Abstract
Alveolar capillary dysplasia with misalignment of pulmonary veins (ACDMPV) is a lethal lung developmental disorder caused by heterozygous point mutations or genomic deletion copy-number variants (CNVs) of FOXF1 or its upstream enhancer involving fetal lung-expressed long noncoding RNA genes LINC01081 and LINC01082. Using custom-designed array comparative genomic hybridization, Sanger sequencing, whole exome sequencing (WES), and bioinformatic analyses, we studied 22 new unrelated families (20 postnatal and two prenatal) with clinically diagnosed ACDMPV. We describe novel deletion CNVs at the FOXF1 locus in 13 unrelated ACDMPV patients. Together with the previously reported cases, all 31 genomic deletions in 16q24.1, pathogenic for ACDMPV, for which parental origin was determined, arose de novo with 30 of them occurring on the maternally inherited chromosome 16, strongly implicating genomic imprinting of the FOXF1 locus in human lungs. Surprisingly, we have also identified four ACDMPV families with the pathogenic variants in the FOXF1 locus that arose on paternal chromosome 16. Interestingly, a combination of the severe cardiac defects, including hypoplastic left heart, and single umbilical artery were observed only in children with deletion CNVs involving FOXF1 and its upstream enhancer. Our data demonstrate that genomic imprinting at 16q24.1 plays an important role in variable ACDMPV manifestation likely through long-range regulation of FOXF1 expression, and may be also responsible for key phenotypic features of maternal uniparental disomy 16. Moreover, in one family, WES revealed a de novo missense variant in ESRP1, potentially implicating FGF signaling in etiology of ACDMPV.
Keywords: Copy-number variants, genomic imprinting, hypoplastic left heart syndrome and single umbilical artery, transcriptional enhancer, uniparental disomy
INTRODUCTION
Alveolar capillary dysplasia with misalignment of pulmonary veins (ACDMPV; MIM 265380) is a lethal neonatal lung disorder caused by abnormalities in air-blood barrier structure and function (Langston 1991; Bishop et al. 2011). Affected newborns typically present with severe respiratory failure and refractory pulmonary hypertension within a few hours after birth and die in the first month of life. Histopathologically, ACDMPV is characterized by decrease in number of capillaries adjacent to the alveolar epithelium, alveolar wall thickening, hypertrophy of the muscular layer of small pulmonary arteries with abnormal muscular extensions into intra-acinar vessels, and malposition of the small pulmonary veins. In addition, the majority of patients with ACDMPV manifest extra-pulmonary anomalies of the gastrointestinal, genitourinary, and cardiovascular systems (Sen et al. 2004; Bishop et al. 2011).
Heterozygous point mutations in FOXF1 (OMIM 601089) and genomic deletion copy-number variants (CNVs) at chromosomal region 16q24.1 including FOXF1 or its upstream regulatory region have been identified in the vast majority of patients with ACDMPV (Stankiewicz et al. 2009; Sen et al. 2013a, b; Szafranski et al. 2013a, b; Szafranski et al. 2014). FOXF1, expressed in lung mesenchyme and vascular endothelium, belongs to the forkhead family of transcription factors, and is a target of sonic hedgehog signaling (SHH) from epithelium.
Homozygous Foxf1−/− mice die by embryonic day 8.5 because of defects in the development of extraembryonic and lateral mesoderm-derived tissues (Mahlapuu et al. 2001), whereas heterozygous Foxf1+/− mice exhibit features resembling ACDMPV (Kalinichenko et al. 2001).
The FOXF1 promoter overlaps a CpG island, does not contain a TATA-box, and requires enhancer function for its activity (Chang et al. 2001; Kim et al. 2005; Szafranski et al. 2013a,b). We have shown that the lung-specific enhancer region, mapping ~270 kb upstream of FOXF1, harbors genes for long non-coding RNAs (lncRNAs) that regulate FOXF1 expression (Szafranski et al. 2013a; Szafranski et al. 2014). Further, we have also identified another FOXF1 enhancer located within the FOXF1 intron (Szafranski et al. 2013b).
Interestingly, all 17 reported pathogenic genomic deletions involving FOXF1 or its upstream regulatory regions, for which parental origin was determined, arose de novo on the maternal chromosome 16, suggesting that the FOXF1 locus is imprinted (Stankiewicz et al. 2009; Sen et al. 2013b; Szafranski et al. 2013a, b; Dharmadhikari et al. 2015). Segregation analysis of a missense mutation in FOXF1 (c.416G>T; p. Arg139Leu) in a familial case of ACDMPV provided additional support for imprinting of FOXF1 in humans (Sen et al. 2013a). Furthermore, previous bioinformatics studies, aimed at identification of imprinted genes, indicated that the FOXF1 locus may be imprinted (Luedi et al. 2007).
We present 13 novel ACDMPV-causing de novo deletion CNVs in 16q24.1, 12 of which arose on maternal chromosome 16, providing statistically significant support for imprinting of the FOXF1 locus. Surprisingly, we also identified one small pathogenic genomic deletion in the upstream regulatory region and three causative variants involving FOXF1 that all arose on paternal chromosome 16, highlighting the complexity of genomic and epigenetic regulation of FOXF1 expression that underlies etiology of ACDMPV. Lastly, we describe the results of whole exome sequencing (WES) in three unrelated ACDMPV families negative for both FOXF1 point mutations and deletion CNVs. Our results demonstrate complexity of genomic and epigenetic regulation of the FOXF1 gene in 16q24.1 and implicate the role of other genes in ACDMPV.
METHODS
Subject recruitment
After informed consent, using protocols approved by the Institutional Review Board for Human Subject Research at Baylor College of Medicine (BCM) (H8712), histopathological specimens and DNA samples (peripheral blood or lung) from probands with ACDMPV: 20 postnatal (pts 114.3, 115.3, 117.3, 119.3, 120.3 (Decipher 285653), 121.3, 122.3, 123.3, 124.3, 125.3, 126.3, 127.3, 128.3, 130.3, 133.3, 134.3, 136.3, 138.5, 139.3, and 141.3) and two prenatal (135.3 and 140.3) and their family members (blood) were obtained.
Histopathological studies
Histopathological evaluations of all cases suspected of ACDMPV were performed in formalin-fixed paraffin-embedded (FFPE) specimens from lung biopsies or autopsies stained with hematoxylin and eosin.
Molecular biology
DNA isolation and sequencing, RNA isolation, RT-qPCR, cloning of the 16q24.1 region deleted in patient 122.3 and of the FOXF1 promoter, and transcriptional activity assay were performed as described in Supplemental Methods.
Array CGH analyses
Genomic CNVs in the FOXF1 locus were analyzed using customized 16q24.1 region-specific (1 Mb region flanking FOXF1) high-resolution 4×180K microarrays, manufactured by Agilent Technologies (Santa Clara, CA, USA), as previously described (Szafranski et al. 2013a) (pts 114.3, 115.3, 117.3, 119.3, 120.3 (Decipher 285653), 121.3, 122.3, 125.3, 126.3, 127.3, 128.3, 133.3, 135.3, 136.3, 139.3, and 140.3).
Characterization of deletion breakpoints
Deletion junction fragments were amplified using long-range PCR with LA Taq DNA polymerase (TaKaRa Bio, Madison, WI, USA) and primers designed by Primer3 software (http://frodo.wi.mit.edu/primer3) as described (Szafranski et al. 2013a, b). The sequence of a complex genomic rearrangement in exon 1 of FOXF1 has been deposited in the GenBank database (http://ncbi.nlm.nih.gov/genbank) under accession number KT963011.
Parental origin of deletions and point mutations
Parental origin of the deletions was determined using informative microsatellites or single nucleotide polymorphisms (SNPs) mapping to the deleted genomic interval. For point mutations, PCR product containing the pathogenic variants and the neighboring SNPs were cloned into pGEM-T vector (Promega, Madison, WI, USA) and 10 clones were used for plasmid isolation and sequencing.
Bioinformatic analysis of the distant upstream FOXF1 enhancer region
Reference DNA sequences, chromatin modification, location of CpG islands, and ChIP-seq data for the selected transcription regulators were accessed using the UCSC Genome Browser (http://genome.ucsc.edu, GRCh37/hg19). High-throughput chromosome conformation capture (Hi-C) analyses were performed as described in Supplemental Methods.
Whole exome sequencing
Three family trios with sporadic ACDMPV, negative for FOXF1 mutations and deletions (using Sanger sequencing and custom-designed region-specific high-resolution array CGH) (pts 114.3, 121.3, and 128.3), were analyzed using whole exome sequencing (WES) as described in Supplemental Methods.
RESULTS
Clinical characterization
Histopathological examination of lung specimens revealed the characteristic pathognomonic features of ACDMPV in all cases analyzed. Identified anomalies involving other organs are listed in Table 1 and Supplemental Table S1.
Table 1.
Additional non-lung clinical features in 37 ACDMPV patients with the reported and novel pathogenic deletions involving the FOXF1 locus in chromosome 16q24.1. Features present in greater than 10% of patients are bolded.
| Cardiac | Frequency | Gastrointestinal | Frequency | Genitourinary | Frequency | Other | Frequency |
|---|---|---|---|---|---|---|---|
| Patent ductus arteriosus | 17 (46%) | Intestinal malrotation | 8 (22%) | Hydronephrosis | 9 (24%) | Single umbilical artery | 7 (19%) |
| Atrioventricular septal defect | 6 (16%) | Annular pancreas | 4 (11%) | Renal pelviectasis | 5 (14%) | Broad flat nasal bridge | 2 (5%) |
| Hypoplastic left heart syndrome | 5 (14%) | Imperforate anus | 3 (8%) | Hydroureter | 4 (11%) | Deep-set eyes | 2 (5%) |
| Ventricular septal defect | 5 (14%) | Duodenal atresia | 2 (5%) | Hypospadias | 2 (5%) | Butterfly vertebra | 2 (5%) |
| Atrial septal defect | 4 (11%) | Duodenal dilation proximal to the pancreas | 1 (3%) | Bicornuate uterus with cervical duplication/Uterus didelphys | 2 (5%) | Cystic hygroma | 2 (5%) |
| Patent foramen ovale | 3 (8%) | Absent spleen | 1 (3%) | Tortuous dilated ureters and thickened urinary bladder wall, | 1 (3%) | Fetal hydrops | 2 (5%) |
| Aortic coarctation | 3 (8%) | Abnormal placement of anus | 1 (3%) | Right renal cyst extending into the abdomen | 1 (3%) | Segmental abnormality of T10 vertebral body | 1 (3%) |
| Bicuspid aortic valve | 3 (8%) | Esophageal atresia | 1 (3%) | Posterior rib fusions | 1 (3%) | ||
| Persistent left superior vena cava | 3 (8%) | Tracheoesophageal fistula | 1 (3%) | Brachycephaly | 1 (3%) | ||
| Tetralogy of Fallot | 2 (5%) | Adhesions between bowel loops, second part of duodenum and gallbladder | 1 (3%) | Cleft lip | 1 (3%) | ||
| Significant R/L shunt | 2 (5%) | Stomach and initial part of intestines malformed and tubular in nature | 1 (3%) | Cleft palate | 1 (3%) | ||
| Hypoplasia of mitral valve | 2 (5%) | Suspected bowel obstruction | 1 (3%) | Pleural effusion | 1 (3%) | ||
| Pulmonary artery stenosis | 2 (5%) | Shortened mesenteric root with kinking and luminal narrowing of the small intestine | 1 (3%) | Polyhydramnios | 1 (3%) | ||
| Hypoplastic aortic arch | 2 (5%) | Omphalocele with a diameter of 6 cm only intestines present | 1 (3%) | Hypertelorism | 1 (3%) | ||
| Right ventricular dilatation and hypertrophy | 2 (5%) | Bilateral choroid plexus cysts | 1 (3%) | ||||
| Hypoplasia of left ventricle | 2 (5%) | Mild retrognathia | 1 (3%) | ||||
| Interrupted aortic arch | 1 (3%) | Thickened nuchal fold | 1 (3%) | ||||
| Dilated pulmonary artery | 1 (3%) | Bilateral cerebellar heterotopia | 1 (3%) | ||||
| Parachute configuration of mitral valve with mild dilation of the left ventricle | 1 (3%) | Hypoglycaemia | 1 (3%) | ||||
| Dysplastic tricuspid valve and two mitral valve leaflets | 1 (3%) | Hypotonia | 1 (3%) | ||||
| Pulmonary valve atresia | 1 (3%) | ||||||
| Right ventricular outflow tract obstruction |
Genomic deletions
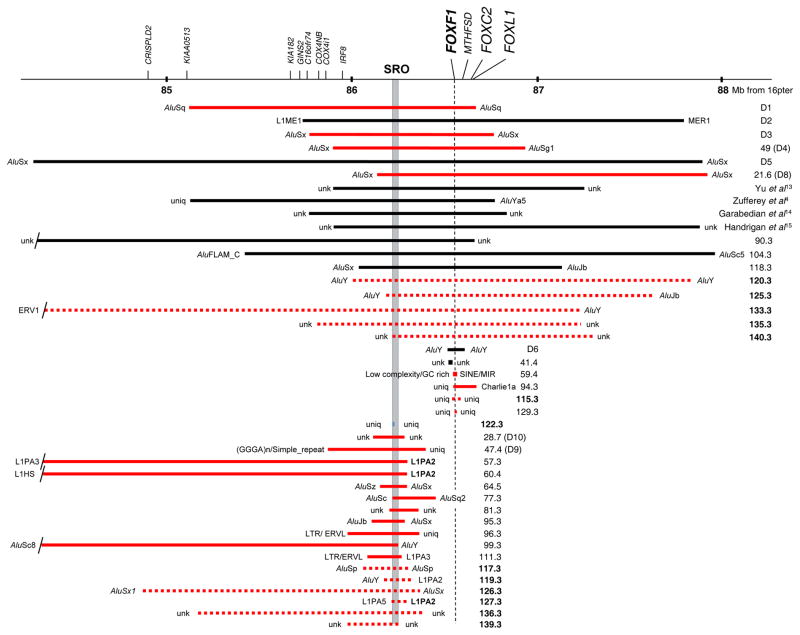
We identified and characterized novel different-sized genomic deletions at 16q24.1 in 13 unrelated patients with ACDMPV (pts 115.3, 117.3, 119.3, 120.3 (Decipher 285653), 122.3, 125.3, 126.3, 127.3, 133.3, 135.3, 136.3, 139.3, and 140.3) (Fig. 1 and Supplemental Table S1). Twelve out of 13 deletions (pts 115.3, 117.3, 119.3, 120.3, 125.3, 126.3, 127.3, 133.3, 135.3, 136.3, 139.3 and 140.3), for which the parental origin could have been determined, arose de novo on the maternal chromosome 16 (Supplemental Table S1). In one of those cases (pt 115.3), the CNV deletion involved only FOXF1, in five cases (pts 118.3, 120.3, 125.3, 133.3, 135.3, and 140.3), deletions encompassed FOXF1 and its upstream enhancer region, and in seven cases (pts 117.3, 119.3, 122.3, 126.3, 127.3, 136.3, and 139.3) the deletion CNVs harbored only the upstream enhancer, leaving FOXF1 intact. We did not find any evidence of somatic mosaicism in the parental DNA samples from peripheral blood using PCR with primers specific for the patients’ deletion junction fragment. Recently, we showed that new mutations that occur in the maternal allele are more likely to be recurrently transmitted to offspring (Campbell et al. 2014). Given that all published and all but one described here new deletions in the 16q24.1 FOXF1 region arose de novo on the maternal chromosome 16, the recurrence risk for ACDMPV may potentially be elevated in comparison to that observed for other sporadic diseases.
Fig. 1.
A compilation of chromosome 16q24.1 deletions pathogenic for ACDMPV. Deletions which occurred on maternal chromosome 16, are shown in red, the deletion on paternal chromosome is shown in blue, and deletions, for which parental origin could not be determined, are shown in black. Numbers refer to ACDMPV cases. Locations of deletion breakpoints (BPs) are indicated by names of flanking repetitive elements. Abbreviations: SRO, (smallest deletion overlap - delineating upstream enhancer region); unk, unknown sequence; uniq, unique sequence. Note that most of the deletions are flanked by retrotransposons, mainly by Alu repetitive segments. The LIPA2 element (chr16:86,266,902-86,272,916, GRCh37/hg19) within LINC01081 at three distal deletion breakpoints in patients 57.3, 60.4, and 127.3 is bolded (Supplemental Table S1). Thirteen novel deletions are dashed and their number bolded to distinguished from the published cases.
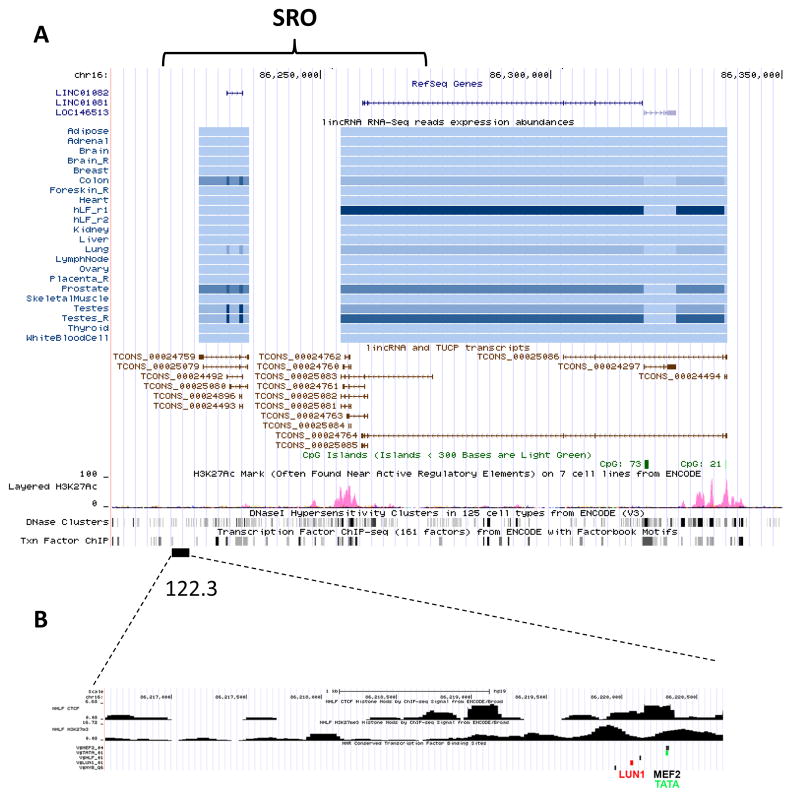
In patient 122.3, we identified a small ~ 4.1 kb de novo deletion in the centromeric portion of the upstream FOXF1 enhancer region, mapping ~ 9.1 kb upstream to LINC01082 (Fig. 2). Surprisingly, three informative SNPs, mapping to the deleted region, consistently showed that the deletion arose de novo on the paternal chromosome 16 (Supplemental Table S1).
Fig. 2.
UCSC browser display of the enhancer region upstream to FOXF1. a An ~ 60 kb SRO showing overlapping LINC01081 and LINC01082, CpG islands, H3K27Ac methylation, DNaseI hypersensitivity clusters, and transcription factor ChIP-Seq data. b The ~ 4.1 kb deletion CNV identified in pt 122.3 maps to the FOXF1 upstream enhancer region. Location of the transcription factor and CTCF binding sites, and a diagram of histone modification in the deleted region is shown.
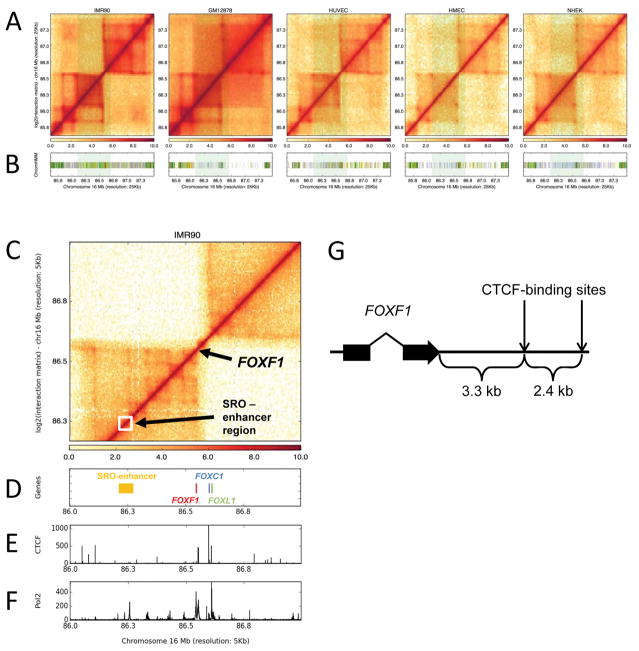
Bioinformatic analyses of the FOXF1 locus on 16q24.1
Hi-C analysis of chromatin interactions around the FOXF1 gene revealed that FOXF1 and its upstream enhancer reside within the same topologically associated domain (TAD), spanning ~400 kb upstream of FOXF1 (Fig. 3). Intriguingly, FOXF1 maps at the distal edge of the TAD (Fig. 3), consistently with previous suggestion by Parris et al. (2013) based on distribution of the CTCF binding sites. This domain exhibits stronger or more frequent chromatin interactions within its boundaries in fetal lung fibroblasts IMR-90 compared to non-lung cell lines: GM12878, HUVEC, NHEK, and HMEC. The strength of these interactions positively correlated with FOXF1 expression, which was stronger in IMR-90 cells than in, e.g., HUVEC, and was around the threshold level in peripheral blood lymphocytes (GM12878).
Fig. 3.
Genomic in cis interactions at chromosome 16q24.1. a Hi-C contact maps are visualized as heatmaps for IMR-90, GM12878, HUVEC, NHEK, and HMEC cell lines. b Tiles mark active TSS (red), transcribed (green), enhancer (yellow), low (gray) and heterochromatin (purple) state calls with ChromHMM within the represented locus. Shaded region highlights the active chromatin region in IMR-90 cells whereas the same locus in not enriched for active chromatin states in other cell types, especially on the left-side of TAD boundary. c Zoomed-in view of Hi-C contact map around the FOXF1 locus in IMR-90 cells at 5 kb resolution. d Tiles mark genomic locations of SRO-enhancer region (yellow) and FOXF1 (red), FOXC1 (blue) and FOXL1 (green) genes. e Histogram represents CTCF ChIP-seq enrichment levels within the visualized locus. f Histogram represents RNA PolII ChIP-Seq enrichment levels. g Positions of two strong CTCF-binding sites (chr16:86,551,417–528 and 86,553,812–944; hg19) at the TAD boundary, 3.3 and 5.7 kb downstream of the 3′ end of FOXF1 (chr16: 86,548,070; hg19).
In silico analysis of the FOXF1 upstream enhancer region identified an 880 bp-long CpG island (71% GC-rich) located 0.3 kb from the known transcription start site of LINC01081 (Supplemental Fig. S1). We have previously shown that LINC01081 positively regulates FOXF1 expression (Szafranski et al. 2014). The methylation status of this CpG island is unknown. However, if this region is differentially methylated, it might contribute to the proposed epigenetic regulation of LINC01081 and thus also FOXF1 expression.
We also found that the ~4.1 kb region of the FOXF1 upstream enhancer, adjacent upstream to another lncRNA gene, LINC01082 and deleted in patient 122.3, contains the TATA-box (TTATAAATAGGAATT; chr16:86,220,297-86,220,311) and the binding sites for several transcription factors including myocyte enhancer factor-2 (MEF2), RING finger protein LUN1, hepatic leukemia factor (HLF), and myeloblastosis proto-oncogene protein (MYB) (Fig. 2a). Importantly, LUN1 and MEF2 are relatively highly expressed in the human lungs (Brand et al. 1997; Chu et al. 2001), and might be involved in long distance interaction with the FOXF1 promoter.
Reporter assay
Because the 4.1 kb region, deleted in patient 122.3, contains the TATA-box located close to the lncRNA gene, LINC01082, we tested whether this region exhibits promoter activity. We found that the deleted fragment did not exhibit any promoter activity, even when compared with the residual activity of the FOXF1 promoter (Supplemental Fig. S2), suggesting instead its function as a scaffold for LUN1, MEF2 and TATA-binding TFIID.
Molecular mechanisms of formation of 16q24.1 deletions
To infer the molecular mechanism of formation of the identified deletions and to better assess their recurrence risk, we mapped and sequenced 18 breakpoint junctions of nine 16q24.1 deletion CNVs (Fig. 1, Supplemental Table S1). Twelve breakpoints map to Alu repeats and three within LINE1 elements. In total, 53% (16 out of 30) of all characterized 16q24 deletions were Alu-Alu-mediated. Interestingly, in three cases (pts 57.3, 119.3, 127.3), the deletion breakpoints map to the same LINE element L1PA2 (chr16:86,266,902-86,272,916, GRCh37/hg19) within LINC01081, indicating that it is a genomic recombination hotspot (Fig. 1 and Supplemental Table S1). Microhomologies between 7 and 41 bp were found in six out of 10 cases analyzed, suggesting that those six deletions might have arisen by a template switching replicative mechanism such as fork stalling and template switching (FoSTeS), or microhomology-mediated break-induced replication (MMBIR) (Hastings et al. 2009).
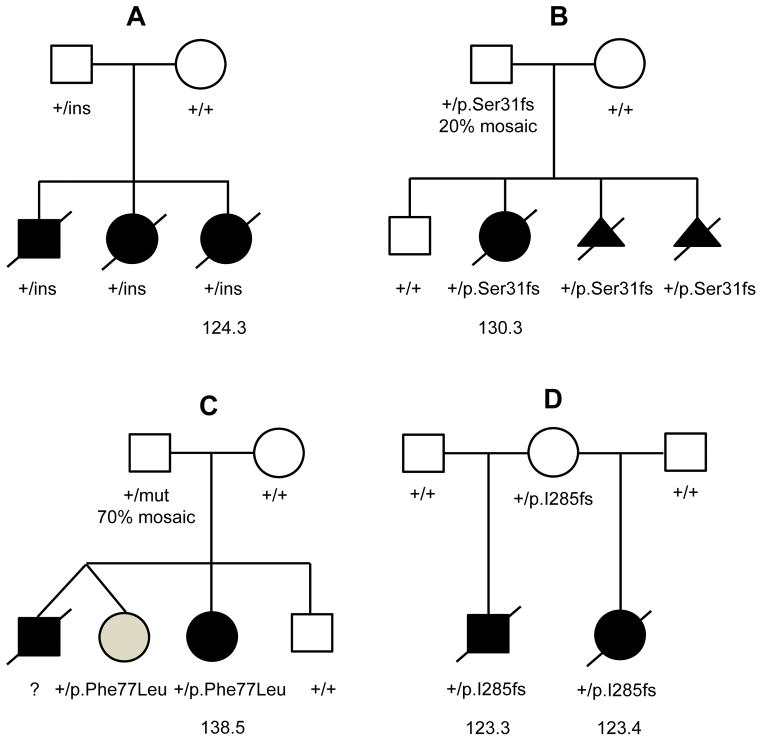
Familial cases of parentally transmitted FOXF1 mutations
We have identified three ACDMPV families with novel pathogenic variants in FOXF1 transmitted from the reportedly healthy carrier fathers (Fig. 4). Sequencing of FOXF1 and its flanking regions in patient 124.3 (Fig. 4a) revealed a complex genomic rearrangement within a noncoding portion of the FOXF1 1st exon, mapping six base pairs upstream of the FOXF1 ATG codon (Supplemental Fig. S3a). A copy of a portion of the 1st intron of the lncRNA FENDRR (chr16:86,540,260/271-86,540,607/610), encoded upstream and opposite to FOXF1, was inserted into the untranslated portion of the FOXF1 1st exon, replacing 5 to 15 bp in the position chr16:86,544,155/165-86,544,169. In addition, 265 bp of this inserted fragment (chr16:86,540,342-86,540,607/610) was inverted. This small insertion occurred within the centromeric portion of (CGG)n simple repeat, which is normally divided by a unique sequence containing the FOXF1 AUG codon (Supplemental Fig. S3b). Importantly, it also introduced five alternative AUG initiation codons into the 5′ untranslated part of the FOXF1 1st exon, none of which is in frame with FOXF1, generating potential translation start sites for five novel peptides. This complex rearrangement within FOXF1 was inherited from the reportedly healthy father, in whom it arose de novo on the grandmaternal chr16. No evidence of somatic mosaicism of this rearrangement was detected in grandmaternal peripheral blood DNA.
Fig. 4.
Unusual inheritance and manifestation of pathogenic variants in the FOXF1 locus. Pedigrees of ACDMPV families with reportedly healthy parent transmitting FOXF1 pathogenic variant to their affected children. a Family 124 with the complex genomic insertion rearrangement (ins) within the 5′ non-coding part of the FOXF1 1st exon. b Family 130 with the frameshift mutation within the FOXF1 1st exon. c Family 138 with the pathogenic missense mutation in the FOXF1 1st exon transmitted by healthy father, 70% mosaic in peripheral blood. A twin sister (shaded symbol) of the deceased ACDMPV patient has partial anomalous venous return (Reiter et al. (2016). d Family 123 with the frameshift mutation transmitted by healthy mother, likely germline mosaic for the mutation.
In family 130 (Fig. 4b) with two children affected by ACDMPV, we found a deletion of five nucleotides in the coding region of the FOXF1 1st exon, resulting in a translational frameshift (c.90_96del; p.Ser31fs). This pathogenic variant occurred de novo in the father who was found to be approximately 20% mosaic for the mutation in the peripheral blood nucleated cells.
We found a missense FOXF1 mutation c.C231A, (p.Phe77Leu) in family 138 (Fig. 4c) with four children, one of them affected by ACDMPV, that was inherited from the healthy father who was approximately 70% mosaic for the mutation in the peripheral blood nucleated cells (Reiter et al. 2016).
In family 134 (pedigree not shown), the affected newborn had an in-frame duplication c.54_59dup (p.Gly22_Gly23dup) in the 1st exon of FOXF1. The variant was located within a stretch of 11 Gly residues. There are few known in-frame deletions and duplications within this Gly repeat (e.g., p.Gly19del, p.Gly13_Gly17del, p.Gly17dup), listed in the ExAC database (http://exac.broadinstitute.org), interpreted as non-pathogenic. Moreover, the number of Gly in this repeat varies between species (e.g., there are six residues in rabbit, 12 in macaque). The healthy father is heterozygous for this variant. Therefore, we concluded that this Gly duplication is unlikely to be pathogenic for ACDMPV. Thus, the causative factor for the disease in this case remains unknown.
In addition, in family 123 (Fig. 4d), two siblings died of ACDMPV six years apart. Sequencing of FOXF1 from one of the siblings revealed the presence of a deleterious frame-shift mutation c.849_850del (p.I285fs) in the 1st exon. This variant was the cause of ACDMPV also in the other sibling, and was transmitted from the healthy mother who is likely germline mosaic or low-level somatic mosaic.
Whole exome sequencing
Three ACDMPV cases (families 114, 121, and 128), negative for FOXF1 mutations and CNVs in FOXF1 or its upstream enhancer region, were analyzed by WES to identify additional to FOXF1 ACDMPV genes. From the list of variants obtained for each proband, we filtered out synonymous or non-exonic SNVs/indels and variants with minor allele frequency > 1% in 1000 Genomes, Exome Variant Server, and in-house exome databases, which left 762 (pt 114.3), 681 (pt 121.3), and 709 (pt 128.3) variants. Analysis of WES data in family 114 revealed one de novo missense mutation c.1564T>C (p.Trp522Arg) in ZMYND11 validated by Sanger sequencing (Table 2). In family 121, we identified four de novo variants confirmed by Sanger sequencing: missense mutations c.463C>T (p.Arg155Cys) in SLC50A1 and c.881A>G (p.Tyr294Cys) in ESRP1, a non-frameshift deletion c.533_542delinsC (p.Ser179_Ser173del) in MPRIP, and a frameshift insertion c.2819_2820insT (p.Gly941fs) in DOCK8 (Table 2). None of those de novo variants were present in ESP or 1000 Genomes databases. By exploring ExAC database we found that the variant in SLC50A1 was reported in two healthy individuals (of Latino and European ancestry) and the variant in MPRIP was present in 152 individuals (MAF=0.0015). However, given the complexity of the FOXF1 locus and its epigenetic regulation, none of these variants should be definitively excluded as a potential contributor to ACDMPV. In family 128, we did not find any de novo variants.
Table 2.
WES-detected SNVs identified in three families with ACDMPV patients negative for FOXF1 mutations and CNVs on chromosome 16q24.1.
| Gene | Protein | Phenotype | Variant | SIFT | Polyphen2 | MutationTaster | RadialSVM | Inheritance | Family | ||
|---|---|---|---|---|---|---|---|---|---|---|---|
| ZMYND11 | Transcriptional repressor | Mental retardation, autosomal dominant 30 (OMIM 616083) | g.10:298327_T>C | c.1564T>C | p.Trp522Arg | D | D | D | D | de novo | 114 |
| SLC50A1 | Sugar transporter | - | g.1:155110692_C>T | c.463C>T | p.Arg155Cys | D | B | D | T | de novo | 121 |
| ESRP1 | Epithelial RNA splicing regulator | - | g.8:95677280_A>G | c.881A>G | p.Tyr294Cys | D | D | D | T | de novo | 121 |
| MPRIP | Myosin phosphatase Rho-interacting protein | - | g.17:17039561_CCA GCAGCAG>C | c.533_542delinsC | p.Ser179_Ser173del | - | - | - | - | de novo | 121 |
| DOCK8 | Dedicator of cytokinesis | Hyper-IgE recurrent infection syndrome, autosomal recessive (OMIM 243700) | g.9:386371_C>CT | c.2819_2820insT | p.Gly941TrpfsTer943 | - | - | - | - | de novo | 121 |
| PLXNB2 | Semaphorin transmembrane receptor | - | g.22:50728383_G>C | c.631C>G | p.Leu211Val | T | B | D | T | paternal | 121 |
| g.22:50720372_C>T | c.3256G>A | p.Ala1086Thr | T | B | N | T | paternal | 128 | |||
D, deleterious; B, benign; T, tolerant; N, neutral
Moreover, in families 121 and 128, we identified inherited missense variants c.631C>G (p.Leu211Val) in pt 121.3 and c.3256G>A (p.Ala1086Thr in pt 128.3 in PLXNB2 encoding plexin B2 (Table 2). Further, we identified homozygous and compound heterozygous variants in all affected probands from 114, 121 and 128 families. In patient 114.3, we found 66 homozygous variants in 63 genes and 27 compound heterozygous in 10 genes, in patient 121.3, we identified 56 homozygous and 24 compound heterozygous variants in 49 and 7 genes, respectively, and in patient 128.3, we identified five homozygous variants in five genes and five compound heterozygous variants in two genes.
CNV analyses of WES data did not reveal any non-polymorphic deletion or duplication in probands 114.3 and 121.3 and no genomic imbalances were identified by whole-genome array CGH in pt 128.3. By analyzing B-allele frequency in WES data in probands 114.3, 121.3, and 128.3, we did not identify any AOH region larger than 5 Mb.
DISCUSSION
To date, approximately 150 imprinted genes clustering in 16 genomic loci have been described in mice (Barlow et al. 2014). In humans, disease related genomic imprinting has been well defined only for a few loci: 15q11.2 in Prader-Willi (PWS, OMIM 176270) and Angelman (OMIM 105830) syndromes, 11p15 in Beckwith-Wiedemann syndrome (BWS, OMIM 130650) and Silver-Russell syndrome (OMIM 180860), 14q32 in Kagami-Ogata syndrome (OMIM 608149), 20q13.32 in McCune-Albright syndrome (OMIM 174800), and 6q25.3 in transient neonatal diabetes mellitus 1 (OMIM 601410) (Bartolomei and Ferguson-Smith 2011). However, recent analyses have shown that the occurrence of non-canonical imprinting, with a biased allele-specific gene expression as opposed to complete allele silencing, is likely underestimated (Gregg 2014). These partial allelic imbalances may result, e.g., from incomplete methylation of imprinting control regions (ICRs) or from an ICR being epigenetically modified only in a subpopulation of cells (Gregg 2014).
We have accumulated the largest collection of ACDMPV samples worldwide (N=141 families), in which we have identified 86 pathogenic variants in the FOXF1 locus: 38 deletion CNVs, a complex rearrangement and 47 point mutations. In the vast majority of the remaining 55 families, DNA was not of sufficient quality for genetic testing. We have previously reported pathogenic genomic deletions involving FOXF1 or its upstream regulatory region in 17 patients with histopathologically-verified ACDMPV that arose de novo on the maternal chromosome 16. Based on these results, we proposed that the FOXF1 locus in chromosome 16q24.1 is imprinted in the human lungs (Stankiewicz et al. 2009; Sen et al. 2013a, b; Szafranski et al. 2013a, b; Dharmadhikari et al. 2015). We previously suggested that this imprinting is incomplete (~35% expression from one parental allele vs ~65% expression from the other allele) (Szafranski et al. 2013a). Together with 13 novel deletions reported here, 30 out of 31 CNV deletions involving FOXF1 or its upstream enhancer in patients with ACDMPV arose de novo on the maternal chr16, now providing statistically significant evidence for genomic imprinting at this locus (p<4E-06). However, we have now also identified an upstream deletion CNV (pt 122.3) and three non-deletion variants in FOXF1 (pts 124.3, 130.3, 138.3), pathogenic for ACDMPV, that arose on paternal chromosome 16q24.1, indicating complex genomic and epigenetic regulation of the FOXF1 locus.
The 4.1 kb de novo deletion within the upstream FOXF1 enhancer on paternal chromosome 16 in pt 122.3 removed the binding sites for a number of transcription factors, including MEF2 and LUN1 that exhibit increased expression in the lungs. MEF2 regulates cell proliferation as a target of several growth factor signaling pathways and has been shown to play an important role in myogenesis, including morphogenesis of visceral muscles (Brand 1997; Black and Olson 1998). We hypothesize that loss of MEF2 binding in patient 122.3 might have contributed to the abnormal development of lung vasculature, a feature typical for ACDMPV. LUN1, which is highly expressed in alveolar epithelium (Chu et al. 2001) has binding sites located also in regulatory region of genes for E-cadherin and talin, which regulate cell motility (Oyanagi et al. 2004). Gene expression profiling in ACDMPV lungs and Foxf1+/− mouse lungs showed that E-cadherin is one of the Foxf1 targets (Sen et al. 2014). Thus LUN1 might control cell motility during alveolar development, targeting E-cadherin expression directly and indirectly through FOXF1. The deleted interval in pt 122.3 also includes the TATA-box, present in 25% of eukaryotic promoters; however, we found no promoter activity within this region. Since the upstream regulatory region becomes juxtaposed with the FOXF1 promoter, we propose that the identified transcription factor binding sites, in particular those for MEF2, LUN1, and TBP (TFIID), similarly as the relatively closely located GLI2-binding sites (Szafranski et al. 2013a), may interact with the FOXF1 promoter following chromatin looping to directly up-regulate FOXF1 promoter activity.
In patient 124.3, we found a complex genomic rearrangement within the noncoding portion of FOXF1 exon 1, potentially interfering with initiation of transcription and translation. The most plausible explanation of the absence of ACDMPV phenotype in the father is that he could be a mosaic for this rearrangement, as shown for the fathers of pts 130.3 and 138.3.
The other two identified paternally transmitted pathogenic variants in families 130 and 138, mapping within the coding portions of FOXF1, were inherited from the reportedly healthy fathers who are mosaics for the mutations in the blood. These two cases exemplify incomplete penetrance of ACDMPV likely due to somatic mosaicism for a pathogenic variant manifesting as non-mosaic in their affected children. The clinical relevance of somatic mosaicism has become more evident only recently (Campbell et al. 2014). Family 138 also illustrates variable expressivity of ACDMPV with two siblings presenting with severe pulmonary hypertension after birth, one of whom had hypoxemia, but survived beyond infancy, and the other had partial anomalous pulmonary venous return. The third sibling died in the neonatal period from ACDMPV (Reiter et al. 2016).
Given that all but one ACDMPV variants that arose on paternal chromosome 16 mapped within the FOXF1 gene, whereas all but one deletions that included the upstream enhancer arose on the maternal chromosome, we propose that the FOXF1 locus is imprinted through epigenetic modification of its distant lung-specific enhancer. In support of this notion, we have found that whereas the FOXF1 promoter is not methylated, the CpG island overlapping cluster of GLI-binding sites within the upstream enhancer is differentially methylated, and this methylation reduces regulatory function of the enhancer (Szafranski et al. 2013a). Moreover, the promoter region of the lncRNA gene, LINC01081, that positively regulates FOXF1 expression, located within the enhancer, overlaps with another CpG island, suggesting possibility of the regulation of the expression of LINC01081 by allele-specific differential methylation of its promoter. Most recently, Dello Russo et al. (2015) reported a de novo ~ 2.6 Mb deletion (chr16:83,676,990-86,292,585) at maternal chromosome 16q23.3q24.1, encompassing LINC01082 and disrupting LINC01081, in a patient with a rare developmental lung disease pulmonary capillary hemangiomatosis, providing further evidence for genomic imprinting and demonstrating allelic affinity of this genomic locus.
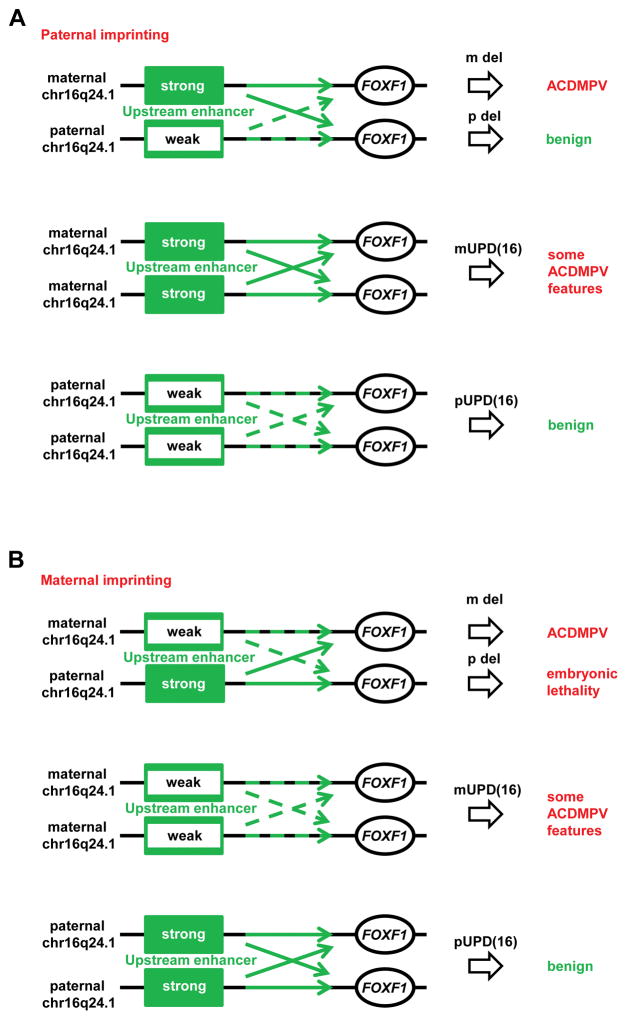
Whether epigenetic modification of the upstream enhancer occurs on paternal or on maternal chromosome 16 is currently unclear and requires further studies. Unlike ICRs of maternally imprinted genes that are typically located at the imprinted gene promoter, the intergenic localization of the FOXF1 locus ICR suggests paternal imprinting (Ferguson-Smith 2011). Also the location of all but one pathogenic deletion on maternal chromosome suggests paternal imprinting. In the paternal imprinting model (Fig. 5A), deletion of the strong enhancer on maternal chromosome 16 leads to ACDMPV, whereas deletion of the weak enhancer on paternal chromosome 16 is benign. In the maternal imprinting model (Fig. 5B), deletion of the weak enhancer on maternal chromosome 16 slightly decreases FOXF1 expression, resulting in ACDMPV whereas deletion of the strong enhancer on paternal chromosome 16 reduces expression of FOXF1 more dramatically and is embryonic lethal.
Fig. 5.
Proposed model of ACDMPV and UPD(16) etiologies due to (a) paternal or (b) maternal imprinting of the FOXF1 upstream enhancer on chromosome 16q24.1. Epigenetic modification of the enhancer reduces its ability to stimulate FOXF1 transcription. In paternal imprinting model (a), the majority of FOXF1 transcription depends on the strong enhancer located on the maternal chromosome 16. Thus deletion of the enhancer on this chromosome would significantly reduce FOXF1 expression and cause ACDMPV whereas the deletion on the paternal chromosome 16q24.1 would reduce FOXF1 expression less with no clinical consequences. Consequently, maternal UPD(16) would increase FOXF1 expression level (pathogenic) whereas paternal UPD(16) would slightly decrease FOXF1 expression level (benign). In the maternal imprinting model (b), the upstream deletion of the weak enhancer on the maternal chromosome 16 would reduce FOXF1 expression, resulting in ACDMPV. The deletion of the strong enhancer on the paternal chromosome would reduce FOXF1 expression would be embryonic lethal. According to this model, in maternal UPD(16), the level of FOXF1 would be insufficient to prevent development of some ACDMPV features and other anomalies typical for maternal UPD(16). In contrast, point mutations in FOXF1 are found on both parental alleles, suggesting in-trans function of the FOXF1 enhancer, likely using lncRNAs (Szafranski et al. 2013a).
Interestingly, multiple congenital malformations, including pulmonary hypoplasia, heart defects, tracheoesophageal fistula, gut malrotation, absent gall bladder, renal agenesis, hydronephrosis, imperforate anus, and single umbilical artery (SUA), seen in the vast majority of children with ACDMPV, are also observed in patients with maternal uniparental disomy 16, UPD(16). In stark contrast, a relatively normal phenotype was reported in few patients with paternal UPD(16) (Kohlhase et al. 2000; Hamvas et al. 2009), and the presence of imprinted gene(s) on chromosome 16 was suggested as causative for maternal UPD(16) phenotype (Yong et al. 2002). Differences in the clinical features observed in maternal UPD(16) cases compared to paternal UPD(16) cases and similarities between ACDMPV and maternal UPD(16) phenotypes, indicate that the identified genomic imprinting at the FOXF1 locus may be responsible for some phenotypic features of maternal UPD(16) (Dharmadhikari et al. 2015). The underlying mechanism could be similar to that in patients with maternal (but not paternal) duplication/triplication of the imprinted PWS/AS region in 15q11.2, e.g., due to inv dup(15). In the paternal imprinting model (Fig. 5A), in maternal UPD(16), FOXF1 expression is increased, manifesting typical features of UPD(16) including organs involved also in patients with ACDMPV, whereas in paternal UPD(16), FOXF1 expression only slightly decreases and is benign. In the maternal imprinting model (Fig. 5B), the level of FOXF1 in maternal UPD(16) is reduced, whereas paternal UPD(16) increases FOXF1 expression and is benign. However, given that there are only two reports of apparently benign paternal UPD16 (isodisomy) cases vs. high prevalence of maternal UPD16 (heterodisomy) cases due to common trisomy 16 (>1% of all pregnancies), it is also possible that paternal UPD(16) is early embryonically lethal.
The observed enhancer-dependent regulation and proposed genomic imprinting in the FOXF1 locus are likely mediated by genomic insulator sites binding CTCF as was shown for the BWS region on chromosome 11p15. Supporting this model, in silico Hi-C analyses of the chromosome 16q24.1 genomic structure showed that this region is organized into ~ 400 kb TADs with FOXF1 being located at the TAD boundary (Fig. 3). TAD boundaries exhibit conservation across species and remain largely constant across multiple cell types (Dixon et al. 2012), suggesting that variation in intra-domain interactions, such as chromatin looping, may be crucial for dynamic regulation of gene expression in a cell type-specific fashion. Using a chromosome conformation capture-on-chip (4C) analysis, we have previously shown that the region upstream of FOXF1, including its promoter, comes in contact with the upstream enhancer sequences in a time and tissue specific manner (Szafranski et al. 2013a); these interactions are stronger or more frequent in fetal lung fibroblasts than in cells of tissues other than lungs (Fig. 3).
Recently, disruption of TADs, resulting in “enhancer adoption”, has been shown as a novel disease-causing mechanism in patients with limb anomalies (Lupiáñez et al. 2015). We suggest that deletion CNVs or balanced paracentric inversions (Parris et al. 2013) removing or replacing, respectively, the FOXF1 TAD boundary with CTCF binding sites (Guo et al. 2015), would expose genes neighboring TAD to a non-physiological environment deregulating their expression. This mechanism could explain our observation that in contrast to FOXF1 point mutations (Sen et al. 2013b) and upstream deletion CNVs (Stankiewicz et al. 2009; Szafranski et al. 2013a; Szafranski et al. 2014), genomic deletions of FOXF1 at its TAD boundary, and the flanking genes were associated with severe congenital heart defects, including hypoplastic left heart syndrome (HLHS) and SUA (Table 1 and Supplemental Table S1). Co-existence of HLHS and SUA has been well documented (Tasha et al. 2014; Araujo et al. 2015). We have previously suggested that HLHS may result from variants in the neighboring FOXC2 and FOXL1 genes; however, screening for mutations in patients with HLHS revealed no pathogenic variants in those genes (Iascone et al. 2012). Alternatively, disruption of lncRNA FENDRR that maps 1.7 kb upstream of FOXF1 in the opposite orientation, and likely utilizes the same bi-directional promoter as FOXF1 could lead to HLHS and SUA. Corroboratively, Grote et al. (2013) reported that homozygous loss of Fendrr in mice led to hypoplasia of the myocardium affecting ventricular walls and the interventricular septum and ventral body wall (omphalocele), likely due to in trans deregulation of the cardiac master transcriptional regulators Gata6 and Nkx2-5. Further, Sauvageau et al. (2013) and Lai et al. (2015) independently demonstrated defects in lungs and heart in the Fendrr−/− mouse neonates.
Interestingly, most of deletion CNVs in 16q24.1 were flanked by retrotransposons with greater than 50% being Alu-mediated and many representing different Alu families (Szafranski et al. 2013a). Recently, Alu-mediated genomic rearrangements were shown to be products of replication and not recombination errors (Gu et al. 2015). Of note, Jacques et al. (2015) demonstrated that transposable elements have contributed hundreds of thousands of novel regulatory elements to the primate lineage and reshaped the human transcriptional landscape. In vertebrates, transposable elements occur in more than two-thirds of mature lncRNAs, whereas they seldom occur in protein-coding transcripts. Moreover, transposable elements were found in biased positions and orientations within lncRNAs, particularly at their transcription start sites, which suggests a role in the regulation of lncRNA transcription (Fatica and Bozzoni 2014). We suggest that the high rate of the retrotransposon-mediated CNVs in 16q24.1 may result from replication-transcription collisions due to their residual transcriptional activity.
Besides variants in the FOXF1 locus, CNVs or SNVs in other genes involved in SHH or other signaling pathways essential for lung development might be also causative for ACDMPV. Our WES analyses in three unrelated ACDMPV families (114, 121, and 128) revealed de novo variants in five genes: DOCK8, ESRP1, MPRIP, SLC50A1, and ZMYND11. All these genes are involved in cell signaling or transcription regulation in general and their variants may contribute to development of ACDMPV. ESRP1 (pt 121.3) is particularly interesting in this context. It encodes endothelial splicing regulatory protein 1 (ESRP1) functioning as an epithelium-specific regulator of FGFR2 splicing into FGFR2-IIIb isoform] (Warzecha et al. 2009). Various isoforms of FGFR2 are involved in epithelial-mesenchymal crosstalk during embryonic development, and they also play a role in epithelial-mesenchyme transitions during lung and heart development. Thus, loss of ESRP1 or its function might contribute to ACDMPV by affecting FGF signaling.
In families 121 and 128, we identified two inherited missense variants in PLXNB2 encoding plexin B2. Plexins function as receptors of semaphorins and were shown to play a crucial role in lung branching morphogenesis (Kagoshima et al. 2001). Interestingly, loss of class 3 semaphorins (SEMA3) was attributed to dysmorphic vascularization during mouse lung development, resembling features of ACDMPV (Joza et al. 2012). Since both variants were inherited from healthy carrier father, they may function as modifiers of the pathway(s) contributing to ACDMPV. Nevertheless, other variants in PLXNB2 might still be causative for ACDMPV.
In aggregate, our data highlight complexity of genomic architecture of the FOXF1 locus at chromosome 16q24.1 and regulation of FOXF1 expression through epigenetic modification of its upstream enhancer. Unlike the 31 identified CNVs that all arose de novo and, with one exception, on maternally inherited chromosome 16, FOXF1 SNVs can be inherited from either parent, who may be a mosaic carrier. We propose that genomic imprinting of the FOXF1 locus is due to parent- and tissue-specific activity of the FOXF1 enhancer regulated by lncRNAs LINC01081 and LINC01082 and chromatin folding within a defined TAD, with FOXF1 being located at its boundary. The FOXF1 promoter is presumably activated by the enhancer-bound transcription factors (e.g., GLI2, MEF2, LUN1, and TFIID). This complex gene regulation in 16q24.1, in particular a non-canonical mode of FOXF1 locus imprinting, likely contributes to variable expressivity and incomplete penetrance of ACDMPV. We also suggest that variants in two other genes could be causative (ESRP1) or function as modifiers (PLXNB2) of the ACDMPV phenotype.
Supplementary Material
Acknowledgments
We thank Drs. K. Aagaard, A.L. Beaudet, J.W. Belmont, A.K. Groves, B. Lee, J.R. Neilson, S.E. Plon, I.B. van den Veyver, and H.Y. Zoghbi for helpful discussion and J.A. Rosenfeld-Mokry for critically reading the manuscript. This work was supported by grants awarded by the US National Heart, Lung, and Blood Institute (NHLBI) grant RO1HL101975 to PSt, NORD grants to PSz, US National Human Genome Research Institute (NHGRI)/NHLBI grant HG006542 to the Baylor-Hopkins Center for Mendelian Genomics, and National Institute of Neurological Disorders and Stroke (NINDS) grant NS058529 to JRL.
Footnotes
Conflict of interest No competing interest is declared.
Contributor Information
Przemyslaw Szafranski, Department of Molecular and Human Genetics, Baylor College of Medicine, Houston, TX, USA.
Tomasz Gambin, Department of Molecular and Human Genetics, Baylor College of Medicine, Houston, TX, USA.
Avinash V. Dharmadhikari, Department of Molecular and Human Genetics, Baylor College of Medicine, Houston, TX, USA. Interdepartmental Program in Translational Biology and Molecular Medicine, Baylor College of Medicine, Houston, TX, USA
Kadir Caner Akdemir, Genomic Medicine Department, MD Anderson Cancer Center, Houston, TX, USA.
Shalini N. Jhangiani, Department of Molecular and Human Genetics, Baylor College of Medicine, Houston, TX, USA. Human Genome Sequencing Center, Baylor College of Medicine, Houston, TX, USA
Jennifer Schuette, Division of Critical Care Medicine, Children’s National Health System, Washington, DC, USA.
Nihal Godiwala, Division of Critical Care Medicine, Children’s National Health System, Washington, DC, USA.
Svetlana A. Yatsenko, Department of Obstetrics, Gynecology, and Reproductive Sciences, Center for Medical Genetics and Genomics, Magee-Womens Hospital of UPMC, Pittsburgh, PA, USA. Department of Pathology, University of Pittsburgh School of Medicine, Pittsburgh, PA, USA
Jessica Sebastian, Department of Medical Genetics, Children’s Hospital of Pittsburgh of UPMC, Pittsburgh, PA, USA.
Suneeta Madan-Khetarpal, Department of Medical Genetics, Children’s Hospital of Pittsburgh of UPMC, Pittsburgh, PA, USA.
Urvashi Surti, Department of Obstetrics, Gynecology, and Reproductive Sciences, Center for Medical Genetics and Genomics, Magee-Womens Hospital of UPMC, Pittsburgh, PA, USA. Department of Pathology, University of Pittsburgh School of Medicine, Pittsburgh, PA, USA. Department of Human Genetics, Graduate School of Public Health, University of Pittsburgh, PA, USA.
Rosanna G. Abellar, Department of Pathology, Columbia University Medical Center, New York, NY, USA
David A. Bateman, Department of Pediatrics, Columbia University Medical Center, New York, NY, USA
Ashley L. Wilson, Children’s Hospital of New York-Presbyterian, New York, NY, USA
Melinda H. Markham, Division of Neonatology, Division of Maternal Fetal Medicine, Vanderbilt University Medical Center, Nashville, TN, USA
Jill Slamon, Department of Obstetrics and Gynecology, Division of Maternal Fetal Medicine, Vanderbilt University Medical Center, Nashville, TN, USA.
Fernando Santos-Simarro, INGEMM, Instituto de Genética Médica y Molecular, IdiPAZ, Madrid, Spain. CIBERER, ISCIII, Madrid, Spain.
María Palomares, INGEMM, Instituto de Genética Médica y Molecular, IdiPAZ, Madrid, Spain. CIBERER, ISCIII, Madrid, Spain.
Julián Nevado, INGEMM, Instituto de Genética Médica y Molecular, IdiPAZ, Madrid, Spain. CIBERER, ISCIII, Madrid, Spain.
Pablo Lapunzina, INGEMM, Instituto de Genética Médica y Molecular, IdiPAZ, Madrid, Spain. CIBERER, ISCIII, Madrid, Spain.
Brian Chung Hon-Yin, Department of Paediatrics and Adolescent Medicine, The University of Hong Kong, Hong Kong, China. Department of Obstetrics and Gynaecology, and Centre for Genomic Sciences, The University of Hong Kong, Hong Kong, China.
Wong Wai-Lap, Department of Paediatrics and Adolescent Medicine, The University of Hong Kong, Hong Kong, China.
Yoyo Wing Yiu Chu, Department of Paediatrics and Adolescent Medicine, The University of Hong Kong, Hong Kong, China.
Gary Tsz Kin Mok, Department of Paediatrics and Adolescent Medicine, The University of Hong Kong, Hong Kong, China.
Kerem Eitan, Pediatric Pulmonary Unit, Department of Pediatrics, Hadassah-Hebrew University Medical Center, Jerusalem, Israel.
Joel Reiter, Pediatric Pulmonary Unit, Department of Pediatrics, Hadassah-Hebrew University Medical Center, Jerusalem, Israel.
Namasivayam Ambalavanan, Departments of Pediatrics, University of Alabama at Birmingham, Alabama, USA. Cell Developmental and Integrative Biology, University of Alabama at Birmingham, Birmingham, AL, USA.
Scott A. Anderson, Department of Surgery, Division of Pediatric Surgery, University of Alabama at Birmingham and Children’s of Alabama, Birmingham, AL, USA
David R. Kelly, Department of Pathology, University of Alabama at Birmingham and Pathology and Laboratory Medicine Service, Children’s of Alabama, Birmingham, AL, USA
Joseph Shieh, Division of Medical Genetics, Department of Pediatrics, and Institute for Human Genetics, University of California San Francisco, San Francisco, CA, USA.
Taryn C. Rosenthal, Genetics Department, Kaiser Permanente San Jose Medical Center, San Jose, CA, USA
Kristin Scheible, Department of Pediatrics, University of Rochester, Rochester, NY, USA.
Laurie Steiner, Division of Neonatology, University of Rochester, Rochester, NY, USA.
M. Anwar Iqbal, Pathology and Laboratory Medicine, Rochester, Rochester, NY, USA.
Margaret McKinnon, Department of Medical Genetics, University of British Columbia, Vancouver, Canada.
Sara Jane Hamilton, Department of Medical Genetics, University of British Columbia, Vancouver, Canada.
Kamilla Schlade-Bartusiak, Department of Medical Genetics, University of British Columbia, Vancouver, Canada.
Dawn English, Department of Medical Genetics, University of British Columbia, Vancouver, Canada.
Glenda Hendson, Department of Pathology, University of British Columbia, Vancouver, Canada.
Elizabeth R. Roeder, Department of Pediatrics, Baylor College of Medicine, San Antonio, TX, USA. Department of Molecular and Human Genetics, Baylor College of Medicine, San Antonio, TX, USA
Thomas S. DeNapoli, Department of Pathology, Children’s Hospital of San Antonio, San Antonio, TX, USA
Rebecca Okashah Littlejohn, Department of Pediatrics, Baylor College of Medicine, San Antonio, TX, USA.
Daynna J. Wolff, Department of Pathology and Laboratory Medicine, Medical University of South Carolina, Charleston, SC, USA
Carol L. Wagner, Department of Pediatrics, Medical University of South Carolina, Charleston, SC, USA
Alison Yeung, Victorian Clinical Genetics Services, Murdoch Childrens Research Institute, Parkville, SA, Australia.
David Francis, Victorian Clinical Genetics Services, Murdoch Childrens Research Institute, Parkville, SA, Australia.
Elizabeth K. Fiorino, Division of Pediatric Pulmonary Medicine, The Children’s Heart Center Steven and Alexandra Cohen Children’s Medical Center of New York, New York, NY, USA
Morris Edelman, Division of Pediatric Pathology, The Children’s Heart Center Steven and Alexandra Cohen Children’s Medical Center of New York, New York, NY, USA.
Joyce Fox, Division of Medical Genetics, The Children’s Heart Center Steven and Alexandra Cohen Children’s Medical Center of New York, New York, NY, USA.
Denise A. Hayes, Pediatric Cardiology, The Children’s Heart Center Steven and Alexandra Cohen Children’s Medical Center of New York, New York, NY, USA
Sandra Janssens, Centre for Medical Genetics Ghent, University Hospital Ghent, Ghent, Belgium.
Elfride De Baere, Centre for Medical Genetics Ghent, University Hospital Ghent, Ghent, Belgium.
Bjorn Menten, Centre for Medical Genetics Ghent, University Hospital Ghent, Ghent, Belgium.
Anne Loccufier, Department of Obstetrics, Gynaecology, and Fertility, AZ St Jan Brugge, Brugge, Begium.
Lieve Van Walleghem, Department of Anatomopathology, AZ St Jan Brugge, Brugge, Begium.
Philippe Moerman, Department of Pathology UZ Leuven, Leuven, Belgium.
Yves Sznajer, Center for Human Genetics, Cliniques Universitaires St-Luc, Universite Catholique de Louvain, Brussels, Belgium.
Amy S. Lay, Division of Pediatric Cardiology, Children’s Mercy Hospital, Kansas City, MS, USA
Jennifer L. Kussmann, Division of Clinical Genetics, Children’s Mercy Hospital, Kansas City, MS, USA
Jasneek Chawla, Division of Paediatric Respiratory & Sleep Medicine, Lady Cilento Children’s Hospital, Children’s Health Queensland Hospital and Health Service, Brisbane, QLD, Australia. The University of Queensland, Brisbane, QLD, Australia.
Diane J. Payton, Division of Anatomical Pathology, Lady Cilento Children’s Hospital, Children’s Health Queensland Hospital and Health Service, Brisbane, QLD, Australia. Pathology Queensland, Brisbane, QLD, Australia
Gael E. Phillips, Division of Anatomical Pathology, Lady Cilento Children’s Hospital, Children’s Health Queensland Hospital and Health Service, Brisbane, QLD, Australia. Pathology Queensland, Brisbane, QLD, Australia
Erwin Brosens, Clinical Genetics Department, Erasmus MC-Sophia, Rotterdam, Netherlands. Paediatric Surgery, Erasmus MC-Sophia, Rotterdam, Netherlands.
Dick Tibboel, Paediatric Surgery, Erasmus MC-Sophia, Rotterdam, Netherlands.
Annelies de Klein, Clinical Genetics Department, Erasmus MC-Sophia, Rotterdam, Netherlands.
Isabelle Maystadt, Institut de Pathologie et de Genetique, Gosselies, Belgium.
Richard Fisher, James Cook University Hospital, Middlesborough, UK.
Neil Sebire, Department of Paediatric Histopathology, Great Ormond Street Hospital for Children and UCL Institute of Child Health, London, UK.
Alison Male, Clinical Genetics Unit, Great Ormond Street Hospital for Children and UCL Institute of Child Health, London, UK.
Maya Chopra, Department of Molecular and Clinical Genetics, Royal Prince Alfred Hospital, Sydney, NSW, Australia.
Jason Pinner, Obstetrics, Gynaecology and Neonatology, Royal Prince Alfred Hospital, Westmead, NSW, Australia.
Girvan Malcolm, Obstetrics, Gynaecology and Neonatology, Royal Prince Alfred Hospital, Westmead, NSW, Australia.
Gregory Peters, Cytogenetics Department, The Children’s Hospital at Westmead, Westmead, NSW, Australia.
Susan Arbuckle, Histopathology Department, The Children’s Hospital at Westmead, Westmead, NSW, Australia.
Melissa Lees, Clinical Genetics Unit, Great Ormond Street Hospital for Children NHS Trust, London, UK.
Zoe Mead, Department of Histopathology, Addenbrooke’s NHS Trust Pathology Department, Addenbrooke’s Hospital, Cambridge, UK.
Oliver Quarrell, Dept of Clinical Genetics, Sheffield Children’s Hospital, Sheffield, UK.
Richard Sayers, Dept of Clinical Genetics, Sheffield Children’s Hospital, Sheffield, UK.
Martina Owens, Molecular Genetics Department, Royal Devon and Exeter NHS Foundation Trust, Exeter, UK.
Charles Shaw-Smith, Molecular Genetics Department, Royal Devon and Exeter NHS Foundation Trust, Exeter, UK.
Janet Lioy, Division of Neonatology, The Children’s Hospital of Philadelphia, The University of Pennsylvania, Perelman School of Medicine, Philadelphia, PA, USA.
Eileen McKay, Department of Pathology, The Children’s Hospital of Philadelphia, Philadelphia, PA, USA.
Nicole de Leeuw, Department of Human Genetics, Radboud University Medical Center, Nijmegen, the Netherlands.
Ilse Feenstra, Department of Human Genetics, Radboud University Medical Center, Nijmegen, the Netherlands.
Liesbeth Spruijt, Department of Human Genetics, Radboud University Medical Center, Nijmegen, the Netherlands.
Frances Elmslie, South West Thames Regional Genetics Service, St George’s University Hospital, London, UK.
Timothy Thiruchelvam, Critical Care and Cardiorespiratory Unit, Great Ormond Street Hospital NHS Trust, London, UK.
Carlos A. Bacino, Department of Molecular and Human Genetics, Baylor College of Medicine, Houston, TX, USA. Texas Children’s Hospital, Houston, TX, USA
Claire Langston, Department of Pathology and Immunology, Baylor College of Medicine, Houston, TX, USA.
James R. Lupski, Department of Molecular and Human Genetics, Baylor College of Medicine, Houston, TX, USA. Human Genome Sequencing Center, Baylor College of Medicine, Houston, TX, USA. Texas Children’s Hospital, Houston, TX, USA. Department of Pediatrics, Baylor College of Medicine, Houston, TX, USA
Partha Sen, Department of Pediatrics, Baylor College of Medicine, Houston, TX, USA.
Edwina Popek, Department of Pathology and Immunology, Baylor College of Medicine, Houston, TX, USA.
Paweł Stankiewicz, Department of Molecular and Human Genetics, Baylor College of Medicine, Houston, TX, USA. Interdepartmental Program in Translational Biology and Molecular Medicine, Baylor College of Medicine, Houston, TX, USA.
References
- Araujo E, Júnior, Palma-Dias R, Martins WP, Reidy K, da Silva Costa F. Congenital heart disease and adverse perinatal outcome in fetuses with confirmed isolated single functioning umbilical artery. J Obstet Gynaecol. 2015;35:85–87. doi: 10.3109/01443615.2014.935720. [DOI] [PubMed] [Google Scholar]
- Barlow DP, Bartolomei MS. Genomic imprinting in mammals. Cold Spring Harb Perspect Biol. 2014;6:a018382. doi: 10.1101/cshperspect.a018382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bartolomei MS, Ferguson-Smith AC. Mammalian genomic imprinting. Cold Spring Harb Perspect Biol. 2011;3:a002592. doi: 10.1101/cshperspect.a002592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bishop NB, Stankiewicz P, Steinhorn RH. Alveolar capillary dysplasia. Am J Respir Crit Care Med. 2011;184:172–179. doi: 10.1164/rccm.201010-1697CI. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Black BL, Olson EN. Transcriptional control of muscle development by myocyte enhancer factor-2 (MEF2) proteins. Annu Rev Cell Dev Biol. 1998;14:167–196. doi: 10.1146/annurev.cellbio.14.1.167. [DOI] [PubMed] [Google Scholar]
- Brand NJ. Myocyte enhancer factor 2 (MEF2) Int J Biochem Cell Biol. 1997;29:1467–1470. doi: 10.1016/s1357-2725(97)00084-8. [DOI] [PubMed] [Google Scholar]
- Campbell IM, Shaw CA, Stankiewicz P, Lupski JR. Somatic mosaicism: implications for disease and transmission genetics. Trends Genet. 2015;31(7):382–392. doi: 10.1016/j.tig.2015.03.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campbell IM, Yuan B, Robberecht C, Pfundt R, Szafranski P, McEntagart ME, Nagamani SC, Erez A, Bartnik M, Wiśniowiecka-Kowalnik B, Plunkett KS, Pursley AN, Kang SH, Bi W, Lalani SR, Bacino CA, Vast M, Marks K, Patton M, Olofsson P, Patel A, Veltman JA, Cheung SW, Shaw CA, Vissers LE, Vermeesch JR, Lupski JR, Stankiewicz P. Parental somatic mosaicism is underrecognized and influences recurrence risk of genomic disorders. Am J Hum Genet. 2014;95:173–182. doi: 10.1016/j.ajhg.2014.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chang VW, Ho Y. Structural characterization of the mouse Foxf1a gene. Gene. 2001;267:201–211. doi: 10.1016/s0378-1119(01)00400-0. [DOI] [PubMed] [Google Scholar]
- Chu D, Kakazu N, Gorrin-Rivas MJ, Lu HP, Kawata M, Abe T, Ueda K, Adachi Y. Cloning and characterization of LUN, a novel ring finger protein that is highly expressed in lung and specifically binds to a palindromic sequence. J Biol Chem. 2001;276:14004–14013. doi: 10.1074/jbc.M010262200. [DOI] [PubMed] [Google Scholar]
- Dello Russo P, Franzoni A, Baldan F, Puppin C, De Maglio G, Pittini C, Cattarossi L, Pizzolitto S, Damante G. A 16q deletion involving FOXF1 enhancer is associated to pulmonary capillary hemangiomatosis. BMC Med Genet. 2015;16:94. doi: 10.1186/s12881-015-0241-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dharmadhikari AV, Szafranski P, Kalinichenko VV, Stankiewicz P. Genomic and Epigenetic Complexity of the FOXF1 Locus in 16q24.1: Implications for Development and Disease. Curr Genomics. 2015;16:107–116. doi: 10.2174/1389202916666150122223252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dixon JR, Selvaraj S, Yue F, Kim A, Li Y, Shen Y, Hu M, Liu JS, Ren B. Topological domains in mammalian genomes identified by analysis of chromatin interactions. Nature. 2012;485:376–380. doi: 10.1038/nature11082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fatica A, Bozzoni I. Long non-coding RNAs: new players in cell differentiation and development. Nat Rev Genet. 2014;15:7–21. doi: 10.1038/nrg3606. [DOI] [PubMed] [Google Scholar]
- Ferguson-Smith AC. Genomic imprinting: the emergence of an epigenetic paradigm. Nat Rev Genet. 2011;12:565–575. doi: 10.1038/nrg3032. [DOI] [PubMed] [Google Scholar]
- Galambos C, Sims-Lucas S, Ali N, Gien J, Dishop MK, Abman SH. Intrapulmonary vascular shunt pathways in alveolar capillary dysplasia with misalignment of pulmonary veins. Thorax. 2015;70:84–85. doi: 10.1136/thoraxjnl-2014-205851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garabedian MJ, Wallerstein D, Medina N, Byrne J, Wallerstein RJ. Prenatal diagnosis of cystic hygroma related to a deletion of 16q24.1 with haploinsufficiency of FOXF1 and FOXC2 genes. Case Rep Genet. 2012;2012:490408. doi: 10.1155/2012/490408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gregg C. Known unknowns for allele-specific expression and genomic imprinting effects. F1000Prime Rep. 2014;6:75. doi: 10.12703/P6-75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grote P, Wittler L, Hendrix D, Koch F, Währisch S, Beisaw A, Macura K, Bläss G, Kellis M, Werber M, Herrmann BG. The tissue-specific lncRNA Fendrr is an essential regulator of heart and body wall development in the mouse. Dev Cell. 2013;24:206–214. doi: 10.1016/j.devcel.2012.12.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gu S, Yuan B, Campbell IM, Beck CR, Carvalho CM, Nagamani SC, Erez A, Patel A, Bacino CA, Shaw CA, Stankiewicz P, Cheung SW, Bi W, Lupski JR. Alu-mediated diverse and complex pathogenic copy-number variants within human chromosome 17 at p13.3. Hum Mol Genet. 2015;24:4061–4077. doi: 10.1093/hmg/ddv146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guo Y, Xu Q, Canzio D, Shou J, Li J, Gorkin DU, Jung I, Wu H, Zhai Y, Tang Y, Lu Y, Wu Y, Jia Z, Li W, Zhang MQ, Ren B, Krainer AR, Maniatis T, Wu Q. CRISPR Inversion of CTCF Sites Alters Genome Topology and Enhancer/Promoter Function. Cell. 2015;162:900–910. doi: 10.1016/j.cell.2015.07.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamvas A, Nogee LM, Wegner DJ, Depass K, Christodoulou J, Bennetts B, McQuade LR, Gray PH, Deterding RR, Carroll TR, Kammesheidt A, Kasch LM, Kulkarni S, Cole FS. Inherited surfactant deficiency caused by uniparental disomy of rare mutations in the surfactant protein-B and ATP binding cassette, subfamily a, member 3 genes. J Pediatr. 2009;155:854–859. doi: 10.1016/j.jpeds.2009.06.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Handrigan GR, Chitayat D, Lionel AC, Pinsk M, Vaags AK, Marshall CR, Dyack S, Escobar LF, Fernandez BA, Stegman JC, Rosenfeld JA, Shaffer LG, Goodenberger M, Hodge JC, Cain JE, Babul-Hirji R, Stavropoulos DJ, Yiu V, Scherer SW, Rosenblum ND. Deletions in 16q24.2 are associated with autism spectrum disorder, intellectual disability and congenital renal malformation. J Med Genet. 2013;50:163–173. doi: 10.1136/jmedgenet-2012-101288. [DOI] [PubMed] [Google Scholar]
- Hastings PJ, Lupski JR, Rosenberg SM, Ira G. Mechanisms of change in gene copy number. Nat Rev Genet. 2009;10:551–564. doi: 10.1038/nrg2593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iascone M, Ciccone R, Galletti L, Marchetti D, Seddio F, Lincesso AR, Pezzoli L, Vetro A, Barachetti D, Boni L, Federici D, Soto AM, Comas JV, Ferrazzi P, Zuffardi O. Identification of de novo mutations and rare variants in hypoplastic left heart syndrome. Clin Genet. 2012;81:542–554. doi: 10.1111/j.1399-0004.2011.01674.x. [DOI] [PubMed] [Google Scholar]
- Jacques PÉ, Jeyakani J, Bourque G. The majority of primate-specific regulatory sequences are derived from transposable elements. PLoS Genet. 2015;9:e1003504. doi: 10.1371/journal.pgen.1003504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joza S, Wang J, Fox E, Hillman V, Ackerley C, Post M. Loss of semaphorin-neuropilin-1 signaling causes dysmorphic vascularization reminiscent of alveolar capillary dysplasia. Am J Pathol. 2012;181:2003–2017. doi: 10.1016/j.ajpath.2012.08.037. [DOI] [PubMed] [Google Scholar]
- Kagoshima M, Ito T, Kitamura H, Goshima Y. Diverse gene expression and function of semaphorins in developing lung: positive and negative regulatory roles of semaphorins in lung branching morphogenesis. Genes to Cells. 2001;6:559–571. doi: 10.1046/j.1365-2443.2001.00441.x. [DOI] [PubMed] [Google Scholar]
- Kalinichenko VV, Lim L, Shin B, Costa RH. Differential expression of forkhead box transcription factors following butylated hydroxytoluene lung injury. Am J Physiol Lung Cell Mol Physiol. 2001;280:L695–L704. doi: 10.1152/ajplung.2001.280.4.L695. [DOI] [PubMed] [Google Scholar]
- Kim IM, Zhou Y, Ramakrishna S, Hughes DE, Solway J, Costa RH, Kalinichenko VV. Functional characterization of evolutionarily conserved DNA regions in Forkhead box f1 gene locus. J Biol Chem. 2005;280:37908–37916. doi: 10.1074/jbc.M506531200. [DOI] [PubMed] [Google Scholar]
- Kohlhase J, Janssen B, Weidenauer K, Harms K, Bartels I. First confirmed case with paternal uniparental disomy of chromosome 16. Am J Med Genet. 2000;91:190–191. doi: 10.1002/(sici)1096-8628(20000320)91:3<190::aid-ajmg6>3.0.co;2-i. [DOI] [PubMed] [Google Scholar]
- Lai KM, Gong G, Atanasio A, Rojas J, Quispe J, Posca J, White D, Huang M, Fedorova D, Grant C, Miloscio L, Droguett G1, Poueymirou WT, Auerbach W, Yancopoulos GD, Frendewey D, Rinn J, Valenzuela DM. Diverse Phenotypes and specific transcription patterns in twenty mouse lines with ablated lincRNAs. PLoS One. 2015;10:e0125522. doi: 10.1371/journal.pone.0125522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Langston C. Misalignment of pulmonary veins and alveolar capillary dysplasia. Pediatr Pathol. 1991;11:163–70. doi: 10.3109/15513819109064753. [DOI] [PubMed] [Google Scholar]
- Luedi PP, Dietrich FS, Weidman JR, Bosko JM, Jirtle RL, Hartemink AJ. Computational and experimental identification of novel human imprinted genes. Genome Res. 2007;17:1723–1730. doi: 10.1101/gr.6584707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lupiáñez DG, Kraft K, Heinrich V, Krawitz P, Brancati F, Klopocki E, Horn D, Kayserili H, Opitz JM, Laxova R, Santos-Simarro F, Gilbert-Dussardier B, Wittler L, Borschiwer M1, Haas SA, Osterwalder M, Franke M, Timmermann B, Hecht J, Spielmann M, Visel A, Mundlos S. Disruptions of topological chromatin domains cause pathogenic rewiring of gene-enhancer interactions. Cell. 2015;161:1012–1025. doi: 10.1016/j.cell.2015.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mahlapuu M, Enerback S, Carlsson P. Haploinsufficiency of the forkhead gene Foxf1, a target for sonic hedgehog signalling, causes lung and foregut malformations. Development. 2001;128:2397–2406. doi: 10.1242/dev.128.12.2397. [DOI] [PubMed] [Google Scholar]
- Oyanagi H, Takenaka K, Ishikawa S, Kawano Y, Adachi Y, Ueda K, Wada H, Tanaka F. Expression of LUN gene that encodes a novel RING finger protein is correlated with development and progression of non-small cell lung cancer. Lung Cancer. 2004;46:21–28. doi: 10.1016/j.lungcan.2004.03.009. [DOI] [PubMed] [Google Scholar]
- Parris T, Nik AM, Kotecha S, Langston C, Helou K, Platt C, Carlsson P. Inversion upstream of FOXF1 in a case of lethal alveolar capillary dysplasia with misalignment of pulmonary veins. Am J Med Genet A. 2013;161A:764–770. doi: 10.1002/ajmg.a.35832. [DOI] [PubMed] [Google Scholar]
- Prothro SL, Plosa E, Markham M, Szafranski P, Stankiewicz P, Killen SA. Prenatal Diagnosis of Alveolar Capillary Dysplasia with Misalignment of Pulmonary Veins. J Pediatr. 2016;170:317–8. doi: 10.1016/j.jpeds.2015.11.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reiter J, Szafranski P, Breuer O, Perles Z, Dagan T, Stankiewicz P, Karem E. Variable Phenotypic Presentation of a Novel FOXF1 Missense Mutation in a Single Family. Pediatr Pulmonol. 2016 doi: 10.1002/ppul.23425. in press. [DOI] [PubMed] [Google Scholar]
- Sauvageau M, Goff LA, Lodato S, Bonev B, Groff AF, Gerhardinger C, Sanchez-Gomez DB, Hacisuleyman E, Li E, Spence M, Liapis SC, Mallard W, Morse M, Swerdel MR, D’Ecclessis MF, Moore JC, Lai V, Gong G, Yancopoulos GD, Frendewey D, Kellis M, Hart RP, Valenzuela DM, Arlotta P, Rinn JL. Multiple knockout mouse models reveal lincRNAs are required for life and brain development. Elife. 2013;2:e01749. doi: 10.7554/eLife.01749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sen P, Dharmadhikari AV, Majewski T, Mohammad MA, Kalin TV, Zabielska J, Ren X, Bray M, Brown HM, Welty S, Thevananther S, Langston C, Szafranski P, Justice MJ, Kalinichenko VV, Gambin A, Belmont J, Stankiewicz P. Comparative analyses of lung transcriptomes in patients with alveolar capillary dysplasia with misalignment of pulmonary veins and in foxf1 heterozygous knockout mice. PLoS One. 2014;9:e94390. doi: 10.1371/journal.pone.0094390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sen P, Gerychova R, Janku P, Jezova M, Valaskova I, Navarro C, Silva I, Langston C, Welty S, Belmont J, Stankiewicz P. A familial case of alveolar capillary dysplasia with misalignment of pulmonary veins supports paternal imprinting of FOXF1 in human. Eur J Hum Genet. 2013a;21:474–477. doi: 10.1038/ejhg.2012.171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sen P, Thakur N, Stockton DW, Langston C, Bejjani BA. Expanding the phenotype of alveolar capillary dysplasia (ACD) J Pediatr. 2004;145:646–651. doi: 10.1016/j.jpeds.2004.06.081. [DOI] [PubMed] [Google Scholar]
- Sen P, Yang Y, Navarro C, Silva I, Szafranski P, Kolodziejska KE, Dharmadhikari AV, Mostafa H, Kozakewich H, Kearney D, Cahill JB, Whitt M, Bilic M, Margraf L, Charles A, Goldblatt J, Gibson K, Lantz PE, Garvin AJ, Petty J, Kiblawi Z, Zuppan C, McConkie-Rosell A, McDonald MT, Peterson-Carmichael SL, Gaede JT, Shivanna B, Schady D, Friedlich PS, Hays SR, Palafoll IV, Siebers-Renelt U, Bohring A, Finn LS, Siebert JR, Galambos C, Nguyen L, Riley M, Chassaing N, Vigouroux A, Rocha G, Fernandes S, Brumbaugh J, Roberts K, Ho-Ming L, Lo IF, Lam S, Gerychova R, Jezova M, Valaskova I, Fellmann F, Afshar K, Giannoni E, Muhlethaler V, Liang J, Beckmann JS, Lioy J, Deshmukh H, Srinivasan L, Swarr DT, Sloman M, Shaw-Smith C, van Loon RL, Hagman C, Sznajer Y, Barrea C, Galant C, Detaille T, Wambach JA, Cole FS, Hamvas A, Prince LS, Diderich KE, Brooks AS, Verdijk RM, Ravindranathan H, Sugo E, Mowat D, Baker ML, Langston C, Welty S, Stankiewicz P. Novel FOXF1 mutations in sporadic and familial cases of alveolar capillary dysplasia with misaligned pulmonary veins imply a role for its DNA binding domain. Hum Mutat. 2013b;34:801–811. doi: 10.1002/humu.22313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stankiewicz P, Sen P, Bhatt SS, Storer M, Xia Z, Bejjani BA, Ou Z, Wiszniewska J, Driscoll DJ, Maisenbacher MK, Bolivar J, Bauer M, Zackai EH, McDonald-McGinn D, Nowaczyk MM, Murray M, Hustead V, Mascotti K, Schultz R, Hallam L, McRae D, Nicholson AG, Newbury R, Durham-O’Donnell J, Knight G, Kini U, Shaikh TH, Martin V, Tyreman M, Simonic I, Willatt L, Paterson J, Mehta S, Rajan D, Fitzgerald T, Gribble S, Prigmore E, Patel A, Shaffer LG, Carter NP, Cheung SW, Langston C, Shaw-Smith C. Genomic and genic deletions of the FOX gene cluster on 16q24.1 and inactivating mutations of FOXF1 cause alveolar capillary dysplasia and other malformations. Am J Hum Genet. 2009;84:780–791. doi: 10.1016/j.ajhg.2009.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Szafranski P, Dharmadhikari AV, Brosens E, Gurha P, Kolodziejska KE, Zhishuo O, Dittwald P, Majewski T, Mohan KN, Chen B, Person RE, Tibboel D, de Klein A, Pinner J, Chopra M, Malcolm G, Peters G, Arbuckle S, Guiang SF, 3rd, Hustead VA, Jessurun J, Hirsch R, Witte DP, Maystadt I, Sebire N, Fisher R, Langston C, Sen P, Stankiewicz P. Small noncoding differentially methylated copy-number variants, including lncRNA genes, cause a lethal lung developmental disorder. Genome Res. 2013a;23:23–33. doi: 10.1101/gr.141887.112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Szafranski P, Dharmadhikari AV, Wambach JA, Towe CT, White FV, Grady RM, Eghtesady P, Cole FS, Deutsch G, Sen P, Stankiewicz P. Two deletions overlapping a distant FOXF1 enhancer unravel the role of lncRNA LINC01081 in etiology of alveolar capillary dysplasia with misalignment of pulmonary veins. Am J Med Genet A. 2014;164A:2013–2019. doi: 10.1002/ajmg.a.36606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Szafranski P, Yang Y, Nelson MU, Bizzarro MJ, Morotti RA, Langston C, Stankiewicz P. Novel FOXF1 deep intronic deletion causes lethal lung developmental disorder, alveolar capillary dysplasia with misalignment of pulmonary veins. Hum Mutat. 2013b;34:1467–1471. doi: 10.1002/humu.22395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tasha I, Brook R, Frasure H, Lazebnik N. Prenatal detection of cardiac anomalies in fetuses with single umbilical artery: diagnostic accuracy comparison of maternal-fetal-medicine and pediatric cardiologist. J Pregnancy. 2014;2014:265421. doi: 10.1155/2014/265421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Warzecha CC, Sato TK, Nabet B, Hogenesch JB, Carstens RP. ESRP1 and ESRP2 are epithelial cell-type-specific regulators of FGFR2 splicing. Mol Cell. 2009;33:591–601. doi: 10.1016/j.molcel.2009.01.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yong PJ, Marion SA, Barrett IJ, Kalousek DK, Robinson WP. Evidence for imprinting on chromosome 16: the effect of uniparental disomy on the outcome of mosaic trisomy 16 pregnancies. Am J Med Genet. 2002;112:123–132. doi: 10.1002/ajmg.10702. [DOI] [PubMed] [Google Scholar]
- Yu S, Shao L, Kilbride H, Zwick DL. Haploinsufficiencies of FOXF1 and FOXC2 genes associated with lethal alveolar capillary dysplasia and congenital heart disease. Am J Med Genet A. 2010;152A:1257–1262. doi: 10.1002/ajmg.a.33378. [DOI] [PubMed] [Google Scholar]
- Zufferey F, Martinet D, Osterheld MC, Niel-Bütschi F, Giannoni E, Schmutz NB, Xia Z, Beckmann JS, Shaw-Smith C, Stankiewicz P, Langston C, Fellmann F. 16q24.1 microdeletion in a premature newborn: usefulness of array-based comparative genomic hybridization in persistent pulmonary hypertension of the newborn. Pediatr Crit Care Med. 2011;12:e427–432. doi: 10.1097/PCC.0b013e3182192c96. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.