Abstract
Purpose
The pathogenesis of groin hernia is not fully understood and some suggested risk factors are debatable. This population-based study evaluates the association between groin hernia repair and tobacco use.
Method
An observational study based on register linkage between the Swedish Hernia Register and the Västerbotten Intervention Program (VIP). All primary groin hernia repairs performed from 2001 to 2013 in the county of Västerbotten, Sweden, were included.
Results
VIP provided data on the use of tobacco in 102,857 individuals. Neither smoking nor the use of snus, increased the risk for requiring a groin hernia repair. On the contrary, heavy smoking decreased the risk for men, HR 0.75 (95% CI 0.58–0.96), as did having a BMI over 30 kg/m2 HR (men) 0.33 (95% CI 0.27–0.40).
Conclusion
Tobacco use is not a risk factor for requiring a groin hernia repair, whereas having a low BMI significantly increases the risk.
Keywords: Hernia, Tobacco, BMI
Introduction
Previous research has identified family history [1, 2], low BMI [3], abdominal aortic aneurysm [4], patent processus vaginalis [5], abnormal collagen metabolism [6, 7] and certain abdominal operations such as appendectomy and prostatectomy [8], as being risk factors for the development of groin hernia.
There have been speculations regarding tobacco as a possible risk factor [9, 10], but until now there has only existed circumstantial evidence of a connection. Furthermore, there is epidemiological evidence indicating that recurrence of hernia is more common [11, 12] and that the primary hernia occurs at a younger age [13] among smokers. Others studies have shown that smokers have changes in collagen metabolism [10, 14, 15] and suggested that there might be a connection with the development of hernia [10]. However, no large-scale research has been performed to see if tobacco use increases the risk for developing a groin hernia.
The aim of this study was to evaluate the correlation between tobacco use and risk for requiring a groin hernia requiring surgical repair. It is based on a register linkage between the Swedish Hernia Register (SHR) [16] and the Västerbotten Intervention Program (VIP) [17]. Tobacco products evaluated are cigarettes and snus, a moist form of oral smokeless tobacco [18].
Our hypothesis was that tobacco use is a risk factor for requiring a groin hernia repair.
Materials and methods
The Västerbotten Intervention Program
The VIP is an ongoing population-based health survey operated by the county of Västerbotten, Sweden. It started as a small pilot study in 1985. From 1990 the program was expanded to include the whole county of Västerbotten in 1992. All citizens are invited to participate at the ages of 40, 50 and 60 (until 1995 even 30-year olds were invited) as described in previous reports [17]. Since 2005 participation rates have been 66–67%. Each year 6500–7000 routine health examinations are included in the register. By 2007 the total number of examinations registered had amounted to 113,203 [17]. An extensive questionnaire constitutes part of the examination, covering amongst other things the use of tobacco [17].
The Swedish Hernia Register
The SHR started in 1992 and has since grown to include data on over 300,000 groin hernia repairs (GHR). Today, almost all units performing GHR in Sweden are included [19]. Since 2001 all surgical departments in the county of Västerbotten are affiliated. An external review has established that coverage by the SHR of hernia repair surgery performed in Sweden is over 95% [16].
Study population
The present cohort study is based on the population registered in the VIP up until January 29, 2013. GHR outcome was added as a variable by register linkage with the SHR. All patients aged fifteen or older with first time GHR performed at any of the surgical units in the county of Västerbotten between January 1, 2001 and December 31, 2013 were included.
It is Swedish law that every permanently residing citizen is assigned a specific identification number used for identification purposes [20]. The SHR has permission to use this number for following up patients and linking their GHR to the unit where it was performed. This identification system was also used for the register linkage of present cohort.
Included individuals were followed till end of 2013, date of GHR or day of death.
The unit of Epidemiology and Global Health at Umeå University provided the service of register linkage and anonymization of data.
Exclusion
Patients who underwent a GHR before participating in the VIP were excluded. Individuals who exclusively smoked pipe, cigar or pipe and cigar were excluded.
Variables and group definitions
The definition of groin hernia repair (GHR) in this study included all first time inguinal, femoral and combined repairs. Bilateral hernia surgery was regarded as a single event.
For statistical analyses, the VIP questionnaire on tobacco use was categorized and divided into groups (Text box 1 in appendix). Many worded answers to the questions on tobacco use e.g. “No, never smoked” and “Yes, I smoke occasionally (not daily)” where treated as missing.
Text box 1.
Tobacco use grouping
| Categorized as | |
|---|---|
| VIP question: “Do you smoke?” | |
| (A) No, never smoked | Never smoked |
| (B) Not now, but smoked regularly before | Previous use |
| (C) Not now, but have smoked now and again | Previous use |
| (D) Yes, I smoke occasionally (not daily) | Light smoker |
| (E) Yes, I smoke cigarettes 1–4 each day | Light smoker |
| (F) Yes, I smoke cigarettes 5–14 each day | Light smoker |
| (G) Yes, I smoke cigarettes 15–24 each day | Heavy smoker |
| (H) Yes, I smoke cigarettes 25 or more each day | Heavy smoker |
| VIP question: “Have you ever used snus? | |
| 1. No | Never used |
| 2. Yes, I used to do it, but not anymore | Previous use |
| 3. Yes, I use less than 2 boxes each week | Light use |
| 4. Yes, I use 2–4 boxes each week | Light use |
| 5. Yes, I use more than 4 but less than 7 boxes each week | Heavy use |
| 6. Yes, I use 7 boxes or more each week | Heavy use |
VIP questions above are translated from Swedish to English. The answer “yes” was added to each group
BMI values were categorized into three groups, “<25 kg/m2”, “25–29.9 kg/m2”, and “>30 kg/m2”.
Level of education was categorized according to number of years of education, <9, 9–12, and >12 years.
“Age” was age at inclusion in the BIP and was also divided into three groups, ≤45, 46–55, and ≥55 years.
Due to the great difference in incidence of groin hernia between men and women all analyses were separated depending on gender.
Statistics
Independent sample t test was used to compare continuous variables such as time in the study, age and BMI. Chi-square test was used for all categorical variables.
Hazard ratio (HR) was calculated using Cox regression. Confidence intervals (95%) are presented with HR in the tables, Wald statistics was used to test statistical significance. For multivariate analyses, the results were stratified for “age at inclusion” since the variable did not satisfy the proportional hazards assumption, this allowed us to adjust for “age at inclusion” while estimating the effects of BMI, education and tobacco.
IBM® SPSS® Statistics Version 22 was used for data management and analyses.
Ethics
Ethical approval was granted by the Regional Ethics Committee in BLINDED Umeå Sweden.
Results
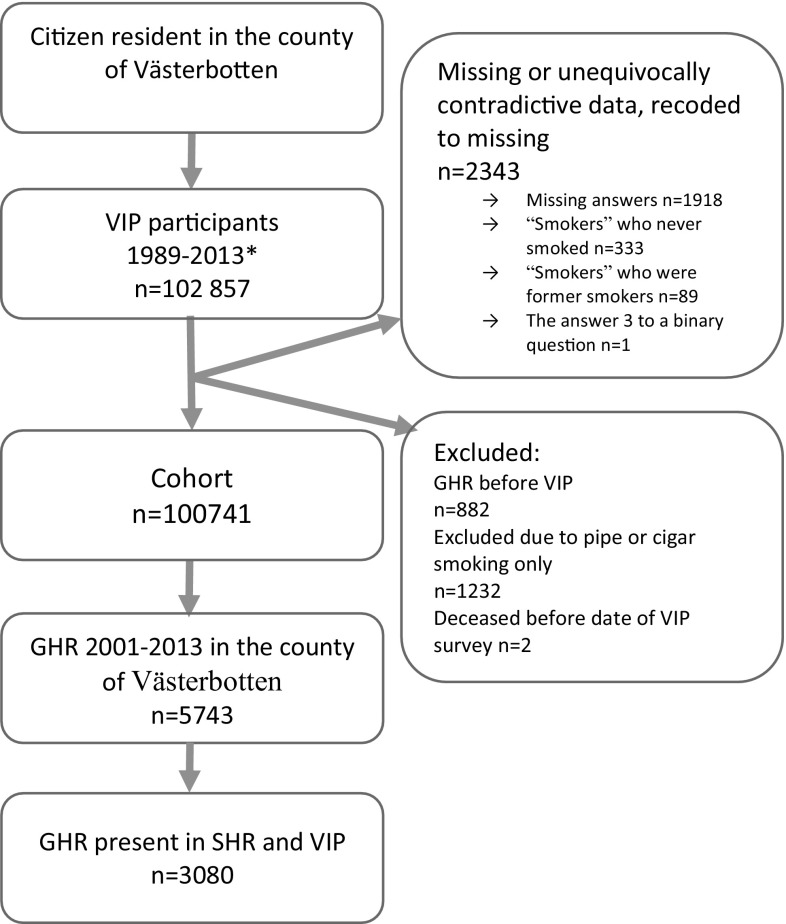
This study included a total of 102,857 individuals. After exclusion 100,741 remained for analysis. In the category smoking, 423 were recoded as missing due to answers not being interpretable. A total of 5743 primary GHRs performed in Västerbotten during the study period were registered in the SHR, of which 3080 were also present in the BIP (Fig. 1).
Fig. 1.
Flow chart, exclusion and missing data. Flow chart, showing exclusion and cleaning of data. * VIP participants 1989 to January 29, 2013
Basal characteristics showed that there were significant differences between the GHR and none-GHR groups among men with regards to the following variables: smoking, use of snus, BMI, education level, and age at inclusion. Among women, significant differences, between the GHR and non-GHR groups were seen for BMI, education level, and age at inclusion (Table 1).
Table 1.
Baseline characteristics from the Västerbotten Intervention Program cohort between 1989 and 2013 with 3080 groin hernia repairs added from Swedish Hernia Register
| Men n = 48,662 | Women n = 52,079 | |||||||
|---|---|---|---|---|---|---|---|---|
| None-GHR | GHR | Total | p | None-GHR | GHR | Total | p | |
| n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | |||
| Smoking | ||||||||
| Never smoked | 23,221 (51.2) | 912 (47.7) | 24,133 (51.1) | 0.001 | 25,933 (50.9) | 78 (49.4) | 26,011 (50.9) | 0.305 |
| Previous use | 14,972 (33.0) | 718 (37.5) | 15,690 (33.2) | 15,605 (30.6) | 42 (26.6) | 15,647 (30.6) | ||
| Light smoker | 5238 (11.6) | 211 (11.0) | 5449 (11.5) | 7839 (15.4) | 32 (20.3) | 7871 (15.4) | ||
| Heavy smoker | 1911 (4.2) | 72 (3.8) | 1983 (4.2) | 1555 (3.1) | 6 (3.8) | 1561 (3.1) | ||
| Snus | ||||||||
| Never used | 25,802 (56.8) | 1212 (63.2) | 27,014 (57) | <0.001 | 44,010 (87.8) | 145 (94.8) | 44,155 (87.8) | 0.069 |
| Previous use | 7835 (17.2) | 308 (16.1) | 8143 (17.2) | 2500 (5.0) | 4 (2.6) | 2504 (5.0) | ||
| Light use | 8522 (18.7) | 314 (16.4) | 8836 (18.7) | 2840 (5.7) | 3 (2.0) | 2843 (5.7) | ||
| Heavy use | 3294 (7.2) | 83 (4.3) | 3377 (7.1) | 792 (1.6) | 1 (0.7) | 793 (1.6) | ||
| BMI | ||||||||
| BMI <25 | 14,886 (32.6) | 846 (43.8) | 15,732 (33) | <0.001 | 24,511 (48.1) | 97 (60.2) | 24,608 (48.1) | 0.008 |
| BMI 25–29.9 | 22,597 (49.4) | 960 (49.7) | 23,557 (49.5) | 17,369 (34.1) | 44 (27.3) | 17,413 (34.1) | ||
| BMI ≥30 | 8221 (18.0) | 124 (6.4) | 8345 (17.5) | 9092 (17.8) | 20 (12.4) | 9112 (17.8) | ||
| Education | ||||||||
| 0–9 years | 11,460 (24.8) | 728 (37.1) | 12,188 (25.3) | <0.001 | 13,366 (26.0) | 68 (41.7) | 13,434 (26.1) | <0.001 |
| 9–12 years | 23,473 (50.7) | 841 (42.9) | 24,314 (50.4) | 20,883 (40.7) | 58 (35.6) | 20,941 (40.7) | ||
| >12 years | 11,324 (24.5) | 392 (20.0) | 11,716 (24.3) | 17,089 (33.3) | 37 (22.7) | 17,126 (33.3) | ||
| Age at inclusion | ||||||||
| <45 | 14,575 (31.2) | 273 (13.8) | 14,848 (30.5) | <0.001 | 15,131 (29.1) | 22 (13.4) | 15,153 (29.1) | <0.001 |
| 46–55 | 13,210 (28.3) | 409 (20.7) | 13,619 (28.0) | 14,418 (27.8) | 27 (16.5) | 14,445 (27.7) | ||
| 56–65 | 18,899 (40.5) | 1296 (65.5) | 20,195 (41.5) | 22,366 (43.1) | 115 (70.1) | 22,481 (43.2) | ||
The Västerbotten Intervention Program cohort between 1989 and 2013 with 3080 groin hernia repairs added from Swedish Hernia Register. p Values are Chi-Square tests, used to examine differences within each group
Univariate analyses for men revealed that heavy smoking and use of snus reduced the HR whereas a BMI <25, low education and high age increased the HR. For women, low BMI and high age increased the HR (Table 2).
Table 2.
Univariate Cox regression analyses for requiring a groin hernia repair
| Men | Women | |||
|---|---|---|---|---|
| HR (95% CI) | p | HR (95% CI) | p | |
| Smoking | ||||
| Never smoked | 1.00 | 1.00 | ||
| Previous use | 1.09 (0.99–1.20) | 0.08 | 0.97 (0.66–1.41) | 0.86 |
| Light smoker | 0.91 (0.78–1.05) | 0.19 | 1.22 (0.81–1.84) | 0.35 |
| Heavy smoker | 0.71 (0.56–0.91) | 0.01 | 1.01 (0.44–2.31) | 0.99 |
| Snus | ||||
| Never used | 1.00 | 1.00 | ||
| Previous use | 0.99 (0.87–1.12) | 0.84 | 0.74 (0.27–2.01) | 0.56 |
| Light use | 0.85 (0.75–0.96) | 0.01 | 0.45 (0.14–1.42) | 0.17 |
| Heavy use | 0.69 (0.55–0.86) | <0.01 | 0.70 (0.10–4.99) | 0.72 |
| BMI | ||||
| <25 | 1.00 | 1.00 | ||
| 25–29.9 | 0.80 (0.73–0.88) | <0.01 | 0.63 (0.44–0.89) | 0.01 |
| ≥30 | 0.33 (0.27–0.4) | <0.01 | 0.59 (0.36–0.95) | 0.03 |
| Education | ||||
| 0–9 years | 1.00 | 1.00 | ||
| 9–12 years | 0.83 (0.75–0.92) | <0.01 | 0.84 (0.59–1.2) | 0.35 |
| >12 years | 0.80 (0.71–0.91) | <0.01 | 0.71 (0.47–1.06) | 0.09 |
| Age at inclusion | ||||
| <45 | 1.00 | 1.00 | ||
| 46–55 | 1.87 (1.60–2.17) | <0.01 | 1.44 (0.82–2.53) | 0.20 |
| 56–65 | 3.19 (2.80–3.63) | <0.01 | 2.88 (1.82–4.54) | <0.01 |
Univariate analyses using Cox regression to calculate hazard ratio (HR) and p values. p values are Wald-p. Based on the Västerbotten Intervention Program cohort between 1989 and 2013 with 3080 groin hernia repairs added from Swedish Hernia Register
In the multivariate analyses of the tobacco variables, no significant increased risk amongst tobacco users was seen (Tables 3, 4). On the contrary, in men, heavy smoking significantly lowered the HR (HR 0.75, 95% CI 0.58–0.96, Table 3), but this was not the case for women. A BMI of 25–29.9 and BMI >30 significantly reduced the HR in all multivariate analyses in both genders (Tables 3, 4). As regards level of education, 9–12 years of education increased HR significantly for men but not for women in both the smoking and the snus analyses.
Table 3.
Multivariate Cox regression analyses focused on smoking
| Men | Women | |||
|---|---|---|---|---|
| HR (95% CI) | p | HR (95% CI) | p | |
| Smoking | ||||
| Never smoked | 1.00 | 1.00 | ||
| Previous use | 0.97 (0.87–1.07) | 0.54 | 1.13 (0.76–1.68) | 0.54 |
| Light smoker | 0.92 (0.79–1.08) | 0.32 | 1.25 (0.79–1.98) | 0.35 |
| Heavy smoker | 0.75 (0.58–0.96) | 0.03 | 1.22 (0.49–3.05) | 0.67 |
| BMI | ||||
| <25 | 1.00 | 1.00 | ||
| 25–29.9 | 0.72 (0.65–0.79) | <0.01 | 0.56 (0.38–0.83) | 0.01 |
| ≥30 | 0.33 (0.27–0.40) | <0.01 | 0.52 (0.31–0.88) | 0.02 |
| Education | ||||
| Education 0–9 years | 1.00 | 1.00 | ||
| Education 9–12 years | 1.16 (1.03–1.29) | 0.01 | 1.18 (0.79–1.78) | 0.42 |
| Education > 12 years | 1.03 (0.90–1.18) | 0.67 | 0.95 (0.60–1.51) | 0.83 |
Multivariate analyses with focus on smoking, based on the 100,741 individuals in the Västerbotten Intervention Program cohort between 1989 and 2013 with 3080 groin hernia repairs added from Swedish Hernia Register Hazard ratio (HR) calculated by Cox regression adjusted for all variables in the table, stratified for age at inclusion. p values are Wald-p
Table 4.
Multivariate Cox regression analyses focued on snus
| Men | Women | |||
|---|---|---|---|---|
| HR (95% CI) | p | HR (95% CI) | p | |
| Snus | ||||
| Never used | 1.00 | 1.00 | ||
| Previous use | 1.10 (0.96–1.25) | 0.17 | 1.33 (0.48–3.72) | 0.58 |
| Light use | 0.93 (0.82–1.07) | 0.31 | 0.74 (0.23–2.36) | 0.61 |
| Heavy use | 1.04 (0.82–1.32) | 0.72 | 1.22 (0.17–8.94) | 0.84 |
| BMI | ||||
| < 25 | 1.00 | 1.00 | ||
| 25–29.9 | 0.71 (0.65–0.79) | <0.01 | 0.56 (0.38–0.82) | 0.01 |
| ≥ 30 | 0.33 (0.27–0.40) | <0.01 | 0.51 (0.30–0.87) | 0.01 |
| Education | ||||
| Education 0–9 years | 1.00 | 1.00 | ||
| Education 9–12 years | 1.16 (1.04–1.30) | 0.01 | 1.18 (0.79–1.77) | 0.42 |
| Education > 12 years | 1.04 (0.91–1.19) | 0.54 | 0.93 (0.59–1.47) | 0.75 |
Multivariate analyses with focus on snus, based on the 100,741 individuals in the Västerbotten Intervention Program cohort between 1989 and 2013 with 3080 groin hernia repairs added from Swedish Hernia Register Hazard Ratio (HR) calculated by Cox regression adjusted for all variables in the table, stratified for age at inclusion. p values are Wald-p
Discussion
Main findings
Tobacco variables examined in this study did not increase the risk for groin hernia requiring repair, neither in univariate nor in multivariate analysis.
The variable found to have greatest impact on risk for GHR was a BMI >25 kg/m2 that significantly decreased risk in all analyses, in both genders.
Strengths
The main strength of this study was the size of the study population. Extensive exposure data on BMI, tobacco use and educations level where collected from 102,857 individuals. The longitudinal approach of a cohort study adds strength.
The >95% coverage of the SHR database is itself a considerable strength [16].
The fact that high exposure groups were used when investigating the effect of smoking and the use of snus, adds reliability to the conclusion that tobacco use does not increase the risk of GHR.
Limitations
Information on the use of tobacco only accounts for the amount consumed at one point in time, there is no continuous follow-up. For this reason, changes in tobacco consumption over time cannot be accounted for. The time from when the information was provided at inclusion to event or the end of the study varies from a few days to 22.8 years.
Since VIP data are based on questionnaires, there is room for subjective assessment. Questionnaires have other drawbacks since some responders might not answer all the questions or provide missing or unequivocally contradictive data.
The VIP is an intervention program and participants receive health counseling based on their answers. This could have an effect on our analyses as some individuals may have changed their habits during the survey.
The VIP program has three inclusion ages (40, 50 and 60) while the SHR includes all GHRs occurring from the age of fifteen. Consequently, some patients had undergone GHR before inclusion in the VIP survey, and were thus excluded from the study.
Participation in the VIP and SHR is voluntary, thus risking selection bias in the study population. The good coverage of the SHR minimizes this risk. The VIP has a coverage of 66–67% somewhat limiting the basis of this cohort. However, only slight social selection bias was reported [21]. There is an underestimation of the incidence of GHR in present study since the total VIP cohort since 1989 was used. The first year SHR that included all GHRs in the county of Västerbotten was 2001, so only GHR after that year were included. We have no reason to suspect that there was a difference in risk factors for developing a groin hernia in need of repair before or after 2001.
Another aspect worth considering is that both heavy smoking and high BMI may have influenced surgeons and anesthesiologists in their risk–benefit calculation before deciding whether or not to perform a GHR. There is a possibility that this might have reduced the number of hernias considered suitable for operation in the heavy smoking and high BMI groups. Previous research has concluded that elective day-case surgery is associated with reduced risk for complications compared to emergency surgery [22], increasing the indication for elective day-case surgery on patients with several risk factors.
This study is based on hernia requiring repair and not the presence of groin hernia. Consequently, risk factors for developing a groin hernia requiring surgery are not necessarily the same as risk factors for actual formation of groin hernia. As with all observational studies, correlation is not necessarily the same as causation.
Relation to current knowledge
In this study, tobacco use did not increase the HR for GHR. We could only find two studies indicating an increased risk for hernia among smokers. In one of these, serum pancreas elastase activity was found to be increased among smokers with a direct or indirect hernia, and tobacco use was mentioned as a possible risk factor [10]. An observational cohort including 75 patients found earlier onset of primary hernia among smokers [13], indicating an association.
This study showed that individuals who smoke heavily had a decreased HR for undergoing a groin hernia repair, whereas other smaller case–control studies examining risk factors among men [1, 23, 24], women [25], and both genders [26] have failed to show any significant effect of smoking. There are, however, two studies with results that correlate with ours. One reported a close to significant decrease in hazard ratio (0.82, 95% CI 0.65–1) among current smokers [27], and another reported a significantly decreased hazard ratio among individuals who smoked more than fifteen grams of tobacco each day [28].
Since the use of snus is uncommon outside Scandinavia, no other studies on its effect on hernia formation exist to our knowledge.
In the present cohort high BMI was a protective factor against developing a groin hernia requiring surgery. This finding correlates well with the results of previous trials [3, 25, 27, 28].
Conclusion
Tobacco use is not a risk factor for requiring a groin hernia repair. A high BMI is associated with lower risk, though more extensive analysis is required to confirm this.
Appendix
See the Text box 1 in appendix.
Compliance with ethical standards
Conflicts of interest
The authors have been declares no conflict of interest.
Funding
The study was financially supported by the SHR that is exclusively funded by the Swedish government. There was no other source of funding.
Ethical statement
Present study was aproved by the Regional Ethics Committee in Umeå Sweden.
Statement on human rights
For this type of study, formal consent is not required.
Statement on the welfare of animals
This article does not contain any studies with animals performed by any of the authors.
Informed consent
Informed consent was obtained from all individuals at participation in VIP and SHR. This study has been performed in accordance with Swedish law.
References
- 1.Lau H, Fang C, Yuen WK, Patil NG. Risk factors for inguinal hernia in adult males: a case-control study. Surgery. 2007;141:262–266. doi: 10.1016/j.surg.2006.04.014. [DOI] [PubMed] [Google Scholar]
- 2.Carbonell JF, Sanchez JL, Peris RT, et al. Risk factors associated with inguinal hernias: a case control study. Eur J Surg. 1993;159:481–486. [PubMed] [Google Scholar]
- 3.Zendejas B, Hernandez-Irizarry R, Ramirez T, et al. Relationship between body mass index and the incidence of inguinal hernia repairs: a population-based study in Olmsted County. MN Hernia. 2014;18:283–288. doi: 10.1007/s10029-013-1185-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lehnert B, Wadouh F. High coincidence of inguinal hernias and abdominal aortic aneurysms. Ann Vasc Surg. 1992;6:134–137. doi: 10.1007/BF02042733. [DOI] [PubMed] [Google Scholar]
- 5.van Veen RN, van Wessem KJ, Halm JA, et al. Patent processus vaginalis in the adult as a risk factor for the occurrence of indirect inguinal hernia. Surg Endosc. 2007;21:202–205. doi: 10.1007/s00464-006-0012-9. [DOI] [PubMed] [Google Scholar]
- 6.Klinge U, Zheng H, Si ZY, Schumpelick V, Bhardwaj R, Klosterhalfen B. Synthesis of type I and III collagen, expression of fibronectin and matrix metalloproteinases-1 and -13 in hernial sac of patients with inguinal hernia. Int J Surg Investig. 1999;1:219–227. [PubMed] [Google Scholar]
- 7.Burcharth J, Rosenberg J. Hernias as medical disease. Ugeskr Laeger. 2008;170:3314–3318. [PubMed] [Google Scholar]
- 8.Abe T, Shinohara N, Harabayashi T, et al. Postoperative inguinal hernia after radical prostatectomy for prostate cancer. Urology. 2007;69:326–329. doi: 10.1016/j.urology.2006.09.043. [DOI] [PubMed] [Google Scholar]
- 9.Simons MP, Aufenacker T, Bay-Nielsen M, et al. European Hernia Society guidelines on the treatment of inguinal hernia in adult patients. Hernia. 2009;13:343–403. doi: 10.1007/s10029-009-0529-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cannon DJ, Read RC. Metastatic emphysema: a mechanism for acquiring inguinal herniation. Ann Surg. 1981;194:270–278. doi: 10.1097/00000658-198109000-00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sorensen LT, Friis E, Jorgensen T, et al. Smoking is a risk factor for recurrence of groin hernia. World J Surg. 2002;26:397–400. doi: 10.1007/s00268-001-0238-6. [DOI] [PubMed] [Google Scholar]
- 12.Burcharth J, Pommergaard HC, Bisgaard T, Rosenberg J. Patient-related risk factors for recurrence after inguinal hernia repair: a systematic review and meta-analysis of observational studies. Surg Innov. 2014 doi: 10.1177/1553350614552731. [DOI] [PubMed] [Google Scholar]
- 13.Jansen PL, Klinge U, Jansen M, Junge K. Risk factors for early recurrence after inguinal hernia repair. BMC Surg. 2009;9:18. doi: 10.1186/1471-2482-9-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Jorgensen LN, Kallehave F, Christensen E, Siana JE, Gottrup F. Less collagen production in smokers Surgery. 1998;123:450–455. [PubMed] [Google Scholar]
- 15.Norman PE, Curci JA. Understanding the effects of tobacco smoke on the pathogenesis of aortic aneurysm. Arterioscler Thromb Vasc Biol. 2013;33:1473–1477. doi: 10.1161/ATVBAHA.112.300158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Haapaniemi SA. Swedish thesis on groin hernia surgery. Hernia. 2001;5:204–205. doi: 10.1007/s10029-001-0035-z. [DOI] [PubMed] [Google Scholar]
- 17.Norberg M, Wall S, Boman K, Weinehall L. The Västerbotten intervention programme: background, design and implications. Glob Health Action. 2010;22:3. doi: 10.3402/gha.v3i0.4643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Burris JL, Wahlquist AE, Alberg AJ, et al. A longitudinal, naturalistic study of U.S. smokers’ trial and adoption of snus. Addict Behav. 2016;63:82–88. doi: 10.1016/j.addbeh.2016.07.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.The Swedish Hernia Register (SHR) www.svensktbrackregister.se. Accessed 10 Nov 2016
- 20.Ludvigsson JF, Otterblad-Olausson P, Pettersson BU, Ekbom A. The Swedish personal identity number: possibilities and pitfalls in healthcare and medical research. Eur J Epidemiol. 2009;24:659–667. doi: 10.1007/s10654-009-9350-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Norberg M, Blomstedt Y, Lönnberg G, et al. Community participation and sustainability–evidence over 25 years in the Västerbotten Intervention Programme. Glob Health Action. 2012;5:1–9. doi: 10.3402/gha.v5i0.19166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Nilsson H, Stylianidis G, Haapamäki M, Nilsson E, Nordin P. Mortality after groin hernia surgery. Ann Surg. 2007;245:656–660. doi: 10.1097/01.sla.0000251364.32698.4b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ashindoitiang JA, Ibrahim NA, Akinlolu OO. Risk factors for inguinal hernia in adult male Nigerians: a case control study. Int J Surg. 2012;10:364–367. doi: 10.1016/j.ijsu.2012.05.016. [DOI] [PubMed] [Google Scholar]
- 24.de Goede B, Timmermans L, van Kempen BJ, et al. Risk factors for inguinal hernia in middle-aged and elderly men: results from the Rotterdam Study. Surgery. 2015;157:540–546. doi: 10.1016/j.surg.2014.09.029. [DOI] [PubMed] [Google Scholar]
- 25.Liem MS, van der Graaf Y, Zwart RC, Geurts I, van Vroonhoven TJ. Risk factors for inguinal hernia in women: a case-control study. The Coala Trial Group Am J Epidemiol. 1997;146:721–726. doi: 10.1093/oxfordjournals.aje.a009347. [DOI] [PubMed] [Google Scholar]
- 26.Flich J, Alfonso JL, Delgado F, Prado MJ, Cortina P. Inguinal hernia and certain risk factors. Eur J Epidemiol. 1992;8:277–282. doi: 10.1007/BF00144814. [DOI] [PubMed] [Google Scholar]
- 27.Ruhl CE, Everhart JE. Risk factors for inguinal hernia among adults in the US population. Am J Epidemiol. 2007;165:1154–1161. doi: 10.1093/aje/kwm011. [DOI] [PubMed] [Google Scholar]
- 28.Rosemar A, Angerås U, Rosengren A. Body mass index and groin hernia: a 34-year follow-up study in Swedish men. Ann Surg. 2008;247:1064–1068. doi: 10.1097/SLA.0b013e31816b4399. [DOI] [PubMed] [Google Scholar]