Abstract
Objective
To determine if recent growth in hospital and physician electronic health record (EHR) adoption and use is correlated with decreases in expenditures for elderly Medicare beneficiaries.
Data Sources
American Hospital Association (AHA) General Survey and Information Technology Supplement, Health Information Management Systems Society (HIMSS) Analytics survey, SK&A Information Services, and the Centers for Medicare & Medicaid Services (CMS) Chronic Conditions Data Warehouse Geographic Variation Database for 2010 through 2013.
Study Design
Fixed effects model comparing associations between hospital referral region (HRR) level measures of hospital and physician EHR penetration and annual Medicare expenditures for beneficiaries with one of four chronic conditions. Calculated hospital penetration rates as the percentage of Medicare discharges from hospitals that satisfied criteria analogous to Meaningful Use (MU) Stage 1 requirements and physician rates as the percentage of physicians using ambulatory care EHRs.
Principal Findings
An increase in the hospital penetration rate was associated with a small but statistically significant decrease in total Medicare and Medicare Part A acute care expenditures per beneficiary. An increase in physician EHR penetration was also associated with a significant decrease in total Medicare and Medicare Part A acute care expenditures per beneficiary as well as a decrease in Medicare Part B expenditures per beneficiary. For the study population, we estimate approximately $3.8 billion in savings related to hospital and physician EHR adoption during 2010–2013. We also found that an increase in physician EHR penetration was associated with an increase in lab test expenses.
Conclusions
Health care markets that had steeper increases in EHR penetration during 2010–2013 also had steeper decreases in total Medicare and acute care expenditures per beneficiary. Markets with greater increases in physician EHR had greater declines in Medicare Part B expenditures per beneficiary.
Keywords: Electronic health record, EHR, Health IT, meaningful use, Medicare expenditures
The 2009 Health Information Technology for Economic and Clinical Health (HITECH) Act, which includes the Medicare and Medicaid Electronic Health Record (EHR) Incentive Programs, was designed to increase the adoption and use of electronic health records by hospitals and physicians. The long‐term goal was to change the way information is used across the health care system and generate increased efficiency as well as enhanced individual and population health. This study provides evidence of the relationship between increasing health information technology (IT) use and Medicare expenditures for elderly beneficiaries with four common chronic conditions: chronic obstructive pulmonary disease (COPD), congestive heart failure (CHF), diabetes, and ischemic heart disease (IHD). As these patients have high health care utilization and receive care across multiple providers, they present an interesting test case for the impact on utilization and costs of new adoption and use of EHRs.
Although health care produces much value—for example, through increased life expectancy (Skinner, Staiger, and Fisher 2006; Ford et al. 2007; Chernew and Newhouse 2012) and improved quality of life (Chernew and Newhouse 2012)—there is also evidence of considerable waste (Berwick and Hackbarth 2012). Some evidence for wasteful health care spending comes from the literature documenting large regional variation in health care spending that cannot be explained by health status, prices, or income (Skinner 2011). Moreover, this variation has been shown to persist over time, such that relatively high‐cost hospital referral regions (HRRs) tend to remain high cost over recent decades (Chicklis et al. 2015). Waste likely results from a number of sources, including lack of widespread adoption of known best practices, failures of care coordination, and use of inappropriate treatments.
Effective health IT use may alleviate some waste (Berwick and Hackbarth 2012). For example, multiple studies have found that automated dose calculations in computerized provider order entry (CPOE) systems produce significant reductions in medication errors (Jones et al. 2014), which in turn should reduce the need for corrective care, thus yielding cost savings. Previous research has found that electronic prescribing to Medicare beneficiaries reduces the incidence of adverse drug events (ADEs) in both hospitals and ambulatory care settings (Encinosa and Bae 2015; Powers et al. 2015). In addition, use of the health information exchange (HIE) capability of health IT can contribute to reductions in redundant care. HIE capability was among the objectives for Stage 1 Meaningful Use (MU) of EHRs during the first 2 years of the EHR Incentive Programs (2011 and 2012) and was changed to an objective for MU Stage 2 in 2013 (CMS 2012). The Office of the National Coordinator for Health Information Technology (ONC) has also made HIE a policy priority in the hope that it could lead to lower health care costs through the identification and reduction of waste (ONC 2015a). Indeed, recent research has found evidence that HIE does reduce some forms of utilization and costs in emergency departments (Frisse et al. 2012; Bailey et al. 2013a,b; Lammers, Adler‐Milstein, and Kocher 2014), and hospitals that use at least a basic EHR and participate in health information organizations are more likely to engage in HIE (Furukawa et al. 2013). However, evidence for effects of HIE in settings other than emergency departments is not well established at this time (Rudin et al. 2014; Rahurkar, Vest, and Menachemi 2015).
Previous studies have examined the relationship between health IT and costs before HITECH's enactment. Agha examined a nationwide sample of hospitals and Medicare claims data for the period 1998–2005 and found that hospital medical expenditures increased by 1.3 percent after EHR adoption (Agha 2014). Furukawa and colleagues (Furukawa, Raghu, and Shao 2010) estimated 6–10 percent higher costs per discharge attributable to electronic medical record (EMR) implementation in a sample of California hospitals during 1998–2007. Dranove and colleagues (Dranove et al. 2012) found higher hospital operating costs in the short term attributable to adoption of EHR but evidence of declining costs after 3 years among hospitals in locations that favored complementarities with health IT—for example, locations heavily populated by other industries (such as communications, business services, finance, and electronic components) that are heavy IT users. Such regions provide a richer labor market of workers with specialized IT‐related skills that can more readily enable hospitals to find the workforce they need to adapt to the newly adopted technology.
This paper updates and complements the previous provider‐level analyses with a market‐level study, thus contributing to a better understanding of the relationship between EHR adoption and use and the costs of care for Medicare beneficiaries with certain chronic conditions. In particular, we examine changes in EHR penetration rates at the market level among both hospitals and physician offices between 2010 and 2013, when the financial incentives were implemented for providers satisfying the Stage 1 objectives for MU of EHRs (Blumenthal and Tavenner 2010; Centers for Medicare and Medicaid Services 2014). We use the HRR as our definition of a market. HRRs are defined by the Dartmouth Atlas of Health Care as regional markets based around hospitals providing major cardiovascular surgical procedures and neurosurgery to Medicare patients (Dartmouth Atlas of Health Care Working Group 1998). While previous research has found a cross‐sectional correlation between physician EHR use and expenditures (McLaughlin and Lammers 2015), the present study is among the first to examine the relationship of physician EHR adoption and use in ambulatory settings to costs using panel data. This study contributes to understanding whether policy interventions such as EHR diffusion can alter the persistence of cost variation across HRRs (Chicklis et al. 2015).
We hypothesize that EHRs enable hospitals and ambulatory care physicians to manage complex clinical information about patients more efficiently, thus allowing them to deliver care at a lower cost than they otherwise would without the use of EHRs (Hagen et al. 2008). Furthermore, social norms and the flow of information through local professional and social networks, which have been hypothesized to contribute to regional variations in health care utilization and spending (Phelps 2000; Skinner and Staiger 2007, 2009), may also contribute to how effectively EHRs are implemented within provider markets. In a widely cited New Yorker article exploring broad differences in health care expenditures among neighboring communities, Atul Gawande posited the role of leading local institutions, such as hospitals and physician groups, in setting practice norms within markets (Gawande 2009). In this study we seek evidence about whether expanding EHR use is associated with a reversal of these dynamics and thus with a reduction in spending among health care markets.
Based on a review of prior literature describing health IT's intended impacts on costs (Hagen et al. 2008; McCormick et al. 2012; Agha 2014), we identified five expenditure categories to use as dependent variables: (1) total Medicare Part A and Part B expenditures (from here on referred to as “total Medicare fee‐for‐service [FFS] expenditures”); (2) Part A expenditures for acute care hospital inpatient care; (3) total Part B expenditures; (4) Part B expenditures for imaging services from hospital outpatient departments and noninstitutional providers; and (5) Part B expenditures for laboratory tests from hospital outpatient departments and noninstitutional providers.
Data and Methods
We used regression analysis of longitudinal data on annual HRR‐level measures of hospital and physician office adoption of EHR and annual FFS expenditures for Medicare beneficiaries age 65 or older with at least one of four chronic conditions: COPD, CHF, diabetes, and IHD. Our analytic sample consists of a balanced panel of 306 HRRs over 4 years—2010 through 2013.
Data
Our EHR measures come from several sources: the 2010–2013 IT Supplements to the American Hospital Association (AHA) Annual Survey, the Healthcare Information and Management Systems Society (HIMSS) Analytics Survey, and the SK&A1 Information Services Survey of Physicians; our expenditure measures come from the Centers for Medicare & Medicaid Services’ (CMS) Chronic Conditions Data Warehouse Geographic Variation Database (GVDB).
Hospital EHR Market Penetration Rate
We constructed two measures of hospital EHR adoption and use, both of which are intended to capture whether a hospital has reached the level of MU Stage 1 criteria for financial incentive payments from CMS.
AHA IT Measure
Following Blavin, Buntin, and Friedman (2010), we constructed this measure based on whether a hospital was MU ready—that is, whether it had implemented the eight core health IT applications included in the Stage 1 MU criteria reported in the AHA IT Supplement. The eight applications are (1) patient demographics, (2) patient problem lists, (3) patient medication lists, (4) discharge summaries, (5) CPOE for medications, (6) drug allergy alerts, (7) drug–drug interaction alerts, and (8) any one of four clinical decision support rules. If a hospital met all eight criteria, we considered it MU ready. Then, to use it as one of our measures of hospital EHR market penetration, we calculated the percentage of Medicare discharges in each HRR from hospitals that reported MU readiness.
Only a subset of hospitals responds to the AHA IT supplement survey. Our sample comprised 3,816 unique short‐term acute care hospitals that responded in at least 1 year during 2010 through 2013 to the AHA General Survey. The highest rate of participation in the IT supplement survey among short‐term acute care hospitals during those 4 years was 62.0 percent (2,870) in 2011; the lowest was 57.6 percent (2,644) in 2010. For any of these years, we dropped from our sample those hospitals that did not respond to both the AHA General Survey and the IT supplement, and did not include them in the calculation of the HRR‐level measure. This resulted in 7,407 (41 percent) hospital‐year observations from the AHA General Survey that could not be included.
HIMSS Measure
Our second measure of hospital EHR market penetration was the percentage of Medicare beneficiary discharges in each HRR from hospitals at or above Stage 4 of the HIMSS Electronic Medical Record Adoption Model (EMRAM). HIMSS assigns the EMRAM stages based on each hospital's health IT capabilities, as documented in the annual HIMSS Analytics Survey. The EMRAM stages range from 0 (key ancillary department systems for laboratory, radiology, and pharmacy information have not yet been completely installed) through 7. Stages 1 through 4 reflect the progressive addition of various capabilities, including clinical data repository, nursing documentation, clinical decision support, and CPOE. Higher stages (5 through 7) reflect the addition of other more advanced features. Stage 4 EMRAM is regarded as reflecting capabilities equivalent to Stage 1 MU (Davis 2010; Appari, Johnson, and Anthony 2013; Murphy 2013).
We constructed this alternative hospital EHR market penetration rate from an unbalanced panel of 4,513 short‐term acute care hospitals spanning 2010–2013, for a total of 17,028 hospital‐year observations. We matched hospitals between the HIMSS survey and the AHA General Survey, and used the HRR identifiers and number of Medicare discharges for each hospital to produce another measure of the percentage of Medicare discharges in an HRR from hospitals that reported the equivalent of MU Stage 1. We used several identifiers common to both the HIMSS and AHA surveys, including Medicare provider number, hospital name, and zip code, to match observations between the two surveys. Of the short‐term acute care hospitals appearing in the AHA General Survey, the highest rate of matches with observations in the HIMSS survey was 96 percent (4,429 and 4,363 in 2011 and 2012, respectively); the lowest rate was 88 percent (4,047 in 2010). We dropped from the sample those hospitals that could not be matched from the HIMSS survey to the AHA General Survey in any year and did not include them in the calculation of the HRR‐level measure. This resulted in 1,259 (7 percent) hospital‐year observations from the AHA General Survey that could not be included.
These two measures both purportedly represent MU Stage 1, but we found that their correlation coefficient is only 0.32 at the hospital level.
Physician EHR Market Penetration Rate
We used the SK&A database to calculate the percentage of physician respondents in each HRR who were working in a medical office that reported use of an EHR. There were 2,420,212 physician‐year observations spanning 2010–2013. We averaged the quarterly data for each physician respondent in each year (adding the number of “yes” responses for a given physician and dividing by 4) and then calculated the percentage of physician respondents each year in each HRR who reported using an EHR in ambulatory care settings.
Medicare Expenditures
Because our explanatory variables of interest consist of HRR‐level measures of the EHR prevalence, we included only expenditures for services provided within each beneficiary's HRR of residence. We further limited the sample of beneficiaries to those who incurred at least 50 percent of their expenditures in their home HRR. The GVDB reports standardized Medicare payments that eliminate variation due to factors such as payment adjustments for local wage levels and subsidies for training new doctors (Centers for Medicare and Medicaid Services 2015b), enabling the use of payments as a uniform measure of resource use across different markets (O'Donnell et al. 2013).
Sample of Medicare Beneficiaries
We use a sample of Medicare beneficiaries having at least one of four common chronic conditions. We sought to mitigate the effects of heterogeneity in our sample by restricting it to those beneficiaries age 65 and older enrolled in Medicare Parts A and B for all 12 months of the calendar year or, for those who died during the year, all months during which the beneficiary was alive. After applying these selection criteria, we had a sample of approximately 14.9 million beneficiaries (54 percent of all elderly Medicare FFS beneficiaries) in each year from 2010 through 2013. In addition to calculating HRR‐level averages of annual expenditures per beneficiary for this sample, we also calculated HRR‐level averages of demographic characteristics to use as covariates.
Panel Data Analysis
We constructed a panel dataset of HRR‐level observations. To mitigate bias due to unobserved heterogeneity among HRRs, we estimated regression models of the following form that account for HRR fixed effects:
| (1) |
where is the average standardized expenditures per beneficiary within market m in year t; α a constant term; M mt a set of time‐varying market characteristics, including average beneficiary characteristics and health care market features that may be correlated with both EHR use and expenditures; T t a set of year fixed effects to control for trends common across all HRRs; U mt the percentage of Medicare discharges from hospitals in market m during year t that satisfy MU requirements; P mt the percentage of physicians in market m during year t who work in an office with an EHR; μ m a market fixed effect; and ω mt a random error term. The key parameters θ and ψ allow us to test whether changes in EHR penetration are associated with expenditures.
For each type of expenditure, we estimate two different models to obtain results for each of our two measures of hospital EHR market penetration. We also included controls for beneficiary characteristics, such as race (the percentage of non‐white beneficiaries); age (four categories specifying percentages of beneficiaries’ ages 71–75, 76–80, 80–85, and 86 or older); and percentages residing in rural or micropolitan statistical areas (micropolitan statistical areas are defined by the Office of Management and Budget as areas centered in an urban cluster with a population of 10,000 to 49,999 people; rural areas are defined as containing open areas and settlements with fewer than 1,000 people per square mile). In addition, we included the average Hierarchical Condition Category (HCC) score, a beneficiary‐level risk score calculated by CMS based on such characteristics as age, sex, eligibility for Medicaid, and diagnoses from the previous calendar year. Furthermore, we included controls for relevant market characteristics that fluctuate over time, including hospital market concentration (Herfindahl–Hirschman Index); the percentages of Medicare beneficiaries discharged from nonprofit, for‐profit, and government‐owned hospitals; the percentage of Medicare beneficiaries discharged from critical access hospitals (CAH)2; and members of multihospital systems, hospitals that belong to the Association of American Medical Colleges’ Council of Teaching Hospitals, and those with residency training programs. We calculated standard errors to account for clustering by HRR.
Total Cost Savings and EHR Adoption
We use our regression estimates to calculate total nationwide cost savings related to EHR adoption for the FFS Medicare population in our sample during 2010–2013. We do this by multiplying the regression coefficients for hospital EHR by the observed percentage point change in nationwide hospital EHR penetration for 2010–2013 and by the number of Medicare beneficiaries in our sample. We do the same with the coefficients and percentage point change for physician EHR penetration to get a corresponding nationwide cost savings estimate for physician EHR use.
Geographic Variation across HRRs
To assess the degree to which EHR penetration correlates with nationwide geographic variation in expenditures, we use our regression estimates to predict national coefficients of variation (CV) in each year for each expenditure type. The CV is calculated as the standard deviation of predicted expenditures divided by the mean of predicted expenditures. We also calculated, for comparison, an unadjusted CV for each expenditure type in each year.
Results
We find a notable increase in the percentage of hospitals meeting Stage 1 MU levels and the percentage of physicians using EHRs in ambulatory care settings between 2010 and 2013 (Table 1). In fact, in 2010, 125 (41 percent of) HRRs did not have any Medicare discharges from hospitals that were MU ready and 74 (24 percent of) HRRs did not have any Medicare discharges from hospitals that had achieved EMRAM 4 or higher. By 2013, only 20 HRRs did not have any Medicare discharges from MU‐ready hospitals and 5 HRRs did not have any such discharges from hospitals at EMRAM 4 or above. Although, on average, all EHR indicators increased during the study period, the correlations between them at the HRR level were low, ranging from 0.31 for the SK&A‐based measure and the AHA‐based measure to 0.40 for the AHA‐based and the HIMSS‐based measures. During the same time period, total FFS, Part A acute inpatient, total Part B, lab test, and imaging expenditures per beneficiary all decreased, as shown in Table 1. We converted all dollar figures to constant 2013 dollars using the GDP deflator (Bureau of Economic Analysis—U.S. Department of Commerce 2015).
Table 1.
Average Health IT and Expenditures in 2010 and 2013
| Hospitals MU Ready | Hospitals at EMRAM Stage 4 or above | Physician EHR | Per‐Beneficiary Total of All Medicare Part A and Part B Expenditures | Per‐Beneficiary Expenditures for Inpatient Acute Care Hospital Services | Per‐Beneficiary Expenditures for Total Medicare Part B Expenditures | Per‐Beneficiary Expenditures on Imaging | Per‐Beneficiary Expenditures on Laboratory Testing | |
|---|---|---|---|---|---|---|---|---|
| 2010 | 14% | 20% | 53% | $11,147 | $3,692 | $4,378 | $194 | $116 |
| 2013 | 41% | 55% | 70% | $10,484 | $3,265 | $4,292 | $191 | $94 |
We calculated hospital EHR variables as national averages over hospital‐level data, the physician EHR variable as national averages over physician‐level data, and per beneficiary expenditures as national averages over beneficiary‐level data. All dollar values are in 2013 dollars.
Table 2 reports results for our models estimating the relationship between hospital and physician EHR market penetration rates and average Medicare expenditures per beneficiary across the five categories of expenditures. Using the AHA‐based measure, a 1 percentage point increase in the percentage of discharges occurring in MU‐ready hospitals was associated with a small but statistically significant $0.93 decrease in total annual Medicare expenditures per beneficiary. Using the HIMSS‐based measure, we find a $1.12 decrease. Given the observed changes in hospital EHR adoption and the number of Medicare beneficiaries in our sample, these results translate, respectively, into savings of $372 million and $581 million in total Medicare FFS expenditures. A 1 percentage point increase in physician EHR penetration was associated with approximately a $13 decrease in total Medicare FFS expenditures per beneficiary. Given the observed change in physician IT adoption and the number of Medicare beneficiaries in the sample, the physician EHR results translate into savings of approximately $3.4 billion in total Medicare FFS expenditures.
Table 2.
Medicare Expenditures and Health IT, 2010–2013
| Medicare Part A and Part B | Medicare Part A Acute Care | Medicare Part B | Imaging | Lab Test | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| AHA | HIMSS | AHA | HIMSS | AHA | HIMSS | AHA | HIMSS | AHA | HIMSS | |
| AHA MU Ready Index | −0.93* (0.49) | −0.48** (0.22) | −0.17 (0.22) | −0.027 (0.033) | 0.006 (0.029) | |||||
| HIMSS EMRAM Stage 4 or above | −1.12* (0.64) | −0.46 (0.29) | −0.17 (0.31) | −0.044 (0.043) | −0.068 (0.047) | |||||
| Physician EHR | −13.48*** (4.18) | −13.07*** (4.22) | −6.44*** (1.94) | −6.32*** (2.01) | −3.98** (1.81) | −3.93** (1.77) | −0.46 (0.28) | −0.44 (0.29) | 0.49* (0.25) | 0.55** (0.26) |
Each column represents a different regression model. Columns labeled AHA present models with hospital health IT derived from AHA IT data, and columns labeled HIMSS present models with hospital EHR use derived from HIMSS data. The dependent variable for these models represents Medicare expenditures averaged over our sample beneficiaries in each HRR. Select covariate results are reported in Table 3. Standard errors, adjusted for clustering by HRR, are presented in parentheses.
***p < .01, **p < .05, *p < .10.
If we look only at Part A acute care expenditures, we find that a 1 percentage point increase in the AHA‐based measure, again, is associated with a small but statistically significant decrease in average expenditures per beneficiary (−$0.48). This translates into $192 million in acute care expenditures savings associated with growth in hospital EHR use for our sample. With the HIMSS EMRAM measure, we find a similar sign and magnitude for the relationship (−$0.46), but less precisely estimated and not statistically significant. As in the case with total FFS expenditures, a statistically significant negative relationship exists between physician EHR penetration and Part A acute care expenditures: a 1 percentage point increase is associated with approximately a $6 reduction in Part A acute care expenditures per beneficiary. This result implies a $1.6 billion reduction for these beneficiaries in annual acute care expenditures associated with observed increases in physician EHR adoption.
For total Medicare Part B expenditures, we find that, even though both hospital EHR indices have a negative relationship with expenditures and the magnitude of this relationship is the same for both measures (−$0.17), neither is statistically significant. However, we find that physician EHR penetration has a statistically significant negative relationship with Part B expenditures per beneficiary (−$3.93 to −$3.98, for a 1 percentage point change in penetration), which implies $1 billion in savings for Part B expenditures in our sample due to the observed increase in physician EHR use during our study period.
The results for imaging expenditures show a negative association for hospital and physician EHR but are small in magnitude and not statistically significant. For lab test expenditures, hospital EHR penetration rates, whether using the AHA or HIMSS measures, show a statistically insignificant relationship with these expenditures. In contrast, all regressions show a positive relationship between physician EHR penetration and average lab test expenditures. In particular, a 1 percentage point increase in physician EHR penetration is associated with a $0.49 to $0.55 increase in lab test expenditures per beneficiary.
Aside from the results for the EHR explanatory variables, a number of interesting patterns emerge for the covariates included in the regressions (Table 3). Consistent with expectations that the oldest Medicare beneficiaries incur greater expenditures for care relative to younger beneficiaries, we find that the percentage of beneficiaries age 86 or older in an HRR has a significant positive relationship with total expenditures—between $223 and $232 per percentage point—and with Part A acute care expenditures—$94 and $98 per percentage point (both relative to the base group, the percentage of beneficiaries 65–69 years old). The percentage of beneficiaries residing in rural areas has a significant negative association of −$6 per percentage point with total Part B expenditures and −$1.35 per percentage point with imaging expenditures, a possible indicator of greater barriers to accessing physician care and imaging services in rural areas.
Table 3.
Covariates from Expenditures and Health IT Regressions, 2010–2013
| Medicare Part A and Part B | Medicare Part A Acute Care | Medicare Part B | Imaging | Lab Test | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| AHA | HIMSS | AHA | HIMSS | AHA | HIMSS | AHA | HIMSS | AHA | HIMSS | |
| Percentage ages 81–85 | 22.76 (43.08) | 19.97 (43.64) | 13.71 (22.05) | 12.56 (22.63) | −15.67 (17.83) | −16.09 (17.78) | −8.93*** (2.68) | −9.04*** (2.67) | −4.92** (2.50) | −4.60** (2.33) |
| Percentage age 85 and older | 223.31*** (48.13) | 231.71*** (48.11) | 94.38*** (24.21) | 98.34*** (24.56) | 13.03 (21.48) | 14.46 (21.10) | −2.76 (3.64) | −2.48 (3.64) | 4.98 (3.98) | 5.07 (3.71) |
| Percentage non‐white | −39.08 (33.34) | −38.02 (33.30) | −24.49 (19.64) | −24.13 (19.37) | −21.79 (16.26) | −21.65 (16.40) | −1.40 (2.07) | −1.35 (2.09) | 3.86* (2.04) | 3.19* (1.94) |
| Percentage rural | −2.50 (6.09) | −2.71 (6.08) | 1.92 (3.53) | 1.86 (3.47) | −6.21** (2.99) | −6.24** (3.01) | −1.35** (0.53) | −1.36** (0.54) | −0.92 (0.78) | −0.85 (0.73) |
| Percentage in hospital with residency training | −2.43* (1.27) | −2.33* (1.30) | −1.40** (0.63) | −1.35** (0.65) | −0.44 (0.45) | −0.43 (0.45) | −0.097 (0.77) | −0.093 (0.077) | −0.051 (0.072) | −0.037 (0.068) |
| Percentage in CAH | −3.71 (3.62) | −3.93 (3.59) | −4.00* (2.21) | −4.12* (2.16) | −0.29 (1.90) | −0.33 (1.90) | 0.08 (0.37) | −0.08 (0.37) | −0.60 (0.70) | −0.56 (0.65) |
| Herfindahl Index | 5.66 (7.26) | 6.24 (7.32) | 7.63* (4.16) | 7.91* (4.23) | −2.62 (3.20) | −2.52 (3.19) | 0.38 (0.55) | 0.40 (0.55) | −0.56 (0.58) | −0.53 (0.54) |
Each column represents a different regression model. Columns labeled AHA present models with hospital EHR derived from AHA IT data, and columns labeled HIMSS present models with hospital EHR derived from HIMSS data. Other variables included but not reported here are percentage ages 71–75, percentage ages 76–80, percentage living in Micropolitan areas, average HCC score, percentage Medicare discharges from government hospitals, percentage Medicare discharges from for‐profit hospitals, percentage discharges from members of the Council of Teaching Hospitals, percentage discharges from multihospital system members. Standard errors, adjusted for clustering by HRR, are presented in parentheses.
***p < .01, **p < .05, *p < .10.
Among covariates that describe hospital market characteristics, the percentage of Medicare patients discharged from hospitals with residency training programs has a significant negative association with total FFS expenditures of approximately −$2.43 per percentage point and Part A acute care expenditures of approximately −$1.40 per percentage point, suggesting greater efficiency in these teaching hospitals. The percentage of Medicare patients discharged from critical access hospitals (CAH) has a significant negative association with Part A acute care expenditures of approximately −$4, possibly due to a change in how expenditures for CAHs are calculated for the GVDB during the study period.2 Hospital market concentration has a positive relationship with acute care expenditures of approximately $8 per percentage point increase in the Herfindahl–Hirschman Index, even controlling for variation across markets in health care prices.
Geographic Variation across HRRs
The trends in the unadjusted CV for each expenditure type are shown in Figure 1, and the trends in the regression‐adjusted CVs are shown in Figure 2. All unadjusted CVs, except that of Part B expenditures, which increases slightly, decrease slightly or remain approximately the same between 2010 and 2013. On the other hand, the adjusted CVs for each expenditure type increase moderately over the study period.
Figure 1.
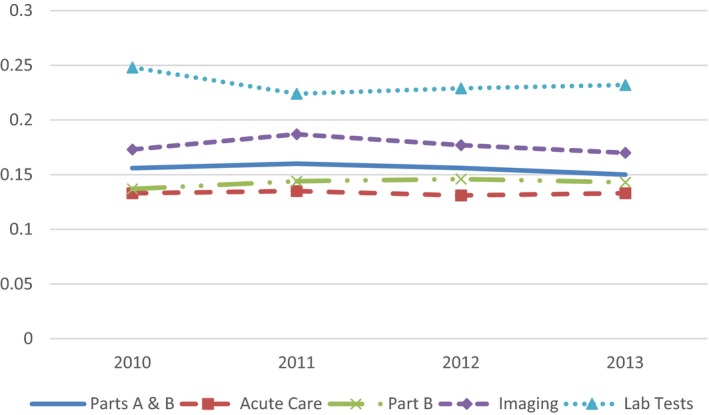
Trends in the Raw Coefficient of Variation in HRR‐Level Total, Acute Inpatient, Part B, Outpatient Imaging, and Outpatient Lab Test Expenditures
Figure 2.
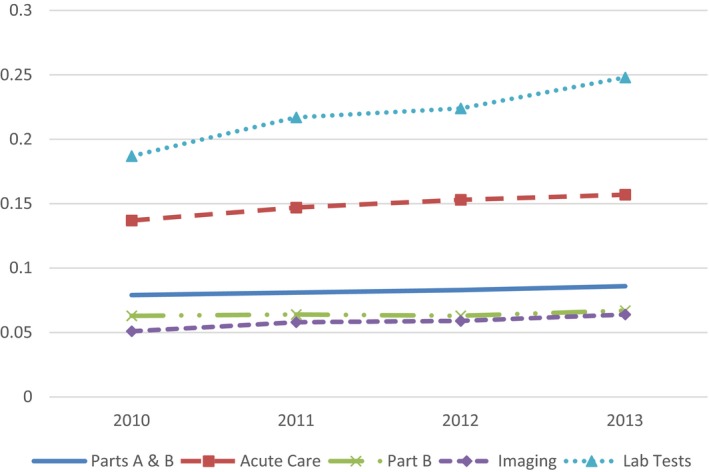
Trends in the Regression‐Adjusted Coefficient of Variation in HRR‐Level Total, Acute Inpatient, Part B, Outpatient Imaging, and Outpatient Lab Test Expenditures
Discussion
Our findings show that increases in hospital adoption of EHR consistent with criteria for MU Stage 1 and increases in physician use of office EHRs have statistically significant negative relationships with per beneficiary total Medicare FFS expenditures and acute care expenditures at the HRR level during the 4‐year period immediately preceding and following enactment of the Medicare and Medicaid EHR Incentive Programs. These results are largely consistent with the intentions for the HITECH Act to help reduce waste and enable more efficient delivery of care to patients. We tested the relationship with two widely used hospital EHR measure sources. Although these two measures show considerable differences from one another in identifying EHR capabilities of individual hospitals, the results obtained from using each measure are remarkably consistent across the five types of expenditures we examined. Results for all but lab tests show a negative relationship between expenditures and hospital EHR, regardless of using AHA or HIMSS measures; the magnitudes are quite similar for total FFS, acute care, Part B, and imaging expenditures.
Although total FFS, acute care, and Part B expenditures per beneficiary all were negatively correlated with higher levels of market penetration in at least one EHR measure, the relatively smaller categories of imaging and lab tests expenditures show either no significant association or a modest increase related to physician EHR penetration. The results for lab tests may reflect the increased ease of ordering tests and receiving results enabled by EHR, as found in some previous studies (McCormick et al. 2012). That imaging does not show a similar increase may be due to the countervailing effect of concern for patient welfare due to radiation exposure from some imaging procedures (Goldzweig et al. 2015).
The small to moderate upward trends in variation in regression‐adjusted expenditures across HRRs over the 4 years suggest that changing characteristics of HRRs, including EHR use, may be contributing to modest increases in geographic variation in resource use during this early phase of the HITECH programs. This trend may reflect variation in the timing of provider achievement of MU goals in the early HITECH period. If most providers are able to achieve similar levels of MU in the future, the trend may level off or reverse. Recent evidence suggests that many hospitals that successfully attested to meeting MU Stage 1 criteria may be facing significant challenges to meet MU Stage 2 (DesRoches, Painter, and Jha 2015), highlighting the importance of monitoring geographic variation in health care use and future EHR MU trends.
Limitations
Although our use of HRR fixed effects mitigates bias in estimating the relationship between EHR penetration and average Medicare expenditures, we cannot infer causation from our results. Unobserved HRR characteristics that vary over time, including changes in health behaviors of the population (Krumholz et al. 2015) and innovations in quality improvement, payment incentives, and care management introduced during this period (Kahn et al. 2015), may confound the relationship between EHR use and health care expenditures. While it is possible that these other changes account for some of the correlations we find, it is also possible that adoption of EHRs enhanced, if not enabled, other innovations to have those effects (Hsiao et al. 2015). Furthermore, it is important to recognize that the observed relationships between EHR adoption and expenditures are at the market level, so we cannot infer that any individual patient is more likely to experience a decrease in expenditures if her physician uses an EHR or if she is admitted to an MU‐ready hospital. And although the AHA and HIMSS data provide a rich set of variables with which to approximate the MU criteria, unfortunately SK&A, the only source of comprehensive nationwide data on physician use of EHRs that covers the full time period we analyze, provides a more limited measure of EHR use. Our use of a nationwide set of market‐level measures, although aiding the generalizability of our study, also prohibits a thorough exploration of the direct mechanisms by which health IT may be related to expenditure reductions.
It is also important to recognize that as we examined the association of EHRs with expenditures among a particular group of FFS Medicare beneficiaries with at least one of four chronic conditions, our findings may not generalize across the full population of Medicare beneficiaries, including those in managed care plans, and may not extend to non‐Medicare patients in commercial plans. Managed care brings to bear other cost‐control mechanisms that may obviate cost‐control features of health IT. Moreover, the opportunity for reductions in expenditures among other patient groups may be limited relative to our study population, which consists of high utilizers of health care.
Implications for Policy and Practice
The national health IT landscape has undergone a significant transformation over the past decade. In 2006, ONC began the Health IT Adoption Initiative to lay the groundwork for tracking the adoption of EHRs by physicians and hospitals at a time when less than 10 percent of hospitals had any form of EHR (DesRoches, Painter, and Jha 2014). Today the landscape is markedly different. Use of EHRs has increased substantially and has become recognized as a cornerstone of efforts to achieve a high‐quality, patient‐centered health care system. Forty‐six percent of eligible professionals, including 54 percent of eligible physicians and 95 percent of eligible hospitals (as of April 2015), have attested to meeting the MU Stage 1 criteria (ONC 2015b). Much of this growth has occurred after the enactment of the HITECH Act, which authorized financial incentives for adopting and using EHRs, resources for technical assistance to providers, funding to advance the electronic exchange of health information, investments to expand the health IT workforce, and funding to establish innovative community‐based models to demonstrate the impact of health IT (Charles, Gabriel, and Searcy 2015).
Given the results of this study, we estimate $85 to $87 in Medicare FFS savings per beneficiary per year associated with a combination of hospital and physician EHR penetration.3 To provide context for these EHR‐related savings, a recent study found that Medicare FFS beneficiaries aligned with the Pioneer Accountable Care Organization Model, another CMS program with a goal of reducing costs while improving quality, experienced savings between $11.18 and $35.62 per beneficiary per month ($134 to $427 per beneficiary per year) relative to other FFS beneficiaries (Nyweide et al. 2015). To provide further context, through 2013, the Medicare incentive program made payments of just over 4 billion dollars to eligible professionals and nearly 7.9 billion dollars to eligible hospitals (Centers for Medicare and Medicaid Services 2015a). While these payments are three times the savings we estimated for Medicare FFS, our calculations only represent financial outcomes for a subset of the total population affected by recent EHR adoption. There may be savings or losses related to EHR MU, to Medicare, and to other payers for other populations aside from those we observe here. In addition, a complete cost–benefit analysis would need to take into account costs of EHR adoption and maintenance borne by providers. Our findings show that the resulting growth in adoption and use of EHRs by the targeted groups of providers has a strong association with decreasing expenditures in the largest categories of Medicare FFS expenditures. Although we caution against a causal interpretation of these findings, they suggest that some intended improvements in efficiency of health care delivery have been realized as a result of the HITECH programs.
Supporting information
Appendix SA1: Author Matrix.
Acknowledgments
Joint Acknowledgment/Disclosure Statement: Funding for this study came through a contract to provide independent evaluation services for the U.S. Department of Health and Human Services, Office of the National Coordinator for Health Information Technology. The views expressed in this article are those of the authors and do not necessarily reflect the views or policies of the U.S. Department of Health and Human Services; nor does mention of trade names, commercial practices, or organizations imply endorsement by the U.S. Government. We thank Meghan Gabriel, Dustin Charles, Talisha Searcy, and Lorenzo Moreno for helpful comments on earlier drafts of this paper. We also thank Swaati Bangalore, John McCauley, and Samuel Canas for valuable data management and programming assistance.
Disclosures: None.
Disclaimers: None.
Notes
SK&A is a market research firm that collects information in each quarter from a census of ambulatory health care sites having at least one provider with prescribing authority in the 50 states and the District of Columbia.
Prior to 2012, GVDB only adjusted CAH expenditures by dividing actual amounts paid by the local wage index. Starting with 2012, GVDB began adjusting CAH expenditures using the same method used for inpatient acute care hospitals paid under the prospective payment system (PPS). For all inpatient PPS hospitals, in addition to adjusting for the local wage index, GVDB also excludes from its calculations various other types of payments through Medicare, including extra payments for medical education. Thus, the standardized payment amounts for inpatient hospital services in the GVDB are often lower than actual payment amounts. By controlling for CAH prevalence in each HRR, in effect we control for this change in how expenditures in the GVDB were calculated for CAHs. The method of calculating standardized payments in the GVDB for non‐CAH acute care hospitals paid under PPS is consistently applied throughout all years of our study.
Using coefficient estimates reported in Table 2 for the regression with Total Medicare Parts A and B as the dependent variable and calculating the average annual percentage point change in hospitals and physicians with EHR reported in Table 1: $0.93 x ((41‐14)/3) = $8.37 for hospitals, and $13.48 x ((70‐53)/3) = $76.39 for physicians. Therefore, $8.37 + $76.39 = $84.76 is the average annual savings per beneficiary summed over hospital and physician EHR results.
References
- Agha, L. 2014. “The Effects of Health Information Technology on the Costs and Quality of Medical Care.” Journal of health economics 34: 19–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Appari, A. , Johnson E. M., and Anthony D. L.. 2013. “Meaningful Use of Electronic Health Record Systems and Process Quality of Care: Evidence from a Panel Data Analysis of U.S. Acute‐Care Hospitals.” Health services research 48 (2 Pt 1): 354–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bailey, J. E. , Pope R. A., Elliott E. C., Wan J. Y., Waters T. M., and Frisse M. E.. 2013a. “Health Information Exchange Reduces Repeated Diagnostic Imaging for Back Pain.” Annals of Emergency Medicine 62 (1): 16–24. [DOI] [PubMed] [Google Scholar]
- Bailey, J. E. , Wan J. Y., Mabry L. M., Landy S. H., Pope R. A., Waters T. M., and Frisse M. E.. 2013b. “Does Health Information Exchange Reduce Unnecessary Neuroimaging and Improve Quality of Headache Care in the Emergency Department?” Journal of general internal medicine 28 (2): 176–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berwick, D. M. , and Hackbarth A. D.. 2012. “Eliminating Waste in US Health Care.” Journal of the American Medical Association 307 (14): 1513–6. [DOI] [PubMed] [Google Scholar]
- Blavin, F. E. , Buntin M. J., and Friedman C. P.. 2010. “Alternative Measures of Electronic Health Record Adoption among Hospitals.” American Journal of Managed Care 16 (12 Suppl HIT): e293–301. [PubMed] [Google Scholar]
- Blumenthal, D. , and Tavenner M.. 2010. “The ‘Meaningful Use’ Regulation for Electronic Health Records.” New England Journal of Medicine 363 (6): 501–4. [DOI] [PubMed] [Google Scholar]
- Bureau of Economic Analysis—U.S. Department of Commerce . 2015. “National Income and Product Accounts Table 1.1.9: Implicit Price Deflators for Gross Domestic Product” [accessed on July 16, 2015]. Available at http://www.bea.-gov/iTable/iTable.cfm?ReqID=9&step=1#reqid=9&step=3&isuri=1&903=13
- Centers for Medicare and Medicaid Services . 2014. “2014 Definition Stage 1 Meaningful Use” [accessed on July 14, 2015]. Available at http://www.cms.gov/Regulations-and-Guidance/Legislation/EHRIncentivePrograms/Meaningful_Use.html
- Centers for Medicare and Medicaid Services . 2015a. “EHR Incentive Program: Medicare Incentive Payments” [accessed on February 1, 2016]. Available at https://www.cms.gov/Regulations-and-Guidance/Legislation/EHRIncentivePrograms/DataAndReports.html
- Centers for Medicare and Medicaid Services . 2015b. “Measure Methodology Reports—Medicare Spending Per Beneficiary (MSPB) Measure” [accessed on July 14, 2015]. Available at http://www.qualitynet.org/dcs/ContentServer?c=Page&pagename=QnetPublic/Page/QnetTier4&cid=1228772057350
- Charles, D. , Gabriel M., and Searcy T.. 2015. Adoption of Electronic Health Record Systems among U.S. Non‐Federal Acute Care Hospitals: 2008–2014. Washington, DC: Office of the National Coordinator for Health Information Technology. [Google Scholar]
- Chernew, M. E. , and Newhouse J. P.. 2012. Chapter One—Health Care Spending Growth Handbook of Health Economics, Vol. 2. Waltham, MA: Elsevier. [Google Scholar]
- Chicklis, C. , MaCurdy T., Bhattacharya J., Shafrin J., Zaidi S., and Rogers D.. 2015. “Regional Growth in Medicare Spending, 1992‐2010.” Health Services Research 50 (5): 1574–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- CMS . 2012. “Stage 1 Changes Tipsheet” [accessed on June 1, 2016]. Available at https://www.cms.gov/Regulations-and-Guidance/Legislation/EHRIncentivePrograms/Downloads/Stage1ChangesTipsheet.pdf
- Dartmouth Atlas of Health Care Working Group . 1998. The Dartmouth Atlas of Health Care in the United States. Hanover, NH: The Center for the Evaluative Clinical Sciences, Dartmouth Medical School. [Google Scholar]
- Davis, M. W. 2010. The State of U.S. Hospitals Relative to Achieving Meaningful Use Measurements. Chicago, IL: HIMSS Analytics. [Google Scholar]
- DesRoches, C. M. , Painter M. W., and Jha A. K.. 2014. Health Information Technology in the United States: Progress and Challenges Ahead, 2014. Princeton, NJ: Robert Wood Johnson Foundation. [Google Scholar]
- DesRoches, C. M. , Painter M. W., and Jha A. K.. 2015. Health Information Technology in the United States, 2015: Transition to a Post‐HITECH World. Cambridge, MA: Mathematica Policy Research. [Google Scholar]
- Dranove, D. , Forman C., Goldfarb A., and Greenstein S.. 2012. The Trillion Dollar Conundrum: Complementarities and Health Information Technology. National Bureau of Economic Research Working Paper Series No. 18281. Cambridge, MA: NBER. [Google Scholar]
- Encinosa, W. E. , and Bae J.. 2015. “Meaningful Use IT Reduces Hospital‐Caused Adverse Drug Events Even at Challenged Hospitals.” Healthcare 3 (1): 12–7. [DOI] [PubMed] [Google Scholar]
- Ford, E. S. , Ajani U. A., Croft J. B., Critchley J. A., Labarthe D. R., Kottke T. E., Giles W. H., and Capewell S.. 2007. “Explaining the Decrease in U.S. Deaths from Coronary Disease, 1980–2000.” New England Journal of Medicine 356 (23): 2388–98. [DOI] [PubMed] [Google Scholar]
- Frisse, M. E. , Johnson K. B., Nian H., Davison C. L., Gadd C. S., Unertl K. M., Turri P. A., and Chen Q.. 2012. “The Financial Impact of Health Information Exchange on Emergency Department Care.” Journal of the American Medical Informatics Association 19 (3): 328–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Furukawa, M. F. , Raghu T. S., and Shao B. B. M.. 2010. “Electronic Medical Records, Nurse Staffing, and Nurse‐Sensitive Patient Outcomes: Evidence from California Hospitals, 1998–2007.” Health services research 45 (4): 941–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Furukawa, M. F. , Patel V., Charles D., Swain M., and Mostashari F.. 2013. “Hospital Electronic Health Information Exchange Grew Substantially in 2008‐12.” Health Affairs (Project Hope) 32 (8): 1346–54. [DOI] [PubMed] [Google Scholar]
- Gawande, A. 2009. “The Cost Conundrum: What a Texas Town Can Teach Us about Health Care.” The New Yorker, June 1, pp. 36–44.19663044 [Google Scholar]
- Goldzweig, C. L. , Orshansky G., Paige N. M., Miake‐Lye I. M., Beroes J. M., Ewing B. A., and Shekelle P. G.. 2015. “Electronic Health Record‐Based Interventions for Improving Appropriate Diagnostic Imaging: A Systematic Review and Meta‐Analysis.” Annals of Internal Medicine 162 (8): 557–65. [DOI] [PubMed] [Google Scholar]
- Hagen, S. , Richmond P., Vavrichek B., Baumgardner J., and Orszag P. R.. 2008. Evidence on the Costs and Benefits of Health Information Technology. Washington, DC: Citeseer. [Google Scholar]
- Hsiao, C. J. , King J., Hing E., and Simon A. E.. 2015. “The Role of Health Information Technology in Care Coordination in the United States.” Medical Care 53 (2): 184–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones, S. S. , Rudin R. S., Perry T., and Shekelle P. G.. 2014. “Health Information Technology: An Updated Systematic Review with a Focus on Meaningful Use.” Annals of Internal Medicine 160 (1): 48–54. [DOI] [PubMed] [Google Scholar]
- Kahn, C. N. , Ault T., Potetz L., Walke T., Chambers J. H., and Burch S.. 2015. “Assessing Medicare's Hospital Pay‐for‐Performance Programs and Whether They Are Achieving Their Goals.” Health Affairs 34 (8): 1281–8. [DOI] [PubMed] [Google Scholar]
- Krumholz, H. M. , Nuti S. V., Downing N. S., Normand S. L., and Wang Y.. 2015. “Mortality, Hospitalizations, and Expenditures for the Medicare Population Aged 65 Years or Older, 1999–2013.” Journal of the American Medical Association 314 (4): 355–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lammers, E. J. , Adler‐Milstein J., and Kocher K. E.. 2014. “Does Health Information Exchange Reduce Redundant Imaging? Evidence from Emergency Departments.” Medical Care 52 (3): 227–34. [DOI] [PubMed] [Google Scholar]
- McCormick, D. , Bor D. H., Woolhandler S., and Himmelstein D. U.. 2012. “Giving Office‐Based Physicians Electronic Access to Patients’ Prior Imaging and Lab Results Did Not Deter Ordering of Tests.” Health Affairs 31 (3): 488–96. [DOI] [PubMed] [Google Scholar]
- McLaughlin, C. G. , and Lammers E.. 2015. “Geographic Variation in Health IT and Health Care Outcomes: A Snapshot before the Meaningful Use Incentive Program Began.” Healthcare 3 (1): 18–23. [DOI] [PubMed] [Google Scholar]
- Murphy, K. 2013. “Stages of Meaningful Use, EMR Adoption: HIMSS Analytics Q&A” [accessed on July 2, 2015]. Available at https://ehrintelligence.com/news/stages-of-meaningful-use-emr-adoption-himss-analytics-qa
- Nyweide, D. J. , Lee W., Cuerdon T. T., Pham H. H., Cox M., Rajkumar R., and Conway P. H.. 2015. “Association of Pioneer Accountable Care Organizations vs Traditional Medicare Fee for Service with Spending, Utilization, and Patient Experience.” Journal of the American Medical Association 313 (21): 2152–61. [DOI] [PubMed] [Google Scholar]
- O'Donnell, B. E. , Schneider K. M., Brooks J. M., Lessman G., Wilwert J., Cook E., Martens G., Wright K., and Chrischilles E. A.. 2013. “Standardizing Medicare Payment Information to Support Examining Geographic Variation in Costs.” Medicare & Medicaid Research Review 3 (3): E1, E2–E17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- ONC . 2015a. Connecting Health and Care for the Nation: A Shared Nationwide Interoperability Roadmap. Washington, DC: Office of the National Coordinator for Health Information Technology. [Google Scholar]
- ONC . 2015b. “Health IT Dashboard” [accessed on July 13, 2015]. Available at http://dashboard.healthit.gov/index.php
- Phelps, C. E. 2000. “Information Diffusion and Best Practice Adoption.” Handbook of Health Economics 1: 223–264. [Google Scholar]
- Powers, C. , Gabriel M. H., Encinosa W., Mostashari F., and Bynum J.. 2015. “Meaningful Use Stage 2 E‐Prescribing Threshold and Adverse Drug Events in the Medicare Part D Population with Diabetes.” Journal of the American Medical Informatics Association 22 (5): 1094–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rahurkar, S. , Vest J. R., and Menachemi N.. 2015. “Despite the Spread of Health Information Exchange, There Is Little Evidence of Its Impact on Cost, Use, and Quality of Care.” Health Affairs 34 (3): 477–83. [DOI] [PubMed] [Google Scholar]
- Rudin, R. S. , Motala A., Goldzweig C. L., and Shekelle P. G.. 2014. “Usage and Effect of Health Information Exchange: A Systematic Review.” Annals of Internal Medicine 161 (11): 803–11. [DOI] [PubMed] [Google Scholar]
- Skinner, J. 2011. “Causes and Consequences of Regional Variations in Health Care.” Handbook of Health Economics 2: 45–93. [Google Scholar]
- Skinner, J. , and Staiger D.. 2007. Technology Adoption from Hybrid Corn to Beta Blockers. Chicago, IL: University of Chicago Press. [Google Scholar]
- Skinner, J. , and Staiger D.. 2009. Technology Diffusion and Productivity Growth in Health Care. Cambridge, MA: National Bureau of Economic Research. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Skinner, J. S. , Staiger D. O., and Fisher E. S.. 2006. “Is Technological Change in Medicine Always Worth It? The Case of Acute Myocardial Infarction.” Health Affairs 25 (2): w34–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix SA1: Author Matrix.


