Abstract
The original concept of the NAD World was proposed in 2009, providing a comprehensive framework to investigate critical issues of biological robustness and trade-offs in mammalian aging and longevity control. Significant progress has been made over the past 7 years, advancing our understanding of the mechanisms by which biological robustness is maintained, and providing extensive support to the concept of the NAD World. Three key organs and tissues have been identified as basic elements in this control system for mammalian aging and longevity: the hypothalamus as the control center of aging, skeletal muscle as an effector, and adipose tissue as a modulator. While the hypothalamus sends a signal to skeletal muscle through the sympathetic nervous system, adipose tissue remotely regulates hypothalamic function by coordinating NAD+ biosynthesis at a systemic level. Skeletal muscle might also communicate with other organs and tissues by secreting various myokines. The mammalian NAD+-dependent protein deacetylase SIRT1 and the key NAD+ biosynthetic enzyme NAMPT mediate these inter-tissue communications. In this review, the function of each organ or tissue and their inter-tissue communications will be discussed in terms of understanding mammalian aging and longevity control. With such an emphasis on the system architecture, the concept is now reformulated as the NAD World 2.0, providing several important predictions. The concept of the NAD World 2.0 will provide a new foundation to understand a control system for mammalian aging and longevity and accelerate the development of an effective anti-aging intervention for humans.
Introduction
If you are asked to define ‘aging’ in one simple phrase, what would it be? One such definition of aging could be ‘breakdown of biological robustness’. In his insightful review article, Kitano defines ‘robustness’ as ‘a property that allows a system to maintain its functions against internal and external perturbations’.1 Each individual of living species is a robust biological system, and each biological system has been evolved to maintain its functionality against various types of perturbations for its survival and reproduction. A good example is the regulation of blood glucose levels. In human adults, fasting blood glucose levels are normally maintained within a relatively narrow range, 4–6 mmol/l. After meals, blood glucose levels shoot up but go back to normal levels within 2–3 h as far as insulin secretion and action are normal. While the functionality of insulin secretion and action is genetically defined, our current life style with nutrient-dense diets and the lack of enough exercise constantly imposes serious perturbations to this critical functionality that our system is designed to keep robust. Such complex interaction between environmental and genetic factors affects a delicate balance between insulin sensitivity and secretion, causing insulin resistance and reduced β-cell function over time.2–4 When our biological system can no longer maintain appropriate robustness to keep fasting glucose levels <7 mmol/l, our system would be derailed into a pathological condition, called type 2 diabetes. Interestingly, people who manifest insulin resistance do not necessarily develop type 2 diabetes,5–7 and insulin resistance and impaired β cell function can be reversed dose-dependently by progressive weight loss.8 Therefore, the development of insulin resistance and the reduction in β cell function, both of which are a part of normal aging, cannot be explained simply by aging theories that assume probabilistic functional deterioration as a cause of aging, such as the ‘wear and tear’ theory originally proposed by Weismann,9 but need to be reevaluated in the light of the mechanism of biological robustness.
Indeed, aging is the process of systemic, progressive functional decline, and it is conceivable that such functional decline is the result of biological robustness breakdown.10–12 To address this idea, it is very important to understand what comprises biological robustness in our system. System components, structure, and dynamics need to be identified. In this regard, significant progress has been made in the field of aging and longevity research in the past 20 years, and several evolutionarily conserved signaling pathways and regulators for aging and longevity control have been identified: Insulin/insulin-like growth factor 1 (IGF-1) signaling,13 mechanistic target of rapamycin (mTOR) signaling,14,15 and nicotinamide adenine dinucleotide (NAD+)-dependent sirtuins.16,17 These key components have been shown to mediate fundamental cellular processes that contribute to the cellular and molecular hallmarks of aging, such as mitochondrial dysfunction, epigenetic alterations, genomic instability, loss of proteostasis, and others,18 and determine lifespan in diverse model organisms. Now that we have better understanding of these regulatory components, it is time to elucidate the system structure and dynamics for aging and longevity control. To achieve this goal, we need to understand (1) in which organ or tissue each key component plays a major role in affecting the process of aging and determining lifespan, (2) what intrinsic and extrinsic perturbations alter the functionality of each key component in those specific organs and tissues, (3) where and how these functional changes in each key component begin to affect the biological robustness of the system, and (4) what determines the threshold and the rate of the biological robustness breakdown.19–21
Another critical issue to understand the process of aging and the determination of lifespan is the role of biological trade-offs in the context of biological robustness. Systems that have evolved to comprise a greater scale of complexity are optimized for perturbations they have encountered during the course of evolution, but are also inevitably susceptible to unexpected perturbations.1,22 In addition, robustness trade-offs extend not only between robustness and fragility, but also between robustness, resources, and performance.1,23 Identifying robustness trade-offs for each biological process in different species is critically important as the time course of aging-related breakdowns of physiological functions diverge substantially among species, implying that each species may have their own robustness trade-offs for each biological process. This may be a foundation of theoretical framework where reduction of robustness is related to reduction of other factors such as energy supply capability that is related to resource demands. This also suggests that biological trade-offs in resource allocation between reproduction and late-life events, which is predicted by the disposable soma theory proposed by Kirkwood,24 may not always be observed, dependent on the internal configuration of each system. Indeed, at least in Caenorhabditis elegans, while somatic tissues use their energy and resources to maintain the germ line and thereby reproductive integrity,24 stress responses to DNA damage in the germ line confer systemic protection of somatic tissues against other stresses through the induction of the innate immune response and the activation of the ubiquitin–proteasome system.25,26 Thus, identifying trade-offs between robustness and fragility in each biological system is critical to determine how and where the aging process is triggered as cascading system failures against the biological robustness in each organism.
The original concept of the NAD World was proposed in 2009 as an attempt to address all these critical issues of biological robustness and trade-offs in mammalian aging and longevity control.19,20 Since then, many critical findings have been made, adding new knowledge to further support the concept of the NAD World. In this review, I will summarize this progress and reformulate the concept as the NAD World 2.0, with an emphasis on the importance of the inter-tissue communication in the systemic regulation of mammalian aging and longevity.
The basic concept of the NAD world
The NAD World was originally proposed as a systemic regulatory network that intimately connects NAD+ metabolism, biological rhythm, and aging and longevity control in mammals.19–21,27,28 In the original concept, two key components comprise the NAD World: The mammalian NAD+-dependent protein deacetylase SIRT1, and systemic NAD+ biosynthesis mediated by nicotinamide phosphoribosyltransferase (NAMPT), a key NAD+ biosynthetic enzyme in mammals (Figure 1). It has been firmly established that SIRT1 is a critical metabolic regulator in many different organs and tissues.16,17,29,30 For instance, SIRT1 promotes glucose-stimulated insulin secretion in pancreatic β cells, stimulates fatty acid mobilization and adipokine production in adipose tissue, regulates glucose and lipid metabolism in the liver, and enhances fatty acid β-oxidation in skeletal muscle (Figure 1). Because NAD+ is absolutely required for all these important functions of SIRT1, NAMPT-mediated NAD+ biosynthesis plays an important role in regulating SIRT1 activity.31,32 In mammals, NAMPT has two different forms, intracellular and extracellular NAMPT (iNAMPT and eNAMPT, respectively; Figure 1).33,34 Surprisingly, eNAMPT has higher enzymatic activity compared with iNAMPT,35 and its novel function of supporting hypothalamic NAD+ has recently been found,36 as discussed later. SIRT1 and NAMPT together regulate the system dynamics of the NAD World. A good example of their cooperation is the regulation of a novel circadian feedback loop through the key circadian transcriptional regulators CLOCK/BMAL1, producing the circadian oscillation of NAD+ in peripheral organs and tissues and potentially in the suprachiasmatic nucleus.37–39 This circadian oscillation of NAD+ also impacts the activities of other sirtuins, namely mitochondrial SIRT3 and nuclear SIRT6, allowing the circadian regulation of oxidative metabolism in mitochondria and lipid/carbohydrate metabolism in the liver, respectively.40,41 In this regard, the importance of SIRT6 should also be emphasized because whole-body SIRT6-overexpressing mice have been reported to show lifespan extension, although it was observed only in males.42
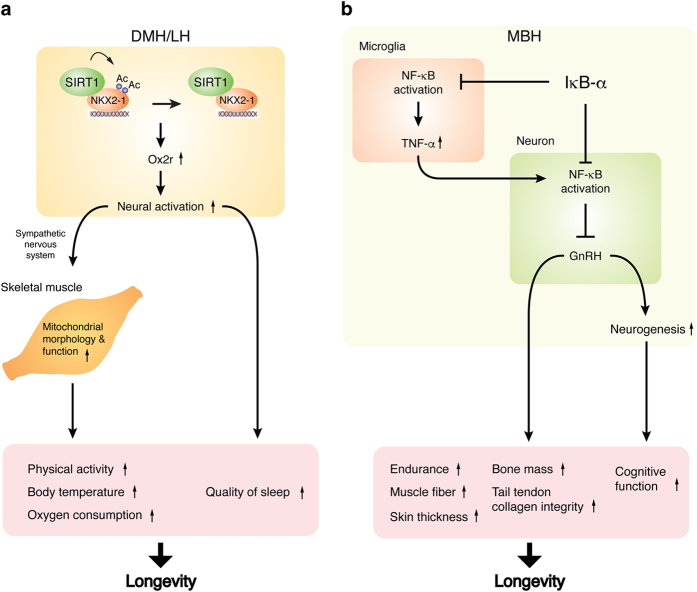
Figure 1.
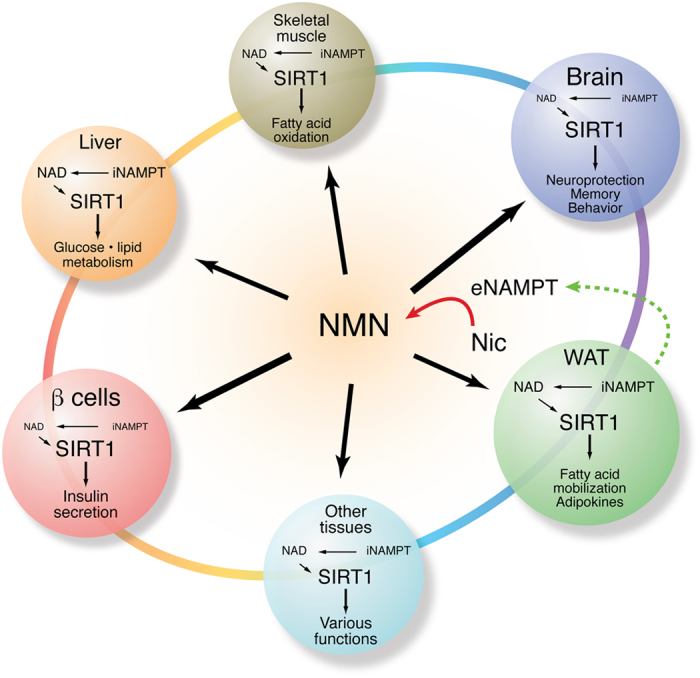
The original concept of the NAD World.20 The NAD World is a systemic regulatory network that fundamentally connects NAD+ metabolism, biological rhythm, and aging and longevity control in mammals. Two critical components comprise the NAD World: the mammalian NAD+-dependent protein deacetylase SIRT1, and systemic NAD+ biosynthesis mediated by nicotinamide phosphoribosyltransferase (NAMPT). While SIRT1 functions as a key mediator that orchestrates metabolic responses to changes in nutritional availability in multiple tissues, NAMPT-mediated NAD+ biosynthesis functions as a pace maker that produces circadian-oscillatory NAD+ production and fine-tunes SIRT1 activity at a systemic level. NAMPT has intra- and extracellular forms in mammals, iNAMPT and eNAMPT, respectively. iNAMPT is ubiquitously expressed, but its levels are varied (The font size reflects a relative level of iNAMPT). eNAMPT, which is actively secreted from adipose tissue and has a higher enzymatic activity than iNAMPT, likely synthesizes nicotinamide mononucleotide (NMN) from nicotinamide (Nic) extracellularly. The availability of NMN is particularly important for tissues and organs that possess very low levels of iNAMPT, such as pancreatic β cells and central neurons. The concept of the NAD World provides several important predictions for the biological robustness and trade-offs in mammalian aging and longevity control. See text for details.
Several critical predictions were made in the original concept of the NAD World. First, the decline in systemic NAD+ biosynthesis could be an important trigger for a variety of pathophysiological changes that significantly contribute to aging through decreased activities of SIRT1 and other sirtuins. This prediction has been demonstrated to be correct over the past 5 years. Indeed, NAMPT-mediated NAD+ biosynthesis declines with age in multiple organs and tissues, such as pancreas, adipose tissue, skeletal muscle, liver, and brain,43–48 reducing the activities of SIRT1 and other sirtuins in those organs and tissues. In addition, chronic activation of poly-ADP-ribose polymerases (PARPs), which might potentially be caused by a gradual accumulation of nuclear DNA damage, also accelerates NAD+ depletion and reduces sirtuin activity.45 Second, the concept indicated potential points of fragility in the biological system of mammals, namely, organs and tissues that have very low levels of iNAMPT. When systemic NAD+ biosynthesis begins to decline, these organs and tissues would respond first to the change and start having functional defects due to inadequate NAD+ biosynthesis and thereby reduced sirtuin activity. Two strong candidates for such fragility points are pancreatic islets and the brain (central neurons), both of which have been found to possess very low levels of iNAMPT.35 This predicted susceptibility of pancreatic islets and central neurons to NAD+ has been successfully demonstrated by the fact that changing NAD+ biosynthesis pharmacologically or genetically affects their functionality significantly.35,46,49,50 Last, the concept proposed that aging is the process in which biological robustness gradually alters and eventually breaks down according to a functional hierarchy determined by the susceptibility to systemic NAD+ biosynthesis. In other words, the cascade of robustness breakdown triggered by a decrease in systemic NAD+ biosynthesis and the resultant functional defects in susceptible organs and tissues is the central process of aging. This particular hypothesis has been addressed by enhancing the functionality of these fragility organs and tissues through genetic manipulation of SIRT1,51–53 which has led us to surprising but critical findings, as discussed in the next section.
Identifying the hypothalamus as a high-order control center of aging
Given that pancreatic islets and central neurons are two strong candidates of fragility points in the mammalian biological system, the prediction was that overexpression of SIRT1 in these fragility points would enhance their functionality and significantly alter the dynamics of the aging process, potentially extending lifespan. To test this prediction, pancreatic β-cell-specific SIRT1-overexpressing (BESTO) mice were generated first.51 Interestingly, BESTO mice showed enhancement of glucose-stimulated insulin secretion in pancreatic islets, demonstrating the importance of SIRT1 in pancreatic β-cell function. Other groups also confirmed the finding.54,55 However, unexpectedly, this phenotype of BESTO mice was lost completely when they became old.52 Importantly, administration of nicotinamide mononucleotide (NMN), a key NAD+ intermediate and a product of the NAMPT reaction, restored the phenotype in aged BESTO mice and even enhanced insulin secretion in old wild-type control mice.52 It has also been reported that eNAMPT and NMN potentiate glucose-stimulated insulin secretion in human islets.49 These findings strongly suggest that pancreatic islets are indeed a fragility point that is very susceptible to the decline in NAD+ biosynthesis. Nonetheless, upregulating SIRT1 in pancreatic islets fails to affect the process of aging likely due to their high susceptibility to NAD+ decline.
To examine the other candidate, central neurons, brain-specific SIRT1-overexpressing (BRASTO) mice were generated using the mouse prion promoter.56 Strikingly, BRASTO mice exhibited significant delay in aging and lifespan extension in both males and females.53 Several physiological traits, including physical activity, body temperature, oxygen consumption, and quality of sleep, were significantly maintained when BRASTO mice became old. In particular, their skeletal muscle maintained youthful morphology and function of the mitochondria during the aging process,53 implicating that sarcopenia could be prevented by stimulating SIRT1 in the brain. This phenotype is caused by enhanced neural activity in two hypothalamic regions called the dorsomedial and lateral hypothalamic nuclei (DMH and LH, respectively), which stimulates skeletal muscle through the sympathetic nervous system. SIRT1 and its binding partner NKX2-1, an NK2 family homeodomain transcription factor, together upregulate the expression of the orexin type 2 receptor (Ox2r) gene, leading to neural activation in these hypothalamic nuclei.53 Results from DMH/LH-specific Sirt1, Nkx2-1, and Ox2r knockdown provided further support to the importance of SIRT1/NKX2-1/OX2R-mediated signaling pathway to counteract age-associated physiological decline (Figure 2a). In addition, overexpressing SIRT1 only in the DMH of aged wild-type mice restored youthful levels of physical activity and body temperature.53 All these findings strongly suggest that neurons in the brain, particularly those in the hypothalamus, play a crucial role in regulating the process of aging and determining lifespan.57
Figure 2.
The hypothalamus as the high-order control center of aging. (a) SIRT1/NKX2-1/OX2R-mediated signaling in the dorsomedial and lateral hypothalamic nuclei (DMH and LH, respectively) regulates the aging process and longevity in mammals.53 SIRT1 and its binding partner NKX2-1 (NK2 homeobox 1) upregulate the transcription of the orexin type 2 receptor (Ox2r) gene, leading to neural activation during the dark time. This neural activation stimulates two separate functions: one is the stimulation of skeletal muscle through the sympathetic nervous system, which maintains mitochondrial morphology and function during the aging process, and the other is the stimulation of delta activity in electroencephalogram, which contributes to the maintenance of the quality of sleep. These functions contribute to the promotion of longevity. (b) NF-κB signaling in the mediobasal hypothalamus (MBH) systemically regulates aging and longevity in mammals.58 In the MBH, NF-κB activation in microglia enhances the production of the inflammatory cytokine tumor necrosis factor-α (TNF-α). TNF-α then activates NF-κB signaling in MBH neurons that produce gonadotropin-releasing hormone (GnRH). GnRH is able to prevent various age-associated changes shown in this figure. Thus, inhibiting NF-κB signaling in the MBH prolongs lifespan, whereas activating NF-κB in the MBH shortens lifespan in mice.
Another group also reached the same conclusion regarding the importance of the hypothalamus in mammalian aging and longevity control. Cai’s group58 demonstrated that inhibiting nuclear factor-κB (NF-κB) in neurons of the mediobasal hypothalamus (MBH) extends lifespan in mice, whereas activating NF-κB in MBH neurons shortens their lifespan. In the MBH, microglial NF-κB activation at an earlier stage of aging results in the production of tumor necrosis factor-α (TNF-α), which further stimulates hypothalamic neurons and activates their NF-κB. NF-kB activation suppresses transcription of the gonadotropin-releasing hormone (Gnrh) gene, resulting in the decline in neurogenesis in the hypothalamus and hippocampus, muscle strength (endurance), muscle (fiber) size, skin thickness, bone mass, and tail tendon collagen integrity (Figure 2b).58 Given that TNF-α decreases NAMPT and NAD+ levels47 and also that SIRT1/6 and SIRT2 could suppress NF-κB signaling in neurons and microglia, respectively,59–61 NAD+ biosynthesis could be suppressed by microglia-mediated inflammation in the hypothalamus, leading to reduced sirtuin activity and thereby causing systemic age-associated functional decline.
These findings strongly suggest that the hypothalamus functions as a high-order control center of aging in mammals, controlling the process of aging and limiting lifespan.57,58 These recent studies also shed new light on the hypothalamic/neuroendocrine theory of aging proposed by Dilman62 in 1971 and the concept of ‘the aging clock’ proposed by Everitt in 1973.63 Remarkably, almost a half century ago, Dilman62 already pointed out that aging is ‘a process of disordered homeostatic stability of internal environment’ so that ‘permanent deviations from the law of constancy of the internal environment’ could ultimately produce ‘the specific lesions of ageing’. It has now been suggested that certain subsets of neurons in specific hypothalamic regions, such as SIRT1/NKX2-1-double-positive neurons in the DMH and GnRH-producing neurons in the MBH, might be a key fragility point in our system, and their functional decline could trigger the breakdown of the biological robustness at a systemic level. Given that SIRT1 and NKX2-1 regulate orexin signaling, it is intriguing that overexpression of the uncoupling protein 2 (UCP2) in orexin/hypocretin neurons exhibits increased energy efficiency and median lifespan extension, another support for the importance of hypothalamic neurons in mammalian aging and longevity control.64 Further investigation is currently ongoing to elucidate the characteristics and the functions of these key hypothalamic neurons in mammalian aging and longevity control.
Skeletal muscle as an effector in aging and longevity control
Skeletal muscle receives a signal from the hypothalamus, a control center of aging, through the sympathetic nervous system.65 This stimulation increases the expression of the β2 adrenergic receptor gene and the tissue levels of cAMP and over time maintains mitochondrial structural integrity and function in skeletal muscle.53,65 Most recently, the neuromuscular junction has been identified as a target of the sympathetic nervous system, and sympathetic input is crucial for the maintenance and function of the neuromuscular junction.65 Obviously, the mechanics and the regulation of skeletal muscle position it to be an actuator in the system. However, skeletal muscle has recently been recognized as an endocrine organ that affects the functions of other organs and tissues through secretion of humoral factors, categorically called myokines.66 Interestingly, we have recently found that skeletal muscle produces a certain myokine in response to the sympathetic nervous tone stimulated by the hypothalamus (our unpublished finding). In flies, it has been shown that skeletal muscle modulates age-associated phenotypes at a systemic level and eventually affects lifespan through the secretion of growth factors and cytokines.67 For instance, Demontis and Perrimon68 demonstrated that in Drosophila, muscle-specific overexpression of foxo and its target gene 4E-BP reduces protein aggregates via the autophagy/lysosome system not only in muscle but also in the retina, brain, and adipose tissue, systemically mitigating age-associated functional decline and extending lifespan through decreasing food intake and insulin release. The same group also demonstrated that in Drosophila, muscle-specific overexpression of the transcription factor Mnt, a basic helix-loop-helix factor homologous to human MNT/MAD, decreases age-related muscle dysfunction and ribosomal rRNA levels and nucleolar size in adipocytes and extends lifespan through the upregulation of Myoglianin, a myokine homologous to human myostatin and GDF-11.69 In mammals, skeletal muscle-specific enhancement of 4E-BP activity protects against age- and diet-induced insulin resistance and metabolic decline directly through increased peroxisome proliferator-activated receptor γ-coactivator 1α (PGC-1α) and enhanced respiration.70 These phenotypes, particularly adipose phenotypes, appear to be mediated by the myokine FGF21,70 whose overexpression has been reported to extend lifespan in mice.71 Based on these findings, we hypothesize that in addition to its function as an actuator in the system, skeletal muscle functions as an effector that regulates the functions of other organs and tissues through the production and secretion of specific myokines in response to a signal from the control center of aging, namely the hypothalamus, and contributes to the maintenance of biological robustness. In this model, intrinsic and extrinsic perturbations to the high-order fragility point, such as microglia-induced inflammation72 and constant exposure to blue light,73 could affect the actuator/effector function of skeletal muscle through decreased sympathetic nervous tone, potentially triggering the breakdown of biological robustness. To address this model, it will be of great importance (1) to elucidate the regulation of skeletal muscle function by the hypothalamus and the sympathetic nervous system and (2) to identify key myokines whose production and/or secretion are regulated by the hypothalamus and examine their roles in the communication with other organs and tissues.
Adipose tissue functions as a modulator for the control center of aging
Adipose tissue functions not only for fat storage but also as an endocrine organ that secretes a variety of factors, called adipokines, including leptin, adiponectin, and resistin.74 Interestingly, both fully differentiated white and brown adipocytes actively secrete eNAMPT, which possesses a significantly higher enzymatic activity than iNAMPT.35 We have recently demonstrated that SIRT1-dependent deacetylation of iNAMPT at lysine 53 (K53) predisposes the protein to secretion in adipocytes (Figure 3).36 Whole-body and adipose tissue-specific Sirt1 knockout mice completely fail to secrete eNAMPT in response to fasting, confirming the physiological relevance of this SIRT1-mediated eNAMPT secretion from adipose tissue.36 These findings reveal that SIRT1 and NAMPT comprise a novel NAD+-regulatory feedback loop through the regulation of eNAMPT secretion. Surprisingly, adipose tissue-specific Nampt knockout and knockin (ANKO and ANKI) mice exhibit reciprocal changes in circulating eNAMPT levels, hypothalamic NAD+ levels, SIRT1 target gene expression, and physical activity.36 The defect in physical activity observed in ANKO mice can be ameliorated by administration of NMN, providing support to our conclusion that hypothalamic NAD+ biosynthesis and function are regulated by eNAMPT and its product NMN. Furthermore, systemic injection of a NAMPT-neutralizing antibody reduces hypothalamic NAD+ levels in vivo, whereas treating hypothalamic explants with purified eNAMPT enhances NAD+, SIRT1 activity, and neural activity ex vivo.36 These findings strongly indicate that NAD+/SIRT1-mediated eNAMPT secretion from adipose tissue plays a crucial role in remotely regulating hypothalamic NAD+ biosynthesis and function (Figure 3). In other words, adipose tissue functions as a modulator for the hypothalamus, the control center of aging, through the secretion of eNAMPT. This model leads us to an interesting prediction that having optimal adiposity that maximizes circulating eNAMPT activity would maximize the biological robustness of our system through the regulation of systemic NAD+ biosynthesis. Interestingly, it has been reported that the lifespan response of 41 recombinant inbred strains of mice to diet restriction (DR), the most reproducible experimental regimen that delays aging and extends lifespan in a wide variety of organisms, ranges from extension to shortening of lifespan.75 Importantly, in these strains, the effect of lifespan extension by DR correlates inversely with fat reduction measured at mid-life and later ages.76 In other words, the mouse strains maintaining more fat in their later lives tend to show longer lifespan, implicating that factors associated with maintaining fat are important for survival and lifespan extension under DR. Furthermore, even in the human population, it has been well-known that very low adiposity is not associated with longer lifespan. The optimal body mass index (BMI) that minimizes the risk of death from any cause is 24–25 for men and 22–23 for women, always on the slightly overweight side.77–80 People who have BMI <20 tend to suffer from cardiovascular, neuronal, and pulmonary diseases and have higher death rates when they become old.77,79 Although the precise mechanisms underlying these phenomena remain unknown, it will be of great interest to address the hypothesis that slightly higher adiposity could optimize the functionality of the control center of aging and minimize the risk of death.
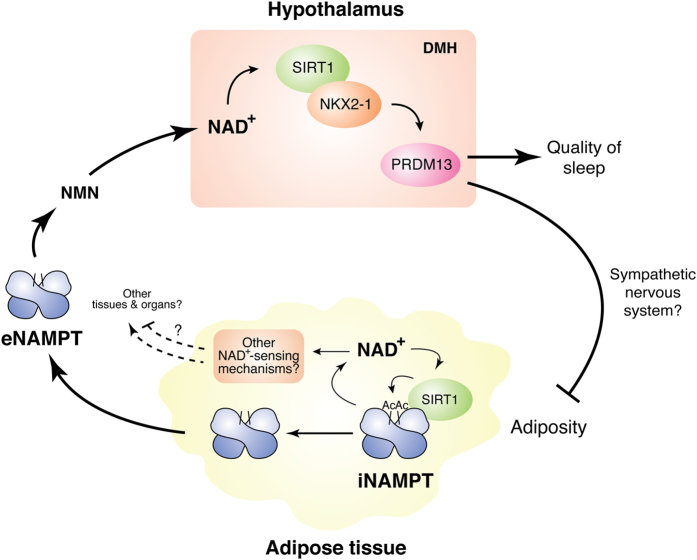
Figure 3.
The feedback mechanism between the hypothalamus and adipose tissue that maintains hypothalamic NAD+ levels through the secretion of eNAMPT.36 In adipose tissue, iNAMPT is acetylated, and SIRT1 specifically deacetylates lysine 53 and predisposes iNAMPT to secretion in a NAD+-dependent manner. eNAMPT secreted from adipose tissue remotely promotes NAD+ biosynthesis in the hypothalamus likely through the extracellular synthesis of NMN and enhances SIRT1 activity and neural activity. In the DMH, SIRT1 and its binding partner NKX2-1 regulate the transcription of Prdm13 (PR domain-containing protein 13), which controls the quality of sleep and adiposity. This NAD+/SIRT1-mediated eNAMPT-secreting function of adipose tissue positions this tissue to be a modulator/sensor in the system. Adipose tissue might also have another NAD+-sensing mechanism that could affect the functions of other organs and tissues. DMH, dorsomedial hypothalamic nuclei.
This inter-tissue communication between the hypothalamus and adipose tissue likely comprises a critical feedback loop for aging and longevity control (Figure 3). Many studies have already demonstrated that different hypothalamic nuclei regulate adipose tissue through the autonomic nervous system.81 We identified Prdm13 (PR domain-containing protein 13) as a gene highly and selectively expressed in the DMH.82 The expression of Prdm13 in the hypothalamus increases under DR, whereas it decreases during aging. In addition, its expression also shows robust diurnal oscillation and is significantly upregulated in the DMH of long-lived BRASTO mice. Interestingly, DMH-specific Prdm13-knockdown mice exhibit a significant defect in sleep quality during non-REM sleep and a progressive increase in adiposity, two common age-associated complications in rodents and humans (Figure 3).82 Nonetheless, these mice show no change in their food intake, suggesting that PRDM13 in the DMH directly regulates adiposity. Given that Prdm13 is under the regulation of the SIRT1/NKX2-1-mediated signaling pathway in the DMH,82 the hypothalamus as the control center of aging and adipose tissue as a modulator comprise a complex NAD+-dependent feedback loop through these key players. For instance, when NAMPT and NAD+ levels decrease over age in adipose tissue,47 this would decrease SIRT1 activity and secretion of enzymatically active eNAMPT from adipose tissue to blood circulation. Decreasing circulating eNAMPT activity would affect NAD+ biosynthesis and SIRT1 activity in the hypothalamus, leading to decreased Prdm13 expression in the DMH over age.82 Decreased PRDM13 activity in the DMH would stimulate adipose tissue probably through the sympathetic nervous system, increasing adiposity to compensate the decrease in eNAMPT secretion in aged individuals. In this model, one interesting question is whether adipose tissue can also function as a sensor that detects NAD+ changes sensitively and sends signals to other organs and tissues (Figure 3). Further investigation will be necessary to address this interesting possibility. Another interesting question is whether enforcing this feedback loop between the hypothalamus and adipose tissue could affect the system dynamics of the aging process and contribute to the determination of lifespan in mammals. This particular question is currently being addressed by analyzing ANKI mice.36
NAD world 2.0: a systems-biological approach to understand, and control aging and longevity in mammals
As summarized above, these new findings over the past 7 years have significantly advanced our understanding of the system architecture for mammalian aging and longevity control, providing critical information that deepens the original concept of the NAD World. In particular, identifying the inter-tissue communication between the hypothalamus, skeletal muscle, and adipose tissue provides new insights into how biological robustness is regulated throughout our biological system in terms of understanding mammalian aging and longevity control. Although further extensive studies will be required to elucidate the entire system architecture of the NAD World, it has at least basic elements of a control system from an engineering point-of-view: The hypothalamus as the controller, skeletal muscle as an actuator, and adipose tissue as a possible sensor. As discussed in previous sections, however, each organ or tissue usually has more than one function designated by a specific engineering term. Thus, both biological and engineering terms are used in parallel to further describe the functionality of these organs and tissues in the NAD World (Figure 4).
Figure 4.
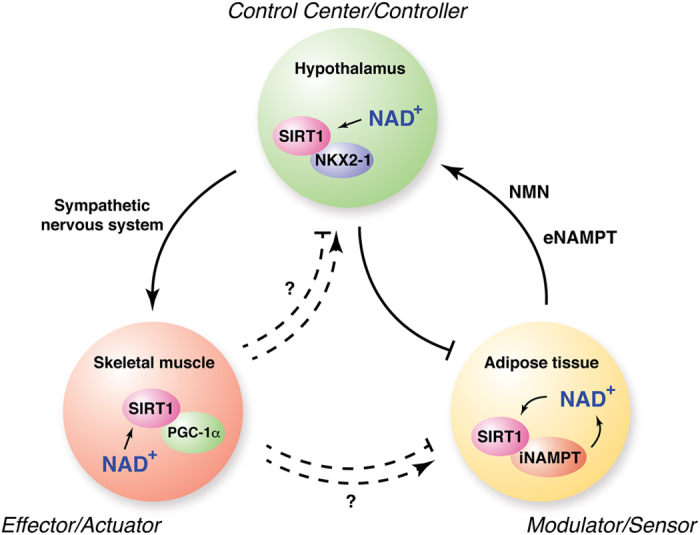
The concept of the NAD World 2.0. The original concept of the NAD World is now reformulated as the NAD World 2.0, with an emphasis on the importance of the inter-tissue communication between three key organs and tissues, namely, the hypothalamus as the control center of aging/controller, skeletal muscle as an effector/actuator, and adipose tissue as a modulator/possible sensor (both biological and engineering terms are described in parallel). Cooperative functions of SIRT1 and NAMPT, both iNAMPT and eNAMPT, play a crucial role in regulating the system dynamics of this inter-tissue communications. The NAD World 2.0 as a control system provides new insights into the regulation of biological robustness and fragility in mammalian aging and longevity control. See text for details.
How is the NAD World controlled? As a control system, the following three mechanisms play a critical role in controlling the NAD World:
The NAD+-driven regulation of SIRT1 activity in a specific subset of hypothalamic neurons, such as SIRT1/NKX2-1-double-positive neurons in the DMH (Figure 4). Maintaining appropriate activity levels of SIRT1, likely as well as other sirtuins, in these specific hypothalamic neurons is critical to control the function of skeletal muscle as an actuator, determining physical activity levels of individuals.36,53 This particular signal also stimulates the effector function of skeletal muscle, producing certain specific myokines and possibly affecting the hypothalamus or other organs and tissues (Figure 4). Prdm13, a downstream target of the SIRT1/NKX2-1 signaling, also negatively regulates adiposity.82 In this regard, the level of hypothalamic NAD+ is the critical target of control, and it is regulated by the feedback loop between the hypothalamus and adipose tissue. Importantly, the set point of hypothalamic NAD+ could be affected by internal and external perturbations and thereby shifted over time, which could derail the entire system from the range of biological robustness.
The feedback loop between the hypothalamus and adipose tissue through the secretion of enzymatically active eNAMPT (Figures 3 and 4). As discussed in the previous section, the secretion of eNAMPT is regulated by adipose NAD+ and SIRT1,36 which positions adipose tissue to be a sensor of NAD+ in the system. In addition, adipose tissue modulates NAD+ levels in a circadian-oscillatory manner, propagating its internal rhythm to other organs and tissues, including the hypothalamus. It should be noted that adipose NAD+ levels are an independent valuable that could be affected by different perturbations with different time constants. Because eNAMPT plays an important role in coordinating systemic NAD+ biosynthesis, its reaction product, NMN, must have an important function to maintain the biological robustness throughout the system. Indeed, it has already been demonstrated that NMN shows remarkable effects of ameliorating disease conditions, including type 2 diabetes, ischemia/reperfusion injury, and Alzheimer’s disease.47,83–85 In this regard, how NMN uptake is regulated is another important target of control, and intensive investigation is currently underway to address this critical issue.
Another possible feedback loop between the hypothalamus and skeletal muscle through the secretion of specific myokines (Figure 4). Compared with the other two mechanisms, this particular feedback mechanism is rather speculative at this moment. Nonetheless, different from other tissues, one important feature that skeletal muscle has is a feed-forward control of its own NAD+ biosynthesis in response to exercise. It has been demonstrated that skeletal muscle induces NAMPT and NAD+ levels in response to exercise in rodents and humans.86–88 Given that skeletal muscle functions as an effector/actuator, this specific feature of skeletal muscle likely plays an important role in enhancing a signal back to the hypothalamus or to other organs and tissues, enforcing the strength of this feedback mechanism and contributing to the maintenance of biological robustness. Further studies will be necessary to elucidate molecular details of the feedback mechanisms that skeletal muscle mediates in this control system.
This reformulated version of the NAD World concept, now called the NAD World 2.0, defines the system architecture for mammalian aging and longevity control, and provides several interesting predictions to further investigate this control system. First, any perturbations to NAD+ levels in the hypothalamus, particularly in key hypothalamic neurons, could change the process of aging and eventually affect lifespan. Hypothalamic neurons are a critical fragility point, and their function could be impaired by even a slight decrease in NAD+ availability, potentially caused by accumulation of inflammation and other damages.72 When the feedback loop between the hypothalamus and adipose tissue functions normally, such decreases in hypothalamic NAD+ levels could be compensated by increasing eNAMPT secretion from adipose tissue. However, NAMPT-mediated NAD+ biosynthesis also independently declines over age in adipose tissue, likely due to chronic inflammation developed within adipose tissue. Thus, the system would eventually reach a point where the robustness of this feedback loop between the hypothalamus and adipose tissue can no longer be maintained. Once this breakdown starts happening, the hypothalamus would lose its function and eventually derail the entire system. If this is the case, any manipulation that enhances the resilience of key hypothalamic neurons against such NAD+ reduction could counteract age-associated functional decline and possibly extend lifespan in mammals. To address this prediction, it will be of great importance to examine the aging process and the lifespan of ANKI mice that have increased levels of circulating eNAMPT.36 ANKI mice are predicted to preserve hypothalamic NAD+ and function longer than control wild-type mice and show significant delay in aging and possibly lifespan extension.
Second, the feedback mechanism between the hypothalamus and adipose tissue predicts the importance of NMN as a systemic signaling molecule that maintains biological robustness. Given that NAD+ levels decline with age in various organs and tissues in rodents and humans,43–48 boosting NAD+ biosynthesis with NMN or nicotinamide riboside, another NAD+ intermediate that is converted to NMN, in key system-controlling organs and tissues could maintain biological robustness and delay the aging process in mammals.43,47,89,90 In particular, when the feedback mechanism can no longer maintain normal NAD+ levels in the hypothalamus, intervening the system with NMN administration would be expected to normalize hypothalamic NAD+ levels and ameliorate ‘hallmarks of aging’, including inter-cellular or inter-tissue communications.18 In this regard, sarcopenia would be an interesting model to test this prediction. As observed in aged BRASTO mice, an enhanced signal from the hypothalamus would be expected to maintain the structure and the function of skeletal muscle as an effector/actuator. NMN treatment would be able to achieve this goal through the stimulation of hypothalamic function.
Third, specific myokines secreted from skeletal muscle in response to signals from the hypothalamus would affect the process of aging and possibly lifespan in mammals. Potentially, these myokines might be an important part of the feedback mechanism between the hypothalamus and skeletal muscle. In this regard, FGF21 is an interesting candidate. It has been reported that FGF21 acts directly on the suprachiasmatic nucleus of the hypothalamus and the dorsal vagal complex of the hindbrain, mimicking the physiological response to fasting.91 Overexpression of FGF21 has also been reported to extend lifespan in mice.71 Another interesting candidate is myostatin (GDF-8), a myokine that negatively regulates muscle mass. Interestingly, myostatin-deficient heterozygous mice have been reported to show 10% and 16% extension for median and maximal lifespan, respectively.92 There may be other myokines that can affect other hypothalamic nuclei, such as DMH, and comprise a feedback loop between the hypothalamus and skeletal muscle. This prediction is currently being tested by manipulating a myokine identified to respond to a signal from the hypothalamus.
Concluding remarks
The NAD World 2.0 is a reformulated version of the original concept of the NAD World, emphasizing the importance of the inter-tissue communications between the hypothalamus as the control center of aging/controller, skeletal muscle as an effector/actuator, and adipose tissue as a modulator/possible sensor in the systemic regulation of aging and longevity in mammals. Although further investigation is absolutely necessary to dissect precise details of the system dynamics in this control system, the NAD World 2.0 provides new insights and predictions into how we can better understand mammalian aging and longevity control and how we can manipulate such a control system to alter the process of aging and longevity. It will be of great importance to further elucidate the kinetics of feedback mechanisms between the hypothalamus and adipose tissue or skeletal muscle. Of course, other organs and tissues might also be important, adding more layers of regulation to this control system. In addition, further investigating the features of key fragility points, particularly hypothalamic neurons that have very low levels of iNAMPT, will provide critical insights into how biological robustness breakdown contributes to the aging process. Last, by taking such a systems-biological approach, we will be able to develop an effective intervention, using NAD+ intermediates such as NMN and NR, which would allow us to control the aging process and eventually extend healthspan and lifespan in humans. In the next 5–10 years, new exciting progress in the field of aging and longevity research will surely drive further evolution of the concept of the NAD World 2.0.
Acknowledgments
I apologize to those whose work is not cited due to space limitations. I thank Hiroaki Kitano for providing critical comments on this review and members in the lab of SI for constructive discussions and suggestions. SI is supported by grants from the National Institute on Aging (AG037457, AG047902).
Footnotes
SI was a co-founder of Metro Midwest Biotech.
References
- Kitano, H. Towards a theory of biological robustness. Mol. Syst. Biol. 3, 137 (2007). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Basu, R. et al. Mechanisms of the age-associated deterioration in glucose tolerance: contribution of alterations in insulin secretion, action, and clearance. Diabetes 52, 1738–1748 (2003). [DOI] [PubMed] [Google Scholar]
- Iozzo, P. et al. Independent influence of age on basal insulin secretion in nondiabetic humans. European Group for the Study of Insulin Resistance. J. Clin. Endocrinol. Metab. 84, 863–868 (1999). [DOI] [PubMed] [Google Scholar]
- Muoio, D. M. & Newgard, C. B. Mechanisms of disease: molecular and metabolic mechanisms of insulin resistance and beta-cell failure in type 2 diabetes. Nat. Rev. Mol. Cell Biol. 9, 193–205 (2008). [DOI] [PubMed] [Google Scholar]
- Ahrén, B. & Pacini, G. Islet adaptation to insulin resistance: mechanisms and implications for intervention. Diabetes Obes Metab. 7, 2–8 (2005). [DOI] [PubMed] [Google Scholar]
- Kahn, S. E. , Hull, R. L. & Utzschneider, K. M. Mechanisms linking obesity to insulin resistance and type 2 diabetes. Nature 444, 840–846 (2006). [DOI] [PubMed] [Google Scholar]
- Weir, G. C. & Bonner-Weir, S. Five stages of evolving beta-cell dysfunction during progression to diabetes. Diabetes 53(Suppl 3): S16–S21 (2004). [DOI] [PubMed] [Google Scholar]
- Magkos, F. et al. Effects of moderate and subsequent progressive weight loss on metabolic function and adipose tissue biology in humans with obesity. Cell Metab. 23, 591–601 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weismann, A. in Essays upon Heredity and Kindred Biological Problems. Vol. 1, 2nd edn (eds Poulton, E.B., Shonland, S. & Shipley A. E.) 1–66 (Clarendon Press, Oxford, 1881).
- Cohen, A. A. Complex systems dynamics in aging: new evidence, continuing questions. Biogerontology 17, 205–220 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Imai, S. SIRT1 and caloric restriction: an insight into possible trade-offs between robustness and frailty. Curr Opin Clin Nutr Metab Care 12, 350–356 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kriete, A. Robustness and aging--a systems-level perspective. Biosystems 112, 37–48 (2013). [DOI] [PubMed] [Google Scholar]
- Kenyon, C. J. The genetics of ageing. Nature 464, 504–512 (2010). [DOI] [PubMed] [Google Scholar]
- Stanfel, M. N. , Shamieh, L. S. , Kaeberlein, M. & Kennedy, B. K. The TOR pathway comes of age. Biochim. Biophys. Acta 1790, 1067–1074 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zoncu, R. , Efeyan, A. & Sabatini, D. M. mTOR: from growth signal integration to cancer, diabetes and ageing. Nat. Rev. Mol. Cell Biol. 12, 21–35 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haigis, M. C. & Sinclair, D. A. Mammalian sirtuins: biological insights and disease relevance. Annu. Rev. Pathol. 5, 253–295 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Imai, S. & Guarente, L. NAD+ and sirtuins in aging and disease. Trends. Cell Biol. 24, 464–471 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lopez-Otin, C. , Blasco, M. A. , Partridge, L. , Serrano, M. & Kroemer, G. The hallmarks of aging. Cell 153, 1194–1217 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Imai, S. From heterochromatin islands to the NAD World: a hierarchical view of aging through the functions of mammalian Sirt1 and systemic NAD biosynthesis. Biochim. Biophys. Acta 1790, 997–1004 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Imai, S. The NAD World: a new systemic regulatory network for metabolism and aging—Sirt1, systemic NAD biosynthesis, and their importance. Cell Biochem. Biophys. 53, 65–74 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Imai, S. Dissecting systemic control of metabolism and aging in the NAD World: the importance of SIRT1 and NAMPT-mediated NAD biosynthesis. FEBS Lett. 585, 1657–1662 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carlson, J. M. & Doyle, J. Highly optimized tolerance: robustness and design in complex systems. Phys. Rev. Lett. 84, 2529–2532 (2000). [DOI] [PubMed] [Google Scholar]
- Kitano, H. Biological robustness. Nat. Rev. Genet. 5, 826–837 (2004). [DOI] [PubMed] [Google Scholar]
- Kirkwood, T. B. & Holliday, R. The evolution of ageing and longevity. Proc. R. Soc. Lond. B Biol. Sci. 205, 531–546 (1979). [DOI] [PubMed] [Google Scholar]
- Douglas, P. M. & Dillin, A. The disposable soma theory of aging in reverse. Cell Res. 24, 7–8 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ermolaeva, M. A. et al. DNA damage in germ cells induces an innate immune response that triggers systemic stress resistance. Nature 501, 416–420 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Imai, S. ‘Clocks’ in the NAD World: NAD as a metabolic oscillator for the regulation of metabolism and aging. Biochim. Biophys. Acta 1804, 1584–1590 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Imai, S. & Yoshino, J. The importance of NAMPT/NAD/SIRT1 in the systemic regulation of metabolism and ageing. Diabetes Obes. Metab. 15(Suppl 3): 26–33 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Canto, C. , Menzies, K. J. & Auwerx, J. NAD(+) metabolism and the control of energy homeostasis: a balancing act between mitochondria and the nucleus. Cell Metab. 22, 31–53 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Satoh, A. , Stein, L. & Imai, S. The role of mammalian sirtuins in the regulation of metabolism, aging, and longevity. Handb. Exp. Pharmacol. 206, 125–162 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Revollo, J. R. , Grimm, A. A. & Imai, S. The NAD biosynthesis pathway mediated by nicotinamide phosphoribosyltransferase regulates Sir2 activity in mammalian cells. J. Biol. Chem. 279, 50754–50763 (2004). [DOI] [PubMed] [Google Scholar]
- Revollo, J. R. , Grimm, A. A. & Imai, S. The regulation of nicotinamide adenine dinucleotide biosynthesis by Nampt/PBEF/visfatin in mammals. Curr. Opin. Gastroenterol. 23, 164–170 (2007). [DOI] [PubMed] [Google Scholar]
- Garten, A. et al. Physiological and pathophysiological roles of NAMPT and NAD metabolism. Nat. Rev. Endocrinol. 11, 535–546 (2015). [DOI] [PubMed] [Google Scholar]
- Imai, S. Nicotinamide phosphoribosyltransferase (Nampt): a link between NAD biology, metabolism, and diseases. Curr. Pharm. Des. 15, 20–28 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Revollo, J. R. et al. Nampt/PBEF/visfatin regulates insulin secretion in β cells as a systemic NAD biosynthetic enzyme. Cell Metab. 6, 363–375 (2007). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yoon, M. J. et al. SIRT1-mediated eNAMPT secretion from adipose tissue regulates hypothalamic NAD(+) and function in mice. Cell Metab. 21, 706–717 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chang, H. C. & Guarente, L. SIRT1 mediates central circadian control in the SCN by a mechanism that decays with aging. Cell 153, 1448–1460 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nakahata, Y. , Sahar, S. , Astarita, G. , Kaluzova, M. & Sassone-Corsi, P. Circadian control of the NAD+ salvage pathway by CLOCK-SIRT1. Science 324, 654–657 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ramsey, K. M. et al. Circadian clock feedback cycle through NAMPT-mediated NAD+ biosynthesis. Science 324, 651–654 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Masri, S. et al. Partitioning circadian transcription by SIRT6 leads to segregated control of cellular metabolism. Cell 158, 659–672 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peek, C. B. et al. Circadian clock NAD+ cycle drives mitochondrial oxidative metabolism in mice. Science 342, 1243417 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kanfi, Y. et al. The sirtuin SIRT6 regulates lifespan in male mice. Nature 483, 218–221 (2012). [DOI] [PubMed] [Google Scholar]
- Gomes, A. P. et al. Declining NAD(+) Induces a pseudohypoxic state disrupting nuclear-mitochondrial communication during aging. Cell 155, 1624–1638 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Massudi, H. et al. Age-associated changes in oxidative stress and NAD+ metabolism in human tissue. PLoS ONE 7, e42357 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mouchiroud, L. et al. The NAD(+)/Sirtuin pathway modulates longevity through activation of mitochondrial UPR and FOXO signaling. Cell 154, 430–441 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stein, L. R. & Imai, S. Specific ablation of Nampt in adult neural stem cells recapitulates their functional defects during aging. EMBO J. 33, 1321–1340 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yoshino, J. , Mills, K. F. , Yoon, M. J. & Imai, S. Nicotinamide mononucleotide, a key NAD(+) intermediate, treats the pathophysiology of diet- and age-induced diabetes in mice. Cell Metab. 14, 528–536 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhu, X. H. , Lu, M. , Lee, B. Y. , Ugurbil, K. & Chen, W. In vivo NAD assay reveals the intracellular NAD contents and redox state in healthy human brain and their age dependences. Proc. Natl Acad. Sci. USA 112, 2876–2881 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spinnler, R. et al. The adipocytokine Nampt and its product NMN have no effect on beta-cell survival but potentiate glucose stimulated insulin secretion. PLoS ONE 8, e54106 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stein, L. R. et al. Expression of Nampt in hippocampal and cortical excitatory neurons is critical for cognitive function. J Neurosci. 34, 5800–5815 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moynihan, K. A. et al. Increased dosage of mammalian Sir2 in pancreatic b cells enhances glucose-stimulated insulin secretion in mice. Cell Metab. 2, 105–117 (2005). [DOI] [PubMed] [Google Scholar]
- Ramsey, K. M. , Mills, K. F. , Satoh, A. & Imai, S. Age-associated loss of Sirt1-mediated enhancement of glucose-stimulated insulin secretion in β cell-specific Sirt1-overexpressing (BESTO) mice. Aging Cell 7, 78–88 (2008). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Satoh, A. et al. Sirt1 extends life span and delays aging in mice through the regulation of Nk2 homeobox 1 in the DMH and LH. Cell Metab. 18, 416–430 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bordone, L. et al. Sirt1 regulates insulin secretion by repressing UCP2 in pancreatic beta cells. PLoS Biol. 4, e31 (2006). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luu, L. et al. The loss of Sirt1 in mouse pancreatic beta cells impairs insulin secretion by disrupting glucose sensing. Diabetologia 56, 2010–2020 (2013). [DOI] [PubMed] [Google Scholar]
- Satoh, A. et al. SIRT1 promotes the central adaptive response to diet restriction through activation of the dorsomedial and lateral nuclei of the hypothalamus. J Neurosci. 30, 10220–10232 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Satoh, A. & Imai, S. Systemic regulation of mammalian ageing and longevity by brain sirtuins. Nat. Commun. 5, 4211 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang, G. et al. Hypothalamic programming of systemic ageing involving IKK-beta, NF-kappaB and GnRH. Nature 497, 211–216 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kawahara, T. L. et al. SIRT6 links histone H3 lysine 9 deacetylation to NF-kappaB-dependent gene expression and organismal life span. Cell 136, 62–74 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pais, T. F. et al. The NAD-dependent deacetylase sirtuin 2 is a suppressor of microglial activation and brain inflammation. EMBO J. 32, 2603–2616 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yeung, F. et al. Modulation of NF-kB-dependent transcription and cell survival by the SIRT1 deacetylase. EMBO J. 23, 2369–2380 (2004). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dilman, V. M. Age-associated elevation of hypothalamic threshold to feedback control, and its role in development, ageing, and disease. Lancet 1, 1211–1219 (1971). [DOI] [PubMed] [Google Scholar]
- Everitt, A. V. The hypothalamic-pituitary control of ageing and age-related pathology. Exp. Gerontol. 8, 265–277 (1973). [DOI] [PubMed] [Google Scholar]
- Conti, B. et al. Transgenic mice with a reduced core body temperature have an increased life span. Science 314, 825–828 (2006). [DOI] [PubMed] [Google Scholar]
- Khan, M. M. et al. Sympathetic innervation controls homeostasis of neuromuscular junctions in health and disease. Proc. Natl Acad. Sci. USA 113, 746–750 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karstoft, K. & Pedersen, B. K. Skeletal muscle as a gene regulatory endocrine organ. Curr. Opin. Clin. Nutr. Metab. Care 19, 170–175 (2016). [DOI] [PubMed] [Google Scholar]
- Demontis, F. , Piccirillo, R. , Goldberg, A. L. & Perrimon, N. The influence of skeletal muscle on systemic aging and lifespan. Aging Cell 12, 943–949 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Demontis, F. & Perrimon, N. FOXO/4E-BP signaling in Drosophila muscles regulates organism-wide proteostasis during aging. Cell 143, 813–825 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Demontis, F. , Patel, V. K. , Swindell, W. R. & Perrimon, N. Intertissue control of the nucleolus via a myokine-dependent longevity pathway. Cell Rep. 7, 1481–1494 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsai, S. et al. Muscle-specific 4E-BP1 signaling activation improves metabolic parameters during aging and obesity. J. Clin. Invest. 125, 2952–2964 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang, Y. et al. The starvation hormone, fibroblast growth factor-21, extends lifespan in mice. Elife 1, e00065 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Valdearcos, M. , Xu, A. W. & Koliwad, S. K. Hypothalamic inflammation in the control of metabolic function. Annu. Rev. Physiol. 77, 131–160 (2015). [DOI] [PubMed] [Google Scholar]
- Vandewalle, G. , Maquet, P. & Dijk, D. J. Light as a modulator of cognitive brain function. Trends Cogn. Sci. 13, 429–438 (2009). [DOI] [PubMed] [Google Scholar]
- Halberg, N. , Wernstedt-Asterholm, I. & Scherer, P. E. The adipocyte as an endocrine cell. Endocrinol. Metab. Clin. North Am. 37, 753–768, (2008). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liao, C. Y. , Rikke, B. A. , Johnson, T. E. , Diaz, V. & Nelson, J. F. Genetic variation in the murine lifespan response to dietary restriction: from life extension to life shortening. Aging Cell 9, 92–95 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liao, C. Y. et al. Fat maintenance is a predictor of the murine lifespan response to dietary restriction. Aging Cell 10, 629–639 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Calle, E. E. , Thun, M. J. , Petrelli, J. M. , Rodriguez, C. & Heath, C. W. Jr . Body-mass index and mortality in a prospective cohort of U.S. adults. New Engl. J. Med. 341, 1097–1105 (1999). [DOI] [PubMed] [Google Scholar]
- Hozawa, A. et al. Relationship between BMI and all-cause mortality in Japan: NIPPON DATA80. Obesity (Silver Spring) 16, 1714–1717 (2008). [DOI] [PubMed] [Google Scholar]
- Jee, S. H. et al. Body-mass index and mortality in Korean men and women. New Engl. J. Med. 355, 779–787 (2006). [DOI] [PubMed] [Google Scholar]
- Matsuo, T. et al. Age- and gender-specific BMI in terms of the lowest mortality in Japanese general population. Obesity (Silver Spring) 16, 2348–2355 (2008). [DOI] [PubMed] [Google Scholar]
- Seoane-Collazo, P. et al. Hypothalamic-autonomic control of energy homeostasis. Endocrine 50, 276–291 (2015). [DOI] [PubMed] [Google Scholar]
- Satoh, A. , Brace, C. S. , Rensing, N. & Imai, S. Deficiency of Prdm13, a dorsomedial hypothalamus-enriched gene, mimics age-associated changes in sleep quality and adiposity. Aging Cell 14, 209–218 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caton, P. W. , Kieswich, J. , Yaqoob, M. M. , Holness, M. J. & Sugden, M. C. Nicotinamide mononucleotide protects against pro-inflammatory cytokine-mediated impairment of mouse islet function. Diabetologia 54, 3083–3092 (2011). [DOI] [PubMed] [Google Scholar]
- Long, A. N. et al. Effect of nicotinamide mononucleotide on brain mitochondrial respiratory deficits in an Alzheimer's disease-relevant murine model. BMC Neurol. 15, 19 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yamamoto, T. et al. Nicotinamide mononucleotide, an intermediate of NAD+ synthesis, protects the heart from ischemia and reperfusion. PLoS ONE 9, e98972 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brandauer, J. et al. AMP-activated protein kinase regulates nicotinamide phosphoribosyl transferase expression in skeletal muscle. J. Physiol. Pharmacol. 591, 5207–5220 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Costford, S. R. et al. Skeletal muscle NAMPT is induced by exercise in humans. Am. J. Physiol. Endocrinol. Metab. 298, E117–E126 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koltai, E. et al. Exercise alters SIRT1, SIRT6, NAD and NAMPT levels in skeletal muscle of aged rats. Mech. Ageing Dev. 131, 21–28 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Canto, C. et al. The NAD(+) precursor nicotinamide riboside enhances oxidative metabolism and protects against high-fat diet-induced obesity. Cell Metab. 15, 838–847 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Imai, S. A possibility of nutriceuticals as an anti-aging intervention: Activation of sirtuins by promoting mammalian NAD biosynthesis. Pharmacol. Res. 62, 42–47 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bookout, A. L. et al. FGF21 regulates metabolism and circadian behavior by acting on the nervous system. Nat. Med. 19, 1147–1152 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mendias, C. L. et al. Haploinsufficiency of myostatin protects against aging-related declines in muscle function and enhances the longevity of mice. Aging Cell 14, 704–706 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]