Abstract
This article reviews the development of the hepatopancreatobiliary (HPB) endoscopic ultrasound (EUS) service at Freeman Hospital and seeks to identify from our experience learning points for good practice and pitfalls to avoid. The Freeman HPB EUS service has expanded rapidly over the past 10 years in response to the consolidation of cancer care and aligned to the needs of the cancer network. Effective multidisciplinary teamwork and increased subspecialisation by the endosonographers has allowed the efficient use of capacity and development of skills. Mechanisms for monitoring diagnostic performance put in place at the outset of the EUS–fine needle aspiration programme have helped to identify interventions that have led to improved test performance. An excellent working relationship between all stakeholders is critical to the success of such a service as is a preparedness to seek and respond to the views of patients and referrers.
Introduction
The endoscopic ultrasound (EUS) service at Freeman Hospital, Newcastle upon Tyne, was developed with a pancreatobiliary focus as part of the regional hepatopancreatobiliary (HPB) unit which serves the North of England Cancer Network (population 3.3 million). Large changes in the provision of pancreatic and complex biliary surgery in the UK in the past 10 years have resulted in centralisation of pancreatic malignancy in specialist centres serving a population of 2–4 million. These changes have had a major impact on referral patterns in the North East region. In 1997, there were 10 hospitals in the North East performing pancreatic resections. Since 2003, the HPB unit at Freeman Hospital has been the only hospital performing complex biliary surgery and pancreatic resections, with a consequent marked increase in referrals (figure 1) and surgery (figure 2). This consolidation of pancreatic cancer care was used as a driver for investment and improvement in the HPB EUS service. Radial EUS was introduced to the unit in 1996 by a surgeon (RMC) and the service was subsequently supported by a radiologist (DLR). By 2001 it was recognised that greater capacity was required to accommodate the increase in pancreatic cancer referrals. A dedicated EUS list was created on which KWO received training from DLR. Linear EUS and EUS guided fine needle aspiration (FNA) were then identified as priorities. Following a short sabbatical by KWO at a high volume pancreatic EUS centre (Massachusetts General Hospital) to observe linear EUS in October 2002, a successful business case (supported by the medical, surgical, radiology and cardiothoracic directorates) was made in early 2003 for the purchase of a Hitachi ultrasound workstation, two electronic linear and one electronic radial echoendoscope. The decision was taken to use linear EUS preferentially for all pancreatobiliary EUS procedures thereby enabling staging and tissue sampling in one procedure. A small number of mediastinal EUS–FNA are performed in support of the cardiothoracic unit. Oesophagogastric EUS examinations are performed at the Northern Oesphago Gastric Unit at the Royal Victoria Infirmary.
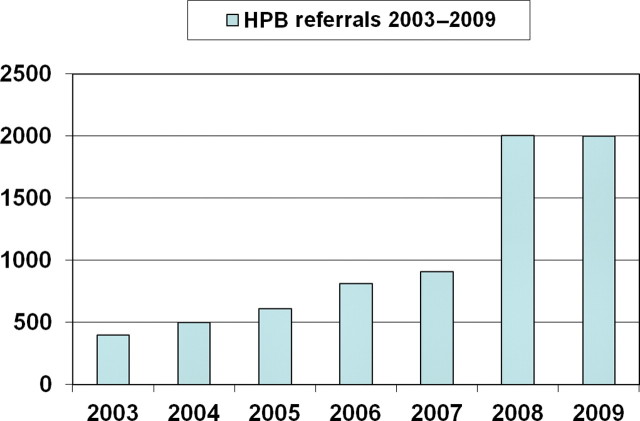
Figure 1.
Referrals to the hepatopancreatobiliary (HPB) multidisciplinary team between 2003 and 2009.
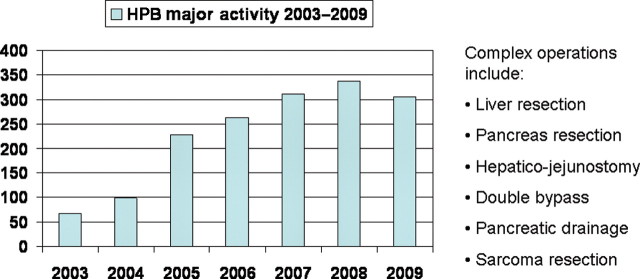
Figure 2.
Hepatopancreatobiliary (HPB) unit complex surgery between 2003 and 2009.
The HPB team
The HPB team of surgeons, physicians, radiologists, oncologists, specialist nurses and dedicated administrative staff function as a cohesive group. The development and rapid growth of the EUS service, both diagnostic and therapeutic, has been built on the encouragement and strong support of other team members. Suspected cancer cases are predominantly accepted as generic referrals and patients are allocated to a consultant based on current workload, waiting times and, where relevant, subspecialist interest. To minimise waiting, appropriately screened patients may at this stage of the referral process be booked directly for EUS before being seen by a surgeon or physician. In such cases, where possible, the patient will be seen by the nurse specialist and/or responsible consultant at the time of EUS. There has been a substantial increase in both malignant and benign referrals to the unit from approximately 400 a year in 2003 to 2000 in 2008 (figure 1), with a concomitant increase in complex HPB surgery (figure 2). There is a clear recognition by all colleagues of the need to focus expertise to maximise skills. This supportive and cooperative working environment has proved fruitful to innovations in endoscopic practice and the growth of the service.
Evolution of the service
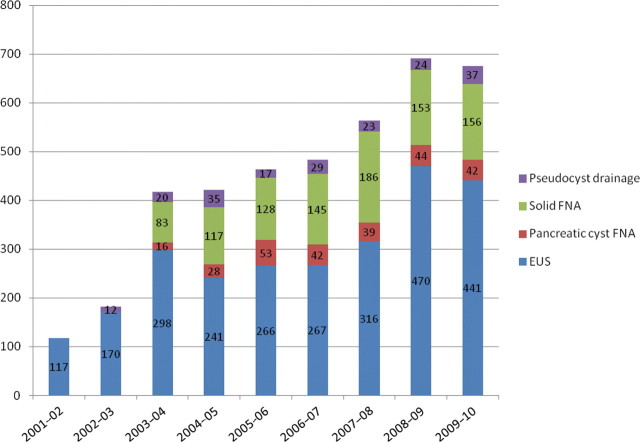
The service has developed rapidly (figure 3) from performing 117 diagnostic radial EUS per year in 2001/2002 to a total of 676 (almost entirely linear EUS) in 2009/2010, comprising 441 EUS, 198 EUS–FNA and 37 EUS guided drainage of pancreatic fluid collections.
Figure 3.
Pancreatobiliary endoscopic ultrasound (EUS) procedures between 2001 and 2010. FNA, fine needle aspiration.
It has gone from provision by a single endosonographer with only one dedicated diagnostic list between 2003 and 2007 resulting in long waiting times and ad hoc extra lists to a two provider four list service currently.
The present model is provision of EUS by pancreatobiliary physicians who perform the full range of EUS guided intervention in addition to advanced endoscopic retrograde cholangiopancreatography (ERCP) (sphincter of Oddi manometry, SpyGlass cholangioscopy, electrohydraulic lithotripsy and intraductal ultrasound) thus allowing the complementary nature of these two imaging and therapeutic procedures to be fully exploited. In a proportion of cases, ERCP and EUS are performed sequentially under the same sedation, thereby enabling rapid diagnosis, staging, tissue sampling and stenting of an obstructed biliary tree in the same procedure.1
Following a successful business case highlighting the difficulties of a single handed service, the work already done to maximise capacity, the need to reduce waiting times and the significant revenue generated by the EUS service, a colleague (MN) was appointed in October 2007 and a further investment in equipment made. Neither endosonographer does general internal medicine. Giving up general internal medicine and focusing on pancreatobiliary medicine and endoscopy has facilitated the rapid development of the service.
List provision has recently increased from three to four lists for diagnostic procedures (EUS and EUS–FNA), and four, shortly to be five, ERCP lists are available for therapeutic EUS guided procedures that require screening. A successful bid was made to the League of Friends in September 2010 for funding to purchase a new £100 000 state of the art ultrasound workstation to augment the service.
Optimising efficiency and working with the team
The demand for HPB EUS has increased rapidly in recent years. We have sought to develop and maintain an efficient high quality service by working flexibly to optimise the use of capacity, monitoring and responding to performance indicators, such as the diagnostic accuracy of EUS–FNA, and seeking patient and referrer feedback through surveys.
To ensure prompt EUS for staging and/or tissue diagnosis, a number of slots on the EUS lists are ring fenced for direct booking following multidisciplinary team (MDT) discussion. Cross cover arrangements are in place between KWO and MKN to ensure that very few EUS lists are lost through the year. Leave is coordinated to avoid simultaneous absences. An adjustment to work patterns can be made, including a new weekly screening list covered by KWO and MKN on alternate weeks without extra remuneration.
All suspected cases of malignancy, however referred, are channelled through the MDT. A significant part of the EUS workload, however, involves benign referrals from across the region and further afield. Where possible (clear indication and a fully informed patient), such patients are brought in directly for EUS and other imaging if necessary. For all patients, the EUS report is communicated as part of the overall management plan to the patient, referring consultants and general practitioner. A recent patient satisfaction survey found that 94% of patients felt well informed about the procedure and 96% had tolerated it well.
In order to involve our referrers in identifying areas for improvement of the service, a user survey was performed in September 2010. A short email questionnaire was sent to all 66 medical gastroenterologists in the region soliciting their views and a reminder was sent after 2 weeks; 20 responses were received from 11 hospitals. Some responses were made on behalf of the whole unit.
All respondents felt that they had a good understanding of the role of EUS in HBP disease; 50% felt that the waiting times (6 weeks for routine and 2 weeks for urgent cases) were appropriate but 50% felt that this was too long for both. Fifty-eight per cent wanted more information on procedures performed and indications and 58% felt that results were not communicated in a timely manner. Responses included ‘faster if possible’, ‘not always… can results be faxed or emailed?’, ‘sometimes a delay’. There was a consensus for shorter waiting times and better communication. The recent addition of a new diagnostic list and the imminent introduction of a further screening list should address the issue of waiting times. We aim to see urgent cases within a week and routines within a month. To improve communication, a copy report and letter will be faxed to the referring consultant and general practitioner in all cases within 3 days of the procedure. Referral guidelines for benign disease are being produced in cooperation with a referring physician.
Teaching and training
EUS is a specialised and complex procedure with the emphasis on the interpretation of ultrasound, an imaging modality with which most non-radiologists have very little experience. As such it requires specific training and has a substantial learning curve. The British Society of Gastroenterology (BSG) published guidelines on EUS training in 20052 and a BSG working party has recently produced detailed recommendations for service provision and training.3 Successful procedural outcome is dependent not only on the endosonographer but also on the endoscopy nurses and, for EUS–FNA, the role of the cytopathologist is fundamental.
A fellowship in pancreaticobiliary medicine was established in October 2003 at Freeman Hospital. This offers training to a senior trainee in all aspects of pancreaticobiliary medicine, including advanced ERCP and EUS. This is a nationally advertised fellowship and has attracted applicants both nationally and internationally. Only trainees who have already completed at least 1 or preferably 2 years of ERCP training and have achieved competence in grade 1 ERCP with a procedural success rate of greater than 80% are considered. Prior exposure to EUS is advantageous but not essential. The majority of appointees to date have been post-CCT (certificate of completion of training).
During the fellowship, the trainee has sole training access to three ERCP lists and three EUS lists a week. The trainee also attends the malignant MDT meeting and two specialist pancreatobiliary outpatient clinics. The emphasis is on MDT work and training; the trainee also has the option to attend a surgical pancreatic clinic as well as ward rounds on the HPB surgical ward.
During this 1 year training period the trainee achieves as a minimum competence in diagnostic radial and linear EUS, mediastinal and pancreaticobiliary FNA as well as exposure to therapeutic EUS (eg, pseudocyst drainage and transmural endoscopic necrosectomy). Our most recent trainee performed 320 EUS procedures of which 120 were EUS–FNA and 20 EUS guided drainage procedures during the year's fellowship.
A comparison of pancreatic EUS–FNA accuracy at the outset of independent practice from our unit4 has documented a significant difference in diagnostic accuracy (56% vs 75%; p<0.05) between commencing EUS–FNA without completing a formal training programme and after formal training.
With regard to endoscopy nurse training, an annual national training course for nurses involved in ERCP and EUS has proved very popular and is in its third year.5 A review article for endoscopy nurses has been published recently.6
Research audit and innovation
From the outset of the service there has been a commitment to monitoring outcomes, and continuous quality assessment has been undertaken to assist service improvement. Audit of outcomes is integral to ensuring an effective high quality service; it informs any discussion about service improvement and can support the argument for investment. A prospective database has been maintained of all EUS FNA procedures since the inception of the service in April 2003. Currently there are over 800 cases of FNA of solid lesions and in excess of 300 cystic lesions of the pancreas on the database. Monitoring of outcome data, including satisfactory aspirate rate and diagnostic performance, has led to simple interventions such as increasing the number of needle passes as well as the introduction of liquid based cytology. It also enabled a cogent and ultimately successful business case to be made for the introduction of an onsite cytopathology technician to reduce the unsatisfactory aspirate rate. This attention to detail has contributed to an improvement in the diagnostic accuracy for solid lesions of the pancreas from 56% in 20034 at the start of the service to 75%1 in 2007, 85% in 2008 and 92% at the end of 2009.
Finding time to initiate and perform research while developing the service proved challenging. Our initial work has taken the form of retrospective database studies.1 4 7 8 Comparative studies to better delineate the role of EUS is an ongoing unit interest. An early study comparing EUS to spiral CT was performed at Freeman Hospital9; more recently, we have compared multislice CT with EUS.10
In a recent retrospective study, we compared EUS–FNA versus biliary brushings and performed an assessment of their simultaneous performance in jaundiced patients with suspected malignant obstruction.1 Combining both procedures under the same conscious sedation was feasible, improved diagnostic accuracy and had a complication rate similar to ERCP alone. Database studies of EUS–FNA performance characteristics in the diagnosis of proximal biliary strictures7 and suspected neoplastic cysts8 have also been undertaken.
The close multidisciplinary working, and surgical support, has led to the development of innovative procedures such as EUS guided drainage of obstructed hepaticojejunostomy loop.11 Our group have been early proponents of the role of aggressive EUS guided drainage in the management of infected pancreatic necrosis.12 We and others have shown that EUS guided transmural endoscopic necrosectomy in selected patients allows safe and effective debridement of infected necrotic debris in very sick individuals in whom surgical intervention would carry a high risk.
Advice for a new service
The recent BSG guidelines on service provision and training3 are a very useful source of information. They recommend that an EUS service is commissioned under the auspices of the cancer network. The guidelines highlight that while a significant proportion of the pancreaticobiliary EUS workload will be benign, the knowledge and skills required to provide a high quality benign EUS service are those that are required for assessment of malignant disease and are unlikely to be performed separately. Pancreaticobiliary EUS is challenging with a long learning curve, and the provision of a high quality effective service requires a focus on acquiring and maintaining these skills. The service should be commissioned with a clear understanding of the demand to be met and provided by individuals who have completed an appropriate training programme. Our tips for success are as follows:
-
■
Assess the need for the service in terms of local referrals and the HPB cancer centre; although there are significant benign indications, the driver for EUS remains cancer care and a solely benign workload may be difficult to sustain.
-
■
Appoint an individual who has completed an appropriate period and volume of training according to BSG guidelines. Learning EUS on the job (a previous necessity) is no longer appropriate.
-
■
Cancer staging and complex benign cases should be performed within the HPB centre.
-
■
Liaise closely and early with your cytopathologists—this relationship is crucial to the success of your EUS–FNA.
-
■
Institute monitoring of key performance indicators—for example, EUS–FNA accuracy, staging accuracy, procedural completion and complication rate—from the outset.
-
■
Ensure surgical support before embarking on EUS guided interventional therapy.
-
■
Consider applications to charitable bodies for equipment funding.
-
■
A good working relationship between stakeholders (surgeons, gastroenterologists and radiologists) is critical, irrespective of which specialty delivers the service.
-
■
A large HPB cancer centre will require at least two practitioners. Trying to run a service with one EUS endoscopist puts a large amount of pressure on that individual.
-
■
Skills accrue fastest and are best maintained with volume.
Conclusion
The development of a comprehensive large volume pancreatobiliary EUS programme at Freeman Hospital has been a multidisciplinary effort, initiated by surgeons, sustained by a radiologist and further developed and expanded by gastroenterologists. We believe that such unity of purpose allied to quality assurance measures and a preparedness to seek and respond to patient and referrer feedback is central to delivering a flexible high quality service.
Footnotes
Competing interests: None.
Provenance and peer review: Commissioned; externally peer reviewed.
References
- 1.Oppong K, Raine D, Nayar M, et al. EUS-FNA versus biliary brushings and assessment of simultaneous performance in jaundiced patients with suspected malignant obstruction. JOP 2010;11:560–7. [PubMed] [Google Scholar]
- 2.Carroll N, Penman I. UK/Ireland EUS Users' Group: Recommendations for Training in Endoscopic Ultrasound, 2004. Glasgow: BSG; http://www.bsg.org.uk (accessed October 2010). [Google Scholar]
- 3.Meenan J, Penman I, Carroll N, et al. Service provision and training for endoscopic ultrasound (EUS) in the UK. Front Gastroenterol 2011. (in press). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Manu N, Diamond J, Wadehra V, et al. Effect of formal training on achieving competence in EUS FNA of solid pancreatic lesions. Endoscopy 2009;41Suppl 1:A377. [Google Scholar]
- 5.Nayar M, Nicholson G, Gray H, et al. The 1st Newcastle ERCP & EUS course for nurses. GI Nursing 2010;8:36–40. [Google Scholar]
- 6.Leeds JS, Diamond J, Nayar MK. Role of endoscopic ultrasound in pancreaticobiliary disorders. GI Nursing 2010;8:43–9. [Google Scholar]
- 7.Nayar MK, Manas DM, Wadehra V, et al. Role of EUS and EUS guided FNA in the management of proximal biliary strictures. Hepatogastroenterology 2011. (in press). [DOI] [PubMed] [Google Scholar]
- 8.Oppong KW, Elamin K, Nayar M, et al. Linear EUS and EUS-FNA in the diagnosis of pancreatic cystic lesions in a single tertiary referral centre. Gut 2009;58Suppl I:A1–156.19307448 [Google Scholar]
- 9.Midwinter MJ, Beveridge CJ, Wilsdon JB, et al. Correlation between spiral computed tomography, endoscopic ultrasonography and findings at operation in pancreatic and ampullary tumours. Br J Surg 1999;86:189–93. [DOI] [PubMed] [Google Scholar]
- 10.Mansfield SD, Scott J, Oppong K, et al. Comparison of multislice computed tomography and endoscopic ultrasonography with operative and histological findings in suspected pancreatic and periampullary malignancy. Br J Surg 2008;95:1512–20. [DOI] [PubMed] [Google Scholar]
- 11.Chatterjee S, Ibrahim B, Charnley RM, et al. Endoscopic ultrasound guided gastroenterostomy for palliative drainage of an obstructed hepatico-jejunostomy loop. Endoscopy 2011. (in press). [DOI] [PubMed] [Google Scholar]
- 12.Charnley RM, Lochan R, Gray H, et al. Endoscopic necrosectomy as primary therapy in the management of infected pancreatic necrosis. Endoscopy 2006;38:925–8. [DOI] [PubMed] [Google Scholar]