Abstract
Objectives
To determine whether patients who are English proficient become aware of e-cigarettes through different marketing tactics and have dissimilar patterns of use than patients who are non-English speaking.
Design
This was a cross-sectional study surveying adult English- and Spanish-speaking patients. ANOVA and chi-squared tests were used to examine differences between groups.
Setting
A large public, safety-net hospital in Los Angeles County, California.
Results
Respondents (N=1899) were predominately Hispanic (78%), foreign-born (68%), and reported Spanish as a primary language (64%). Native English speakers reported the highest use of e-cigarettes (26%), followed by non-native (13%) and non-English speakers (2%) (P<.001). In terms of marketing, native and non-native English speakers were more likely to have friends and family as sources of e-cigarette information (P<.001). Native speakers were more likely to see advertisements for e-cigarettes on storefronts (P=.004) and on billboards (P<.001). Non-English speakers were most likely to learn about e-cigarettes on the news (P<.001) and in advertisements on the television and radio (P=.002). Differences in reasons for use were not significant between the three groups.
Conclusions
Native and non-native English speakers become aware of e-cigarettes through different mechanisms and use e-cigarettes at a significantly higher rate than non-English speakers. These results highlight an opportunity for public health programs to concentrate on specific channels of communication that introduce patient populations to e-cigarettes to slow the spread of e-cigarette usage.
Keywords: Electronic Cigarettes, Language, Public Health
Introduction
Electronic cigarettes are smokeless electronic vaporizers that deliver nicotine in aerosol form.1 They are battery-powered and use heat to vaporize tobacco. Replaceable cartridges contain nicotine that, once aerosolized, can be inhaled by the user. E-cigarettes come in several different shapes and sizes, including cigarettes, cigars, pipes, and mimics of everyday household objects.2 The tobacco industry has spent millions of dollars on acquiring and marketing e-cigarettes, and as many believe e-cigarettes use will lead to tobacco use, they have become a primary public health concern.3
The Food and Drug Administration has only recently established regulations on e-cigarettes, and more evidence is needed to evaluate for safety and smoking cessation effectiveness.4 Studies show that e-cigarettes contain widely varying amounts of chemical products in their vapor, indicating that the quality of these products is not adequately controlled.5,6 For example, known carcinogenic carbonyl compounds like formaldehyde and acetaldehyde have been detected in toxic levels in e-cigarette smoke.7 A 2014 Cochrane review suggested that e-cigarettes may be effective for smoking cessation, but confidence in the results remains low grade and a definitive recommendation cannot be made.8 Clearly, e-cigarettes are already making a large impact on health across the nation.
Recent literature has highlighted television advertisements, the internet, and word-of-mouth as common sources of e-cigarette information.9 Smokers of e-cigarettes in the general population report experimentation and smoking cessation as reasons for use.10,11 Nevertheless, there remains a lack of data regarding the epidemiology and use of e-cigarettes among Spanish-speaking and immigrant populations.
Invented in its current form in 2003, e-cigarettes are still a novel method of tobacco intake; its relative infancy on the international market may contribute to this current gap in research. Studies have suggested that e-cigarette awareness and use have increased over the last 10 years in the United States general and Hispanic populations and that smokers and former smokers are more likely to have been introduced to and used e-cigarettes than never-smokers.12 Some estimates believe that e-cigarettes will overtake combustible cigarettes in equivalent pack volume by as early as 2023.13
Our study seeks to expand on how English-speaking and non-English-speaking Hispanic adults first learn about e-cigarettes. The objective was to determine whether patients who are English proficient become aware of e-cigarettes through different marketing tactics and have dissimilar patterns of use than patients who are non-English speaking. Differentiating patterns in advertising and use by language may help us to understand how methods of advertising relate to eventual e-cigarette use.
Methods
Our cross-sectional study compared three adult patient populations within the Los Angeles County at the University of Southern California (LAC+USC) emergency department. Institutional review board approval was obtained prior to study initiation. We offered Spanish and English surveys to a consecutive sample of emergency department patients between 7 AM and 11 PM over a two-month period in summer 2014. Participants were included in the study if they were Hispanic and aged >18 years. Exclusion criteria were critical illness upon arrival and altered mental status or other inability to respond and provide informed consent.
After screening each participant, a 15-minute standardized questionnaire was distributed in electronic format on a handheld tablet. Survey questions were translated and back-translated between English and Spanish by native speakers in both languages. Questions included general demographics, primary language, e-cigarette awareness and use, e-cigarette marketing tactics, and e-cigarette reasons for use. E-cigarette images were distributed to assist with patient recollection. E-cigarette awareness was assessed through the question: “Have you heard of e-cigarettes or electronic cigarettes?” If the patient answered in the affirmative, the question was followed with, “How did you hear of e-cigarettes?” Different e-cigarette marketing tactics were included and patients were allowed to provide multiple answers. Participants were then asked if they had ever used an e-cigarette product, even one time. Patients were finally asked what their reasons for use were, with the option to give multiple answers. Several of these questions to assess e-cigarette use were adapted from the National Adult Tobacco Survey Questionnaire.14 In addition, to focus questioning on e-cigarettes, patients were asked to provide information on primary language spoken at home, age, sex, education, country of birth, chronic disease states, living situation, and zip code of residence, as these variables were known to be associated with tobacco use. We did not specifically ask about income as the vast majority of patients in our hospital live in neighborhoods under 138% of the poverty line.15
Statistics
ANOVA and chi square tests were utilized to examine differences between groups, with participants divided into native English speaking, non-native English speaking, and non-English speaking based on primary language spoken at home. Among the variables evaluated were patient demographics, smoking awareness, and smoking behavior. Preliminary analysis involved descriptive statistics and tests of linearity for all variables. Confounders were not yet adjusted for, but would have been controlled with stratification or multivariate regression analysis. Additionally, ANCOVA could have been employed as a means to utilize both ANOVA and linear regression models for the purpose of controlling potential confounding variables.
Results
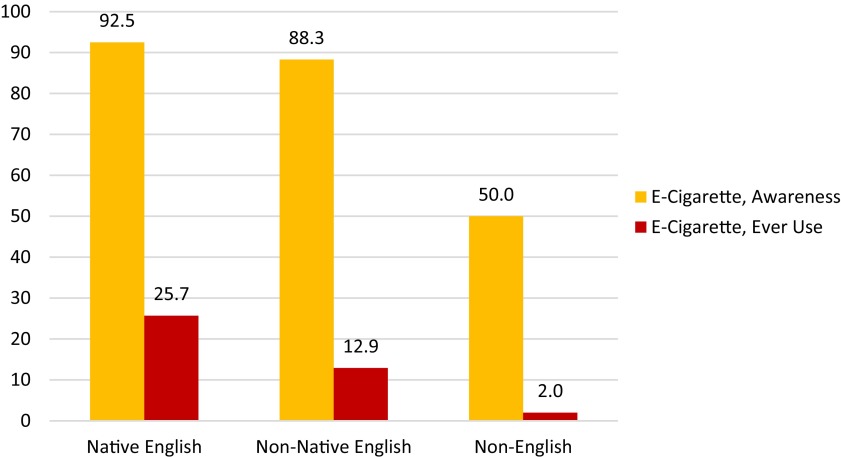
More than 5000 patients were screened, of which 2130 were eligible for consent. Of these, 1899 (89%) agreed to participate. An additional 423 were excluded, as they did not self-identify as being Hispanic. Respondents (N=1476) were 50.8% female with an average age of 46.6 (±14.5 SD). The majority of participants did not attend college (87.3%). More than 10% (11.1%) of patients reported current combustible cigarette use, 77.4% had heard of e-cigarettes, 7.6% had used an e-cigarette at least once, (Table 1) and 1.7% endorsed current e-cigarette use. Bivariate analysis between the three variables showed significant differences between native English speakers, non-native English speakers, and non-English speaking populations. Non-English speakers were older (40.1 years vs 39.9 years vs 50.5 years, P<.001), more likely to be female (41.3% vs 38.4% vs 57.1%, P<.001), less likely to have received some college education (33.0% vs 19.7% vs 4.9%, P<.001), and more likely to be foreign-born (24.6% vs 74.2% vs 99.3%, P<.001). Chronic disease prevalence was significant between the three groups, with native English-speaking populations more likely to have a greater number of chronic diseases (1.4 vs 1.2 vs 1.5, P=.005), a chronic heart problem (12.4% vs 6.6% vs 8.4%, P=.005), a chronic lung problem (9.9% vs 3.6% vs 5.3%, P<.001), and a chronic mental health disorder (12.3% vs 8.6% vs 7.9%, P=.045). Native English speakers were more likely to be current (22.0% vs 13.6% vs 7.3%, P<.001) or former combustible cigarette smokers (19.7% vs 17.1% vs 18.6%, P<.001). Figure 1 demonstrates differences in language populations in e-cigarette awareness and ever use. Native English speakers reported higher awareness (92.5% vs 88.3% vs 50.0%, P<.001) and ever use of e-cigarettes (25.7% vs 12.9% vs 2.0%, P<.001).
Table 1. Participant demographics.
| N=1476 | |
| Hispanic | 81.2% |
| Foreign-born | 77.4% |
| Spanish primary language | 81.7% |
| Total awareness and use | |
| E-cigarette awareness | 77.4% |
| E-cigarette use (current and former) | 7.6% |
| Prior tobacco use in e-cigarette current users | 84.0% |
Figure 1. Awareness and “ever use” by language.
Table 2 and Table 3 display sources where respondents obtained information about e-cigarettes, stratified by language groups. Native English speakers were more likely to find out about e-cigarettes through friends and family (56.4% vs 51.6% vs 36.8%, P<.000), whereas non-English speakers were more likely to find out about e-cigarettes through the news (10.7% vs 15.6% vs 19.2, P=.009). Advertisements were the main sources of e-cigarette information for all participant groups in our study (68.7% vs 73.6% vs 72.6%, P=.418). Among advertisements, more than one half came from TV and radio (53.9% vs 56.8% vs 64.5%, P=.006). Storefronts (25.9% vs 29.2% vs 19.2%, P=.002), billboards (16.5% vs 22.8% vs 12.4%, P<.001), and the internet (11.1% vs 12.0% vs 5.4%, P=.001) showed differences in significance as points of information access between the three groups. Although not statistically significant, all three language populations received a large amount of e-cigarette exposure through advertisements within their own neighborhood (60.1% of all participants).
Table 2. Sources of e-cigarette information among three patient populations.
| Source of e-cigarette information | Native English | Non-Native English | Non-English | P |
| Friends/family | 56.4 | 51.6 | 36.8 | .000 |
| News | 10.7 | 15.6 | 19.2 | .009 |
| Advertisement | 68.7 | 73.6 | 72.6 | .418 |
| Other | 4.5 | 2.4 | 2.2 | .146 |
Table 3. E-cigarette awareness through advertisements among three patient populations.
| Awareness from advertisements | Native English | Non-Native English | Non-English | P |
| TV/radio | 53.9 | 56.8 | 64.5 | .006 |
| Newspaper/magazine | 10.3 | 14.0 | 10.4 | .266 |
| Storefront | 25.9 | 29.2 | 19.2 | .002 |
| Billboard/building/transportation | 16.5 | 22.8 | 12.4 | .001 |
| Internet | 11.1 | 12.0 | 5.4 | .001 |
| Cell phone / text messaging/apps | 2.5 | 2.0 | 1.1 | .279 |
| Advertisements in neighborhood | 53.8 | 60.4 | 63.2 | .371 |
As displayed in Table 4, reasons for use were not statistically significant between groups. Reasons for use included recreational, to try something new, to reduce or quit tobacco smoking, to avoid harmful tobacco materials, and few e-cigarette regulations, among others. The most common reasons for use were experimentation (try something new) (58.9% of all participants) and smoking cessation (25.0% of all participants).
Table 4. Reasons for use among three patient populations.
| Awareness from advertisements | Native English | Non-Native English | Non-English | P |
| Recreational | 17.7 | 18.8 | 22.2 | .912 |
| Try something new | 56.5 | 71.9 | 44.4 | .140 |
| Reduce/quit tobacco smoking | 25.8 | 18.8 | 33.3 | .508 |
| Avoid harmful tobacco materials | 8.1 | 9.4 | 5.6 | .892 |
| Few e-cigarette regulations | 1.6 | 0.0 | 5.6 | .359 |
| Other | 6.5 | 3.1 | 5.6 | .794 |
Discussion
Native and non-native English speakers become aware of e-cigarettes through different mechanisms and use e-cigarettes at a significantly higher rate than non-English speakers. Both native and non-native English speakers tend to learn about e-cigarettes from close acquaintances, as opposed to non-English speakers, who learn about e-cigarettes more from news outlets, television, and radio. Differences in overall awareness in groups may be due to several factors, including friends and family who smoke and exposure to outlets selling e-cigarettes, which tend to cluster in high income neighborhoods with fewer ethnic minorities.9
Marketing is used by the tobacco industry to influence consumer demand for products, and as such, there is the potential for marketing to influence smoking behaviors.1,16,17 E-cigarette marketing is crucial for manufacturing companies, as these products are unfamiliar to the potential user and many appear similar to the point that branding is necessary for differentiation.17,18 Previous literature has shown a substantial relationship between advertising and combustible cigarette smoking, especially involving the initiation of smoking.1,19 There is great concern that a similar relationship has already evolved with e-cigarettes.
E-cigarettes receive much of their marketing in the form of television commercials, internet advertisements, and as retailer point-of-sale promotions.1 Television commercials are unique in that they were traditionally unavailable for tobacco companies due to regulations set forth by the Food and Drug Administration.20,21 E-cigarette companies are able to individualize sales over the internet, where they interact with buyers through direct-to-consumer marketing and social media websites like Twitter and Facebook.20,22,23
Advertisements are a primary source of e-cigarette information for consumers, and new research suggests that advertising has influenced consumer perceptions of harm, likely increasing use.24 Trumbo and Kim looked at e-cigarette marketing to young adults, who became significantly more receptive to experimentation with the product following exposure to television advertising.25 Additionally, a study involving the 2011 National Youth Tobacco Survey revealed a significant exposure-response relationship between prolonged contact with e-cigarette advertising and use.26
Following advertising, the most common source for e-cigarette information in our study was friends and family. This is consistent with previous studies and highlights an opportunity to increase patient education to guide day-to-day conversations. Hall et al described that almost one third of smokers recommended e-cigarettes as a form of smoking cessation to their peers.27 Word-of-mouth is an important way for smokers to share information about products. By targeting forms of interpersonal communication, public health programs can provide more robust dialogue on safety and smoking cessation efficacy.
Previous studies have looked at cigarette smoking in Spanish-speaking populations.28,29 Our non-English speaking population was Hispanic, reflecting the Center for Disease Control’s estimate that non-Hispanics are more likely to smoke than Hispanics.30 Respondents in our study showed greater e-cigarette “ever use” rate than national Hispanic rates; however, this number was still lower than the national average (7.6% vs 8.5%).12 Current and former smoking status, being male, English language, and younger age were all significantly associated with e-cigarette use. Participants who were foreign-born and non-English speaking at home demonstrated much lower levels in e-cigarette “ever use” – this parallels another similar study on Hispanic populations, which showed that cultural buffering may serve as a protective factor against e-cigarette use.31
There are several limitations to our study. We were unable to provide questionnaires for patients who could not speak English or Spanish; thus, non-English speakers in the study were almost exclusively Latino or Hispanic. Respondents did not receive questionnaires between 11PM and 7AM, which may have inadvertently excluded populations of patients that arrived and were discharged overnight. However, we have no reason to believe these patients would be systematically different than those approached during study hours. Our study took place over two months with sampling from one emergency department, overall limiting generalizability. That being said, LAC+USC is the largest public emergency department in the nation seated in the center of highly diverse Los Angeles County. Because this is a cross-sectional study, we cannot conclude whether different forms of e-cigarette exposure resulted in different patterns of use – we can only determine prevalence within the three populations. In order to determine true significance, we will need to adjust for possible confounding variables including age, sex, race, income, education, and smoking status. Finally, as this is a preliminary analysis we did not control for potential confounders such as level of education, age and sex.
Conclusion
These findings show that English speakers and non-English speakers have distinctive patterns of e-cigarette awareness and use. This is especially pertinent in our low-income, urban, safety-net Hispanic population – one historically susceptible to tobacco use.32 Even as full regulations on advertising begin to take effect, continued exposure to e-cigarette marketing tactics may adversely influence perceptions of product safety and efficacy in smoking cessation. By providing culturally sensitive interventions that more effectively target vulnerable populations, we can increase education on safety and mitigate harmful usage.
Acknowledgments
The authors would like to acknowledge the students who participated in the LAC+USC emergency department summer research program: Rochelle Fayngor, Mark Zhang, Joshua Lee, Erin Higginbotham, Zachary Carriker, Sarah Wood, Victor Wang, Pooja Jaeel, Kunal Shah, Brittany Docherty, Kevin Hanley, Melissa Luttio, Ryan McCormick, Sana Ahmed, Sasha Lieblein, Kevin Chen, Melanie Hertenian, Janice Rivelle, Nihaal Shah.
References
- 1. U.S. Department of Health and Human Services E-Cigarette Use Among Youth and Young Adults: A Report of the Surgeon General—Executive Summary. Atlanta, GA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 2016. [Google Scholar]
- 2. Zhu SH, Sun JY, Bonnevie E, et al. . Four hundred and sixty brands of e-cigarettes and counting: implications for product regulation. Tob Control. 2014;23(suppl 3):iii3-iii9. 10.1136/tobaccocontrol-2014-051670 10.1136/tobaccocontrol-2014-051670 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Kornfield R, Huang J, Vera L, Emery SL. Rapidly increasing promotional expenditures for e-cigarettes. Tob Control. 2015;24(2):110-111. 10.1136/tobaccocontrol-2014-051580 10.1136/tobaccocontrol-2014-051580 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. U.S. Food and Drug Administration Deeming tobacco products to be subject to the Federal Food, Drug, and Cosmetic Act, as amended by the Family Smoking Prevention and Tobacco Control Act, 2016. Last accessed Jan 8, 2017 from http://www.fda.gov/TobaccoProducts/Labeling/RulesRegulationsGuidance/ ucm39 [PubMed]
- 5. Sleiman M, Logue JM, Montesinos VN, et al. . Emissions from electronic cigarettes: key parameters affecting the release of harmful chemicals. Environ Sci Technol. 2016;50(17):9644-9651. 10.1021/acs.est.6b01741 [DOI] [PubMed] [Google Scholar]
- 6. Bekki K, Uchiyama S, Ohta K, Inaba Y, Nakagome H, Kunugita N. Carbonyl compounds generated from electronic cigarettes. Int J Environ Res Public Health. 2014;11(11):11192-11200. 10.3390/ijerph111111192 10.3390/ijerph111111192 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Jensen RP, Luo W, Pankow JF, Strongin RM, Peyton DH. Hidden formaldehyde in e-cigarette aerosols. N Engl J Med. 2015;372(4):392-394. 10.1056/NEJMc1413069 [DOI] [PubMed] [Google Scholar]
- 8. McRobbie H, Bullen C, Hartmann-Boyce J, Hajek P. Electronic cigarettes for smoking cessation and reduction. Cochrane Database Syst Rev. 2014;(12):CD010216. 10.1002/14651858.CD010216.pub2 [DOI] [PubMed] [Google Scholar]
- 9. Pepper JK, Emery SL, Ribisl KM, Brewer NT. How U.S. adults find out about electronic cigarettes: implications for public health messages. Nicotine Tob Res. 2014;16(8):1140-1144. 10.1093/ntr/ntu060 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Dutra LM, Glantz SA High international electronic cigarette use among never smoker adolescents. J Adolesc Health. 2014;55(5):595- 597. https://doi.org/ 10.1016/j.jadohealth. 2014.08.010. PMID:25344030. [DOI] [PMC free article] [PubMed]
- 11. Pepper JK, Ribisl KM, Emery SL, Brewer NT. Reasons for starting and stopping electronic cigarette use. Int J Environ Res Public Health. 2014;11(10):10345-10361. 10.3390/ijerph111010345 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. King BA, Patel R, Nguyen KH, Dube SR. Trends in awareness and use of electronic cigarettes among US adults, 2010-2013. Nicotine Tob Res. 2015;17(2):219-227. 10.1093/ntr/ntu191 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Herzog B, Gerberi J. E-Cigs Revolutionizing the Tobacco Industry. Equity Research Report, Wells Fargo Securities, LLC. June 6, 2013. Last accessed on May 25, 2017 from http://www.smallcapfinancialwire.com/wp-content/uploads/2013/11/E-Cigs-Revolutionizing-the-Tobacco-Industry-Interactive-Model.pdf
- 14. King BA, Dube SR, Tynan MA. Current tobacco use among adults in the United States: findings from the National Adult Tobacco Survey. Am J Public Health. 2012;102(11):e93-e100. 10.2105/AJPH.2012.301002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Bishaw A. Areas with concentrated poverty: 2006–2010. American Community Survey Briefs. United States Census Bureau; 2011. [Google Scholar]
- 16. DiFranza JR, Richards JW, Paulman PM, et al. . RJR Nabisco’s cartoon camel promotes camel cigarettes to children. JAMA. 1991;266(22):3149-3153. 10.1001/jama.1991.03470220065028 [DOI] [PubMed] [Google Scholar]
- 17. National Cancer Institute The Role of the Media in Promoting and Reducing Tobacco Use. Smoking and Tobacco Control Monograph No. 19. Bethesda (MD): U.S. Department of Health and Human Services, National Institutes of Health, National Cancer Institute, 2008. NIH Publication No. 07-6242. [Google Scholar]
- 18. Sethuraman R, Tellis GJ, Briesch RA. How well does advertising work? Generalizations from meta-analysis of brand advertising elasticities. J Mark Res. 2011;48(3):457-471. 10.1509/jmkr.48.3.457 [DOI] [Google Scholar]
- 19. Biener L, Siegel M. Tobacco marketing and adolescent smoking: more support for a causal inference. Am J Public Health. 2000;90(3):407-411. 10.2105/AJPH.90.3.407 10.2105/AJPH.90.3.407 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Ganz O, Cantrell J, Moon-Howard J, Aidala A, Kirchner TR, Vallone D. Electronic cigarette advertising at the point-of-sale: a gap in tobacco control research. Tob Control. 2015;24(e1):e110-e112. 10.1136/tobaccocontrol-2013-051337 [DOI] [PubMed] [Google Scholar]
- 21. Legacy for Health Vaporized: E-Cigarettes, Advertising, and Youth. Washington, DC: Legacy for Health; 2014. [Google Scholar]
- 22. Huang J, Kornfield R, Szczypka G, Emery SL. A cross-sectional examination of marketing of electronic cigarettes on Twitter. Tob Control. 2014. a;23(suppl 3):iii26-iii30. 10.1136/tobaccocontrol-2014-051551 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Richardson A, Ganz O, Stalgaitis C, Abrams D, Vallone D. Noncombustible tobacco product advertising: how companies are selling the new face of tobacco. Nicotine Tob Res. 2014;16(5):606-614. 10.1093/ntr/ntt200 10.1093/ntr/ntt200 [DOI] [PubMed] [Google Scholar]
- 24. Pepper JK, Emery SL, Ribisl KM, Southwell BG, Brewer NT. Effects of advertisements on smokers’ interest in trying e-cigarettes: the roles of product comparison and visual cues. Tob Control. 2014;23(suppl 3):iii31-iii36. 10.1136/tobaccocontrol-2014-051718 10.1136/tobaccocontrol-2014-051718 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Trumbo CW, Kim SJ. The effect of electronic cigarette advertising on intended use among college students. Addict Behav. 2015;46:77-81. https://doi.org/ 10.1016/j addbeh.2015.03.005. PMID:25827334. [DOI] [PubMed]
- 26. Agaku IT, Ayo-Yusuf OA. The Effect of Exposure to Pro-Tobacco Advertising on Experimentation With Emerging Tobacco Products Among U.S. Adolescents. Health Educ Behav. 2014;41(3):275-280. 10.1177/1090198113511817 [DOI] [PubMed] [Google Scholar]
- 27. Hall MG, Pepper JK, Morgan JC, Brewer NT. Social Interactions as a Source of Information about E-Cigarettes: A Study of U.S. Adult Smokers. Int J Environ Res Public Health. 2016;13(8):E788. 10.3390/ijerph13080788 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Allen ML, Elliott MN, Fuligni AJ, Morales LS, Hambarsoomian K, Schuster MA. The relationship between Spanish language use and substance use behaviors among Latino youth: a social network approach. J Adolesc Health. 2008;43(4):372-379. 10.1016/j.jadohealth.2008.02.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Maher JE, Boysun MJ, Rohde K, et al. . Are Latinos really less likely to be smokers? Lessons from Oregon. Nicotine Tob Res. 2005;7(2):283-287. 10.1080/14622200500056259 [DOI] [PubMed] [Google Scholar]
- 30. Agaku IT, King BA, Husten CG, et al. ; Centers for Disease Control and Prevention (CDC) . Tobacco product use among adults--United States, 2012-2013. MMWR Morb Mortal Wkly Rep. 2014;63(25):542-547. [PMC free article] [PubMed] [Google Scholar]
- 31. Lam CN, Goldenson NI, Burner E, Unger JB. Cultural buffering as a protective factor against electronic cigarette use among Hispanic emergency department patients. Addict Behav. 2016;63:155-160. 10.1016/j.addbeh.2016.07.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Cantrell J, Anesetti-Rothermel A, Pearson JL, Xiao H, Vallone D, Kirchner TR. The impact of the tobacco retail outlet environment on adult cessation and differences by neighborhood poverty. Addiction. 2015;110(1):152- 161. https://doi.org/ 10.1111/add.12718. PMID:25171184.4909.htm [DOI] [PMC free article] [PubMed]