Abstract
Objectives
To identify the impact of a full suite of health information technology (HIT) on the relationships that support safety and quality among intensive care unit (ICU) clinicians.
Data Sources
A year‐long comparative ethnographic study of three academic ICUs was carried out. A total of 446 hours of observational data was collected in the form of field notes. A subset of these observations—134 hours—was devoted to job‐shadowing individual clinicians and conducting a time study of their HIT usage.
Principal Findings
Significant variation in HIT implementation rates and usage was noted. Average HIT use on the two “high‐use” ICUs was 49 percent. On the “low‐use” ICU, it was 10 percent. Clinicians on the high‐use ICUs experienced “silo” effects with potential safety and quality implications. HIT work was associated with spatial, data, and social silos that separated ICU clinicians from one another and their patients. Situational awareness, communication, and patient satisfaction were negatively affected by this siloing.
Conclusions
HIT has the potential to accentuate social and professional divisions as clinical communications shift from being in‐person to electronically mediated. Socio‐technically informed usability testing is recommended for those hospitals that have yet to implement HIT. For those hospitals already implementing HIT, we suggest rapid, locally driven qualitative assessments focused on developing solutions to identified gaps between HIT usage patterns and organizational quality goals.
Keywords: Health information technology, ethnography, health care teamwork and communications
The last decade has seen significant policy interest in leveraging the benefits of health information technology (HIT) (Bates 2000; Bates and Gawande 2003; Blackwell 2008). The 2009 HITECH Act mandates the “meaningful use” of HIT across a range of clinical settings, providing $20 billion in support for the acquisition of technology, and withholding federal payments for Medicare and Medicaid patients from providers failing to demonstrate compliance (Blumenthal 2010; Blumenthal and Tavenner 2010). The primary policy goals behind encouraging the meaningful use of HIT focus on “improving the quality, safety, and efficiency of care” (Blumenthal 2010; Blumenthal and Tavenner 2010; Buntin, Jain, and Blumenthal 2010). In this paper, we present evidence from an observational study of Federal HIT policy “in action” on the front lines of care, describing care quality and safety effects that are unintended by policy makers. Our focus is on HIT's integration into everyday work on intensive care units (ICUs), showing how clinicians are adapting their relationships with one another by moving into spatial, data, and social silos to complete their policy‐mandated computer work. We also surface clinicians' concerns about the quality and safety implications of these newly siloed relationships.
With the Federal Government pursuing an aggressive HIT adoption timeline, there have been major investments in the sector (Ostrovsky et al. 2014), and implementation in both primary care and acute care settings has accelerated significantly since 2009 (Audet, Squires, and Doty 2014; Charles, Gabriel, and Furukawa 2014). Nonetheless, the cost effectiveness of hospital HIT systems has been challenged (Himmelstein, Wright, and Woolhandler 2010) and mixed evidence regarding the capacity of specific HIT software applications to reduce drug errors (Bates et al. 1998; Koppel et al. 2005; Georgiou et al. 2013; Schiff et al. 2015) has led to calls for further study and optimization (Schiff et al. 2016). There have also been warnings that a range of unintended consequences can accompany HIT implementation (Ash, Berg, and Coiera 2004; Han et al. 2005; Harrison, Koppel, and Bar‐Lev 2007), and a major review has acknowledged the criticality of “the human element” to successful HIT implementation (Buntin et al. 2011, p. 470). Specifically, while technical deficits such as poor planning, clinician computer literacy, and barely functional software are barriers to successful implementation (Kleinke 1998; Spetz, Keane, and Curry 2009; Trivedi et al. 2009), poor change leadership, the poor management of clinician expectations, and aggressive implementation timelines have been identified as central human and cultural challenges (Georgiou and Westbrook 2009; Ford et al. 2014). The increased cognitive load of HIT work, as well as its potential to disrupt the face‐to‐face communications that are central to delivering safe care, has also been identified as challenges in the literature (Pirnejad et al. 2009; Westbrook et al. 2013a; Taylor et al. 2014). Taken seriously by the community, these observations have led to calls for improved understandings of HIT as it affects hospital operational safety (Harrington et al. 2011; Middleton et al. 2013; Payne 2015).
The present paper examines HIT not as a single charting or prescribing application, but rather as an aggregate of “computer work” that shapes clinical relationships. We draw on a year‐long comparative study (Paradis et al. 2013) of three intensive care units (ICUs) to highlight the effects HIT is having on clinical relationships. We approach HIT as part of a “socio‐technical ensemble” (Bijker 1995), viewing technical infrastructures, and the clinicians who work with them, as two sides of a single coin (Bijker and Law 1992; MacKenzie and Wajcman 1999). HIT is on one hand a suite of hardware, software, and networks. On the other, it is a site of social interaction where health care professionals negotiate their relationships with one another and with their patients. We describe how ICU clinicians are integrating computer work into care routines and social relationships in ways that tend to build silos rather than the relationships that support safe, high‐quality care.
Methods
We conducted a comparative ethnography of three ICUs in three academic hospitals in two U.S. cities after gaining IRB approval from each institution. We observed HIT and interprofessional relationships on each unit simultaneously, giving the ICUs pseudonyms—Green Slope, Lakeside, and Mid Valley—to protect their anonymity. The units deployed high‐intensity ICU physician staffing, in which dedicated critical care specialists managed or comanaged patients (Pronovost et al. 2002). To improve comparability, we purposively recruited units that matched in medical specialty and bed count.
Our observations began with two researchers (ML and EP) acting as nonparticipant observers. From December 2012 to December 2013, a total of 446 hours of observations were carried out on the three units. Initial “fly on the wall” impressions were clarified with first informal and then formal interviews with staff and patient's family members. The informal interviews were conducted in natural breaks and pauses in the ICU workflow and sought to clarify the social meanings and motivations that informed clinicians' uses of HIT. The first of the semistructured formal interviews was conducted 4 months after nonparticipant observations began. All formal interviews were conducted in private spaces on the ICU, and digitally recorded and transcribed for analysis. Consistent with our inductive, grounded theory approach to data collection and analysis, these interviews were conducted as checks on emerging interpretations of the norms, roles, and values, we saw HIT occupying. In this way, the social meanings of computers in the ICU that we present here emerged from collaborative conversations with research participants who had the opportunity to refute or refine our socio‐technical interpretations. The researchers kept detailed field notes, recording observations and conversations within minutes of their occurrence, and then writing these up in more detail for future analysis.
Six months after the commencement of observations the ethnographers began conducting a time‐motion study. About 134 hours were spent job‐shadowing 32 nurses and 15 junior doctors. The nurses ranged from their first year in the profession to more than 10 years of experience in the ICU. The junior doctors ranged from their first to their third year of medical residency. Structuring observations in this way focused attention on individual front‐line clinicians and their interactions with their colleagues, patients, and the HIT infrastructure in their environment. These 47 job‐shadowing sessions enabled a time study focusing on the hours between 07:00 hours and 14:00 hours. This period is defined by nursing shift change at its beginning and the transition from medical rounds to care delivery for physicians at its end. See Table 1 for further descriptive statistics of the time study. We logged HIT usage by the minute, with partial minutes rounded up. Usage was defined as time spent using any HIT application or information source. We did not log time spent accessing the Internet or messaging services using privately owned devices, or for nonwork purposes. Table 1 provides descriptive statistics of our time study.
Table 1.
Time Study Descriptive Statistics
| Clinical Specialty | Observation Time (min) | HIT Usage (min) | Percentage Time on CIT | ||||
|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | SD | ||
| Lakeside | Staff nurse (n = 10) | 183 | 28.9 | 87 | 27.2 | 46 | 8.6 |
| Resident physician (n = 5) | 159 | 28.6 | 94 | 44.4 | 57 | 19.1 | |
| Mid Valley | Staff nurse (n = 10) | 183 | 4.4 | 84 | 21.4 | 46 | 11.1 |
| Resident physician (n = 5) | 179 | 7.0 | 86 | 49.1 | 48 | 28.2 | |
| Green Slope | Staff nurse (n = 12) | 181 | 9.5 | 18 | 7.6 | 10 | 4.1 |
| Resident physician (n = 5) | 180 | 0.0 | 7 | 8.2 | 4 | 4.5 | |
We carried out data analysis using the constant comparative method (Glaser and Strauss 1968; Boeije 2002) with initial themes identified, revisited, expanded, and collapsed in conversation between researchers, and researchers and participants prior to interpretation based on our socio‐technical approach. Theme identification and coding were facilitated by NVIVO10 software. EP and ML performed the coding, verifying one another's work. Extracts from the coded material—both interviews and field notes—are presented in the pages that follow to support our interpretation. The passages have been edited to ensure anonymity and clarity, with omissions or substitutions marked in square brackets.
Findings
HIT Infrastructure Variation
We found significant variation in HIT availability and usage between the three ICUs. For each computer that was available on Green Slope, 1.6 computers were available to clinicians on Lakeside and Mid Valley. Recalling that the units were matched in terms of bed size and staff roster, this meant many more computers were available to clinicians on Lakeside and Mid Valley.
Where Lakeside and Mid Valley had 10 and 11 computers, respectively, dedicated to physician use, Green Slope had none. Green Slope had no mobile work stations to support HIT work during rounds, while Lakeside and Mid Valley had 5 and 6 of these stations, respectively. Green Slope clinicians continued to perform significant analog steps in charting, prescribing, and communicating processes that were exclusively digital on Lakeside and Mid Valley.
These disparities in hardware and software availability translated into striking differences in usage (see Figure 1). A descriptive time study showed that the average Lakeside and Mid Valley clinician spent 49 percent of his or her time on a computer; at Green Slope he or she spent just 9 percent. Heavy HIT users on Lakeside and Mid Valley spent up to 90 percent of their time working on a computer. In contrast, the lightest HIT user on Green Slope spent no time at all working with HIT. Given this contrast between Green Slope on one hand, and Lakeside and Mid Valley on the other, we focus on the two heavy users as suggestive of how HIT usage can be integrated into the social and operational world of the ICU, and the care quality and safety consequences of this integration.
Figure 1.
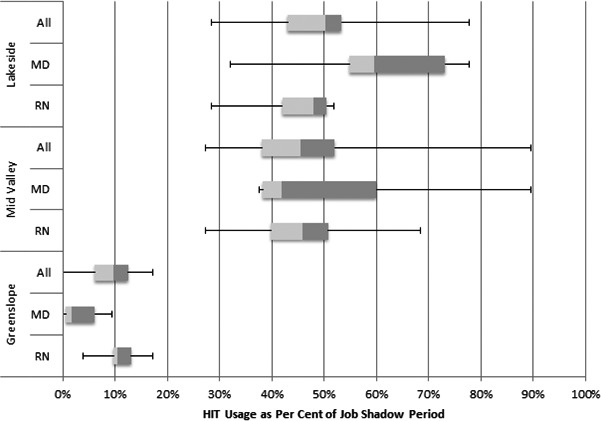
Time Study Interquartile Box Plots
HIT use at Lakeside and Mid Valley siloed clinicians from one another. The following sections describe how computer usage creates spatial, data, and social silos between ICU professionals. The last of these sections draws out not just evidence of social siloing, but of the safety and quality consequences that ICU clinicians and patients see in the loss of relationships.
Spatial Silos
Despite being connected electronically, clinicians tended to work in spatially isolated locations that were, informally if not formally, dedicated to their professional group. An illustrative example came during observations at Lakeside. One of the researchers walked into the room used by the doctors and found a Junior Resident working on a computer with ear buds in. After waving to get her attention, the researcher asked what she was listening to.
“Just ambient music in the background,” she says, a little shyly. [She then puts] her earbuds back in and begins to type again …
While the resident's sonic isolation was relatively unusual, her physical removal into another room, and the sense that to talk to those at work on a computer was to interrupt them, was the norm. In this way, HIT usage reflected social and professional divisions on the high‐use ICUs, with doctors working on “their” computers in one room and nurses on other computers in other locations. This is to say, HIT as it was deployed spatially on the units augmented the physical separation of the professions of putatively interprofessional teams: they were literally siloed. Physical and social effort was then required to track down colleagues from other professions and to interrupt them as they worked elsewhere.
In contrast, Green Slope's low‐HIT environment did not appear as spatially siloed. While their team interactions were not always ideal, clinicians on Green Slope were drawn, or even forced, into face‐to‐face conversations by their predominantly paper‐based information system. Green Slope's paper charts appeared to prevent staff from retiring into the spatial silos we observed on Lakeside and Mid Valley.
Data Silos
Clinicians on high‐use ICUs, in addition to being spatially siloed from one another along professional lines, tended to focus on the discrete subsets of data that were relevant to their profession alone. This data siloing saw nurses electronically documenting the care delivery activities in one place, and social workers adding notes in other virtual areas of patients' electronic charts. Although the system allowed data to be viewed by all, the boundaries of these professional data silos were seldom crossed. Doctors, in particular, isolated themselves from the data generated by other ICU team members. As an illustration, one Lakeside Staff RN remarked while typing up nursing notes on her patient that “no [doctors are] ever going to read what I'm writing here.” Similarly, a social worker at Mid Valley noted:
Nobody, in fact, reads social work notes. [As an example,] I just got a call last Friday [from the doctors];
“Can you please get started on the referral process for [a specific patient]?”
… I said, “Well, yeah, I've had referrals out on him for months.”
“Oh, you're working with him?!” [came the surprised reply.]
Meanwhile my notes are plastered all over his [electronic] chart. That's an example of how I can tell you that nobody reads my notes.
Green Slope's relationships appeared equally as siloed, with the alignment of the various paper‐based or partially online processes of nurses, social workers, and physicians requiring the extra effort of a face‐to‐face meeting. In this sense, while Lakeside and Mid Valley's data silos failed to meet the care coordination and communication‐enhancement goals of HIT policy, these silos seemed no less real on the low‐use unit.
Social Silos
Compounding the spatial and data challenges described above, the use of HIT tended to erect social silos rather than nurturing trust and fostering communication. The manifestations of this social siloing were described by clinicians as a fixation on HIT and an associated loss of familiarity. In turn, clinicians saw these phenomena as responsible for reductions in situational awareness and information flow, as well as missed opportunities for patient safety and care coordination.
An attending physician explained how he saw an intense focus on HIT usage negatively affecting the situational awareness of trainees on his unit.
The [junior doctors] tend to see the computer work as … well, they can get quite fixated. And it's a problem … because when you're not out here with the nurses, getting to know them on a first name basis, you're not really in touch with everything that's going on with the patients. (Lakeside)
This perspective was shared by a staff nurse who described how an HIT‐associated lack of social familiarity could redefine formerly routine colleague‐to‐colleague information transfers as “annoying.”
[Prior to the HIT system] You really knew the docs; you had access to them; and they were familiar faces. And with a familiar face, you know, you're willing to say “good morning” and to give updates … So it used to be better … When you add in the IT and everyone's busy doing their own thing, it [becomes] more of a challenge to stand up and go and give that annoying update. (Mid Valley)
A Lakeside charge nurse described how he saw patient safety and care quality checks as embedded in, and facilitated by, the face‐to‐face contact that HIT use undermined:
Back in the day, the doctors wrote an order on the bedside chart. … And that would give me what I call face time with that physician. [Time where] there's give and take. Today, they put that order in the computer. It comes up on my screen. It goes to pharmacy … It goes everywhere. And … there's never face time unless I run back to them and say [something] and I don't always have the opportunity to run back because I'm tending to the computer.
Similarly, the loss of interprofessional “face time” that included “give and take” for discussing treatment plans was seen as a negative influence on care coordination.
The vision [when HIT was adopted] was everybody would chart in this one system. So, the nurses would have a better holistic view of the patient versus having to have a discussion [with the doctors]. They could easily click through documents and put the big picture together about a patient. So, that was very appealing to nursing … but nursing had an issue with the communication piece, because they felt like the prescribers would talk to them even less than they did before, and that's come true. Unless the nurse approaches the physician … about an order or something like that, there's no explanation behind it. (Mid Valley, Charge RN)
In contrast, the Green Slope ICU's continued reliance on analog treatment and drug ordering charts appeared to build relationships and lines of communication rather than silos. The paper charts acted as points of inter‐ and intraprofessional contact, with clinicians obliged to gather around them to make sense of the various data streams in the course of face‐to‐face interactions.
The HIT‐associated social silos that separated ICU physicians and nurses on Lakeside and Mid Valley were replicated in the relationships between non‐ICU physicians and ICU nurses. It was common for non‐ICU doctors from consulting services (e.g., renal, surgery, infectious diseases) to interact with or physically assess patients on Lakeside and Mid Valley without talking to the staff nurses responsible for those patients. This, despite the fact that the staff nurse was often working on a computer at or near the threshold of the patient's room. One nurse, exasperated as a group of doctors left the room outside of which she had been completing her electronic charting work, noted:
I'm like totally protective of my patients and people are constantly dropping by and don't introduce themselves and go in and leave. Drives me nuts! Aren't you even going to give me an update? What were you looking for? I mean, they could be in there selling Girl Scout cookies for all I know! (Mid Valley, Staff RN)
Although we observed this phenomenon less often between ICU‐based doctors and ICU‐based nurses, it still happened. It was also not an exclusively interprofessional (i.e., physician‐to‐nurse) issue. Intraprofessionally (i.e., physician‐to‐physician), ICU‐based doctors found their non‐ICU colleagues often behaved in a HIT‐siloed manner. A Lakeside Fellow described how non‐ICU doctors would often,
Just walk out of the [patient's] room. And if you're lucky enough to catch them [in the hallway], they'll tell you: “you can look it up in my [electronic] notes,” rather than talk to you.
The spatial and information silos that HIT usage erected between ICU clinicians resulted in less face‐to‐face contact, which was in turn seen as critical to not just maintaining familiarity and trust, but the flow of information on which well‐timed, well‐targeted, well‐coordinated care relied.
HIT‐associated social siloing extended beyond relationships among clinicians: it also shaped their interactions with patients. One family member on Mid Valley described his experience of daily rounds on the ICU as one where the physicians clustered around mobile computers in the hallway just outside the room. Despite being within earshot, he felt as if he were a world away.
They look at the numbers and ignore the patient. And that is bothersome, in my opinion. I still think there needs to be a little bit of a holistic approach to a patient instead of just listening to all the numbers and then walking on by to the next one. (Mid Valley, Family Member)
In this way, computer work isolated physicians from their patients, with the digital representation, or iPatient (Verghese 2008; Wachter 2015), often becoming the central focus of doctors' efforts and discussion. In contrast, the core work of nurses and other allied health providers—which required direct physical interaction with patients rather than their electronic data doubles—appeared to be less socially siloed. As the preceding family member's comments suggest, there could be serious patient satisfaction and experience risks associated with this approach to integrating HIT into the ICU environment.
In contrast, with less HIT infrastructure, Green Slope clinicians—and nurses in particular—spent more time in direct contact with their patients. While time was spent on documentation, and performing analog bridge work for their electronic systems, we observed that Green Slope clinicians appeared less focused on their iPatients' data streams and the tasks of managing information flow.
Discussion
Our study reports the findings of ethnographic research on three ICUs targeting staff experiences of HIT. Building on findings that the introduction of new software applications into clinical environments can reduce contact between doctors and nurses (Westbrook et al. 2013b), we show that HIT is implicated in the spatial, data, and social siloing of Lakeside and Mid Valley's clinicians from one another, and their patients. Performing HIT work in physically isolated spaces, clinicians worked in data silos, writing notes that colleagues from other professions were unlikely to read. HIT‐induced social siloing was seen by ICU nurses and doctors as led by an increased focus on computer work that reduced familiarity. The perceived consequences of being unfamiliar, or socially siloed, were reductions in the following: clinicians' situational awareness beyond their professional expertise; communications that supported care coordination, as well as patient safety and quality updates, and opportunities to gather team wisdom and perspectives; and patient and family satisfaction as clinicians were seen as focused on the iPatient rather than the physical and social body in the bed (Verghese 2008; Toll 2012; Chi and Verghese 2014; Zuger 2014; Wachter 2015).
While our findings could indicate that the HIT systems at Lakeside and Mid Valley created the communications challenges reported by our participants, analyzing them through a socio‐technical lens suggests that HIT may exacerbate long‐standing interprofessional issues and preexisting deficits in team cohesion (Graetz et al. 2014). Approaching HIT and the ICU teams as a socio‐technical ensemble (Bijker 1995) suggests computer work was folded into the hierarchical interprofessional and clinical relationships that prevail on units like Lakeside and Mid Valley. In the context of a long and uneasy history between nurses and doctors simultaneously working to care for patients and maintain jurisdiction over discrete areas of expertise (Stein 1967; Stein, Watts, and Howell 1990; Willis and Parish 1997; Paradis and Whitehead 2015), HIT appears to have been absorbed into a tendency to work independently. Recall that the low‐use unit, Green Slope, also exhibited data siloing. In this sense, the software design characteristics, spatial placement of computers, and communication patterns resulting from the structure of Lakeside and Mid Valley's HIT systems were interpreted and enacted by clinicians using familiar social models that emphasized division rather than collaboration.
The variation we observed in hardware and software availability, as well as HIT usage, suggest that, at least among academic hospitals, the HITECH Act's provisions (Blumenthal 2010) have resulted in a patchwork of approaches and implementation rates. However, as one influential commentator argues, there is no going back in the electronic health information revolution: there will be no return to paper (Blumenthal 2014). With this reality acknowledged, Green Slope's relative backwardness in HIT terms, but forwardness in relationship terms, suggests local hospital implementation protocols can still be amended to avoid the siloing experiences of Lakeside and Mid Valley. Thoughtful implementation that pays attention to how HIT is integrated into the spatial, data, and social environments of acute care becomes even more crucial in the context of the Federal Government's accelerated timeline for HIT adoption. As clinicians on units like Green Slope move toward spending nearly half their time on computers, the siloing experienced by Lakeside and Mid Valley represent a learning opportunity. On Green Slope, paper forms and charts provided time and space for clinical team members to share treatment plans, status updates, and safety concerns. Recreating these physical and social spaces in the digital age is, we argue, a central challenge for HIT designers and clinician implementers. This should be a key focus of future usability research that takes a broad socio‐technical view of the HIT implementation context and operationalizes calls for building in‐hospital capacity in this area (Russ et al. 2012; Atkins and Cullen 2013).
For academic and community hospitals that have already moved toward HIT suites like those of Lakeside and Mid Valley, assessments of how computers are contributing to, or detracting from, an organization's care quality and safety goals will be of central importance. Hospital leaders interested in identifying areas where spatial, data, or social silos are being built, or exacerbated, by HIT will likely need to use qualitative methods. Rapid, highly focused versions of the ethnographic study presented here are one excellent method for surfacing disconnects between HIT usage and hospital care quality goals. A promising variant of this approach is video reflexive ethnography (VRE), which engages the wisdom and experience of clinical teams in self‐reflection on their practices (Iedema et al. 2006; Iedema 2011; Iedema, Mesman, and Carroll 2013). VRE's light‐touch, bottom‐up approach to understanding and remediating health care quality issues is well suited to tapping local wisdom to ensure that the spaces inhabited by clinicians, patients, and computers foster interaction rather than discourage it. Ethnography generally and VRE specifically are well suited to adapting local policies that create and standardize the moments of interprofessional contact (Pronovost et al. 2003; Schwartz et al. 2008) that in turn facilitate interaction rather than spatial, data, and social silos.
While the detailed data that ethnography collects offer a unique way to cut through the noise of multiple interventions and so generate descriptions of Federal HIT policy in action, there are also limitations to this methodology, and to our choice of ICUs as observation sites. As with all observational studies, our data come from specific locations at particular moments in time. Our analysis and theoretically informed efforts to transcend these specifics and so draw out broader lessons will have been shaped by our own biases as social scientists. Although we have followed best practices in the field of health care ethnography (Leslie et al. 2014)—refining our interpretation of the data by consulting with our participants—our findings may not generalize to other ICUs or hospitals. In this way, further localized assessments aimed at surfacing any HIT‐associated siloing issues and generating locally viable solutions are necessary.
Our study does not include measurements of clinical outcomes or patients' experiences of care, and as such it is unable to provide more than first‐level perspectives on the safety and quality implications of implementing HIT. Further quantitative research testing the clinician‐generated thesis that HIT usage is limiting information flow and so jeopardizing safety might include examinations of rates of communication, sentinel events, and health care‐acquired infections on ICUs before and after the implementation of computers. Similarly, research focused on the patient satisfaction consequences to HIT usage will add depth to the descriptive findings presented here. This will be particularly important given existing research in the ambulatory care setting, suggesting that when providers spend less time with patients, satisfaction scores also decrease (Lin et al. 2001).
Conclusion
HIT has the potential to accentuate social and professional divisions as clinical communications shift from being in‐person to electronically mediated. To mitigate these effects at hospitals that have yet to implement, we recommend localized preimplementation usability testing that is socio‐technically informed. For those hospitals already in the implementation phase, we recommend postimplementation assessments that target gaps between HIT usage and quality goals that are aimed at creating locally viable solutions.
Supporting information
Appendix SA1: Author Matrix.
Acknowledgments
Joint Acknowledgment/Disclosure Statement: The research supporting this manuscript was funded by the Gordon and Betty Moore Foundation. The authors thank the anonymous reviewers and editors at Health Services Research for their valuable critiques.
Disclosures: None.
Disclaimers: None.
References
- Ash, J. S. , Berg M., and Coiera E.. 2004. “Some Unintended Consequences of Information Technology in Health Care: The Nature of Patient Care Information System‐related Errors.” Journal of the American Medical Informatics Association 11 (2): 104–12. doi:10.1197/jamia.M1471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Atkins, D. , and Cullen T.. 2013. “The Future of Health Information Technology: Implications for Research.” Medical Care 51 (3 Suppl. 1): S1–3. doi:10.1097/MLR.0b013e3182848a52. [DOI] [PubMed] [Google Scholar]
- Audet, A. M. , Squires D., and Doty M. M.. 2014. “Where Are We on the Diffusion Curve? Trends and Drivers of Primary Care Physicians' Use of Health Information Technology.” Health Services Research 49 (1 Pt 2): 347–60. doi:10.1111/1475‐6773.12139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bates, D. W. 2000. “Using Information Technology to Reduce Rates of Medication Errors in Hospitals.” British Medical Journal 320 (7237): 788–91. doi:10.1136/bmj.320.7237.788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bates, D. W. , and Gawande A. A.. 2003. “Improving Safety with Information Technology.” New England Journal of Medicine 348 (25): 2526–34. doi:10.1056/NEJMsa020847. [DOI] [PubMed] [Google Scholar]
- Bates, D. W. , Leape L. L., Cullen D. J., Laird N., Petersen L. A., Teich J. M., Burdick E., Hickey M., Kleefield S., Shea B., Vander Vliet M., and Seger D. L.. 1998. “EFfect of Computerized Physician Order Entry and a Team Intervention on Prevention of Serious Medication Errors.” Journal of the American Medical Association 280 (15): 1311–6. doi:10.1001/jama.280.15.1311. [DOI] [PubMed] [Google Scholar]
- Bijker, W. E. 1995. Of Bicycles, Bakelites, and Bulbs: Toward a Theory of Sociotechnical Change. Cambridge, MA: MIT Press. [Google Scholar]
- Bijker, W. E. , and Law J.. 1992. Shaping Technology/Building Society: Studies in Sociotechnical Change. Cambridge, MA: MIT Press. [Google Scholar]
- Blackwell, G. 2008. “The Future of IT in Healthcare.” Informatics for Health & Social Care 33 (4): 211–326. [DOI] [PubMed] [Google Scholar]
- Blumenthal, D. 2010. “Launching HITECH.” New England Journal of Medicine 362 (5): 382–5. doi:10.1056/NEJMp0912825. [DOI] [PubMed] [Google Scholar]
- Blumenthal, D. 2014. “Electronic Health Records: The New Lightning Rod in Health Care.” The Commonwealth Fund. Available at http://www.commonwealthfund.org/publications/blog/2014/oct/ehrs-the-new-lightning-rod-in-health-care.
- Blumenthal, D. , and Tavenner M.. 2010. “The ‘Meaningful Use’ Regulation for Electronic Health Records.” New England Journal of Medicine 363 (6): 501–4. doi:10.1056/NEJMp1006114. [DOI] [PubMed] [Google Scholar]
- Boeije, H. 2002. “A Purposeful Approach to the Constant Comparative Method in the Analysis of Qualitative Interviews.” Quality & Quantity 36 (4): 391–409. doi:10.1023/A:1020909529486. [Google Scholar]
- Buntin, M. B. , Jain S. H., and Blumenthal D.. 2010. “Health Information Technology: Laying the Infrastructure for National Health Reform.” Health Affairs 29 (6): 1214–9. doi:10.1377/hlthaff.2010.0503. [DOI] [PubMed] [Google Scholar]
- Buntin, M. B. , Burke M. F., Hoaglin M. C., and Blumenthal D.. 2011. “The Benefits of Health Information Technology: A Review of the Recent Literature Shows Predominantly Positive Results.” Health Affairs 30 (3): 464–71. doi:10.1377/hlthaff.2011.0178. [DOI] [PubMed] [Google Scholar]
- Charles, D. , Gabriel M., and Furukawa M. F.. 2014. Adoption of Electronic Health Record Systems among U.S. Non‐Federal Acute Care Hospitals: 2008–2013, no. 16. Washington, DC: ONC Data Brief. [Google Scholar]
- Chi, J. , and Verghese A.. 2014. “Clinical Education and the Electronic Health Record: The Flipped Patient.” Journal of the American Medical Association 312 (22): 2331–2. doi:10.1001/jama.2014.12820. [DOI] [PubMed] [Google Scholar]
- Ford, E. W. , Pettit L., Silvera G., and Huerta T.. 2014. “EMR Implementation Speed: Patient Safety Culture Paradox.” Journal of Healthcare Information Management 28 (3): 24–31. [Google Scholar]
- Georgiou, A. , and Westbrook J.. 2009. “Clinician Reports of the Impact of Electronic Ordering on an Emergency Department.” Studies in Health Technology and Informatics 150: 678–82. [PubMed] [Google Scholar]
- Georgiou, A. , Prgomet M., Paoloni R., Creswick N., Hordern A., Walter S., and Westbrook J.. 2013. “The Effect of Computerized Provider Order Entry Systems on Clinical Care and Work Processes in Emergency Departments: A Systematic Review of the Quantitative Literature.” Annals of Emergency Medicine 61 (6): 644–53.e16. doi:10.1016/j.annemergmed.2013.01.028. [DOI] [PubMed] [Google Scholar]
- Glaser, B. G. , and Strauss A. L.. 1968. The Discovery of Grounded Theory: Strategies for Qualitative Research. New York: Aldine de Gruyter. [Google Scholar]
- Graetz, I. , Reed M., Shortell S. M., Rundall T. G., Bellows J., and Hsu J.. 2014. “The Association between EHRs and Care Coordination Varies by Team Cohesion.” Health Services Research 49 (1 Pt 2): 438–52. doi:10.1111/1475‐6773.12136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Han, Y. Y. , Carcillo J. A., Venkataraman S. T., Clark R. S. B., Watson R. S., Nguyen T. C., Bayir H., and Orr R. A.. 2005. “Unexpected Increased Mortality after Implementation of a Commercially Sold Computerized Physician Order Entry System.” Pediatrics 116: 1506–12. [DOI] [PubMed] [Google Scholar]
- Harrington, L. , Kennerly D. M. D., Johnson C., and Fache Snyder D.. 2011. “Safety Issues Related to the Electronic Medical Record (EMR): Synthesis of the Literature from the Last Decade, 2000‐2009/PRACTITIONER APPLICATION.” Journal of Healthcare Management 56 (1): 31–43; discussion 43–4. [PubMed] [Google Scholar]
- Harrison, M. I. , Koppel R., and Bar‐Lev S.. 2007. “Unintended Consequences of Information Technologies in Health Care—An Interactive Sociotechnical Analysis.” Journal of the American Medical Informatics Association 14 (5): 542–9. doi:10.1197/jamia.M2384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Himmelstein, D. U. , Wright A., and Woolhandler S.. 2010. “Hospital Computing and the Costs and Quality of Care: A National Study.” American Journal of Medicine 123 (1): 40–6. [DOI] [PubMed] [Google Scholar]
- Iedema, R. 2011. “Creating Safety by Strengthening Clinicians' Capacity for Reflexivity.” British Medical Journal Quality and Safety 20 (Suppl 1): i83–6. doi:10.1136/bmjqs.2010.046714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iedema, R. , Mesman J., and Carroll K.. 2013. Visualising Health Care Practice Improvement: Innovation from within. London: Radcliffe. [Google Scholar]
- Iedema, R. , Rowena Forsyth A., Georgiou J. Braithwaite., and Westbrook J.. 2006. “Video Research in Health: Visibilising the Effects of Computerising Clinical Care.” Qualitative Research Journal 6 (2): 15–30. [Google Scholar]
- Kleinke, J. D. 1998. “Release 0.0: Clinical Information Technology in the Real World.” Health Affairs 17 (6): 23–38. doi:10.1377/hlthaff.17.6.23. [DOI] [PubMed] [Google Scholar]
- Koppel, R. , Metlay J. P., Cohen A., et al. 2005. “Role of Computerized Physician Order Entry Systems in Facilitating Medication Errors.” Journal of the American Medical Association 293 (10): 1197–203. doi:10.1001/jama.293.10.1197. [DOI] [PubMed] [Google Scholar]
- Leslie, M. , Paradis E., Gropper M. A., Reeves S., and Kitto S.. 2014. “Applying Ethnography to the Study of Context in Healthcare Quality and Safety.” British Medical Journal Quality and Safety 23 (2): 99–105. [DOI] [PubMed] [Google Scholar]
- Lin, C. , Albertson G. A., Schilling L. M., et al. 2001. “Is Patients' Perception of Time Spent with the Physician a Determinant of Ambulatory Patient Satisfaction?” Archives of Internal Medicine 161 (11): 1437–42. doi:10.1001/archinte.161.11.1437. [DOI] [PubMed] [Google Scholar]
- MacKenzie, D. A. , and Wajcman J.. 1999. The Social Shaping of Technology, 2nd Edition Buckingham, UK: Open University Press. [Google Scholar]
- Middleton, B. , Bloomrosen M., Dente M. A., Hashmat B., Koppel J. R., Overhage M., Payne T. H., Rosenbloom S. T., Weaver C., and Zhang J.. 2013. “Enhancing Patient Safety and Quality of Care by Improving the Usability of Electronic Health Record Systems: Recommendations from AMIA.” Journal of the American Medical Informatics Association 20 (e1): e2–8. doi:10.1136/amiajnl‐2012‐001458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ostrovsky, A. , Deen N., Simon A., and Mate K.. 2014. A Framework for Selecting Digital Health Technology. IHI Innovation Report. Cambridge, MA: Institute for Healthcare Improvement. [Google Scholar]
- Paradis, E. , and Whitehead C. R.. 2015. “Louder Than Words: Power and Conflict in Interprofessional Education Articles, 1954–2013.” Medical Education 49 (4): 399–407. doi:10.1111/medu.12668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paradis, E. , Reeves S., Leslie M., Aboumatar H., Chesluk B., Clark P., Courtenay M., Franck L., Lamb G., Lyndon A., Mesman J., Puntillo K., Schmitt M., van Soeren M., Wachter B., Zwarenstein M., Gropper M., and Kitto S.. 2013. “Exploring the Nature of Interprofessional Collaboration and Family Member Involvement in an Intensive Care Context.” Journal of Interprofessional Care 28 (1): 74–5. doi:10.3109/13561820.2013.781141. [DOI] [PubMed] [Google Scholar]
- Payne, T. H. 2015. “Electronic Health Records and Patient Safety: Should We Be Discouraged?” British Medical Journal Quality and Safety 24 (4): 239–40. doi:10.1136/bmjqs‐2015‐004039. [DOI] [PubMed] [Google Scholar]
- Pirnejad, H. , Niazkhani Z., van der Sijs H., Berg M., and Bal R.. 2009. “Evaluation of the Impact of a CPOE System on Nurse‐Physician Communication—A Mixed Method Study.” Methods of Information in Medicine 48 (4): 350–60. doi:10.3414/ME0572. [DOI] [PubMed] [Google Scholar]
- Pronovost, P. J. , Angus D. C., Dorman T., Robinson K. A., Dremsizov T. T., and Young T. L.. 2002. “Physician Staffing Patterns and Clinical Outcomes in Critically Ill Patients: A Systematic Review.” Journal of the American Medical Association 288 (17): 2151–62. doi:10.1001/jama.288.17.2151. [DOI] [PubMed] [Google Scholar]
- Pronovost, P. , Berenholtz S., Dorman T., Lipsett P. A., Simmonds T., and Haraden C.. 2003. “Improving Communication in the ICU Using Daily Goals.” Journal of Critical Care 18 (2): 71–5. [DOI] [PubMed] [Google Scholar]
- Russ, A. L. , Weiner M., Russell S. A., Baker D. A., Fahner W. J., and Saleem J. J.. 2012. “Design and Implementation of a Hospital‐Based Usability Laboratory: Insights from a Department of Veterans Affairs Laboratory for Health Information Technology.” Joint Commission Journal on Quality and Patient Safety 38 (12): 531–40. [DOI] [PubMed] [Google Scholar]
- Schiff, G. D. , Amato M. G., Eguale T., Boehne J. J., Wright A., Koppel R., Rashidee A. H., Elson R. B., Whitney D. L., Thach T. T., Bates D. W., and Seger A. C.. 2015. “Computerised Physician Order Entry‐Related Medication Errors: Analysis of Reported Errors and Vulnerability Testing of Current Systems.” British Medical Journal Quality and Safety 24 (4): 264–71. doi:10.1136/bmjqs‐2014‐003555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schiff, G. D. , Hickman T.‐T. T., Volk L. A., Bates D. W., and Wright A.. 2016. “Computerised Prescribing for Safer Medication Ordering: Still a Work in Progress.” British Medical Journal Quality and Safety 25 (5): 315–19. [DOI] [PubMed] [Google Scholar]
- Schwartz, J. M. , Nelson K. L., Saliski M., Hunt E. A., and Pronovost P. J.. 2008. “The Daily Goals Communication Sheet: A Simple and Novel Tool for Improved Communication and Care.” Joint Commission Journal on Quality and Patient Safety 34 (10): 608–13, 561. [DOI] [PubMed] [Google Scholar]
- Spetz, J. , Keane D., and Curry S. A. F.. 2009. “Information Technology Implementation in a Rural Hospital: A Cautionary Tale.” Journal of Healthcare Management 54 (5): 337–47; discussion 348. [PubMed] [Google Scholar]
- Stein, L. I. 1967. “The Doctor‐Nurse Game.” Archives of General Psychiatry 16 (6): 699–703. [DOI] [PubMed] [Google Scholar]
- Stein, L. I. , Watts D. T., and Howell T.. 1990. “The Doctor‐Nurse Game Revisited.” New England Journal of Medicine 322 (8): 546–9. doi:10.1056/nejm199002223220810. [DOI] [PubMed] [Google Scholar]
- Taylor, S. P. , Ledford R., Palmer V., and Abel E.. 2014. “We Need to Talk: An Observational Study of the Impact of Electronic Medical Record Implementation on Hospital Communication.” British Medical Journal Quality and Safety 23 (7): 584–8. doi:10.1136/bmjqs‐2013‐002436. [DOI] [PubMed] [Google Scholar]
- Toll, E. 2012. “The Cost of Technology.” Journal of the American Medical Association 307 (23): 2497–8. doi:10.1001/jama.2012.4946. [DOI] [PubMed] [Google Scholar]
- Trivedi, M. , Daly E., Kern J., Grannemann B., Sunderajan P., and Claassen C.. 2009. “Barriers to Implementation of a Computerized Decision Support System for Depression: An Observational Report on Lessons Learned in ‘Real World’ Clinical Settings.” BMC Medical Informatics and Decision Making 9 (1): 6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Verghese, A. 2008. “Culture Shock—Patient as Icon, Icon as Patient.” New England Journal of Medicine 359 (26): 2748–51. doi:10.1056/NEJMp0807461. [DOI] [PubMed] [Google Scholar]
- Wachter, R. M. 2015. “Chapter 3: The iPatient” In The Digital Doctor: Hope, Hype, and Harm at the Dawn of Medicine's Computer Age, pp. 23–28. New York: McGraw Hill Education. [Google Scholar]
- Westbrook, J. I. , Baysari M. T., Li L., Burke R., Richardson K. L., and O'Day R.. 2013a. “The Safety of Electronic Prescribing: Manifestations, Mechanisms, and Rates of System‐Related Errors Associated with Two Commercial Systems in Hospitals.” Journal of the American Medical Informatics Association 20 (6): 1159–67. doi:10.1136/amiajnl‐2013‐001745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Westbrook, J. I. , Li L., Georgiou A., Paoloni R., and Cullen J.. 2013b. “Impact of an Electronic Medication Management System on Hospital Doctors' and Nurses' Work: A Controlled Pre–Post, Time and Motion Study.” Journal of the American Medical Informatics Association 20 (6): 1150–8. doi:10.1136/amiajnl‐2012‐001414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Willis, E. , and Parish K.. 1997. “Managing the Doctor‐Nurse Game: A Nursing and Social Science Analysis.” Contemporary Nurse 6 (3–4): 136–44. [DOI] [PubMed] [Google Scholar]
- Zuger, A. 2014. “With Electronic Medical Records, Doctors Read When They Should Talk.” New York Times, October 13, 2014. Available at http://well.blogs.nytimes.com/2014/10/13/with-electronic-medical-records-doctors-read-when-they-should-talk/?_r=0. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix SA1: Author Matrix.


