Abstract
Objective
Odontoid fracture is common in cervical injury, representing about 20% of total cervical fractures. Classic odontoid fracture classification focused on anatomy of fracture site has no treatment recommendation and a modified treatment-oriented classification of odontoid fracture was suggested in 2005. We reviewed our odontoid fracture patients to assess the feasibility and efficacy of Grauer’s classification.
Methods
Between October 2000 and September 2015, we collected data from patients who came to our institute for odontoid fracture. Demographic data of patients was reviewed, and neck visual analog scale (VAS) score and fusion rate were assessed by reviewing electronic medical records retrospectively.
Results
Sixty-nine patients out of a total of eighty two odontoid fracture patients were reviewed according to Grauer’s classification. Neck VAS of all subtypes in odontoid fracture classification were decreased at last follow-up (p=0.001). Overall fusion rate was 88.4% at last follow-up. Concordance rate between Grauer’s recommendation and our treatment was 69.9%, especially in type II with the concordance higher than 80%. Complication was minimal representing 7.2%, only in types I and III.
Conclusion
In this study, there were statistically significant improvement in all subtypes in terms of neck VAS at the last follow up, especially in types II and III. Grauer’s classification appears to be meaningful to decide treatment plan for odontoid fractures, especially type II odontoid fracture.
Keywords: Odontoid fracture, Treatment, Classification
INTRODUCTION
In spinal injury population, over 60% is related in cervical injury12). About 20% of cervical spine fractures are odontoid fractures10). In younger patients, these fractures are usually made by high-velocity accidents, whereas falls in elderly patients8). There are variable treatment options from collar immobilization (including collar, halo-vest) to anterior screw fixation or posterior fusion. Anderson and D’Alonzo2) proposed a classification of odontoid fractures and their classification has been still used till today. But classification of Anderson and D’Alonzo has no treatment guideline, and the treatments of odontoid fracture are controversial. In 2005, Grauer et al.8) proposed a modified, treatment-oriented classification of odontoid fractures. This classification divided odontoid fractures into 3 groups, especially type II fractures into three subgroups (subclass A, B, and C). We reviewed odontoid fracture patients treated in our institute to assess the feasibility and efficacy of the Grauer’s classification.
MATERIALS AND METHODS
1. Patients
Between October 2000 and September 2015, we reviewed patients who were diagnosed with odontoid fracture in Korea University Medical Center. We excluded any patients refused recommended treatments or, were transferred to other hospitals. We checked all patients regarding neck visual analogue scale (VAS) score at initial or preoperative and postoperative or final follow-up. Orthotopic, lateral, and open mouth X-rays, Occipitocervical computed tomography (CT) or 3-dimensional reconstruction CT(3D-CT) were evaluated at pretreatment and posttreatment states in all patients. Cervical magnetic resonance imaging (MRI) was evaluated at pretreatment state in all patients, and for patients with spinal cord injury patients, follow-up cervical MRI was also performed at posttreatment state. More than 1-year follow-up was done in all patients and mean follow-up period was 25.52 months (range, 12–60 months). Simple & dynamic cervical spine X-ray, 3D-CT follow-up for instability and fusion assessment were done at 1-year follow-up.
2. External Fixation or Surgical Treatment
In 30 patients, immobilization was performed with cervical Halter traction or skull traction for 2 weeks, and then Halovest for 3 months. Some patients who were not able to do Halovest, external immobilization was done with Philadelphia brace for the same duration.
Anterior cervical stabilization was done via anterior odontoid screw fixation using a odontoid screw in 21 patients. UCSS (Medtronic Inc., Minneapolis, MN, USA) anterior cannulated odontoid lag screw 3.5mm in diameter was implanted in all cases. All patients wore Philadelphia brace for three months.
Posterior stabilization was done with C1 lateral mass —C2 pedicle screws in 18 patients. The 3.5-mm diameter and 22- to 26-mm length atlanto-axial lateral mass/pedicle screws were placed at both intersection 2 mm above the lower edge of posterior arch and medial clination of 5–10 degree. All patients wore Philadelphia brace for 3 months.
3. Statistics Analysis
Statistical analysis was performed with SPSS ver. 13.0 (SPSS Inc., Chicago, IL, USA). A p-value of <0.05 was considered statistically significant. Paired Student t-test was used for comparing pre- and posttreatment VAS score.
RESULTS
We reviewed 82 odontoid fracture patients who came to our institute from October 2000 to September 2015. Thirteen patients were excluded due to refusal of treatment or transfer to other hospitals. Finally, 69 patients were reviewed according to Grauer’s classification and we compared our treatment with recommended treatment by Grauer’s classification and reviewed efficacy of Grauer’s classification.
Fifty male and nineteen female patients were reviewed. Average of patient age was 49.8 years old and standard deviation was 19.6 years. Most of the patients (43 patients, 62.3%) were injured by fall down, 20 (29.0%) by vehicle accident, 6 by others such as fighting and so on. 11 patients were found to have other cervical spine fracture in addition to odontoid fracture. Tow patients had cord injury and weakness, quadriplegia. Initial VAS pain score was 6.17±1.83 (Table 1).
Table 1.
The demographics of patients with odontoid fracture at presentation (n=69)
| Variable | Value |
|---|---|
| Age (yr) | 49.8±19.6 |
| Sex | |
| Male | 50 |
| Female | 19 |
| Trauma mechanism | |
| Fall | 43 |
| Motor vehicle accident | 20 |
| Others | 6 |
| Additional cervical fracture | 11 |
| Associated spinal cord injury | 2 |
| VAS score | 6.17±1.83 |
| Follow-up period (mo) | 25.5±12.1 |
Values are presented as mean±standard deviation or number.
VAS, visual analog scale.
According to Grauer’s classification, 3 patients were in type I fracture, 4 in type IIA, 16 in type IIB, 8 in type IIC, and 38 in type III. In type I, external immobilization is recommended treatment by Grauer’s et al.8). Concurrence of treatment in type I fracture was 1 patient of total 3 patients (33.33%). One patient was treated with anterior odontoid screw fixation, the other was treated with posterior screw fixation. In type IIA, all were corresponded with recommend treatment of Grauer’s classification, external immobilization. In type IIB, 13 of 16 patients (81.25%) underwent anterior screw fixation, 2 treated with external fixation, and 1 was treated with posterior screw fixation, In type IIC, 7 of 8 (87.5%) were treated with posterior screw fixation, the other with external immobilization. In type III, 23 of 38 (60.5%) were treated with external immobilization, but 8 with anterior screw fixation, 7 with posterior screw fixation.
In all subtypes of odontoid fracture, VAS pain score was decreased after treatment (p<0.05 in subtypes IIB, IIC, and III) (Table 2). Fusion rate was higher than 87% in all subgroups except type I (66.6%) which might be because of small number of patients. Complications such as uncontrolled pain, instability were found only in type I, III patients treated with external immobilization, not surgical treatment (Table 3). According to Grauer’s classification, concurrence of actual treatment was highly related in type II fractures.
Table 2.
Analysis of neck VAS according to Grauer’s classification
| Type | Pre VAS | Post VAS | p-value |
|---|---|---|---|
| I (n=3) | 4.67±2.87 | 2.33±0.94 | 0.180 |
| IIA (n=4) | 7.25±0.83 | 4.75±0.43 | 0.062 |
| IIB (n=16) | 6.50±2.03 | 3.19±1.18 | 0.001 |
| IIC (n=8) | 6.25±1.48 | 3.75±1.85 | 0.016 |
| III (n=38) | 6.03±1.68 | 3.05±1.52 | 0.001 |
| Total (n=69) | 6.17±1.83 | 4.70±1.51 | 0.001 |
Values are presented as mean±standard deviation.
VAS, visual analog scale; Pre, pretreatment; Post, posttreatment.
Table 3.
Analysis of treatment results of 69 odontoid fractures according to Grauer’s classification
| Type | Concordance | Fusion rate | Complications |
|---|---|---|---|
| I (n=3) | 1 (33.3) | 2 (66.6) | 1 (33.3) |
| IIA (n=4) | 4 (100) | 4 (100) | 0 (0) |
| IIB (n=16) | 13 (81.3) | 15 (88.2) | 0 (0) |
| IIC (n=8) | 7 (87.5) | 7 (87.5) | 0 (0) |
| III (n=38) | 23 (60.5) | 34 (91.9) | 4 (10.5) |
| Total (n=69) | 48 (69.9) | 61 (88.4) | 5 (7.2) |
DISCUSSION
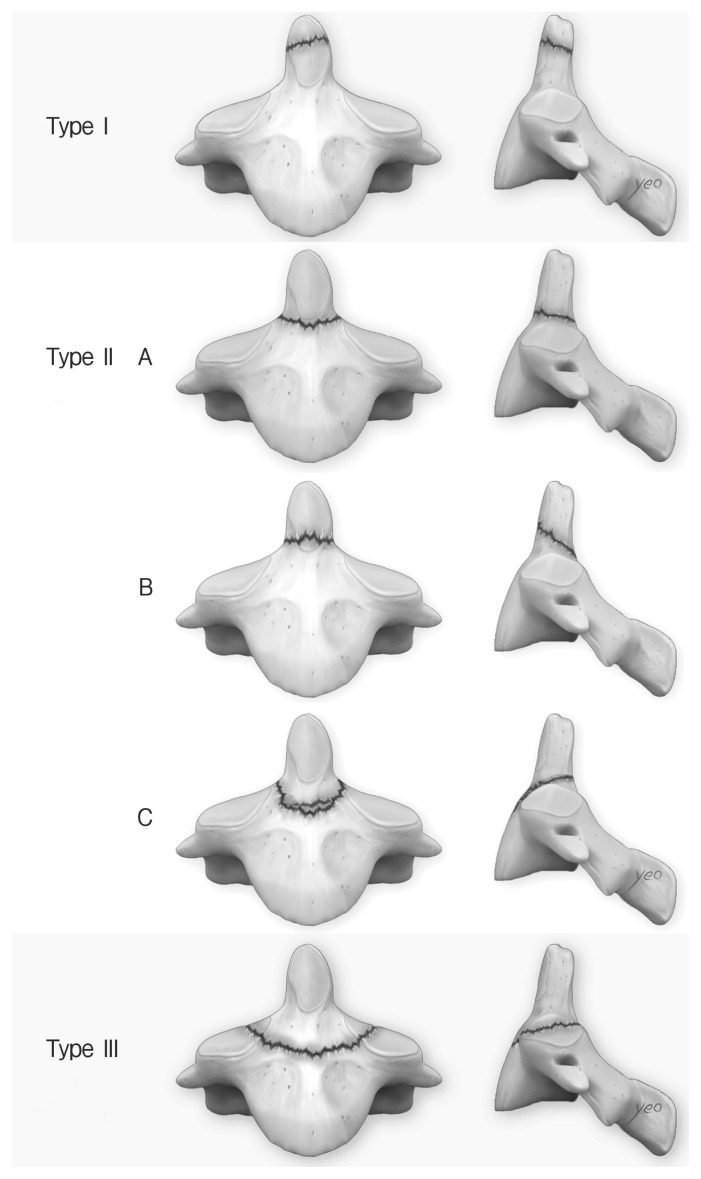
In traumatic cervical spinal injury, odontoid fracture is a common injury. There are several classifications of odontoid fractures. Schatzker’s classification divided odontoid fracture into 2 groups; fracture at below and above attachment of accessory ligaments15). Mourgue’s classification proposed 2 groups as fracture at base (union rate 100%) and neck (union rate less than 50%)6). Althoff’s classification proposed 4 types of odontoid fractures; first type with fracture above the neck have a pseudoarthrosis rate about 64%, second type fracture is through the neck and have pseudoarthrosis rate around 55%, third type in which the fracture includes lateral mass have 50% union rate, fourth type concerns fractures at body of vertebral axis and have high rate of union about 93%1). Commonly applied odontoid fracture classification, Anderson and D’Alonzo classification, and Grauer’s classification have no difference in types I and III. In types I and III odontoid fracture, fracture line was usually in cancellous bone, so healing rate of both fracture groups are relatively high5). Therefore, external immobilization (including traction, halo-vest fixation, brace immobilization, and so on) was used commonly in types I and III odontoid fractures. Type II odontoid fracture is on connection of odontoid and vertebral body, and it makes injury in blood vessel commonly7,16). It makes fracture healing poor, so external immobilization is not proper to treat type II odontoid fracture. So, Grauer et al.8) suggested new classification in 2005, that distributed type II fracture to 3 subtypes, IIA, IIB, and IIC. Type IIA odontoid fracture is transverse fracture without comminution and displacement is less than 1mm. Type IIB is fracture that fracture line is anterosuperior to posteroinferior direction or displacement is over than 1mm. Type IIC is fracture that fracture line is anteroinferior to posterosuperior direction or has significant comminution (Fig. 1). Each types have different treatment recommendation as Table 48).
Fig. 1.
Proposed subclassification of type II odontoid fracture by Grauer et al. 8).
Table 4.
Proposed classification and treatment algorithm of Odontoid fractures by Grauer et al.8)
| Subtype | Description | Treatment guideline |
|---|---|---|
| Type I | Above inferior aspect of C1 anterior arch | External immobilization* |
| Type II | Between types I and II fractures | |
| Type IIA | Nondisplaced fracture | External immobilization |
| Type IIB | Anterior superior to posterior inferior and displaced transverse fractures | Anterior screw fixation |
| Type IIC | Anterior inferior to posterior superior or comminuted fractures | Posterior atlantoaxial fusion |
| Type III | Including at least one of the superior articular facets of C2 | External immobilization |
Halo-vest fixation or Philadelphia brace.
There is controversy about proper treatment in odontoid fractures3). We treated odontoid fracture patients (1 in type I, 4 in type IIA, and 23 in type III) with immobilization as Grauer’s classification recommendation. In our cases, union rate is relatively higher (over than 85%) although several papers have high nonunion rate (13%–72%) with immobilization13,14). Generally, external immobilization is contraindicated because of low bone density, decreased blood supply, etc.7). So, we treated old age patients by anterior or posterior screw fixation although they are in type I, III odontoid fracture. Complication such as uncontrolled neck pain, instability was seen in several cases, but overall complication rate was low. We can consider external immobilization as primary treatment in type I, III patients without any contraindications.
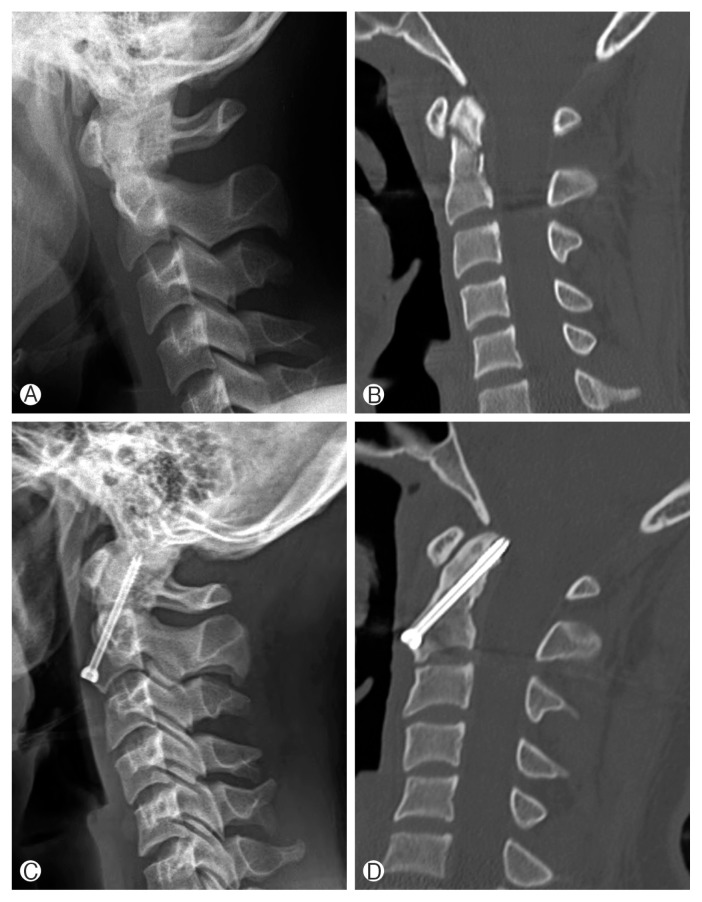
Anterior odontoid screw fixation has clinical effect about high fusion rate and preservation of cervical rotation9). Thirteen patients of type IIB, some patients in other types were treated with anterior odontoid screw fixation (Fig. 2). There was no complication such as pain aggravation, displacement and so on. All 13 patients treated with anterior odontoid screw in type IIB fracture were recovered with bone union. Eight patients in type III fracture were also treated with anterior screw fixation. There was no complication and successful recovery in almost patients. All patients who were treated with anterior odontoid screw fixation had no or minimal limitation of neck rotation. As this result, anterior screw fixation can be a good treatment option in type IIB odontoid fracture if operation is available and avoid excessive neck exercise after operation.
Fig. 2.
An illustrative case of type IIB patient treated by anterior odontoid screw fixation. A 15-year-old male patient had odontoid fracture, type IIB by Grauer’s classification from a vehicle accident trauma. Initial X-ray (A) and CT (B) were evaluated. Anterior screw fixation was done and follow-up X-ray (C) and CT (D) were evaluated at postoperative 12 months, which demonstrated bone union at the fracture site.
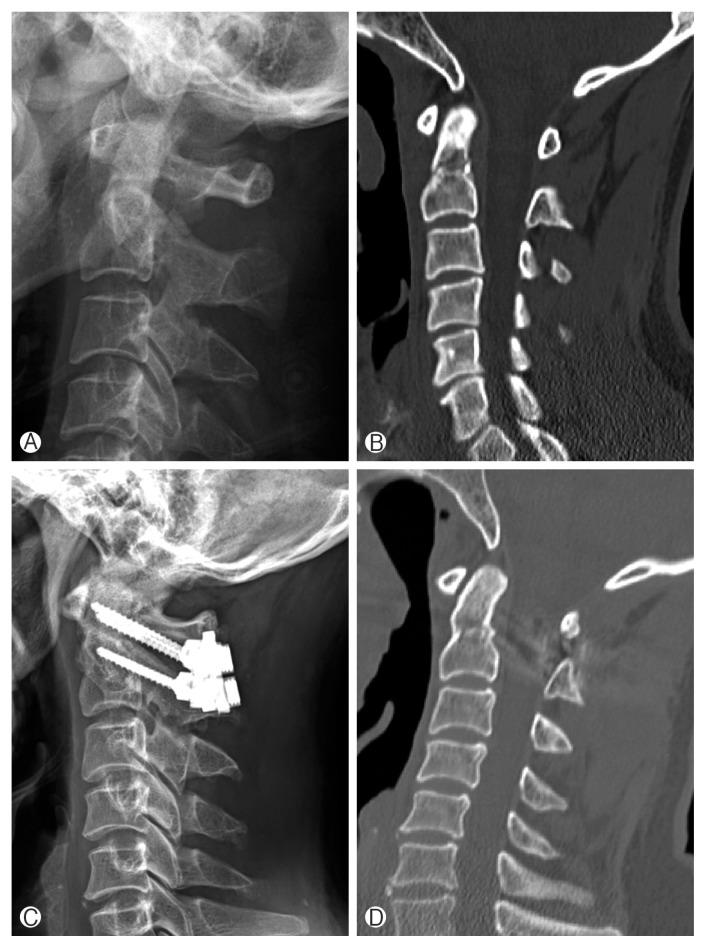
Posterior atlanto-axial pedicle screw fixation and wiring were considered as preferred treatment options in type II odontoid fractures, previously4,11). It was done in 7 patients with type IIC. Some patients who had severe displacement, were not profit to Halo-vest fixation were also treated with posterior screw fixation. Bone union rate was high (87.5% in type IIC) and complication rate was very low (only 1 case in type III, broken screw by secondary trauma). All patients suffered from limitation of neck rotation. Over all fusion rate was higher than 90% in cases of posterior atlanto-axial screw fixation. Posterior atlanto-axial screw fixation can be a good option for type III or severe displacement odontoid fracture patients. In cases of difficult placement of C2 pedicle screw from narrow pedicle or high-riding vertebral artery, C2 translaminar screw fixation can be safely performed (Fig. 3).
Fig. 3.
An illustrative case of type IIC patient treated by posterior atlanto-axial translaminar screw fixation. A 40-year-old male patient was diagnosed of odontoid fracture, type IIC by Grauer’s classification from a fall down trauma. Initial X-ray (A) and CT (B) were evaluated. Posterior screw fixation was done at C1 lateral mass and C2 pedilcle and follow-up X-ray (C) and CT (D) were evaluated at postoperative 12 months.
There were some cases that were discordant with treatment recommendation of Grauer’s classification. When we decided treatment plan, we considered patients condition, instability, bone marrow density. So, we did other treatments in 21 patients, that anterior or posterior fixation in types I and III, posterior fixation or external immobilization in type IIb, external immobilization in type III as Table 5.
Table 5.
Analysis of treatment discordance cases with Grauer’s classification
| Sex/age (yr) | Recommendation (type) | Treatment | Reasons |
|---|---|---|---|
| M/60 | Immobilization (I) | Posterior fixation | Lamina fracture |
| M/66 | Immobilization (I) | Posterior fixation | Lamina fracture |
| M/74 | Anterior fixation (IIb) | Posterior fixation | Pedicle fracture |
| F/91 | Anterior fixation (IIb) | External immobilization | Poor general condition |
| F/51 | Anterior fixation (IIb) | Posterior fixation | Lamina fracture |
| F/54 | Posterior fixation (IIc) | External immobilization | Poor general condition |
| M/13 | External immobilization (III) | Anterior fixation | Dislocation |
| M/41 | External immobilization (III) | Posterior fixation | Lamina fracture |
| M/32 | External immobilization (III) | Posterior fixation | Pedicle fracture |
| F/64 | External immobilization (III) | Anterior fixation | Low BMD* |
| F/47 | External immobilization (III) | Anterior fixation | Low BMD* |
| F/59 | External immobilization (III) | Anterior fixation | Low BMD* |
| F/64 | External immobilization (III) | Anterior fixation | Low BMD* |
| F/74 | External immobilization (III) | Anterior fixation | Low BMD* |
| M/77 | External immobilization (III) | Posterior fixation | Lamina fracture |
| M/42 | External immobilization (III) | Posterior fixation | Pedicle fracture |
| M/52 | External immobilization (III) | Posterior fixation | Pedicle fracture |
| F/51 | External immobilization (III) | Anterior fixation | Low BMD* |
| M/43 | External immobilization (III) | Posterior fixation | Lamina fracture |
| F/62 | External immobilization (III) | Anterior fixation | Low BMD* |
| M/54 | External immobilization (III) | Posterior fixation | Pedicle fracture |
BMD, bone marrow density.
Low BMD means lower than -2.5.
There are some limitations in this study such as small sample size, short-term period, retrospective study, only single center study. It needs to study in larger sample size with multicenter study, long-term follow-up, prospective study.
CONCLUSION
Odontoid fractures could be treated with various procedures including external immobilization, anterior screw fixation, posterior atlanto-axial fusion. Although other factor such as instability, bone density and patients conditions are important, type of odontoid fracture seems to be the most important factor that decides treatment plan in odontoid fracture patients. As followed Grauer’s classification, types I, IIA, III of odontoid fracture is treated with external immobilization using Halo-vest fixation or Philadelphia brace. Anterior screw fixation in type IIB, posterior atlanto-axial fusion in type IIC are usually recommended for treatment.
We refer the proposed treatment-oriented classification by Grauer et al.8) is recommendable when making a treatment plan in odontoid fracture patients.
ACKNOWLEDGMENTS
The authors would like to thank medical illustrator, Sangwon Yeo, for his help with the illustrations.
Footnotes
CONFLICT OF INTEREST
No potential conflict of interest relevant to this article was reported.
REFERENCES
- 1.Althoff B. Fracture of the odontoid process. An experimental and clinical study. Acta Orthop Scand Suppl. 1979;177:1–95. doi: 10.3109/ort.1979.50.suppl-177.01. [DOI] [PubMed] [Google Scholar]
- 2.Anderson LD, D’Alonzo RT. Fractures of the odontoid process of the axis. J Bone Joint Surg Am. 1974;56:1663–1674. [PubMed] [Google Scholar]
- 3.Bransford RJ, Alton TB, Patel AR, Bellabarba C. Upper cervical spine trauma. J Am Acad Orthop Surg. 2014;22:718–729. doi: 10.5435/JAAOS-22-11-718. [DOI] [PubMed] [Google Scholar]
- 4.Brooks AL, Jenkins EB. Atlanto-axial arthrodesis by the wedge compression method. J Bone Joint Surg Am. 1978;60:279–284. [PubMed] [Google Scholar]
- 5.Chen Q, Liu WM, Wang HR, Jiang LB, Xing R, Dong J. Efficacy and safety of different treatments for Grauer type II odontoid fractures: a preliminary study. Int J Clin Exp Med. 2016;9:8145–8152. [Google Scholar]
- 6.de Mourgues GM, Fisher L, Schnepp J, Comtet J, Vidalain JP. Fractures de I’omoplate. A propos d’une serie de 130 cas traitts orthoptdiquemen. Soc Chir Lyon. 1972;8:47–50. [Google Scholar]
- 7.Govender S, Maharaj JF, Haffajee MR. Fractures of the odontoid process. J Bone Joint Surg Br. 2000;82:1143–1147. doi: 10.1302/0301-620x.82b8.10601. [DOI] [PubMed] [Google Scholar]
- 8.Grauer JN, Shafi B, Hilibrand AS, Harrop JS, Kwon BK, Beiner JM, et al. Proposal of a modified, treatment-oriented classification of odontoid fractures. Spine J. 2005;5:123–129. doi: 10.1016/j.spinee.2004.09.014. [DOI] [PubMed] [Google Scholar]
- 9.Lee DS. Anterior screw fixation of anteriorly displaced type III odontoid fracture corrected by transoral digital manipulation. Korean J Spine. 2013;10:101–103. doi: 10.14245/kjs.2013.10.2.101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Maak TG, Grauer JN. The contemporary treatment of odontoid injuries. Spine (Phila Pa 1976) 2006;31(11 Suppl):S53–60. doi: 10.1097/01.brs.0000217941.55817.52. [DOI] [PubMed] [Google Scholar]
- 11.Magerl F, Seemann PS. Stable posterior fusion of the atlas and axis by transarticular screw fixation. In: Kehr P, Weidner A, editors. Cervical spine I, Strasbourg 1985. Wien: Springer-Verlag; 1987. pp. 322–327. [Google Scholar]
- 12.Ochoa G. Surgical management of odontoid fractures. Injury. 2005;36(Suppl 2):B54–64. doi: 10.1016/j.injury.2005.06.015. [DOI] [PubMed] [Google Scholar]
- 13.Patel A, Zakaria R, Al-Mahfoudh R, Clark S, Barrett C, Sarsam Z, et al. Conservative management of type II and III odontoid fractures in the elderly at a regional spine centre: a prospective and retrospective cohort study. Br J Neurosurg. 2015;29:249–253. doi: 10.3109/02688697.2014.958055. [DOI] [PubMed] [Google Scholar]
- 14.Pepin JW, Bourne RB, Hawkins RJ. Odontoid fractures, with special reference to the elderly patient. Clin Orthop Relat Res. 1985;(193):178–183. [PubMed] [Google Scholar]
- 15.Schatzker J, Rorabeck CH, Waddell JP. Fractures of the dens (odontoid process). An analysis of thirty-seven cases. J Bone Joint Surg Br. 1971;53:392–405. [PubMed] [Google Scholar]
- 16.Schiff DC, Parke WW. The arterial supply of the odontoid process. J Bone Joint Surg Am. 1973;55:1450–1456. [PubMed] [Google Scholar]