Abstract
Objective
To determine rates of retention, antiretroviral therapy (ART) use, and viral suppression in an adult cohort from a public tertiary referral hospital in the city of Buenos Aires, Argentina.
Methods
HIV-positive ART-naïve patients ≥ 18 years old starting care 2011–2013 contributed data until the end of 2014. Three outcomes were assessed in 2014: retention in care, ART use, and viral suppression. Patient characteristics associated with each outcome were assessed through logistic regression.
Results
A total of 1 031 patients were included. By the end of 2014, 1.5% had died and 14.8% were transferred to a different center. Of the remaining 859 patients, 563 (65.5%) were retained in 2014. Among those retained, 459 (81.5%) were on ART in 2014. Of those 459 on ART, 270 (58.8%) were virologically suppressed. Younger age was associated with lower retention (OR (odds ratio): 0.67; 95% CI (confidence interval): 0.44–0.92 for ≥ 35 vs. < 35 years), but unrelated with ART use or viral suppression. Low CD4 count at first visit was associated with ART use (OR: 35.72 for CD4 < 200, 7.13 for CD4 200–499 vs. ≥ 500, P < 0.001) and with virologic suppression (OR: 2.17 for CD4 < 200, 2.46 for CD4 200–499 vs. ≥ 500, P: 0.023).
Conclusions
Our hospital in Buenos Aires is still below the recommended 90-90-90 targets of the Joint United Nations Programme on HIV/AIDS (UNAIDS) for ART use and viral suppression. We found a major gap in retention in care. Identifying younger age as being associated with worse retention will help in the design of targeted interventions.
Keywords: HIV, antiretroviral therapy, highly active, treatment outcome, continuity of patient care, Argentina
Three decades after the first AIDS case was diagnosed in Argentina, the latest estimates from the Ministry of Health and the Joint United Nations Programme on HIV/AIDS (UNAIDS) indicate that 126 000 people are living with HIV in the country, with 6 500 new diagnoses and 1 400 AIDS-related deaths occurring annually (1).
In Argentina, with the exception of antenatal care and blood banks, HIV testing is client-initiated, with the requirement of signed informed consent (i.e., an opt-in approach). Rapid tests have been incorporated recently, but are not yet widely available. The country has provided antiretroviral therapy (ART) for free to all individuals in need since 1998 and has recommended universal HIV treatment since 2015. Individualized prescription is common, which results in a number of different first-line regimens. Both brand-name and generic drugs are available and, in 2015, nearly 80% of initial ART regimens were nonnucleoside reverse transcriptase inhibitor–based.
The Argentine health care system can be divided into three subsystems: the public sector, social health insurance (SHI) funds, and the private health sector. The SHI subsystem is further split into provincial health insurance and social health insurance at the national level. SHI at the national level includes the pensioners’ fund, which is an independent scheme that covers the elderly population and their dependents. This particular design imbues the health care sector with a peculiar logic, since it involves the disjointed coexistence of each of these subsystems, which differ with respect to their target population, the services provided, and the origin of the resources available (2). As in many other middle-income countries, protections for health care access and safeguards against unaffordable health expenses continue to be segmented and fragmented (3).
The provision of ART follows a decentralized model: 70% of patients receive ART through the public health system, while the rest receive it through SHI or private insurance. Under national law, that ART provision is at no cost to patients, in all three systems (1). Nearly 30 000 patients from the city of Buenos Aires and the province of Buenos Aires are provided ART through the public health system (1).
In 2015, Argentina subscribed to the UNAIDS 90-90-90 HIV/AIDS regional targets for the year 2020. Under that initiative, 90% of people with HIV should be diagnosed, 90% of those diagnosed should be treated with ART, and 90% of those on ART should achieve an undetectable viral load (4).
The HIV care cascade is a useful tool to further describe the epidemiology of HIV and to assess outcomes of HIV care delivery, including linkage to care, retention in care, ART receipt, and virologic suppression (5, 6). A recent study from the Caribbean, Central and South America network for HIV epidemiology (CCASAnet) cohort showed improvements in the HIV care-continuum indicators of clinical retention, use of ART, and viral suppression from 2003 to 2012 (7). Another study, from the CCASAnet and North American AIDS Cohort Collaboration on Research and Design (NA-ACCORD) cohorts, mapped HIV indicators to provide a comparison between countries and regions (8).
The data currently available do not allow an estimation of the care cascade at the national level in Argentina, although a cohort study conducted by the National HIV and STD Program (Dirección de Sida y ETS, Ministerio de Salud) and supported by UNAIDS showed that within one year of HIV diagnosis, 70% of patients started ART (1). Since information on the HIV care cascade remains limited, we aimed to determine rates of retention, ART use, and virologic suppression in an adult cohort from a public tertiary referral hospital in the city of Buenos Aires.
METHODS
Clinical setting and data sources
The Hospital General de Agudos Juan A. Fernández is a public tertiary referral hospital located in the city of Buenos Aires, Argentina. The hospital’s Infectious Diseases outpatient unit provides care to approximately 4 000 HIV-positive patients, one-third from the city of Buenos Aires itself and two-thirds from the Greater Buenos Aires area (cities surrounding the city of Buenos Aires, part of the province of Buenos Aires). Electronic medical records (EMRs) were implemented in 2011, and since then, clinical data have been collected in the EMR at the time of medical consultation. The EMR captures HIV-related physician visits, antiretroviral prescriptions, and laboratory data. The research database was supplemented with the hospital pharmacy database, which captures antiretroviral drug dispensations. Investigators checked data for internal consistency and missing data, and performed periodic quality assessment and internal audits. When necessary, data were abstracted again and reentered.
Patients signed a form providing informed consent for inclusion in epidemiologic studies at the time of first clinical visit, when they were enrolled in the EMR.
The National HIV and STD Program provided additional information from their databases.
Study design
This study included data from HIV-positive ART-naïve adults (aged ≥ 18 years) linked to care between 1 January 2011 and 31 December 2013. Individuals contributed data from the first physician visit until death, transfer to another center, last contact, or censoring at the end of 2014. Three HIV care cascade outcomes were assessed in 2014: retention in care, ART use, and virologic suppression. Patients lost during follow-up were tracked in the National HIV and STD Program registries to identify additional deaths and transfers.
Definitions
Individuals were considered in the initial denominator, i.e. linked to care, if they had at least one physician visit after HIV diagnosis within the study period.
Retention in care was defined as having at least one visit (e.g., clinic visit, laboratory measurement (CD4 count or HIV-1 viral load), or pharmacy pickup) during 2014.
ART use was defined as prescription of ART for at least 90 days or at least three notations of ART pickup from the pharmacy in 2014.
Virologic suppression was defined as HIV-1 viral load (VL) < 200 copies/ml at last measurement in 2014.
Baseline CD4 was the CD4 count closest to first visit, within 180 days before or after that visit, and no more than 7 days after ART initiation.
Baseline VL was the VL closest to first visit, within 180 days before or after that visit, and before the start of ART.
Statistical analysis
We assessed differences between patients for each outcome, with the chi-square test of proportions used for categorical variables and the Wilcoxon rank-sum test of medians used for continuous variables.
We used a conditional approach, in which only individuals meeting one outcome were analyzed in the next step of the HIV care cascade (5, 9). For virologic suppression, we also presented data using two denominators: individuals on ART and individuals who had at least one VL performed.
Logistic regression was performed to assess adjusted associations between demographic and clinical factors and meeting each indicator. Factors assessed included age at first visit (dichotomized at 35 years, near the cohort median), gender, baseline CD4 count (categorized as < 200, 200–499, and ≥ 500 cells/μL) and VL (in log10 copies/ml), likely HIV transmission mode (men who have sex with men (MSM), heterosexual contact, and unknown or other risk), and place of residence (city of Buenos Aires or other). Variables with fewer than 25% of the values missing were entered in the multivariable model; no model selection was attempted. P values < 0.05 were considered statistically significant. All analyses were performed with the SPSS Statistics 20 software package.
RESULTS
Between 1 January 2011 and 31 December 2013, 1 676 HIV-positive adult patients started care at the Infectious Diseases outpatient unit of the Hospital General de Agudos Juan A. Fernández. Of them, 645 (38.5%) were transferred or self-transferred from other centers and had already started ART (Figure 1).
FIGURE 1. Flow chart showing patient disposition from first visit to virologic suppression in a cohort of HIV-positive patients in Buenos Aires, Argentina, 2011–2014.
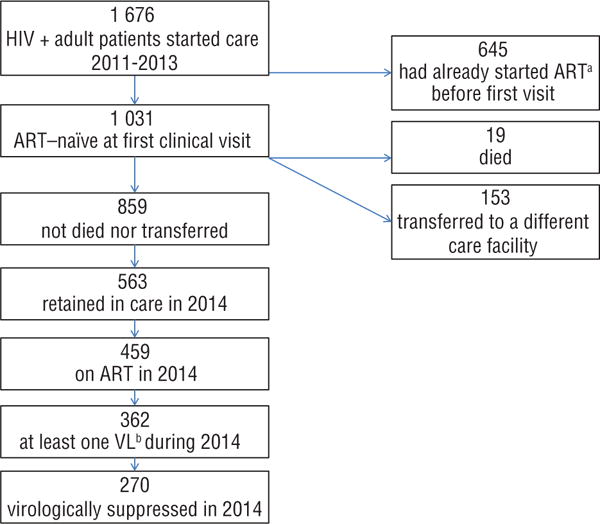
Source: Produced by the authors from study results.
aART = antiretroviral therapy.
bVL= viral load.
This study focused on the 1 031 patients who were ART-naïve at first clinical visit: 798 (77.4%) were male; median age was 33.7 years (interquartile range (IQR): 26.9–41.6); and 52.6% lived in the city of Buenos Aires. The probable HIV transmission route was recorded for 682 patients: 314 (46.0%) reported male sex with men, 282 (41.3%) heterosexual transmission, 21 (3.1%) injection drug use, 6 (0.9%) other risks, and 59 (8.7%) unknown transmission. Baseline median CD4 count was 345 cells/μL (IQR: 138–560) and VL was 4.36 log10 copies/ml (IQR: 3.75–5.00).
By the end of 2014, 19 patients (1.5%) had died, with 14 of them registered in the Hospital General de Agudos Juan A. Fernández EMRs and 5 of them identified by reviewing the National HIV and STD Program registries. All deaths occurred in patients with clinical AIDS. Causes of death were unknown for 5; were AIDS-associated illnesses in 7 (non-Hodgkin lymphoma, 3; tuberculosis, 2; meningeal cryptococcosis, 1; Mycobacterium avium infection, 1); and were non-AIDS-associated illnesses for 7 (sepsis, 3; Hodgkin lymphoma, 2; other, 2).
By 2014, 153 patients (14.8%) either were transferred (22 persons) or self-transferred (131 persons) to a different care facility.
Of the remaining 859 patients, 563 (65.5%) were retained in care in 2014 (Figure 2). Among those retained, 459 (81.5%) were on ART in 2014. Of those on ART, 362 (78.8%) had at least one VL during 2014, and 270 of them (74.6%) achieved virologic suppression. Therefore, 58.8% of the total on ART were virologically suppressed.
FIGURE 2. HIV treatment cascade for adults in a tertiary referral hospital center in Buenos Aires, Argentina, 2011–2014.
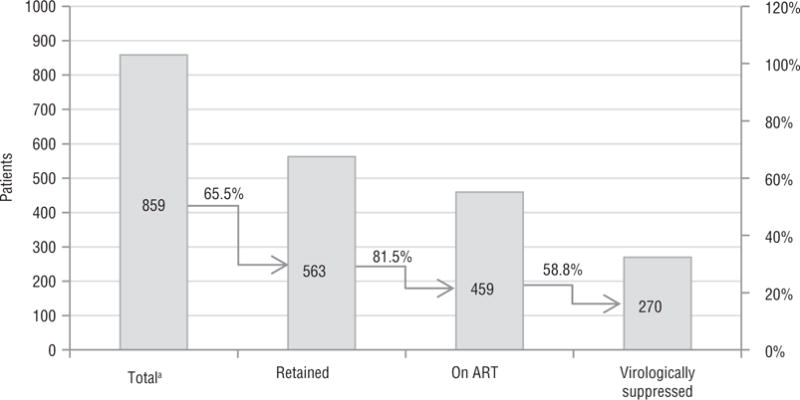
Source: Produced by the authors from study results.
aTotal linked to care and not dead nor transferred to a different center.
Table 1 shows characteristics of patients meeting or not meeting each indicator. Patients retained in care were older than those not retained (median 34 vs. 31.5 years, P < 0.001), but no differences were observed in gender, transmission risk, baseline VL, or place of residence. There was a nonsignificant difference in median CD4 count at first visit by retention status, with higher CD4 counts among those not retained. Data for VL and CD4 counts or pharmacy pickups in the absence of physician visits accounted for 7% of data that defined retention.
TABLE 1.
Characteristics of HIV-positive patients meeting or not meeting indicators for retention in care, antiretroviral therapy (ART) use, and virologic suppression in a cohort from Buenos Aires, Argentina, 2011–2014a
| Characteristic | Total (n = 859) |
Total for retentionb (n = 859)
|
Total for ART usec (n = 563)
|
Total for virologic suppressiond (n = 362)
|
||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Not retained 296 (34.5%) |
Retained 563 (65.5%) |
P | ART not used 104 (18.5%) |
ART used 459 (81.5%) |
P | Not suppressed 92 (25.4%) |
Suppressed 270 (74.6%) |
P | ||
| Age (years) | 33 (27–41) | 31.5 (26–39) | 34 (28–42) | < 0.001 | 32 (27–40) | 34 (28–42) | 0.265 | 33 (27–40) | 34.5 (28–43) | 0.171 |
| Gender | 0.171 | 0.325 | 0.543 | |||||||
| Male | 664 (77.3%) | 237 (35.7%) | 427 (64.3%) | 75 (17.6%) | 352 (82.4%) | 68 (24.6%) | 208 (75.4%) | |||
| Female | 195 (22.7%) | 59 (30.3%) | 136 (69.7%) | 29 (21.3%) | 107 (78.7%) | 24 (27.9%) | 62 (72.1%) | |||
| Transmission risk | 0.962 | 0.298 | 0.146 | |||||||
| MSMe | 276 (32.1%) | 89 (32.2%) | 187 (67.8%) | 39 (20.9%) | 148 (79.1%) | 26 (22.4%) | 90 (77.6%) | |||
| Heterosexual | 249 (29.0%) | 78 (31.3%) | 171 (68.7%) | 26 (15.2%) | 145 (84.8%) | 32 (27.4%) | 85 (72.6%) | |||
| Other/Unknown | 64 (7.5%) | 21 (32.8%) | 43 (67.2%) | 6 (14.0%) | 37 (86.0%) | 11 (40.7%) | 16 (59.3%) | |||
| Missing | 270 (31.4%) | |||||||||
| Residence | 0.498 | 0.013 | 0.626 | |||||||
| Buenos Aires city | 439 (51.1%) | 144 (32.8%) | 295 (67.2%) | 67 (22.7%) | 228 (77.3%) | 47 (26.4%) | 131 (73.6%) | |||
| Other | 394 (45.9%) | 138 (35.0%) | 256 (65.0%) | 37 (14.5%) | 219 (85.5%) | 42 (24%) | 133 (76%) | |||
| Missing | 26 (3%) | |||||||||
| CD4 count (cells/μL) | 358 (134–559) | 377 (187–619) | 343 (121–533) | 0.053 | 648 (510–819) | 360 (171–501) | < 0.001 | 393 (138–593) | 342 (173–488) | 0.153 |
| Missing | 197 (22.9%) | |||||||||
| HIV-1 viral load (log10), copies/μL | 1.38 (3.77–5.00) | 4.43 (3.84–5.12) | 4.36 (3.73–4.94) | 0.325 | 3.6 (3.1–4.2) | 4.5 (3.9–5.1) | < 0.001 | 4.4 (3.9–4.9) | 4.5 (3.9–5.1) | 0.574 |
| Missing | 437 (50.1%) | |||||||||
Data are n (%) or median (interquartile range). Chi-square test of proportions used for categorical variables, and the Wilcoxon rank-sum test of medians used for continuous variables.
Retention indicator: individuals with at least one visit (clinic or laboratory (CD4 or viral load (VL)) or pharmacy pickup) during 2014.
ART use indicator: prescription of ART for at least 90 days or at least three notations of ART pickup from the pharmacy in 2014 among those retained.
Virologic suppression indicator: Viral load (VL)< 200 copies/ml at last measurement in 2014 among those with at least one VL performed in 2014.
MSM = men who have sex with men.
Among patients retained, those on ART were less likely to be residents of the city of Buenos Aires (77.3% vs. 85.5%, P = 0.013), had lower median CD4 counts (360 vs. 648 cells/μL, P < 0.001), and higher median VL (4.5 vs. 3.6 log10 copies/ml, P < 0.001) at first visit.
Among patients on ART with at least one VL performed in 2014, there were no significant differences between those who achieved virologic suppression and those who did not.
In multivariable analysis, younger age was significantly associated with lower retention (odds ratio (OR): 0.67; 95% confidence interval (CI): 0.44–0.92; P = 0.016 for ≥ 35 vs. < 35 years), but not with ART use or virologic suppression (Table 2). Patient residence outside the city of Buenos Aires was associated with lower retention (OR: 0.62; 95% CI: 0.43–0.89; P: 0.014); however, for those retained, there was a trend towards increased ART use for those who lived outside the city. ART use was strongly associated with low baseline CD4 count (OR: 35.72 for CD4 < 200 and 7.13 for CD4 200–499 vs. ≥ 500 cells/μL; P < 0.001).
TABLE 2.
Multivariable analysis of factors associated with retention, antiretroviral therapy (ART) use, and virologic suppression in a cohort of HIV-positive patients from Buenos Aires, Argentina, 2011–2014a
| Characteristic | Retentionb
|
ART usec
|
Virologic suppressiond
|
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Unadjusted ORe (95% CIf) |
P |
Adjusted OR (95% CI) |
P | Unadjusted OR (95% CI) |
P | Adjusted OR (95% CI) |
P | Unadjusted OR (95% CI) |
P | Adjusted OR (95% CI) |
P | |
| Age (years) | 0.006 | 0.016 | 0.570 | 0.303 | 0.368 | 0.822 | ||||||
| < 35 | 0.67 (0.50–0.89) |
0.64 (0.44–0.92) |
0.88 (0.58–1.35) |
1.359 (0.76–2.44) |
0.80 (0.50–1.29) |
0.94 (0.54–1.64) |
||||||
| ≥ 35 | Reference | Reference | Reference | Reference | Reference | Reference | ||||||
| Gender | 0.161 | 0.640 | 0.326 | 0.030 | 0.543 | 0.670 | ||||||
| Male | Reference | Reference | Reference | Reference | Reference | Reference | ||||||
| Female | 1.28 (0.91–1.81) |
1.11 (0.72–1.69) |
0.79 (0.49–1.27) |
0.49 (0.26–0.93) |
0.85 (0.49–1.46) |
0.87 (0.46–1.66) |
||||||
| Residence | 0.498 | 0.009 | 0.014 | 0.092 | 0.603 | 0.802 | ||||||
| City of Buenos Aires | Reference | Reference | Reference | Reference | Reference | Reference | ||||||
| Other | 0.91 (0.68–1.21) |
0.62 (0.43–0.89) |
1.74 (1.12–2.71) |
1.66 (0.92–2.98) |
1.14 (0.70–1.84) |
1.07 (0.62–1.85) |
||||||
| CD4 count (cells/μL) | 0.035 | 0.068 | <0.001 | <0.001 | 0.035 | 0.023 | ||||||
| < 200 | 1.73 (1.12–2.66) |
1.65 (1.05–2.60) |
35.72 (10.84–117.67) |
39.04 (11.60–131–38) |
2.07 (1.06–4.04) |
2.17 (1.07–4.38) |
||||||
| 200–499 | 1.44 (0.97–2.15) |
1.45 (0.96–2.18) |
7.13 (3.85–13.20) |
7.46 (3.95–14.10) |
2.24 (1.17–4.30) |
2.46 (1.26–4.81) |
||||||
| ≥ 500 | Reference | Reference | Reference | Reference | Reference | Reference | ||||||
Adjusted models include all terms in table.
Retention indicator: individuals with at least one visit (clinic or laboratory (CD4 or viral load (VL)) or pharmacy pickup) during 2014.
ART use indicator: prescription of ART for at least 90 days or at least three notations of ART pickup from the pharmacy in 2014 among those retained.
Virologic suppression indicator: viral load (VL)< 200 copies/ml at last measurement in 2014 among those with at least one VL performed in 2014.
OR = odds ratio.
CI = confidence interval.
Low CD4 count at first visit was also associated with virologic suppression (OR: 2.17 for CD4 < 200 and 2.46 for CD4 200–499 vs. ≥ 500 cells/μL; P: 0.023) (Table 2).
DISCUSSION
In this large cohort of HIV-positive ART-naïve patients from Argentina, one-third of patients were not retained in care. Like similar studies performed in other settings, younger age was the primary factor associated with worse retention (10, 11). Younger patients may experience HIV-related stigma, fear of disclosure, and apprehension about losing their jobs more often than older adults do (10).
We also found that worse retention was associated with patient residence outside the city of Buenos Aires. Distance to the clinic and other transportation difficulties are major barriers to retention in care in a wide variety of settings (12, 13). In the city of Buenos Aires, transportation costs are an obstacle for those who are unemployed; for persons who are employed, the barriers include lengthy travel times.
More than one-third of the new patients that we enrolled each year had previously started ART in another center. In the city and province of Buenos Aires, patients can move freely between different ART facilities. Most such patient transfers were not communicated to the clinic of origin (they were “silent transfers”). Therefore, the original clinic counted these patients as lost to care. A previous study in the same HIV-positive adult cohort from the same hospital showed that patients lost to care in the first year of ART were more similar to those known to be alive than those known to be dead (14). Therefore, “silent transfers” might constitute the largest contribution to the lost to follow-up (LTFU) rates that were observed.
In this study, an extended definition for retention was used that accounted not only for clinic visits but also for labs (CD4 count or VL) or pharmacy pickups. This definition made it possible to identify a proportion of patients who received suboptimal care monitoring and, while in care, require targeted interventions. Further characterization of provision of care should also include the evaluation of patients who drop out of care and reenter at a later time.
According to treatment guidelines followed during the study period, patients with a low CD4 count or a high baseline VL were more likely to be prescribed ART (15). Patients with advanced disease were also more likely to be retained, probably through earlier treatment initiation. Yehia et al. noted that the association between retention in care and viral suppression differed by disease severity, and was strongest for patients with a lower CD4 count (16).
The association that low CD4 count at first visit has with virologic suppression should be interpreted with caution. That is because, in the conditional approach we used (in which only individuals meeting one outcome were analyzed in the next step of the HIV care cascade), this effect is limited to patients retained in care and on ART. Therefore, once retention and ART use were achieved, virologic suppression seemed not to be associated with patient baseline characteristics.
Each step of the cascade can be affected by several barriers, both at the individual and system levels. Even when treatment is provided at no cost, such factors as transportation expenses and time away from work may decrease retention.
Our study had several strengths and limitations. The main strength was the use of timely data from an infectious diseases unit within the public health system in Argentina correlated with EMRs and routine data quality assessments (17). Limitations included the lack of a systematic approach to determine health outcomes in patients lost during follow-up, since there was no centralized death registry and most transfers were not notified, i.e., they were “silent transfers.” While we tracked patients in the National HIV and STD Program registries, tracking in other subsystems of the fragmented Argentine health system is ongoing, and might further reduce the proportion of those lost to follow-up. Finally, as this cohort was built from an outpatient unit, the sickest patients diagnosed during admission who never reached ambulatory care may not have been represented; therefore, our results may not be generalizable to the entire HIV-positive population initiating care.
In conclusion, our findings suggest that our hospital is still below the recommended UNAIDS 90-90-90 targets, particularly regarding the major gap in retention in care. Identification of younger age as a factor associated with worse retention will help in the design of targeted interventions. The data presented here might help guide additional efforts to improve treatment outcomes.
We need to further study characteristics of those lost to care at various stages of the HIV care cascade and use estimations of LTFU that include active tracing (18). As universal HIV treatment has been adopted, and ART is been offered to all patients regardless of CD4 count, we estimate that LTFU will decrease and retention will improve in future HIV cascades of care in our population.
Acknowledgments
Funding. This work was supported in part by the NIH-funded Caribbean, Central and South America network for HIV epidemiology (CCASAnet), a member cohort of the International Epidemiologic Databases to Evaluate AIDS (IeDEA) (U01AI069923). This award is funded by the following institutes: Eunice Kennedy Shriver National Institute of Child Health & Human Development (NICHD); Office of The Director, National Institutes of Health (OD); National Institute of Allergy and Infectious Diseases (NIAID); and National Cancer Institute (NCI). The sponsor of this study had no role in study design, data collection, data analysis, data interpretation, or writing of the report. The authors had full access to the data and also had final responsibility for the submission.
Footnotes
Conflicts of interest. All the authors state that they have no conflicts of interest.
Disclaimer. Authors hold sole responsibility for the views expressed in the manuscript, which may not necessarily reflect the opinion or policy of the RPSP/PAJPH or PAHO.
References
- 1.Argentina, Dirección de Sida y ETS, Ministerio de Salud de la Nación Boletín sobre el VIH-sida e ITS en la Argentina. Available from: http://www.msal.gob.ar/images/stories/bes/graficos/0000000852cnt-2015-11-18_boletin-vih-sida-2015.pdf. Accessed 12 April 2016.
- 2.Acuña CH, Chudnovsky M. El sistema de salud en Argentina. Available from: http://www.bibleduc.gov.ar/areas/salud/dircap/mat/matbiblio/salud.pdf Accessed 15 May 2016.
- 3.World Health Organization. A national social health insurance plan for Argentina: simulating its financial feasibility. Available from: http://www.who.int/health_financing/documents/dp_e_10_04-shi_arg.pdf Accessed 15 May 2016.
- 4.Joint United Nations Programme on HIV/AIDS. 90-90-90 an ambitious treatment target to help end the AIDS epidemic. Available from: http://www.unaids.org/sites/default/files/media_asset/90-90-90_en_0.pdf Accessed 10 May 2016.
- 5.Gardner EM, McLees MP, Steiner JF, Del Rio C, Burman WJ. The spectrum of engagement in HIV care and its relevance to test-and-treat strategies for prevention of HIV infection. Clin Infect Dis. 2011;52(6):793–800. doi: 10.1093/cid/ciq243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.McNairy ML, El-Sadr WM. The HIV care continuum: no partial credit given. AIDS. 2012;26(14):1735–8. doi: 10.1097/QAD.0b013e328355d67b. [DOI] [PubMed] [Google Scholar]
- 7.Rebeiro PF, Cesar C, Shepherd BE, De Boni RB, Cortes CP, Rodriguez F, et al. Assessing the HIV Care Continuum in Latin America: progress in clinical retention, cART use and viral suppression. J Int AIDS Soc. 2016;19(1):20636. doi: 10.7448/IAS.19.1.20636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Althoff KN, Rebeiro PF, Hanna DB, Padgett D, Horberg MA, Grinsztejn B, et al. A picture is worth a thousand words: maps of HIV indicators to inform research, programs, and policy from NA-ACCORD and CCASAnet clinical cohorts. J Int AIDS Soc. 2016;19(1):20707. doi: 10.7448/IAS.19.1.20707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mugavero MJ, Amico KR, Horn T, Thompson MA. The state of engagement in HIV care in the United States: from cascade to continuum to control. Clin Infect Dis. 2013;57(8):1164–71. doi: 10.1093/cid/cit420. [DOI] [PubMed] [Google Scholar]
- 10.Yehia BR, Rebeiro P, Althoff KN, Agwu AL, Horberg MA, Samji H, et al. Impact of age on retention in care and viral suppression. J Acquir Immune Defic Syndr. 2015;68(4):413–9. doi: 10.1097/QAI.0000000000000489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rebeiro P, Althoff KN, Buchacz K, Gill J, Horberg M, Krentz H, et al. Retention among North American HIV-infected persons in clinical care, 2000–2008. J Acquir Immune Defic Syndr. 2013;62(3):356–62. doi: 10.1097/QAI.0b013e31827f578a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Geng EH, Nash D, Kambugu A, Zhang Y, Braitstein P, Christopoulos KA, et al. Retention in care among HIV-infected patients in resource-limited settings: emerging insights and new directions. Curr HIV/AIDS Rep. 2010;7(4):234–44. doi: 10.1007/s11904-010-0061-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Yehia BR, Stewart L, Momplaisir F, Mody A, Holtzman CW, Jacobs LM, et al. Barriers and facilitators to patient retention in HIV care. BMC Infect Dis. 2015;15:246. doi: 10.1186/s12879-015-0990-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Tuboi SH, Schechter M, McGowan CC, Cesar C, Krolewiecki A, Cahn P, et al. Mortality during the first year of potent antiretroviral therapy in HIV-1-infected patients in 7 sites throughout Latin America and the Caribbean. J Acquir Immune Defic Syndr. 2009;51(5):615–23. doi: 10.1097/QAI.0b013e3181a44f0a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Argentina, Ministerio de Salud, Dirección de Sida y ETS. Guía para el manejo de los pacientes adultos con infección por VIH. Available from: http://www.msal.gob.ar/images/stories/bes/graficos/0000000109cnt-2013-05_guia-manejo-pacientes-adultos.pdf Accessed 10 May 2016.
- 16.Yehia BR, French B, Fleishman JA, Metlay JP, Berry SA, Korthuis PT, et al. Retention in care is more strongly associated with viral suppression in HIV-infected patients with lower versus higher CD4 counts. J Acquir Immune Defic Syndr. 2014;65(3):333–9. doi: 10.1097/QAI.0000000000000023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Duda SN, Shepherd BE, Gadd CS, Masys DR, McGowan CC. Measuring the quality of observational study data in an international HIV research network. PloS One. 2012;7(4):e33908. doi: 10.1371/journal.pone.0033908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Tweya H, Feldacker C, Estill J, Jahn A, Ng’ambi W, Ben-Smith A, et al. Are they really lost? “true” status and reasons for treatment discontinuation among HIV infected patients on antiretroviral therapy considered lost to follow up in Urban Malawi. PloS One. 2013;8(9):e75761. doi: 10.1371/journal.pone.0075761. [DOI] [PMC free article] [PubMed] [Google Scholar]


