Abstract
Introduction
Quality of health services depend on the entire medical team. A supportive team culture and effective leadership is required for successful quality assurance (QA). The opinion of endoscopy personnel towards QA is unknown, while they have to collaborate in many quality projects.
Methods
A survey was sent to all endoscopy nurses, assistants and managers. It focused on the implementation of a QA programme. Further, a team assessment was included, focusing on leadership and team functioning, using scores on 5-point Likert scales, with 1 being a very positive opinion, and 5 being a very negative opinion towards the item.
Results
294 persons completed the questionnaire (44%). 87% expressed a positive attitude towards a QA programme, and 54% thought that the implementation of a nationwide QA programme for endoscopy would be feasible. Positive effects of QA were expected on publicity (62%) and overall quality (70%). Most important QA aspects were aftercare (97%) and patient experiences (96%). Concerns were raised about the time investment (18%) and disclosure of results towards media (24%). Team assessment showed good scores on `team working' with a mean score of 1.97. Lower scores were given to the `wider organization' (3.00) and `team process' (2.42).
Conclusion
Endoscopy personnel have a positive attitude towards a QA programme. Besides, the team culture and its leadership are ready for the implementation of a QA programme. Efforts should be made to improve team processes and the relation with the wider organisation to ensure an optimal team culture, aimed at quality improvement.
Introduction
Quality assurance (QA) in endoscopy is of utmost importance.1 2 The rising expenditures in healthcare and the increasing demand for endoscopic procedures both stress the need for continuous QA.3 4 Furthermore, in colorectal cancer (CRC) screening programmes, comprehensive monitoring of the quality of the endoscopy service is essential as healthy individuals are invited and may receive an invasive endoscopic procedure. Therefore, during the implementation of a CRC screening programme, a comprehensive QA programme should be enrolled as well.
QA in endoscopy consists of various aspects.5 6 First and foremost, the clinical quality of the procedure is important. A high quality endoscopic procedure consists of a safe, thorough and complete inspection of the gastrointestinal tract. However, the complete journey of a patient through the endoscopy department is important in optimising the benefits of endoscopy, providing maximal clinical benefit at minimal risk, and at maximal patients' satisfaction and willingness to return. This, in turn, enhances the uptake and thereby the cost-effectiveness of CRC screening.7
The attitudes and behaviour of healthcare personnel appears to have a major impact on patient experiences.8 Every endoscopy team member influences the quality of the endoscopy department. Therefore, it is crucial that there is a team culture aimed at providing excellent care with well-organised collaboration both between and within teams. In recent years, the team culture within healthcare departments has increasingly become of interest, following developments in the airline industry.9 10 Within a team culture aimed at quality improvement, personnel should know the targets of their department, feel responsible to achieve these targets and feel free to speak up. It should be stressed that QA is a team responsibility. Dedicated leadership is a key factor to realise this.
In an earlier study, we assessed the opinion of gastroenterologists with respect to QA in endoscopy.11 Gastroenterologists were well aware of the need of QA and were prepared to work on the quality of the endoscopy department. However, as outlined above, the opinion of the other team members is equally important to successfully improve the quality of the service. Therefore, the aim of this study was to assess the opinion about QA of endoscopy personnel other than gastroenterologists. Additionally, a team assessment was performed to explore the team leadership and team performance to determine what organisational areas need attention to enforce a culture aimed at quality improvement.
Methods
A survey was sent to all endoscopy nurses, assistants and managers registered at the Dutch Society of Endoscopy Nurses and Assistants (n=670).12 In a former study, the opinion of gastroenterologists was investigated. As we were interested whether there were differences between their opinion and the opinion of the other endoscopy personnel, we performed this current study and did not send a new survey to the gastroenterologists forming a part of the endoscopy team. In The Netherlands, officially trained endoscopy nurses, as well as general nurses and assistants, can be employed in the endoscopy department. The specialism of endoscopy nurse is an expanding expertise, which requires additional training, besides the general nurse training. Nearly all Dutch hospitals employ trained endoscopy nurses for the direct assistance of endoscopists. Other personnel like endoscopy assistants provide support on the department in patient care, service maintenance and administrative work.
The first part of the survey contained questions enquiring the attitude of the endoscopy personnel towards QA in endoscopy. This part was used before in a former study about the attitude of gastroenterologists towards QA.11 In short, the first part of the questionnaire assessed the overall attitude towards a QA programme, its design, content, the handling of results and the perceived effects of a comprehensive QA programme.
The second part of the survey was a previously used team assessment tool from the UK. The team assessment is an evaluation of the team functioning and leadership and was designed as part of a team leadership programme in endoscopy in the UK. The team assessment was translated into Dutch by a certified translation company. The team assessment tool contained 43 statements subdivided in six separate domains called: ‘communication’ (four questions about the communication within the team), ‘recognition and reward’ (four questions about how team members feels their contributions are rewarded), ‘team culture’ (nine questions about whether team members enjoy working in the team), ‘team process’ (nine questions about planning), ‘team working’ (eight questions about responsibilities within the team) and ‘wider organization’ (nine questions about the relation with the high managerial levels within the hospital).
All answers were given on a 5-point Likert scale, with 1 being a very positive opinion, and 5 being a very negative opinion towards the particular item. Nurses and assistants were given the possibility to complete the questionnaire online or send it back by mail. All non-respondents were sent a reminder 5 weeks after the first mailing. The completed questionnaires were anonymously entered into a database. Statistical analyses were performed using the SPSS statistical package V.17.0.2. Descriptive statistical analyses were performed using χ2 tests for categorical data and Student's t tests for continuous data.
Multivariate ordinal logistic regression was performed to assess correlations between overall attitude towards QA, perceived effects and the willingness to disclose QA results with gender, age and type of hospital where the respondent was employed.
The data from the items of the team assessment were transformed in a summary score for each domain. The higher the summary score, the less positive participants judged about a certain domain. Beforehand, it was decided arbitrarily that scores between 1 and 2 would be regarded as positive, scores between 2 and 3 as reassuring scores, although improvements in these areas should be sought, while scores of 3 and higher would be regarded as insufficient, delineating high priority areas of attention. The summary scores were then used in multivariate regression analyses to assess correlation with age, gender, type of hospital where the respondent was employed at, and overall attitude towards QA.
Results
Study population
Of the 670 questionnaires, a total of 295 (44%) were returned. Table 1 shows the available demographic data of the respondents and the non-respondents. Respondents were significantly more often employed at a general hospital, compared with non-respondents (93% vs 85%, p=0.003).
Table 1.
Demographic data
| Responders n (%) | Non-responders n (%) | p Value | |
|---|---|---|---|
| Total | 294 (44.0) | 376 (56.3) | - |
| Female gender | 269 (91.5) | 346 (92.0) | 0.774 |
| Mean age (years, SD) | 46.5 (8.7) | NA | - |
| Employed at: | |||
| Academic hospital | 22 (7.5) | 56 (15.1) | 0.003 |
| General hospital | 271( 92.5) | 315 (84.9) | |
| Median years of experience on the endoscopy department (IQR) | 10.0 (6.0–17.0) | NA | - |
NA, not available.
Attitude towards QA
The majority of the respondents (87%) expressed a positive attitude towards the implementation of a nationwide QA programme on the endoscopy department. Only one person reported a negative attitude towards it, while 12% of the respondents were neutral. When asked about the feasibility of implementation, 54% of the respondents perceived that it would be feasible to implement a QA programme nationwide. Thirty-eight per cent had no clear opinion, while 8% expected it to be unfeasible.
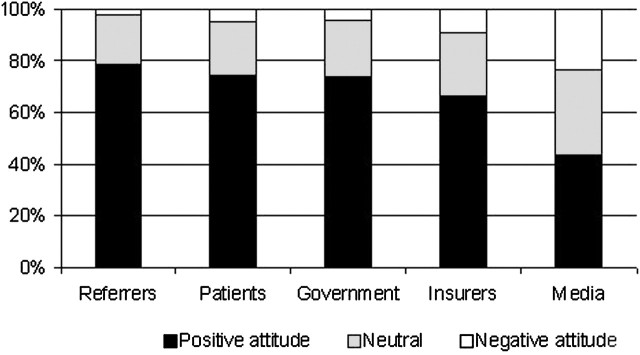
Figure 1 shows the results of the respondents with respect to the disclosure of QA results towards different stakeholders in endoscopy. The nurses and assistants on the endoscopy department were especially reserved towards disclosure of the results to media (24%) and insurers (9%), while a less negative perception was reported to share the results with patients (5%), government (4%) and referrers (2%).
Figure 1.
Attitude of endoscopy personnel towards the disclosure of quality assurance results to different stakeholders.
Eighteen per cent of the respondents were afraid that a comprehensive QA programme on the endoscopy department would lead to reduction of the available time for patient contact, 50% thought there would be no impact on the time, while 33% thought that more time would come available.
The endoscopic capacity would increase according to 33% of the respondents, the quality would increase according to 70% and 62% of the respondents expected that the publicity around the endoscopy department would be positively influenced.
Table 2 shows the priority ranking of different quality aspects according to the endoscopy personnel. Optimal provision of patient information (99%), attentive aftercare (97%) and optimal patient experiences (96%) were regarded to be the most important aspects to consider in a QA programme on the endoscopy department. Least important were the diagnostic findings (77%), use of sedation (78%) and completeness of procedures (80%).
Table 2.
Importance of different quality parameters
| Parameter | (Very) important (%) | Neutral (%) | (Absolutely) not important (%) |
|---|---|---|---|
| Length of waiting list | 85.3 | 12.7 | 2.1 |
| Proper patient information | 98.6 | 1.4 | 0.0 |
| Use of informed consent | 84.2 | 15.8 | 0.0 |
| Waiting time on the department | 87.6 | 11.4 | 1.0 |
| Appropriate indication | 93.5 | 6.2 | 0.3 |
| Monitoring of use of sedation | 78.1 | 18.8 | 3.0 |
| Findings | 77.0 | 19.6 | 3.4 |
| Completeness of procedures | 79.6 | 18.0 | 2.4 |
| Patient experiences | 96.2 | 3.4 | 0.3 |
| Aftercare | 96.9 | 3.1 | 0.0 |
| Complications | 88.3 | 11.7 | 0.0 |
| Correct follow-up advice | 89.3 | 10.0 | 0.7 |
| Complete reporting | 92.8 | 6.9 | 0.3 |
In the multivariate analyses, older age was significantly associated with a less positive general attitude towards QA (OR: 1.04, 95% CI 1.00 to 1.08), whereas type of hospital and gender were not.
Older age was also a significant predictor of a less positive attitude towards sharing the results with the government (OR: 0.97, 95% CI 0.94 to 0.99) and other hospitals (OR: 0.95, 95% CI 0.92 to 0.98), while the type of hospital and gender were not associated with the attitude to disclose results. Willingness to disclose the results to other stakeholders in endoscopy and the perceived effects of a QA programme were not significantly associated with age, gender and type of hospital.
Team assessment
Table 3 shows the mean scores for the six different domains regarding the team assessment. Employees of academic hospitals in comparison with those working in general hospitals scored significantly less favourably for the domains of ‘team culture’ (2.07 vs 2.39, p=0.02) and ‘recognition and reward’ (2.13 vs 2.40, p=0.048).
Table 3.
Team assessment scores
| Domain | Mean domain score | Academic hospital | General hospital | Range of item scores | Cronbach's α |
|---|---|---|---|---|---|
| Communication | 2.05 | 2.19 | 2.04 | 1.78–2.49 | 0.78 |
| Recognition and reward | 2.15 | 2.40 | 2.13* | 1.71–2.50 | 0.56 |
| Team culture | 2.09 | 2.39 | 2.07* | 1.66–2.80 | 0.86 |
| Team process | 2.42 | 2.59 | 2.40 | 2.08–2.88 | 0.89 |
| Team working | 1.97 | 2.12 | 1.95 | 1.63–2.38 | 0.79 |
| Wider organization | 3.00 | 3.00 | 3.00 | 2.66–3.75 | 0.86 |
5-point Likert scale; 1-Very positive; 2-Positive; 3-Neutral; 4-Negative; 5-Very negative.
p<0.05.
Within the domain ‘communication’, team members were most positive about the ability of the team to negotiate solutions when problems arise (mean score: 1.78, SD: 0.72), while a considerable number of team members were unsatisfied with the freedom to speak out their mind within the team (mean score: 2.49, SD: 1.03).
The domain ‘recognition and reward’ showed that team members feel appreciated by other team members for the work they do (mean score: 1.71, SD: 0.66). Less favourable scores were given to the team incentives to generate financial savings (mean scores: 2.50, SD: 0.86).
Endoscopy team members were positive about the flexibility and willingness of colleagues to go the extra mile when needed (mean score: 1.66, SD: 0.80) within the ‘team culture’ domain. On the other hand, a considerable number of respondents indicated that there was a ‘blame culture’ in the endoscopy team (mean score: 2.80, SD: 1.04).
Team members judged the most negative about the larger organisation. A mean score of 3.75 (SD: 1.00) was given to the statement whether the team has influence on higher levels in the organisation, while the best score within this domain was given for the statement that the teams' goodwill was not abused (mean score: 2.65, SD: 1.05).
Multivariate regression analyses showed that older age was the only variable significantly associated with more positive scores within the domains ‘team work’ (OR: 0.99, 95% CI 0.98 to 1.00) and ‘team culture’ (OR: 0.99, 95% CI 0.98 to 1.00). No other correlations between the variables age, gender or type of hospital and one of the domains were found.
Discussion
This study shows that endoscopy nurses and assistants generally have a positive attitude towards QA on the endoscopy department and expect that a QA programme would have a positive effect on the overall quality of the department. However, concerns were raised about the time required for structured QA resulting in less time for patient care and a decreased capacity. Additionally, only half of the respondents expected the implementation of a QA programme nationwide would be feasible. Respondents indicated that the most important quality parameters were patient-related aspects like patient information provision, patient experiences and aftercare. The results from the team assessment showed that the endoscopy personnel were in general satisfied about their team culture, and indicated that attention is needed for the relation with the wider organisation.
Before healthcare innovations such as continuous quality assessment and quality improvement projects can be disseminated throughout a healthcare system, it should be assured that the project is compatible with the beliefs, values and needs of the people who should work with it.13 The results of the first part of this study showed that the majority of the endoscopy teams supports introduction of a QA programme. These results are in line with a previous study in the same setting among gastroenterologists.11 Although there were small differences, gastroenterologists expressed the same attitude towards and perceived the same benefits from a comprehensive, nationwide QA programme.
An important finding is that gastroenterologists and nurses prioritise different quality parameters. In the current study, nurses prioritise patient aspects of care, with especially waiting lists (85%), patient information (99%) and patient experiences (96%) as important quality indicators. In the previous study among endoscopists, these parameters were deemed important by fewer respondents (66%, 95% and 87%, respectively).11 On the other hand, the clinical aspects of the procedure, like completeness (92%), diagnostic yield (82%) and complications (97%), were deemed to be more important by the gastroenterologists, while fewer nurses and assistants rated these parameters important (79%, 77%, 88%, respectively). The differences in priorities of QA might be explained by the important role nurses play in patient satisfaction. Over 60% of patients' satisfaction is determined by nurse interaction, as they have the most intense patient contact.14 15 Moreover, several studies have shown that nurses' personal manner is an important factor in patient satisfaction in endoscopy.8 16 Nurses might be well aware of their ability to influence patients' satisfaction and know they are well suited in addressing these quality parameters that directly influence the patient experiences.
Besides their role in patient satisfaction, it has been suggested that nurses are probably best equipped to identify department strengths, as well as weaknesses, as they are present on the endoscopy department the entire working day.17 Therefore, their knowledge and commitment in QA should be mobilised. Dedicated leadership is a key factor to pursue the right team culture aimed at continuous quality improvement. Our team assessment indicates that the team is motivated and willing to collaborate to actively work on the departments' service. However, low scores on the domain ‘team process’ indicate that improvement should be sought in setting and planning common targets. This is important as the endoscopy team should agree on common goals to provide excellent care and these goals should be understood by everyone in the team.
What is already known on this subject.
-
▶
For successful quality assurance (QA), the entire medical team should be motivated and support the programme.
-
▶
In the implementation of a QA programme, all stakeholders should be heard.
What this study adds.
-
▶
Endoscopy personnel feel positive about the implementation of a QA programme.
-
▶
Endoscopy personnel prioritise different aspects of QA compared to gastroenterologists.
-
▶
The team culture on the endoscopy department and its leadership seems to be sufficient to implement a QA program successfully, although the communication to the wider organisation and within the team may need some attention.
How might it impact on clinical practice in the forseeable future.
-
▶
Endoscopy personnel other than gastroenterologists should be actively engaged in the process of developing a QA programme.
-
▶
Successful QA needs the support of the entire health care team working with it.
Our study showed that endoscopy personnel feel that there is a satisfactory presence of skill and knowledge mix. There is evidence that the skill mix of the team and the number of nurses available in the hospital influence clinical outcomes. In several studies, it has been shown that factors of influence on hospital mortality outcomes are level of experience and number of registered nurses, as well as ratios of nurses to unqualified staff or nurses to patients.18 19
Improvement can be achieved within the domain ‘wider organizations’, which indicates that the communication with higher management levels should be improved. As QA programmes are often designed and controlled by managers, these results emphasise that the management should stay in close contact with the people working with their interventions in order to be effective.13 The implementation of a QA programme should not be a top-down process, but more a close collaboration between the different levels, as is also underlined by the differences in priorities in quality indicators between gastroenterologists and nurses and assistants.
The results of this study should be appreciated in the context of its setting. Currently no comprehensive QA programme for endoscopy is available in The Netherlands. In the coming years, while a CRC screening programme will be enrolled throughout the country, it is expected that a QA programme will become available. Results of the studies discussed above are incorporated in the development of this programme, and it will be interesting to see how satisfied the personnel will be in a couple of years with the proposed QA programme. In this context, there is also a lot to learn from the UK where many developments in QA have taken place a couple of years ago. The success in the UK in raising the quality of endoscopy has depended greatly on the efforts of the nurses and assistants. Therefore, it is recommended to seek their input in developing a QA programme in order to achieve the maximum benefit from the efforts.
A limitation of our study is that the response rate is low despite the fact that the survey was brought to the attention on different occasions. No additional data are available on the non-responders. In the context of the above-mentioned setting of this study, the low uptake might reflect the fact that currently QA is not a general accepted part of the work of the endoscopy personnel other than gastroenterologists. As in the UK nurses have taken a leading role in QA at the endoscopy department, all efforts should be sought to incorporate the nurses and assistants in the development of a QA programme to increase the probability of success of a QA programme.
In conclusion, the implementation of a QA programme in endoscopy is supported by endoscopy nurses, assistants and managers. Moreover, it seems that the current team culture suffices to create an optimal team culture to improve the quality of the endoscopy department. The results emphasise the need for close collaboration with all levels within an organisation to design such a QA programme to properly address all their concerns. QA will only successfully lead to quality improvement as the entire endoscopy team will be dedicated to collaborate in the quality initiatives.
Footnotes
Contributors: VdJ: concept and design, analyses and interpretation of data, drafting and revision of the article, final approval; EJK and MEvL: concept and design, interpretation of data, revision of the article, final approval.
Competing interests: None.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Johanson JF. Continuous quality improvement in the ambulatory endoscopy center. Gastrointest Endosc Clin N Am 2002;12:351–65. [DOI] [PubMed] [Google Scholar]
- 2.Faigel DO, Pike IM, Baron TH, et al. Quality indicators for gastrointestinal endoscopic procedures: an introduction. Gastrointest Endosc 2006;63(4 Suppl):S3–9. [DOI] [PubMed] [Google Scholar]
- 3.Bjorkman DJ, Popp JW., Jr Measuring the quality of endoscopy. Gastrointest Endosc 2006;63(4 Suppl):S1–2. [DOI] [PubMed] [Google Scholar]
- 4.Vijan S, Inadomi J, Hayward RA, et al. Projections of demand and capacity for colonoscopy related to increasing rates of colorectal cancer screening in the United States. Aliment Pharmacol Ther 2004;20:507–15. [DOI] [PubMed] [Google Scholar]
- 5.Valori R, Sint Nicolaas J, de Jonge V. Quality assurance of endoscopy in colorectal cancer screening. Best Pract Res Clin Gastroenterol 2010;24:451–64. [DOI] [PubMed] [Google Scholar]
- 6.Johanson JF, Schmitt CM, Deas TM, Jr, et al. Quality and outcomes assessment in Gastrointestinal Endoscopy. Gastrointest Endosc 2000;52(6 Pt 1):827–30. [PubMed] [Google Scholar]
- 7.Pignone M, Saha S, Hoerger T, et al. Cost-effectiveness analyses of colorectal cancer screening: a systematic review for the U.S. Preventive Services Task Force. Ann Intern Med 2002;137:96–104. [DOI] [PubMed] [Google Scholar]
- 8.Ko HH, Zhang H, Telford JJ, et al. Factors influencing patient satisfaction when undergoing endoscopic procedures. Gastrointest Endosc 2009;69:883–91, quiz 891.e1. [DOI] [PubMed] [Google Scholar]
- 9.Surgenor SD, Blike GT, Corwin HL. Teamwork and collaboration in critical care: lessons from the cockpit. Crit Care Med 2003;31:992–3. [DOI] [PubMed] [Google Scholar]
- 10.Mann S, Marcus R, Sachs B. Grand rounds: lessons from the cockpit: how team training can reduce errors on L&D. Contemporay OB/GYN 2006;51:34–45. [Google Scholar]
- 11.de Jonge V, Kuipers EJ, van Leerdam ME. Opinion of gastroenterologists towards quality assurance in endoscopy. Dig Liver Dis 2011;43:215–19. [DOI] [PubMed] [Google Scholar]
- 12.Team 360 assessment. Quality Solutions for Healthcare. 2011. Avaliable from: http://www.qsfh.co.uk/Page.aspx?PageId=Public (accessed 14 Jan 2012).
- 13.Berwick DM. Disseminating innovations in health care. JAMA 2003;289:1969–75. [DOI] [PubMed] [Google Scholar]
- 14.Gantz NR, Sorenson L, Howard RL. A collaborative perspective on nursing leadership in quality improvement. The foundation for outcomes management and patient/staff safety in health care environments. Nurs Adm Q 2003;27:324–9. [DOI] [PubMed] [Google Scholar]
- 15.Sitzia J, Wood N. Patient satisfaction: a review of issues and concepts. Soc Sci Med 1997;45:1829–43. [DOI] [PubMed] [Google Scholar]
- 16.Lin OS, Schembre DB, Ayub K, et al. Patient satisfaction scores for endoscopic procedures: impact of a survey-collection method. Gastrointest Endosc 2007;65:775–81. [DOI] [PubMed] [Google Scholar]
- 17.Needleman J, Hassmiller S. The role of nurses in improving hospital quality and efficiency: real-world results. Health Aff (Millwood) 2009;28:w625–33. [DOI] [PubMed] [Google Scholar]
- 18.Aiken LH. Charting the future of hospital nursing. Image J Nurs Sch 1990;22:72–8. [DOI] [PubMed] [Google Scholar]
- 19.Aiken LH, Clarke SP, Sloane DM, et al. Hospital nurse staffing and patient mortality, nurse burnout, and job dissatisfaction. JAMA 2002;288:1987–93. [DOI] [PubMed] [Google Scholar]