Abstract
We report 4 cases of acute corneal edema with subsequent thinning and hyperopic shift following routine selective laser trabeculoplasty (SLT) for the treatment of primary open-angle glaucoma. Four women from 3 clinical sites developed acute corneal edema and haze within 2 days of uneventful SLT. In the following weeks to months, all treated corneas thinned to below pre-procedure thicknesses with resultant hyperopic shifts of nearly 2.0 diopters (D) to greater than 6.0 D. All eyes were moderately to highly myopic prior to SLT (spherical equivalent from −5.00 to −12.5 D). The corrected distance visual acuity 6 to 11 months after SLT was within 2 Snellen lines of the pre-procedure acuity in all patients; 2 patients required contact lenses. Corneal edema with subsequent corneal thinning and resultant hyperopic shift is an uncommon but possibly underrecognized complication of SLT, the etiology of which remains unknown but may be associated with moderate to high myopia.
Selective laser trabeculoplasty (SLT) is an increasingly common treatment modality for primary open-angle glaucoma (POAG) and is generally considered a safe and effective method for reducing intraocular pressure (IOP).1 Anterior chamber reaction, ocular discomfort, and an acute rise in IOP may occur but are typically transient and easily treated.2 Serious complications are rare.
In 2009, Moubayed et al.3 reported 2 cases of central corneal edema in women who presented 1 week after routine SLT. The corneal edema resolved in 2 to 4 months with topical steroid treatment. In at least 1 of the cases, residual subepithelial haze remained after the edema resolved. In 2011, Regina et al.4 reported 2 cases of central corneal edema in women, 1 of whom was highly myopic, presenting 1 to 2 days following routine SLT. The edema resolved after several weeks of topical steroid therapy, but central corneal haze and thinning remained, with a hyperopic shift in the myopic patient. In 2014, Song et al.5 reported a case of central corneal edema and haze in a highly myopic man who presented 1 day after routine SLT and resolved after several weeks of topical steroid treatment with residual corneal thinning. We describe an additional 4 cases of acute corneal edema with subsequent stromal thinning and hyperopic shift after routine SLT in moderately to highly myopic patients.
CASE REPORTS
Case 1
A 63-year-old white woman had SLT in her right eye to treat POAG. Eighty-nine pulses at 0.7 mJ per pulse were applied to the trabecular meshwork over 360 degrees. Before SLT, the IOP was 15 mm Hg; 30 minutes after SLT, it was 19 mm Hg. Before the procedure, the refraction was −14.0 +2.50 × 10, the corrected distance visual acuity (CDVA) 20/25, and the central corneal thickness (CCT) by ultrasound pachymetry 544 µm. The pre-SLT IOP-lowering topical medications, bimatoprost and brinzolamide, were continued. Two days after SLT, the patient presented with mild ocular discomfort, photophobia, and worsening blurred vision in the treated eye. The CDVA was 20/600 and the IOP 19 mm Hg. Diffuse corneal edema and haze affecting the central cornea more than the periphery were observed. No anterior chamber reaction was noted.
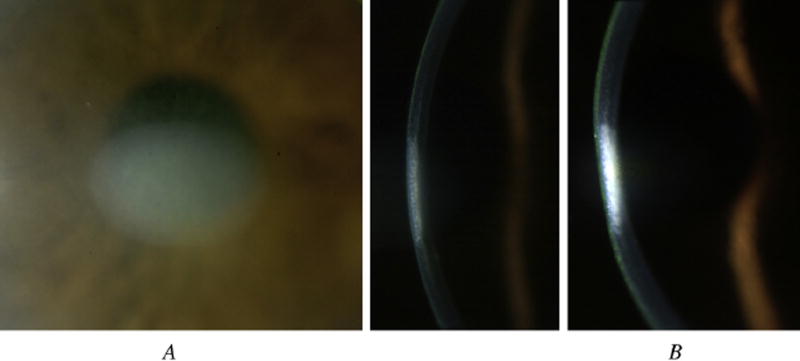
Topical prednisolone acetate was initiated. Five days after SLT, the CDVA was 20/80, the IOP was 21 mm Hg, and the corneal edema was significantly improved peripherally, but a well-demarcated area of central stromal edema and haze remained (Figure 1, A). Two weeks after SLT, the CDVA was 20/50, the IOP was 24 mm Hg, and the area of central stromal haze had thinned (Figure 1, B). At 1 month, the CDVA was 20/50, the refraction was −11.50 +1.25 × 4, the CCT was 432 µm, and the topical steroids were tapered. At 2 months, the CDVA was 20/50, the IOP was 14 mm Hg, and the central corneal haze had improved. At 8 months, the CDVA was 20/40 with a hard contact lens and mild central stromal haze remained.
Figure 1.
Slitlamp photographs of the cornea of patient 1 at 5 days (A) and 14 days (B) after SLT.
Tear fluid obtained 2 days after SLT was analyzed for herpes simplex virus (HSV) by polymerase chain reaction (PCR), enzyme-linked immunosorbent assay (ELISA), and culture, all of which returned negative. Specular microscopy (CellChek XL, Konan Medical) performed 2 months after SLT revealed a similar density (right eye 2670 cells/mm2, left eye 2555 cells/mm2), size, and shape of endothelial cells in the treated and untreated eyes. Corneal tomography (Pentacam, Oculus Optikgeräte GmbH) of the treated eye revealed an area of paracentral thinning inferiorly; the cornea of the fellow untreated eye was normal with no evidence of posterior elevation.
Case 2
A 56-year-old white woman had SLT in the right eye to treat POAG. One hundred ten spots at 1.0 mJ per spot were applied to the trabecular meshwork over 360 degrees. Before SLT, the IOP was 21 mm Hg; 30 minutes after SLT, it was 30 mm Hg (at which point brimonidine was administered and 30 minutes later the IOP was 24 mm Hg). Before the procedure, the refraction was −8.75 +1.00 × 47, the CDVA 20/20, and the CCT 606 µm. The pre-SLT IOP-lowering topical medications, latanoprost and timolol, were continued. One day after SLT, the patient presented with blurred vision in the treated eye and central stromal edema and haze were observed. The CDVA was 20/30, the IOP was 19 mm Hg, and a rare cell was noted in the anterior chamber. Topical prednisolone acetate and nepafenac were initiated. The CDVA decreased to 20/200 over the subsequent week. At 3 weeks, the CDVA improved to 20/60; the IOP was 15 mm Hg, the refraction −4.50 +1.75 × 170, and the CCT 478 µm; the central cornea had flattened with residual anterior stromal haze. Topical steroids were continued for 3 months. At 6 months, the CDVA was 20/30 with a hard contact lens, the CCT was 510 µm, and mild central stromal haze remained.
Case 3
A 46-year-old white woman had SLT in her right eye to treat POAG. Seventy-nine spots at 1.1 mJ per spot were applied to the trabecular meshwork over 360 degrees. Before SLT, the IOP was 17 mm Hg; 60 minutes after SLT it was 14 mm Hg. The pre-procedure refraction was −6.00 +0.50 × 16, the CDVA 20/20, and the CCT 515 µm. The pre-SLT IOP-lowering topical medications, latanoprost and timolol, were continued, and topical nepafenac was started. Two days after SLT, the patient presented with blurred vision in the treated eye. Diffuse dense stromal opacification that extended almost to the limbus was observed. The CDVA was 20/40−2 and the IOP 19 mm Hg; trace flare was noted in the anterior chamber. Topical prednisolone acetate was initiated. The CDVA decreased to 20/70 over the subsequent week. Three weeks after SLT, the CDVA was 20/70 and the IOP 19 mm Hg; the peripheral cornea had cleared with residual central stromal haze. At 6 weeks, the IOP was 20 mm Hg and the CCT 444 µm; a faint central stromal haze remained. Topical steroids were continued for 4 months, at which point the CDVA was 20/40, the refraction +0.25 +0.75 × 180, the IOP 13 mm Hg, and the CCT 475 µm; a faint central stromal haze remained. At 7 months, the uncorrected distance visual acuity (UDVA) was 20/30 and the cornea had cleared. At 11 months, the UDVA was 20/25 and the cornea remained clear.
Case 4
A 56-year-old white woman had SLT in her right eye to treat POAG. Ninety-six spots at 1.0 mJ per spot were applied to the trabecular meshwork over 360 degrees. Before SLT, the IOP was 14 mm Hg; 30 minutes after SLT, it was 16 mm Hg. The pre-procedure refraction was −5.25 +0.50 × 91, the CDVA 20/20, and the CCT 575 µm. The pre-SLT IOP-lowering topical medications, bimatoprost and brinzolamide, were continued. Two weeks after SLT, the patient presented with blurred vision and central stromal haze was noted. The CDVA was 20/60, the IOP 5 mm Hg, and the CCT 552 µm; the anterior chamber was quiet. Topical difluprednate and hypertonic saline were initiated and continued for 3 weeks. Three weeks after SLT, the CDVA was 20/50, the IOP was 12 mm Hg, the manifest refraction was −4.25 sphere, and the stromal haze was less dense. At 7 weeks, the CDVA was 20/25, the IOP 9 mm Hg, the manifest refraction −3.75 sphere, and the CCT 565 µm; the stromal haze had faded significantly. At 7 months, the CDVA was 20/25, the IOP 13 mm Hg, the refraction −2.50 +0.25 × 120, and the cornea had cleared.
DISCUSSION
Selective laser trabeculoplasty is generally a safe and effective procedure for IOP reduction. It is often used as an adjunct or alternative to topical IOP-lowering medications for the treatment of open-angle glaucoma. Initial studies report similar IOP reduction using 90 and 180 degrees of SLT treatment.6 Subsequent studies show a significantly greater IOP reduction, with few additional complications, using 360 degrees compared with 180 degrees of SLT treatment.7,8 Additionally, 360-degree treatment was shown to significantly decrease IOP fluctuations compared with 180-degree treatment.9 Thus, we routinely perform 360-degree treatments.
Commonly reported adverse effects, including anterior chamber reaction, ocular discomfort, and acute elevation of IOP, are usually mild, readily managed, and resolve without long-term sequelae10; however, these side effects have been shown to occur more often with 360-degree SLT treatment than with 180-degree treatment.7 More severe post-procedure reactions, namely hyphema, cystoid macular edema, and choroidal effusion, have also been reported with SLT.11–14 Furthermore, central corneal edema and haze following SLT have recently been described in 5 patients in 3 separate reports.3–5 We describe an additional 4 cases of acute corneal edema and stromal haze, followed by corneal thinning and a hyperopic shift in refraction (Table 1).
Table 1.
Patient characteristics before and after SLT.*
| Pre-SLT | Post-SLT | ||||||
|---|---|---|---|---|---|---|---|
|
|
|
||||||
| Patient | Sex/Age (Y) | CDVA | SE | CCT | CDVA | SE (Δ) | CCT (Δ) |
| 1 | F/63 | 20/25 | −12.5 | 544 | 20/40 | −10.9 (1.63) | 432 (−112) |
| 2 | F/56 | 20/20 | −8.25 | 606 | 20/30 | −3.63 (4.62) | 510 (−96) |
| 3 | F/46 | 20/20 | −5.75 | 515 | 20/25 | +0.625 (6.38) | 475 (−40) |
| 4 | F/56 | 20/20 | −5.00 | 575 | 20/25 | −2.38 (2.62) | 565 (−10) |
CDVA = corrected distance visual acuity; CCT = central corneal thickness (µm); SE = spherical equivalent (diopters); SLT = selective laser trabeculoplasty; Δ = change between post-SLT and pre-SLT values
Data from follow-up visits 3 weeks to 11 months
Recent reports have described corneal endothelial changes after SLT as assessed by specular microscopy.15–17 In extreme cases, these changes could result in endothelial dysfunction and subsequent edema following SLT. However, none of our 4 patients was found to have endothelial pigment prior to treatment. Specular microscopy was performed in patient 1 and did not show any endothelial pigment clumping, and the density, size, and shape of endothelial cells was neither abnormal nor measurably different between the treated and untreated eyes. Furthermore, endothelial dysfunction would not be expected to ultimately result in corneal thinning.
A previous case report speculated that HSV reactivation may be the etiology of acute corneal edema following SLT.3 None of our 4 patients had a history of herpetic eye disease, and all denied orofacial ulcers. Tear-film analysis for HSV by PCR, ELISA, and culture were negative in patient 1; however, reactivation of HSV causing endothelial dysfunction and subsequent corneal edema would not likely be detected in the tear film.18 All the patients were using topical prostaglandin analogs, which have been associated with reactivation of HSV.19,20 Despite a negative history for prior HSV infection, it remains possible that SLT-induced inflammation in the setting of baseline prostaglandin analog use tipped the balance toward a reactivation event. Residual central stromal thinning and haze are atypical for resolved HSV endotheliitis.
Corneal hydrops is a relatively uncommon condition characterized by findings of acute corneal edema followed by stromal thinning, sharing some similarity with the clinical courses described in this case series. Although none of the current patients had obvious corneal ectasia on clinical examination, all were moderately to highly myopic. Unfortunately, none of the patients had pre-SLT corneal topography. Although unlikely, pressure exhibited by the contact trabeculoplasty lens during treatment, patient eye rubbing following treatment, or a combination of these could have induced a break in Descemet membrane causing edema and subsequent thinning. However, tears in Descemet membrane were not detected clinically at any examination and all corneas had diffuse rather than focal edema and haze.
It is well known that laser trabeculoplasty induces cytokine production and activation of matrix metalloproteinases (MMPs). Many of the cytokines and MMPs expressed after laser trabeculoplasty are also involved in destructive inflammatory responses. For example, interleukin 1α and 1β, tumor necrosis factor-α, and MMP-3 are produced following experimental argon laser trabeculoplasty21 and SLT.22,23 These cytokines can enhance collagen degradation mediated by corneal fibroblasts.24,25 Theoretically, laser trabeculoplasty may elevate anterior chamber cytokine levels sufficiently to stimulate corneal fibroblasts to break down stromal collagen, leading to tissue thinning as seen in our 4 cases.
Although the underlying mechanism causing acute corneal edema followed by stromal thinning and hyperopic shift after routine SLT remains obscure, it likely represents a real and either underreported or underrecognized adverse effect. The patient in this series regained visual acuity within 2 Snellen lines of their pre-procedure acuity. However, they experienced hyperopic shifts from nearly 2.0 diopters (D) to greater than 5.0 D and 2 patients required contact lenses for best acuity. All 4 patients were moderately to highly myopic. The patients in 2 previously reported cases of corneal edema and subsequent thinning following SLT were also highly myopic. We recommend caution when planning SLT in patients with these characteristics.
Acknowledgments
Supported in part by an unrestricted grant from Research to Prevent Blindness, New York, New York, and The Eye and Ear Foundation, Pittsburgh, Pennsylvania, USA.
Biography

Jared E. Knickelbein, MD, PhD
UPMC Eye Center Department of Ophthalmology, University of Pittsburgh School of Medicine, Pittsburgh, Pennsylvania, USA
Footnotes
Financial Disclosure: No author has a financial or proprietary interest in any material or method mentioned.
Presented at the ASCRS Symposium on Cataract, IOL and Refractive Surgery, Boston, Massachusetts, USA, April 2014.
References
- 1.Wingard JB, Schuman JS. Laser trabeculoplasty. In: Kahook MY, Schuman JS, editors. Chandler and Grant’s Glaucoma. 5. Thorofare, NJ: Slack, Inc; 2013. pp. 477–485. [Google Scholar]
- 2.Realini T. Selective laser trabeculoplasty; a review. J Glaucoma. 2008;17:497–502. doi: 10.1097/IJG.0b013e31817d2386. [DOI] [PubMed] [Google Scholar]
- 3.Moubayed SP, Hamid M, Choremis J, Li G. An unusual finding of corneal edema complicating selective laser trabeculoplasty. Can J Ophthalmol. 2009;44:337–338. doi: 10.3129/i09-025. [DOI] [PubMed] [Google Scholar]
- 4.Regina M, Bunya VY, Orlin SE, Ansari H. Corneal edema and haze after selective laser trabeculoplasty. J Glaucoma. 2011;20:327–329. doi: 10.1097/IJG.0b013e3181e6668d. [DOI] [PubMed] [Google Scholar]
- 5.Song J, Yu D, Song A, Palmares T, Song HS, Song M. Corneal thinning and opacity following selective laser trabeculoplasty: a case report. [Accessed June 20, 2014];Br J Med Med Res. 2014 4:279–287. Available at: http://www.sciencedomain.org/download.php?f=Song412013BJMMR5446.pdf&aid=2022. [Google Scholar]
- 6.Chen E, Golchin S, Blomdahl S. A comparison between 90° and 180° selective laser trabeculoplasty. J Glaucoma. 2004;13:62–65. doi: 10.1097/00061198-200402000-00012. [DOI] [PubMed] [Google Scholar]
- 7.Nagar M, Ogunyomade A, O’Brart DPS, Howes F, Marshall J. A randomised, prospective study comparing selective laser trabeculoplasty with latanoprost for the control of intraocular pressure in ocular hypertension and open angle glaucoma. [Accessed June 20, 2014];Br J Ophthalmol. 2005 89:1413–1417. doi: 10.1136/bjo.2004.052795. Available at: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1772946/pdf/bjo08901413.pdf. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Shibata M, Sugiyama T, Ishida O, Ueki M, Kojima S, Okuda T, Ikeda T. Clinical results of selective laser trabeculoplasty in open-angle glaucoma in Japanese eyes: comparison of 180 degree with 360 degree SLT. J Glaucoma. 2012;21:17–21. doi: 10.1097/IJG.0b013e3181fc8020. [DOI] [PubMed] [Google Scholar]
- 9.Prasad N, Murthy S, Dagianis JJ, Latina MA. A comparison of the intervisit intraocular pressure fluctuation after 180 and 360 degrees of selective laser trabeculoplasty (SLT) as a primary therapy in primary open angle glaucoma and ocular hypertension. J Glaucoma. 2009;18:157–160. doi: 10.1097/IJG.0b013e3181752c97. [DOI] [PubMed] [Google Scholar]
- 10.Barkana Y, Belkin M. Selective laser trabeculoplasty. [Accessed June 20, 2014];Surv Ophthalmol. 2007 52:634–654. doi: 10.1016/j.survophthal.2007.08.014. Available at: http://www.v2020la.org/pub/PUBLICATIONS_BY_TOPICS/Glaucoma/Selective%20Laser%20Trabeculoplasty.pdf. [DOI] [PubMed] [Google Scholar]
- 11.Kim DY, Singh A. Severe iritis and choroidal effusion following selective laser trabeculoplasty. Ophthalmic Surg Lasers Imaging. 2008;39:409–411. doi: 10.3928/15428877-20080901-10. [DOI] [PubMed] [Google Scholar]
- 12.Rhee DJ, Krad O, Pasquale LR. Hyphema following selective laser trabeculoplasty. Ophthalmic Surg Lasers Imaging. 2009;40:493–494. doi: 10.3928/15428877-20090901-09. [DOI] [PubMed] [Google Scholar]
- 13.Shihadeh WA, Ritch R, Liebmann JM. Hyphema occurring during selective laser trabeculoplasty. Ophthalmic Surg Lasers Imaging. 2006;37:432–433. doi: 10.3928/15428877-20060901-14. [DOI] [PubMed] [Google Scholar]
- 14.Wechsler DZ, Wechsler IB. Cystoid macular oedema after selective laser trabeculoplasty [letter] [Accessed June 20, 2014];Eye. 2010 24:1113. doi: 10.1038/eye.2009.249. Available at: http://www.nature.com/eye/journal/v24/n6/pdf/eye2009249a.pdf. [DOI] [PubMed] [Google Scholar]
- 15.Ong K, Ong L. Selective laser trabeculoplasty may compromise corneas with pigment on endothelium [letter] Clin Exp Ophthal. 2013;41:109–110. doi: 10.1111/j.1442-9071.2012.02841.x. [DOI] [PubMed] [Google Scholar]
- 16.Ong K, Ong L, Ong L. Corneal endothelial changes after selective laser trabeculoplasty. Clin Exp Ophthalmol. 2013;41:537–540. doi: 10.1111/ceo.12068. [DOI] [PubMed] [Google Scholar]
- 17.Ong K, Ong L, Ong LB. Corneal endothelial abnormalities after SLT. J Glaucoma. 2013 Apr 29; doi: 10.1097/IJG.0b013e3182946381. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 18.Fukuda M, Deai T, Hibino T, Higaki S, Hayashi K, Shimomura Y. Quantitative analysis of herpes simplex virus genome in tears from patients with herpetic keratitis. Cornea. 2003;22(suppl):S55–S60. doi: 10.1097/00003226-200310001-00008. [DOI] [PubMed] [Google Scholar]
- 19.Kroll DM, Schuman JS. Reactivation of herpes simplex virus keratitis after initiating bimatoprost treatment for glaucoma. Am J Ophthalmol. 2002;133:401–403. doi: 10.1016/s0002-9394(01)01360-5. [DOI] [PubMed] [Google Scholar]
- 20.Wand M, Gilbert CM, Liesegang TJ. Latanoprost and herpes simplex keratitis. Am J Ophthalmol. 1999;127:602–604. doi: 10.1016/s0002-9394(99)00050-1. [DOI] [PubMed] [Google Scholar]
- 21.Bradley JMB, Anderssohn AM, Colvis CM, Parshley DE, Zhu XH, Ruddat MS, Samples JR, Acott TS. Mediation of laser trabeculoplasty-induced matrix metalloproteinase expression by IL-1β and TNFα. [Accessed June 20 2014];Invest Ophthalmol Vis Sci. 2000 41:422–430. Available at: http://www.iovs.org/cgi/reprint/41/2/422. [PubMed] [Google Scholar]
- 22.Alvarado JA, Betanzos A, Franse-Carman L, Chen J, González-Mariscal L. Endothelia of Schlemm’s canal and trabecular meshwork: distinct molecular, functional, and anatomic features. [Accessed June 20, 2014];AmJ Physiol Cell Physiol. 2004 286:C621–C634. doi: 10.1152/ajpcell.00108.2003. Available at: http://ajpcell.physiology.org/content/ajpcell/286/3/C621.full.pdf. [DOI] [PubMed] [Google Scholar]
- 23.Alvarado JA, Yeh R-F, Franse-Carman L, Marcellino G, Brownstein MJ. Interactions between endothelia of the trabecular meshwork and of Schlemm’s canal: a new insight into the regulation of aqueous outflow in the eye. [Accessed June 20, 2014];Trans Am Ophthalmol Soc. 2005 103:148–162. discussion, 162–163. Available at: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1447570/pdf/1545-6110_v103_p148.pdf. [PMC free article] [PubMed] [Google Scholar]
- 24.Kondo Y, Fukuda K, Adachi T, Nishida T. Inhibition by a selective IκB kinase-2 inhibitor of interleukin-1–induced collagen degradation by corneal fibroblasts in three-dimensional culture. [Accessed June 20, 2014];Invest Ophthalmol Vis Sci. 2008 49:4850–4857. doi: 10.1167/iovs.08-1897. Available at: http://www.iovs.org/content/49/11/4850.full.pdf. [DOI] [PubMed] [Google Scholar]
- 25.Lu Y, Fukuda K, Li Q, Kumagai N, Nishida T. Role of nuclear factor-κB in interleukin-1-induced collagen degradation by corneal fibroblasts. Exp Eye Res. 2006;83:560–568. doi: 10.1016/j.exer.2006.02.008. [DOI] [PubMed] [Google Scholar]