Highlights
-
•
Rare complication of meckel disease.
-
•
The urinary symptoms are the main revealing table.
-
•
Despite the various investigations done, the diagnosis was carried out, in all the reported cases, in per-operatory.
-
•
The treatment of the vescoentericfistula is surgical in all cases. A diverticulectomy and a suture of the bladder fistula were carried out in all the reported cases.
Keywords: Vesicoentericfistula, Meckel’s diverticulum, Surgery
Abstract
Introduction
Enterovesical fistulas usually result from diverticulitis, Crohn's disease, or colorectal cancer. A perforated Meckel's diverticulum can exceptionally result in an vesico-diverticulum fistula, as noted in only seven previously reported cases.
Case report
A 35-year old Arabic male, quadriplegic,who presented epigastralgia evolving for a week, associated with abdominal distension and cloudy urine. On examination he was feverish (38.5 °C), dehydrated with tenderness in the entire distended abdomen; rectal examination revealed a hypotonic sphincter with no other abnormality. After investigations, acute peritonitis diagnosis was retained. Exploratory laparotomy revealed a vesico-diverticular fistula resulting from a performed Meckel’s diverticulum. Diverticulectomy, ileostomy and bladder sutures were performed after peritoneal cleansing. The postoperative course was uneventful. The anatomo-pathological examination confirmed the diagnosis of a perforated Meckel’s diverticulum that did not contain ectopic gastric or pancreatic tissue.
Conclusion
Vesico-diverticular fistula resulting from a perforated Meckel's diverticulum is a rare complication. To our knowledge, this is only the fourth reported case which is not associated to inflammatory bowel disease.
1. Introduction
The vesicoentericfistula has a relatively rare incidence. It is generally associated to the bowel chronic and inflammatory diseases such as Crohn’s disease. Exceptionally, it might be secondary to Meckel’s diverticulum. The vesicoentericfistula due to Meckel’s diverticulum is a special complication, reported in only seven cases in the literature.
2. Observation
A 35-year-old Arabic male, quadriplegic Admitted to the emergency for Febrile, acute abdominal pain associated to abdominal distension and absence of bowel movments. The examination unveiled a dehydrated, 38.5 °C feverish patient. The abdominal palpation revealed a diffuse abdominal tenderness and a hypotonic anal sphincter without any other Abnormalities. A transurethral catheter yielded purulent urines. The biology, showed a hyperleucocytosis at 23200/mm3 and a CRP at 267 mg/l associated with an acute renal failure (creat: 143 μmol/l and urea 11 mmol/l). The abdominal computed Tomography (CT) scan showed an averagely abundant peritoneal effusion associated with a retro-vesical 12,5cm-collection and a 7,5cm-collection behind the rectus abdominal muscle. There was no pneumo-peritoneum. The Appendix was normal. The CT did not show any clear etiology for This acute peritonits. An urgent surgical intervention was decided. A median laparotomy was carried out, discovering a purulent effusion of the peritoneal cavity. There was an abscess in the Bogros cavity. The Appendix had a normal aspect. 40 cm from the ileo-caecalvalve, There was a perforated and adherent to the bladder dome Meckel’s Diverticulum. The separation of the diverticulum from the bladder, revealed of 4 cm loss of bladder continuity (Fig. 1, Fig. 2). A peritoneal washout with Diverticulectomy and ileostomy was performed. The bladder was sutured on two levels and drained by a Foley catheter. The surgical follow-ups were quite simple. The anatomo-pathological examination confirmed the diagnosis of a perforated Meckel’s diverticulum. The re-establishment of the Bowel continuity through elective way was performed after 04 months.
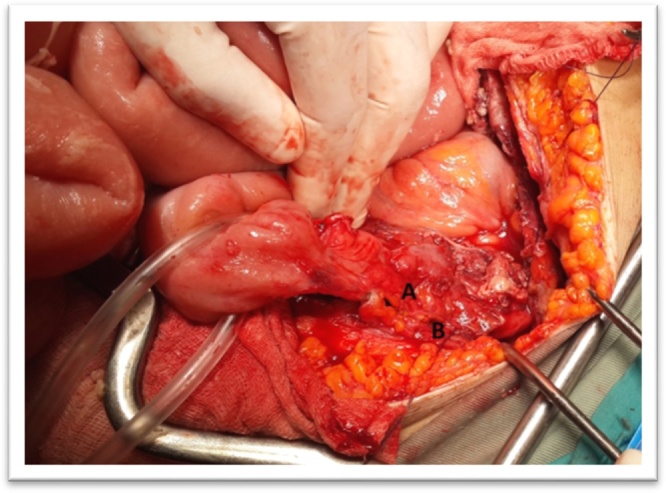
Fig. 1.
Per operative view: Meckel’s diverticulum (A) adherent to the bladder dome (B).
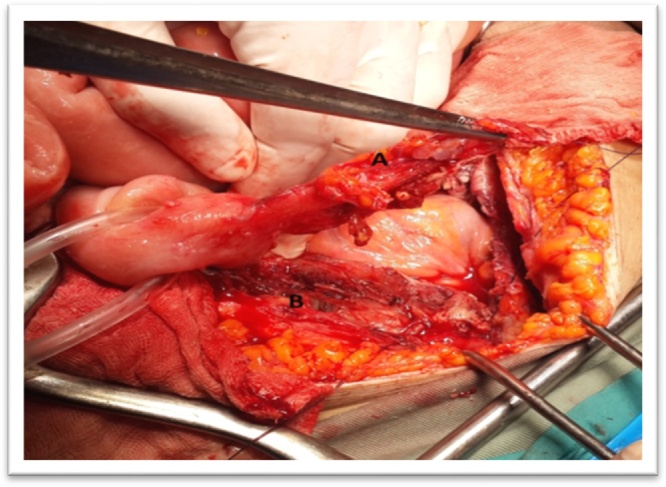
Fig. 2.
Per operative view: Meckel’s diverticulitis (A) bladder fistula (B).
3. Discussion
Meckel’s diverticulum represents the most frequent congenital malformation of the gastro-intestinal tract touching 2–4% of the population [1]. It is caused by an incomplete obliteration of the omphalo-mesenteric canal during the 5th week of gestation [3].
Meckel’s diverticulum is asymptomatic, it complicates in 4–6% of cases [4]. The most frequent complications are the digestive hemorrhage, the intestinal occlusion or the inflammation [2], [5]. The diagnosis is most often carried out during the onset of complications; or still during a laparotomy done during another intervention. Other more rare complications are described such as the entero-colic fistulas, and more recently the fistula between Meckel’s diverticulum and the Appendix or Meckel’s diverticulum and the umbilici [4], [6].
The entero-vesical fistula results from a diverculum, from Crohn’s disease or from a bladder or colorectal cancer [7], [8]. The perforation or the inflammation of Meckel’s diverticulum might also lead to vesicoentericfistulas as it was actually reported in 07 cases in theliterature [9], [10]. In our case, no intestinal or visceral pathologies were associated with the fistula; conversely to the two cases reported where the patients were suffering from Crohn’s disease [13], [14] and another where the entero- visceral fistula was caused by a foreign object ingested and incarcerated at the level of Meckel’s diverticulum [9].
The pre-operatory diagnosis of vesicoenteric fistula is rather hard to make. The urinary symptoms dominate the revealing table such as the urinary infection, the pneumaturia or the fecaluria [8]. The abdominal signs might be summed up in a pain of the right iliac fossa which was noted in only two cases [9], [12]. The imagery does helpfor the diagnosis, particularly the TDM or the abdominal IRM which is much more reliable to highlight the presence of gas in the bladder and the possible solution of continuity between the bladder and an intestinal segment. The cystoscopy could also contribute to the diagnosis by visualizing the fistula in 6.7–67% of the cases [7]. This is reflected by a loss of substance at the level of the posterior superior bladderwall associated with anedematousinfiltration of the mucosa [9], [10].
Despite the support to the diagnosis provided by the various investigations, the diagnosis was carried out, in all the reported cases per-operatory. This is presumably due to the frustrated symptoms as well as the urgent context that minimize the exploration time span. The treatment of the vescoentericfistula is surgical in all cases [11]. A diverticulectomy and a suture of the bladder fistula were carried out in all the reported cases.
4. Conclusion
The vesicoentericfistula due to Meckel’s diverticulum is an extremely rare pathology, usually associated with a past medical history of inflammatory bowel disease which add more rarity to our case. Its main warning signs are urinary. Imaging and particularly the abdomino-pelvic MRI orient the diagnosis However, in all the reported cases the diagnosis has never been made in the pre-operatory settings.
Conflicts of interest
No financial and personal relationships with other people or organisations that could inappropriately influence (bias) their work.
Funding
No source of funding.
Ethical approval
Charles nicolle hospital ethic comitee.
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images.
Authors’ contributions
Bourguiba MA: concept or design, data collection, data analysis or interpretation, writing the paper.
Gharbi M: concept or design, data collection, data analysis or interpretation, writing the paper.
Ghalleb M: data collection, data analysis or interpretation.
Ben Taher A: data collection.
Souai F: data collection.
Bensafta Y: data collection, data analysis or interpretation, writing the paper.
Sayari S: writing the paper.
BEN Moussa M: writing the paper.
Guarantor
Bourguiba Mohamed aboulkacem.
Contributor Information
Bourguiba M.A., Email: belgacembourguiba@yahoo.fr.
Gharbi M., Email: marouagharb@gmail.com.
Ghalleb M., Email: montaghalleb@gmail.com.
Ben Taher A., Email: tahar-atef@hotmail.com.
Souai F., Email: fatensouai@gmail.com.
Bensafta Y., Email: bsyacine@gmail.com.
Sayari S., Email: sayari_sofiene@yahoo.fr.
Ben Moussa M., Email: mounirbm1966@gmail.com.
References
- 1.Sagar J., Kumar V., Shah D.K. Meckel's diverticulum: a systematic review. J. R. Soc. Med. 2006;99(10):501–505. doi: 10.1258/jrsm.99.10.501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Glasgow S.C., Birnabaum E.H., Lowney J.K. Retrorectaltumors: a dignostic and therapeutic challenge. Dis. Colon Rectum. 2005;48:1581–1587. doi: 10.1007/s10350-005-0048-2. [DOI] [PubMed] [Google Scholar]
- 3.DiGiacoma J.C., Cottone F.J. Surgical treatment of Meckel’s diverticulum. South Med. J. 1993;86:671e675. doi: 10.1097/00007611-199306000-00017. [DOI] [PubMed] [Google Scholar]
- 4.Cikman Oztekin, Ali kizaz Hansan. 2014. An extremely rare complication of Meckel’s diverticulum: enterocutaneousfistulization of ombilical hernia. letter to the editor. [Google Scholar]
- 5.Bratus’ V.D., Fomin P.D., Shepet’koIe M., Sydorenko V.M., Kopets’ka A.M., Biliakov-Bel’s’kyĭ O.B., Lissov O.I. Surgical treatment of Meckel diverticulum complicated by an acute hemorrhage. Klin. Khir. 2008;6(June):9–11. [PubMed] [Google Scholar]
- 6.Yang P.F., Chen C.Y., Yu F.J., Yang S.F., Chen Y.T., Kao L.C., Wang J.Y. A rare complication of Meckel’s diverticulum: a fistula between Meckel’s diverticulum and the appendix. Asian J. Surg. 2012;35(October (4)):163–165. doi: 10.1016/j.asjsur.2012.04.018. [DOI] [PubMed] [Google Scholar]
- 7.Mannion R., Cottrell T., Llyod F. Vesicoenteric fistula. Am. J. Surg. 1962;103:116–118. doi: 10.1016/0002-9610(62)90024-7. [DOI] [PubMed] [Google Scholar]
- 8.Karamchandani M., West C. Vesicoenteric fistulas. Am. J. Surg. 1984;147(5):681–683. doi: 10.1016/0002-9610(84)90141-7. [DOI] [PubMed] [Google Scholar]
- 9.Graziotti P., Maffezzini M., Candiano G., Maugeri O. Vesicoenteric fistula created by ingested foreign body in Meckel's diverticulum. J. Urol. 2002;168(6):2547. doi: 10.1016/S0022-5347(05)64197-3. [DOI] [PubMed] [Google Scholar]
- 10.Bouassida M., Mighri M.M., Trigui K., Chtourou M.F., Sassi S., Feidi B., Touinsi H. Meckel’s diverticulum: an exceptional cause of vesicoenteric fistula:case report and literature review. Pan Afr. Med. J. 2014;15(1) doi: 10.11604/pamj.2013.15.9.2440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Varcoe R., Wong S., Taylor C. Diverticulectomy is inadequatetreatment for short Meckel’s diverticulum with heterotopicmucosa. ANZ J. Surg. 2004;74:869e872. doi: 10.1111/j.1445-1433.2004.03191.x. [DOI] [PubMed] [Google Scholar]
- 12.Dearden Christine, Humphreys W.G. 2017. Meckel’s diverticulum: a vesico diverticular fistula. [PMC free article] [PubMed] [Google Scholar]
- 13.Aubert J. Ileobladder fistula due to Meckel's diverticulum: a case, literature review. J. Urol. Nephrol. 1971;77(10):823–832. [PubMed] [Google Scholar]
- 14.Petros J., Argy O. Enterobladder fistula from Meckel's diverticulum in a patient with crohn's ileitis. Dig. Dis. Sci. 1990;35(1):133–136. doi: 10.1007/BF01537234. [DOI] [PubMed] [Google Scholar]