Sir,
A 60-year-old lady presented with multiple violaceous plaques, nodules, and a proliferating growth on the right knee. She had multiple oval and linear, 7 × 4 cm to 8 × 3 cm, hypertrophic verrucous plaques and nodules with a violaceous rim and hypopigmented center. These plaques and nodules were present on bilateral forearms, left palm, left ankle, and right knee [Figure 1] for the last 5 years, and were associated with slight itching. In the last 6 months, the plaque on the right knee showed a gradually progressing circular nodule, 5 × 5 cm, with a moist surface and indurated base and bled on slight touch [Figure 2]. Regional lymphadenopathy was absent. There was no systemic complaint. Biopsy from the hypertrophic violaceous plaque on the knee showed hyperkeratosis, irregular epidermal acanthosis with saw-tooth type rete pegs, and focal basal layer vacuolar degeneration. The superficial dermis and dermoepidermal junction showed lymphohistiocytes in a band-like pattern suggestive of hypertrophic lichen planus (LPH) [Figure 3]. Biopsy from the proliferating nodule did not have any epidermis or dermis. Sections showed sheets of proliferating keratinocytes and tiny squamous pearls with mild pleomorphism of keratinocytes suggestive of well-differentiated squamous cell carcinoma (SCC) [Figure 4]. Routine investigations, chest X-ray, human immunodeficiency virus (HIV), anti-hepatitis C virus (HCV), HBSAg, and abdominal ultrasound study were within normal limits. Magnetic resonance imaging (MRI) showed two lymphnodes of size 1 cm in the right inguinal region which on fine needle aspiration showed reactive lymphadenitis. The patient was referred to an oncosurgeon for wide local excision and primary closure. The excised specimen showed moderately differentiated SCC with tumor depth of 0.8 cm. The superior, inferior, medial, and lateral skin, soft tissue, and deep margins were free of tumor.
Figure 1.
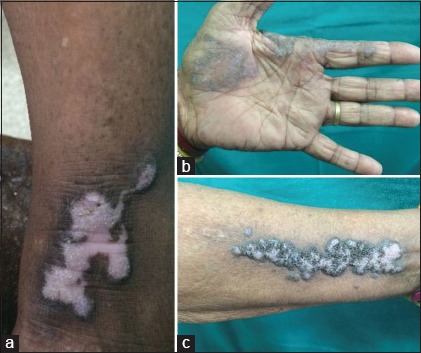
(a) Verrucous irregular plaque on the left lower leg with violaceous rim. (b) Verrucous, violaceous linear plaque on the left palm. (c) Verrucous, violaceous linear plaque on the left forearm
Figure 2.

Violaceous plaque with central hypopigmentation on the right knee with an eccentrically placed proliferating nodule
Figure 3.
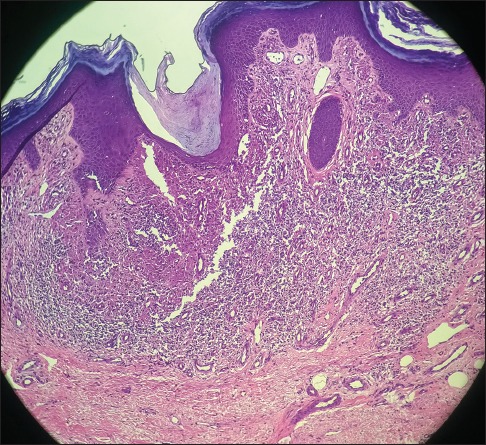
Section shows hyperkeratosis and irregular epidermal acanthosis with saw-tooth rete pegs and focal basal layer vacuolar degeneration. The superficial dermis and dermoepidermal junction show lymphohistiocytes in a band-like pattern suggestive of lichen planus hypertrophicus. (H and E, ×200)
Figure 4.
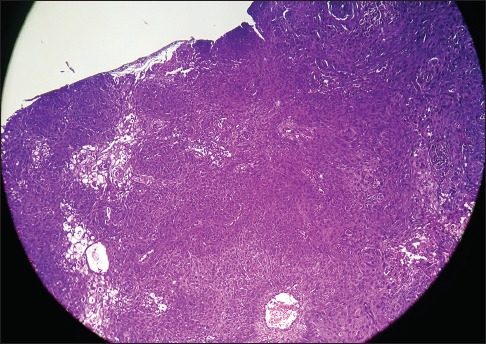
Sections show sheets of proliferating keratinocytes and tiny squamous pearls with mild pleomorphism of keratinocytes suggestive of well-differentiated squamous cell carcinoma. (H and E, ×400)
Lichen planus is not a common premalignant condition; a study showed only 8 SCC developing in 2071 patients of lichen planus followed up for over 9.9 years.[1] LPH and oral lichen planus are two variants which have a higher risk of malignant transformation. Till December 2015, 38 cases of SCC developing in LPH have been reported.[2] SCC arising from LPH is most commonly seen on the lower limbs, similar to this case, but it has also been reported at other sites such as the glans penis.[3,4] The average age of presentation is 61.4 years in women and 51.3 years in men,[2] however, it can also occur in young patients.[3,5] Previously, X-ray and arsenic treatment were considered to be risk factors for the development of SCC in LPH,[3] however, another review did not reveal any significant predisposing factors such as personal history of malignancy, use of phototherapy, systemic immunosuppressant, or actinic damage.[2] In our case, no predisposing factor for the development of SCC could be determined. The average lag time from onset of LPH to development of SCC was determined to be 11 years. In our case, the lag time was significantly shorter at 5 years. This has been seen in other reports also that women had a shorter lag time to development of SCC than men.[2] Majority (42.1%) of the SCC developing in LPH are well-differentiated and localized, and include variants such as keratoacanthoma and verrucous carcinoma, however, metastatic SCC has also been reported.[3]
The pathogenesis of SCC in LPH is said to be due to chronic antigen stimulation and increased cell turnover.[6] Chronic antigenic stimulation by drugs or viruses, chronic pruritus, and scratching may contribute to the pathogenesis.
Pseudoepithelial hyperplasia, which clinically mimics SCC, is an important differential diagnosis for proliferating growth on LPH.[7] It is important to take a deep biopsy of such growths to include some portion of the dermis. A shave biopsy or superficial biopsy may not be sufficient to differentiate the two.[8] Certain features on biopsy such as benign irregular hyperplasia of the epidermis, moderate dyskeratosis, horn cyst formation, and presence of E-cadherin staining pattern can help to differentiate pseudoepithelomatous hyperplasia from SCC.[8]
In conclusion, even though malignant transformation of LPH is rare, one must keep in mind its occurrence. Changes such as rapid growth of pre-existing lesion, ulceration, verrucous changes, bleeding on touch, and not responding to conventional treatment when other existing lesions are responding are some indications for histopathological examination to rule out malignancy.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Sigurgeirsson B, Lindelöf B. Lichen planus and malignancy. An epidemiologic study of 2071 patients and a review of the literature. Arch Dermatol. 1991;127:1684–8. doi: 10.1001/archderm.127.11.1684. [DOI] [PubMed] [Google Scholar]
- 2.Knackstedt TJ, Collins LK, Li Z, Yan S, Samie FH. Squamous Cell Carcinoma Arising in Hypertrophic Lichen Planus: A Review and Analysis of 38 Cases. Dermatol Surg. 2015;41:1411–8. doi: 10.1097/DSS.0000000000000565. [DOI] [PubMed] [Google Scholar]
- 3.Tong LX, Weinstock M, Drews R, Sheikine Y, Kim CC. Widely metastatic squamous cell carcinoma originating from malignant transformation of hypertrophic lichen planus in a 24-year-old woman: Case report and review of the literature. Pediatr Dermatol. 2015;32:e98–101. doi: 10.1111/pde.12549. [DOI] [PubMed] [Google Scholar]
- 4.Wörheide J, Bonsmann G, Kolde G, Hamm H. Squamous epithelial carcinoma at the site of lichen ruber hypertrophicus of the glans penis. Hautarzt. 1991;42:112–5. [PubMed] [Google Scholar]
- 5.Joshi R, Durve U. Squamous cell carcinoma in hypertrophic lichen planus. Indian J Dermatol Venereol Leprol. 2007;73:54–5. doi: 10.4103/0378-6323.30658. [DOI] [PubMed] [Google Scholar]
- 6.Krasowska D, Bogaczewicz J, Chodorowska G. Development of squamous cell carcinoma within lesions of cutaneous lichen planus. Eur J Dermatol. 2007;17:447–8. doi: 10.1684/ejd.2007.0249. [DOI] [PubMed] [Google Scholar]
- 7.Speziali L, Pusiol T, Zorzi MG, Morichetti D, Zumiani G. Pseudoepitheliomatous hyperplasia arising from hypertrophic lichen planus mimicking squamous cell carcinoma. G Ital Dermatol Venereol. 2011;146:310–1. [PubMed] [Google Scholar]
- 8.Pusiol T, Zorzi MG, Morichetti D, Speziali L. Pseudoepitheliomatous hyperplasia arising from hypertrophic lichen planus mimicking squamous cell carcinoma: Limited value of immunohistochemistry. Acta Dermatovenerol Croat. 2012;20:112–4. [PubMed] [Google Scholar]


