspirone can also cause akathisia through a decrease in dopamine via blockade of calcium channels (Sachdev, 1995; Sachdev & Loneragan, 1991; Kumar & Sachdev, 2009).
Delirium
Delirium is a condition characterized by an abrupt disturbance of arousal, awareness, attention, and cognition that fluctuates during the course of the day. The etiology of delirium is typically multifactorial and may include drugs, metabolic abnormalities, infections, trauma, and withdrawal. Pathophysiologically, dysfunction of a final pathway involving the prefrontal cortex, the posterior parietal cortex, and the anteromedial thalamus has been proposed. Not only is delirium a prevalent syndrome in medically ill hospitalized patients, it is also a frequent problem encountered in palliative care settings. In the assessment and treatment of delirium, guidelines recommend addressing the underlying causes, implementing nonpharmacological interventions, and, often, the use of antipsychotic medications (Breitbart & Alici, 2012). Though several agents have been tried for treatment of delirium, antipsychotics remain the gold standard. Such antipsychotics include haloperidol, chlorpromazine, olanzapine, quetiapine, risperidone, and aripiprazole (Breitbart et al., 1996; Friedman et al., 2014; Gilchrist et al., 2012; Hatta et al., 2014; Jung Jin et al., 2009; Kim et al., 2008; Lonergan et al., 2007; Page et al., 2013; Yoo et al., 2011). Haloperidol, the most widely studied agent for the treatment of delirium, is a high-potency antipsychotic agent associated with akathisia and other extrapyramidal symptoms when used in patients with schizophrenia or other psychotic disorders.
Study Objective
The incidence of extrapyramidal symptoms associated with the use of haloperidol or other antipsychotics in patients with delirium has not been vigorously studied. Most studies exploring the efficacy of antipsychotics for the treatment of delirium employ general extrapyramidal symptom scales (such as the Simpson Angus Scale and the Udvalg Kliniske Undersogelser Side Effect Rating Scale) for assessment of extrapyramidal symptoms related to antipsychotic use, but specific assessment scales for akathisia are largely lacking (Breitbart et al., 1996; Friedman et al., 2014; Lonergan et al., 2007). Our objective in this review was to identify any existing literature in which patients taking antipsychotics for delirium were assessed for akathisia in order to establish the prevalence of akathisia and explore the extent to which assessment tools have been used for evaluation of akathisia.
METHODS
A systematic review of the literature was conducted to identify clinical studies that reported on akathisia as a side effect in patients with delirium who were treated with antipsychotics. Included were studies that reported on akathisia symptoms diagnosed using an established scale/tool or via clinical evaluation. The search strategy was carried out (February 2015) by a librarian searching four databases: EM-BASE (Elsevier, 1966; February 2015), MEDLINE (OVID, 1946; February 2015), PsycINFO (OVID, 1806; February 2015), and CINAHL (EBSCO, 1981; February 2015).
In each of these four databases, three main concepts (akathisia, delirium, and antipsychotics) were searched (using keywords and the controlled terms available for each concept) and then combined (with the Boolean operator AND). The search for the antipsychotics concept was further expanded by including search terms for the names of antipsychotic medications used clinically in the treatment of delirium: haloperidol, chlorpromazine, olanzapine, risperidone, quetiapine, ziprasidone, and aripiprazole (Breitbart & Alici, 2012). All the antipsychotic-related concepts were then combined as synonyms (using the Boolean operator OR). No age, date, or language restrictions were applied to the search. Furthermore, the bibliographies of relevant articles, especially comprehensive reviews looking at antipsychotic usage in the treatment of delirium and the side effects/safety of antipsychotics, were examined in order to identify additional studies that reported on akathisia as a side effect.
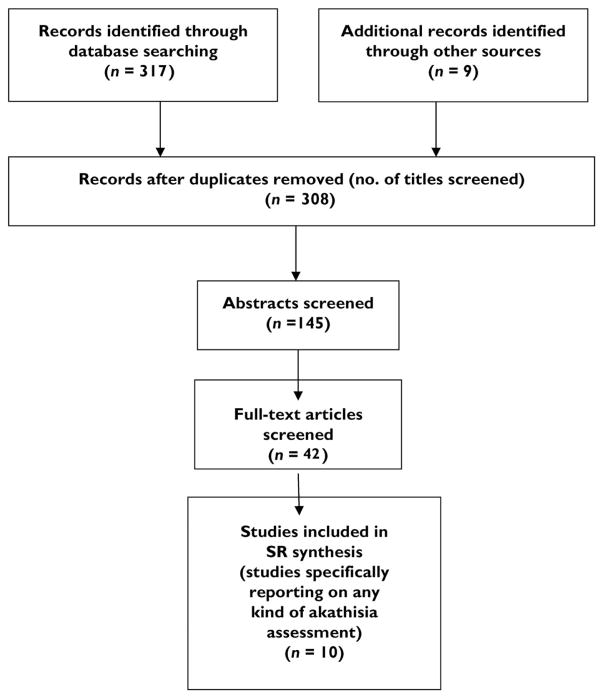
The database searches resulted in retrieval of 317 citations (Figure 1). Endnote (Thompson Reuters) bibliographic citation management software was utilized to manage the citations and remove duplicate records, resulting in 299 unique citations. Some 9 additional citations identified from reference lists yielded a final set of 308 records whose titles were reviewed. Of these, 145 citations were deemed potentially relevant, and their abstracts were read. Abstracts explicitly indicating that akathisia was assessed were included, as well as studies evaluating drug therapies for delirium that could potentially be reporting on extrapyramidal side effects. The full-text documents of 42 of these records were obtained and reviewed, with particular attention paid to the tables and figures in the publications. A final set of 10 articles were included in this systematic review synthesis, as they met the criteria of reporting akathisia as a side effect of treating delirium with antipsychotics. Study design details and information about drug/dosage administered and the number and percentage of patients diagnosed with akathisia side effects were then extracted from the 10 studies (summarized in Table 1).
Fig. 1.
Search process for identification of relevant studies.
Table 1.
Studies reporting on akathisia as a side effect of antipsychotics in patients treated for delirium
| Reference | Design | Dose | Akathisia |
|---|---|---|---|
| Menza et al. (1988) | Prospective study of 14 patients on haloperidol and benzodiazepine vs 4 patients on haloperidol alone | 4 mg of haloperidol in both groups and at least 1 mg of benzodiazepine in the combined group | 2 patients in the haloperidol-only group developed akathisia (14%) |
| Fernandez & Levy (1993) | Case report of 3 patients treated with molindone for HIV delirium and one patient with perphenazine | 1 patient on molindone 60 mg daily, 1 patient on perphenazine, unknown dose, 1 patient on 1 mg of haloperidol as needed q 6 hours was switched to molindone 70 mg daily on average | Out of the 3 patients, 1 had akathisia on perhenazine; none on molindone developed akathisia |
| Han & Kim (2004) | Double-blind trial of risperidone and haloperidol in 24 patients with delirium | Risperidone at 1.02 mg daily and haloperidol at 1.71 mg daily | 1 patient (8%) in the haloperidol group developed akathisia |
| Miyaji et al. (2007) | Retrospective study comparing the risk of adverse effects between 6 patients with delirium on risperidone vs. 29 patients with delirium on oral haloperidol and 20 patients with delirium on i.m. haloperidol | Risperidone 0.75 mg daily, oral haloperidol 1.25 mg daily, and i.m. haloperidol 5 mg daily | Risperidone group 0 patients (0%), oral haloperidol group 1 patient (3%), i.m. haloperidol group 2 patients (10%) |
| Takeuchi et al. (2007) | Open-label trial of 38 patients on perospirone for treatment of delirium | Perospirone at 6.5 mg daily | 1 patient (3%) developed akathisia |
| Kim et al. (2010) | 17 patients on risperidone vs. 15 patients on olanzapine for treatment of delirium | Risperidone 0.9 mg daily and olanzapine 2.4 mg daily | 2 patients (13%) in the olanzapine group developed akathisia |
| Girard et al. (2010) | Randomized placebo-controlled trial of 35 patients on haloperidol vs. 30 patients on ziprasidone vs. 36 patients on placebo for treatment of delirium | Haloperidol 15 mg daily, ziprasidone 111.3 mg daily | 7 patients (28.5%) in the haloperidol group, 6 patients (20%) in the ziprasidone group, and 7 patients (19%) in the placebo group developed akathisia |
| Yoon et al. (2011) | Open-label prospective trial of paliperidone in 15 patients with delirium | Paliperidone 3 to 6 mg a day | 2 patients developed akathisia on paliperidone at 6 mg a day |
| Crawford et al. (2013) | Prospective cohort stady in 119 patients taking haloperidol for delirium | Haloperidol 2.1 mg daily | 13 patients (11%) on haloperidol developed akathisia |
| Maneeton et al. (2013) | A double-blind, randomized controlled trial of 24 patients on quetiapine vs. 28 patients on haloperidol for treatment of delirium | Quetiapine 62.5 mg daily and haloperidol 1.25 mg daily | 0 patients (0%) on quetiapine developed akathisia, 1 patient (3.6%) on haloperidol developed akathisia |
RESULTS
Variable Prevalence of Antipsychotic Induced Akathisia
One of the first studies to explore the prevalence of akathisia in patients with delirium was done by Menza and colleagues (1988) at Massachusetts General Hospital. In a prospective study with 14 patients who had delirium, they used i.v. haloperidol in combination with benzodiazepines and compared those patients with 4 patients who received haloperidol alone. While no patients on benzodiazepines developed akathisia, two of four patients in the haloperidol group did develop akathisia. The authors concluded that benzodiazepines can be helpful in prevention of haloperidol-induced akathisia (Menza et al., 1988). In 1993, Fernandez and Levy reported three cases in which molindone was used for delirious patients with HIV. One of the three developed akathisia after treatment with perphenazine. Akathisia symptoms remitted after substitution of molindone with perphenazine (Fernandez & Levy, 1993).
In a double-blind trial of risperidone and haloperidol in 24 patients with delirium, Han and Kim (2004) reported 1 patient in the haloperidol group who had mild symptoms of akathisia. Another retrospective study comparing the risk of adverse effects between risperidone and haloperidol in delirium found that, while no patients on risperidone developed symptoms of akathisia, 1 of 29 taking oral haloperidol and 2 of 20 patients taking i.m. haloperidol developed clinical akathisia (Miyaji et al., 2007). In a Japanese study, Takeuchi and colleagues (2007) examined the efficacy of perospirone, an atypical antipsychotic with potent serotonin 5HT2 and dopamine D2 antagonist activity at an average dose of 8 mg/daily for treatment of delirium. Of the 38 patients who participated in their study, 1 developed akathisia (Takeuchi et al., 2007). In a seven-day randomized, comparative clinical trial of risperidone versus olanzapine for the treatment of delirium, Kim et al. (2010) reported 1 patient who developed symptoms of akathisia among the 16 who took olanzapine at a mean dose between 1.25 to 2.5 mg/daily. None of the 17 patients who took risperidone developed akathisia (Kim et al., 2010).
The MIND randomized placebo-controlled trial on the feasibility, efficacy, and safety of antipsychotics for ICU delirium reported akathisia in 10 of 35 patients in the haloperidol group at 15 mg daily mg daily, 6 of 30 in the ziprasidone group at 113.3 mg daily, and 7 of 36 in the placebo group (Girard et al., 2010). In a Korean prospective open-label pilot trial exploring the use of paliperidone in the treatment of delirium, Kim et al. (2011) reported 2 of 15 patients who developed akathisia at an average dose of 6 mg/daily. The akathisia symptoms of the two patients who developed akathisia were alleviated with the addition of a beta blocker (Kim et al., 2011).
More recently, a prospective cohort study following 119 patients who took haloperidol at an average dose of 2.1 mg every 24 hours in hospice and palliative care settings in Australia reported 13 patients (11 % of the total sample) who developed symptoms of akathisia (Crawford et al., 2013). Last, a double-blind randomized controlled trial comparing quetiapine versus haloperidol in the treatment of delirium found that, while no patients from the sample of 24 patients who took quetiapine at 67.6 mg daily developed akathisia, 1 of 28 in the haloperidol group developed akathisia at a dose of 0.8 mg daily (Maneeton et al., 2013).
In summary, in the studies we have reviewed, there is a wide variability of antipsychotic-induced akathisia, ranging from 0 to 28.5, among patients with delirium.
Higher Akathisia Prevalence with Certain Drugs
Among all the studies we have found, the highest rates of akathisia were found in a study that evaluated the efficacy of haloperidol and ziprasidone in patients with delirium in an ICU and in palliative care settings. The two studies also included the largest patient samples of all the papers we included in our review (Crawford et al., 2013; Girard et al., 2010). Among the drugs used to treat delirium, haloperidol, the gold standard treatment for this condition, might nevertheless be the antipsychotic with the highest risk for development of akathisia. Therefore, clinicians should consider alternative drugs in delirious patients with a history of akathisia. Moreover, our findings are consistent with the known fact that, within the atypical antipsychotics, ziprasi-done and paliperidone are associated with a higher risk and quetiapine is associated with the lowest risk for development of akathisia as a side effect in studies conducted among patients with schizophrenia (Kumar & Sachdev, 2009; Lieberman & Stroup, 2011).
Dose-Related Risk
The risk for akathisia in patients with delirium taking antipsychotics appears to be a dose-related phenomenon according to the results of the selected studies in this review. For instance, the two patients that developed akathisia on paliperidone were receiving the highest dose administered in that sample (Yoon et al., 2011). In addition, Miyaji et al. (2007) report a higher prevalence of akathisia in patients taking 5 mg of i.m. haloperidol versus patients taking an average dose of 1.2 mg of oral haloperidol. Furthermore, Girard et al. (2010) found the highest prevalence of akathisia among all the studies included in our review, using an average dose of 15 mg of haloperidol daily.
CHALLENGES, LIMITATIONS, AND FUTURE DIRECTIONS
In our search of the literature, we found 10 studies reporting antipsychotic-induced akathisia as a side effect when used for treatment of delirium. These studies have relied on clinical evaluation for assessment of akathisia rather than using specific scales in patients taking antipsychotics for delirium. In contrast, a Dutch study that utilized the Barnes Akathisia Rating Scale (BAS) for assessment of side effects in the use of haloperidol prophylaxis for delirium in an older population did not find a difference in akathisia incidence between haloperidol and placebo (Kalisvaart et al., 2005). Clinically, the symptoms of delirium and psychomotor symptoms associated with pain, distress, anxiety, and discomfort may also resemble those of akathisia. As such, the lack of use of an assessment tool represents a limitation of the studies included herein.
Furthermore, akathisia symptoms might overlap with the characteristic restlessness in dying patients with delirium during the last days of life—a term often referred to as “terminal restlessness.” That could explain why Crawford and colleagues (2013) found a relatively high prevalence of akathisia (11%) in hospice and palliative care settings among delirious patients on a relatively average dose of haloperidol: 2.1 mg daily. However, it is important to note that most of the studies included in our review reporting a relatively smaller akathisia incidence used haloperidol lower than 2 mg daily for treatment of delirium (Crawford et al., 2013; Girard et al., 2010; Han & Kim, 2004; Maneeton et al., 2013; Miyaji et al., 2007).
As previously stated, most of the delirium intervention studies to date have focused on detection of Parkinsonism due to antipsychotics as an extrapyramidal side effect, not on akathisia. Therefore, antipsychotic-induced akathisia among delirious patients treated with antipsychotics could be underre-ported in the literature. Assessment of akathisia is challenging among patients with delirium. For instance, patients with delirium usually present with cognitive impairment. Therefore, they may fail to report an inner feeling of restlessness despite presenting with objective signs of akathisia. In addition, delirium usually presents with concomitant anxiety symptoms and agitation. These symptoms may be difficult to differentiate from akathisia. In addition, antipsychotic-induced akathisia can be difficult to differentiate from terminal delirium, what is referred to as “terminal restlessness” in the literature, a significant source of caregiver distress (White et al., 2007; Wada et al., 2011). Some patients with delirium and a history of antipsychotic use could have chronic akathisia or akathisia at baseline. For example, Pintor and colleagues found a 7.5% prevalence of akathisia in patients at baseline prior to administration of amisulpride for the treatment of delirium (Pintor et al., 2009).
A Japanese study published in Palliative & Supportive Care in 2007 found an unexpectedly high prevalence of akathisia in 483 patients with cancer who met the criteria for different psychiatric diagnoses. Among these patients, 67 (13.9% of the total sample) had delirium (Kawanishi et al., 2007). Though the authors did not report the doses of medications used for the treatment of delirium or the incidence of akathisia among the delirium subgroup of patients, it seems that some populations (e.g., patients with cancer or patients in palliative and hospice care settings) could be particularly sensitive to development of akathisia.
One of our future research projects will involve the study of the prevalence of akathisia using the Barnes Akathisia Rating Scale (BAS) among cancer patients taking antipsychotics.
CONCLUSION
The recognition, assessment, and management of medication-induced akathisia is essential in providing high-quality clinical care to medically ill patients with delirium. Assessment scales that can help differentiate between akathisia and delirium phenomenology are needed to better identify akathisia in this patient population. These instruments ought to be used in clinical studies aimed at determining the incidence and prevalence of akathisia among delirium patients treated with antipsychotics. As medications used to alleviate akathisia symptoms such as anticholinergics and benzodiazepines could potentially worsen delirium, management of akathisia among delirious patients on antipsychotics should be further studied to explore the efficacy of other agents.
References
- American Psychiatric Association (APA) Diagnostic and statistical manual of mental disorders. 5. Arlington, VA: American Psychiatric Publishing; 2013. [DSM–V] [Google Scholar]
- Barnes T, Braude W. Akathisia variants and tardive dyskinesia. Archives of General Psychiatry. 1985;42(9):874–878. doi: 10.1001/archpsyc.1985.01790320042006. [DOI] [PubMed] [Google Scholar]
- Berrios GE. Lad Haskovec and akathisia. History of Psychiatry. 1995;6(22 Pt 2):243–251. doi: 10.1177/0957154X9500602208. [DOI] [PubMed] [Google Scholar]
- Breitbart W, Alici Y. Evidence-based treatment of delirium in patients with cancer. Journal of Clinical Oncology. 2012;30(11):1206–1214. doi: 10.1200/JCO.2011.39.8784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Breitbart W, Marotta R, Platt MM, et al. A double-blind trial of haloperidol, chlorpromazine, and lorazepam in the treatment of delirium in hospitalized AIDS patients. The American Journal of Psychiatry. 1996;153(2):231–237. doi: 10.1176/ajp.153.2.231. [DOI] [PubMed] [Google Scholar]
- Crawford GB, Meera Agar M, Quinn SJ, et al. Pharmaco-vigilance in hospice/palliative care: Net effect of haloperidol for delirium. Journal of Palliative Medicine. 2013;16(11):1335–1341. doi: 10.1089/jpm.2013.0230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fernandez F, Levy JK. The use of molindone in the treatment of psychotic and delirious patients infected with the human immunodeficiency virus: Case reports. General Hospital Psychiatry. 1993;15(1):31–35. doi: 10.1016/0163-8343(93)90088-6. [DOI] [PubMed] [Google Scholar]
- Fleischhacker WW, Miller CH, Schett P, et al. The Hillside Akathisia Scale: A reliability comparison of the English and German versions. Psychopharmacology. 1991;105(1):141–144. doi: 10.1007/BF02316879. [DOI] [PubMed] [Google Scholar]
- Frazier JA, McClellan J, Findling RL, et al. Treatment of early-onset schizophrenia spectrum disorders (TEOSS): Demographic and clinical characteristics. Journal of the American Academy of Child and Adolescent Psychiatry. 2007;46(8):979–988. doi: 10.1097/chi.0b013e31807083fd. [DOI] [PubMed] [Google Scholar]
- Friedman JI, Soleimani L, McGonigle DP, et al. Pharmacological treatments of non-substance-withdrawal delirium: A systematic review of prospective trials. The American Journal of Psychiatry. 2014;171(2):151–159. doi: 10.1176/appi.ajp.2013.13040458. [DOI] [PubMed] [Google Scholar]
- Gogtay N, Rapoport J. Clozapine use in children and adolescents. Expert Opinion on Pharmacotherapy. 2008;9(3):459–465. doi: 10.1517/14656566.9.3.459. [DOI] [PubMed] [Google Scholar]
- Gilchrist NA, Asoh I, Greenberg B. Atypical antipsychotics for the treatment of ICU delirium. Journal of Intensive Care Medicine. 2012;27(6):354–361. doi: 10.1177/0885066611403110. [DOI] [PubMed] [Google Scholar]
- Girard TD, Pandharipande PP, Carson SS, et al. Feasibility, efficacy, and safety of antipsychotics for intensive care unit delirium: The MIND randomized, placebo-controlled trial. Critical Care Medicine. 2010;38(2):428–437. doi: 10.1097/ccm.0b013e3181c58715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Han CS, Kim YK. A double-blind trial of risper-idone and haloperidol for the treatment of delirium. Psychosomatics. 2004;45(4):297–301. doi: 10.1016/S0033-3182(04)70170-X. [DOI] [PubMed] [Google Scholar]
- Hatta K, Kishi Y, Wada K, et al. Antipsychotics for delirium in the general hospital setting in 2453 consecutive inpatients: A prospective observational study. International Journal of Geriatric Psychiatry. 2014;29(3):253–262. doi: 10.1002/gps.3999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jung Jin K, Hyun Kook L, Chi Un P, et al. Comparison of intramuscular olanzapine and haloperidol for the treatment of delirium. European Psychiatry. 2009;24:S1006. [Google Scholar]
- Jung JS, Lee HJ, Cho CH, et al. Association between restless legs syndrome and CLOCK and NPAS2 gene polymorphism in schizophrenia. Chronobiology International. 2014;31(7):838–844. doi: 10.3109/07420528.2014.914034. [DOI] [PubMed] [Google Scholar]
- Kalisvaart KJ, de Jonghe JF, Bogaards MJ, et al. Haloperidol prophylaxis for elderly hip-surgery patients at risk for delirium: A randomized placebo-controlled study. Journal of the American Geriatrics Society. 2005;53(10):1658–1666. doi: 10.1111/j.1532-5415.2005.53503.x. [DOI] [PubMed] [Google Scholar]
- Kawanishi C, Onishi H, Kato D, et al. Unexpectedly high prevalence of akathisia in cancer patients. Palliative & Supportive Care. 2007;5(4):351–354. doi: 10.1017/s1478951507000545. [DOI] [PubMed] [Google Scholar]
- Kim JH, Kim YB, Lee SY, et al. Antipsychotic-associated mental side effects and their relationship to dopamine D2 receptor occupancy in striatal subdivisions: A high-resolution PET study with [11C]raclopride. Journal of Clinical Psychopharmacology. 2011;31(4):507–511. doi: 10.1097/JCP.0b013e318222353a. [DOI] [PubMed] [Google Scholar]
- Kim JJ, Lim HK, Pae CU, et al. Comparison of intramuscular olanzapine and haloperidol for the treatment of delirium. European Neuropsychopharmacology. 2008;18(S4):S424–S425. [Google Scholar]
- Kim SW, Yoo JA, Lee SY, et al. Risperidone versus olanzapine for the treatment of delirium. Human Psychopharmacology. 2010;25(4):298–302. doi: 10.1002/hup.1117. [DOI] [PubMed] [Google Scholar]
- Kumar R, Sachdev P. Akathisia and second-generation antipsychotic drugs. Current Opinion in Psychiatry. 2009;22(3):293–299. doi: 10.1097/yco.0b013e32832a16da. [DOI] [PubMed] [Google Scholar]
- Lieberman JA, Stroup TS. The NIMH–CATIE schizophrenia study: What did we learn? The American Journal of Psychiatry. 2011;168(8):770–775. doi: 10.1176/appi.ajp.2011.11010039. [DOI] [PubMed] [Google Scholar]
- Lonergan E, Britton AM, Luxenberg J. Antipsychotics for delirium. The Cochrane Database of Systematic Reviews. 2007;(2):CD005594. doi: 10.1002/14651858.CD005594.pub2. [DOI] [PubMed] [Google Scholar]
- Loonen AJM, Stahl SM. The mechanism of drug-induced akathisia. CNS Spectrums. 2011;16(1):7–10. [PubMed] [Google Scholar]
- Maneeton B, Maneeton N, Srisurapanont M, et al. Quetiapine versus haloperidol in the treatment of delirium: A double-blind, randomized, controlled trial. Drug Design, Development and Therapy. 2013;7:657–667. doi: 10.2147/DDDT.S45575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Menza MA, Murray GB, Holmes VF, et al. Controlled study of extrapyramidal reactions in the management of delirious, medically ill patients: Intravenous haloperidol versus intravenous haloperidol plus benzodiazepines. Heart & Lung. 1988;17(3):238–241. [PubMed] [Google Scholar]
- Miyaji S, Yamamoto K, Hoshino S, et al. Comparison of the risk of adverse events between risperidone and haloperidol in delirium patients. Psychiatry and Clinical Neurosciences. 2007;61(3):275–282. doi: 10.1111/j.1440-1819.2007.01655.x. [DOI] [PubMed] [Google Scholar]
- Ossowska K. Neuronal basis of neuroleptic-induced extrapyramidal side effects. Polish Journal of Pharmacology. 2002;54(4):299–312. [PubMed] [Google Scholar]
- Page VJ, Ely EW, Gates S, et al. Effect of intravenous haloperidol on the duration of delirium and coma in critically ill patients (Hope–ICU): A randomised, double-blind, placebo-controlled trial. The Lancet, Respiratory Medicine. 2013;1(7):515–523. doi: 10.1016/S2213-2600(13)70166-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pintor L, Fuente E, Bailles E, et al. Study on the efficacy and tolerability of amisulpride in medical/surgical inpatients with delirium admitted to a general hospital. European Psychiatry. 2009;24(7):450–455. doi: 10.1016/j.eurpsy.2009.05.013. [DOI] [PubMed] [Google Scholar]
- Sachdev P. A rating scale for acute drug-induced akathisia: Development, reliability, and validity. Biological Psychiatry. 1994;35(4):263–71. doi: 10.1016/0006-3223(94)91257-2. [DOI] [PubMed] [Google Scholar]
- Sachdev P. Akathisia and restless legs. Cambridge: Cambridge University Press; 1995. [Google Scholar]
- Sachdev P, Loneragan C. The present status of akathisia. The Journal of Nervous and Mental Disease. 1991;179(7):381–391. doi: 10.1097/00005053-199107000-00001. [DOI] [PubMed] [Google Scholar]
- Seneff MG, Mathews RA. Use of haloperidol infusions to control delirium in critically ill adults. The Annals of Pharmacotherapy. 1995;29(7–8):690–693. doi: 10.1177/106002809502907-806. [DOI] [PubMed] [Google Scholar]
- Takeuchi T, Furuta K, Hirasawa T, et al. Pero-spirone in the treatment of patients with delirium. Psychiatry and Clinical Neurosciences. 2007;61(1):67–70. doi: 10.1111/j.1440-1819.2007.01612.x. [DOI] [PubMed] [Google Scholar]
- Wada M, Ito H, Wada M, et al. Drug-induced akathisia as a cause of distress in spouse caregivers of cancer patients. Palliative & Supportive Care. 2011;9(2):209–212. doi: 10.1017/S1478951511000071. [DOI] [PubMed] [Google Scholar]
- White C, McCann MA, Jackson N. First do no harm … Terminal restlessness or drug-induced delirium. Journal of Palliative Medicine. 2007;10(2):345–351. doi: 10.1089/jpm.2006.0112. [DOI] [PubMed] [Google Scholar]
- Yoo JA, Kim SW, Bae KY, et al. Risperidone versus olanzapine for the treatment of delirium. European Neuropsychopharmacology. 2011;21:S493. doi: 10.1002/hup.1117. [DOI] [PubMed] [Google Scholar]
- Yoon HK, Kim YK, Han C, et al. Paliperidone in the treatment of delirium: Results of a prospective open-label pilot trial. Acta Neuropsychiatrica. 2011;23(4):179. doi: 10.1111/j.1601-5215.2011.00568.x. [DOI] [PubMed] [Google Scholar]