Abstract
Purpose
The purpose of this study is to describe the outcomes of a technician-delivered glaucoma referral triaging service with ‘virtual review’ of resultant data by a consultant ophthalmologist.
Patients and methods
The Glaucoma Screening Clinic reviewed new optometrist or GP-initiated glaucoma suspect referrals into a specialist ophthalmic hospital. Patients underwent testing by three ophthalmic technicians in a dedicated clinical facility. Data were reviewed at a different time and date by a consultant glaucoma ophthalmologist. Approximately 10% of discharged patients were reviewed in a face-to-face consultant-led clinic to examine the false-negative rate of the service.
Results
Between 1 March 2014 and 31 March 2016, 1380 patients were seen in the clinic. The number of patients discharged following consultant virtual review was 855 (62%). The positive predictive value of onward referrals was 84%. Three of the 82 patients brought back for face-to-face review were deemed to require treatment, equating to negative predictive value of 96%.
Conclusions
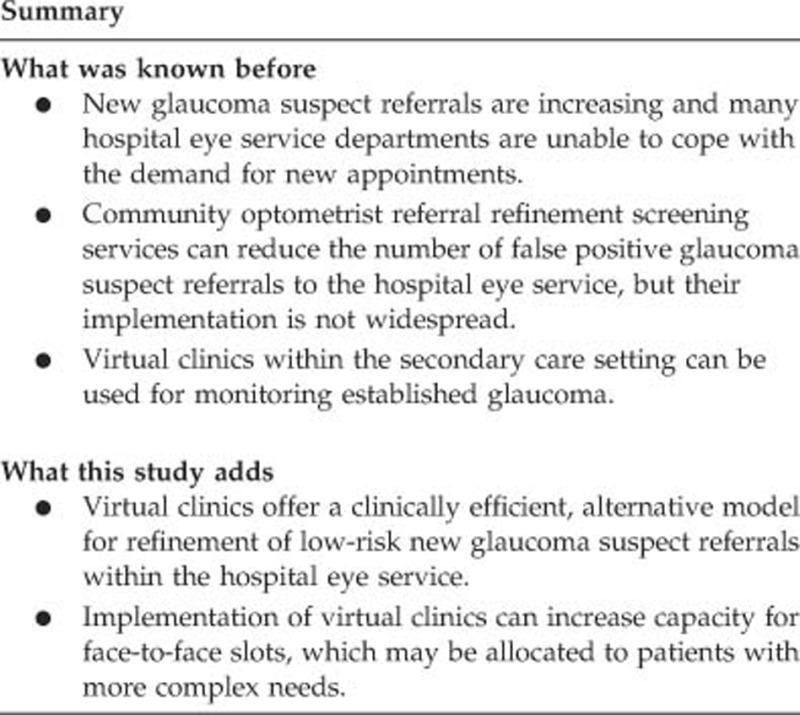
Our technician-delivered glaucoma referral triaging clinic incorporates consultant ‘virtual review’ to provide a service model that significantly reduces the number of onward referrals into the glaucoma outpatient department. This model may be an alternative to departments where there are difficulties in implementing optometrist-led community-based referral refinement schemes.
Introduction
Glaucoma is the leading cause of irreversible blindness worldwide1 and, once diagnosed, requires lifelong monitoring. The disease is more prevalent with advancing age and with our increasingly aging population2 the number of glaucoma cases is only set to increase.3
In 2009, the National Institute for Health and Care Excellence (NICE) released guidance on the diagnosis and management of glaucoma.4 The intent of these guidelines was to both clarify and unify service provision between primary and secondary care on the management of OHT and open-angle glaucoma.5 However, an unintended consequence of these guidelines was a change in the patterns of referral behaviour by community optometrists, which has led to an increased number of referrals to the hospital eye service (HES),6, 7 with little change in the proportion of those with a ‘true positive’ for either OHT or glaucoma.8, 9 To cope with the increase in referrals, some Clinical Commissioning Groups have developed either community optometrist repeat-measures schemes (whereby measurements such as intraocular pressure (IOP) or visual fields (VFs) are repeated to confirm the presence of an ‘abnormal’ result) or community optometrist referral refinement schemes, whereby community optometrists with a special interest in glaucoma are trained to interpret the results of clinical tests used specifically to detect OHT or open angle glaucoma.10 Published results suggest that these schemes are successful at reducing the number of onward referrals to the HES; however, uptake of these types of schemes across the country is not widespread.11, 12, 13, 14, 15, 16, 17, 18
At Moorfields Eye Hospital NHS Foundation Trust, London, we have introduced an in-house referral triaging service that runs as an asynchronous virtual clinic. A virtual clinic is one in which the face-to-face clinician consultation is removed. In a synchronous model, the patient and clinician interact in real time, for example, via a webcam. In the asynchronous model, the interaction occurs at different times. Virtual monitoring clinics are not new to glaucoma monitoring19, 20 and, recently, Trikha et al21 have described a virtual glaucoma refinement service utilising community optometrists.The feasibility of virtual clinics for new patient assessment has been examined by Rathod et al,22 who found good agreement between face-to-face clinical decision-making and that made from assessment of clinical data for patients attending their Glaucoma Assessment Clinic.
In our virtual glaucoma referral triaging service, trained ophthalmic technicians perform diagnostic testing on patients, the results of which are reviewed at a later time/date by a consultant glaucoma ophthalmologist. Technicians are all trained in-house and have internally approved competencies in using the diagnostic equipment within the service. The service was introduced following an unsuccessful pilot community optometrist referral refinement scheme.
Methods
The Glaucoma Screening Clinic (GSC) was started in March 2014. All new optometrist or GP initiated glaucoma/OHT suspect referrals entering the hospital are directed to a centralised booking centre and scrutinised by two optometrists. For the first 12 months, only ‘low-risk’ patients were allocated to the service. ‘Low risk’ was defined as having only one of the following three risk factors: suspicious optic discs, suspicious VFs, and IOP >20 mm Hg. From March 2015 to present, the scrutinising optometrists are allowed to exercise their clinical judgment and include patients who present with up to three risk factors (where positive family history in a first degree relative is also included as a risk factor) into the GSC, if the evidence presented in the referral letter is inconclusive. As an example, a patient referred with optic disc asymmetry, a nonspecific VF defect and IOP of 21 mm Hg would be directed into the GSC. Referrals in which it was clear that the patient showed definitive signs of having the condition or were angle closure suspects, or patients referred with an IOP >32 mm Hg have been deemed ineligible for the GSC. Patients booked into the GSC are sent a patient information leaflet advising them of the nature of the clinic, and that they do not see a doctor on the day of their appointment.
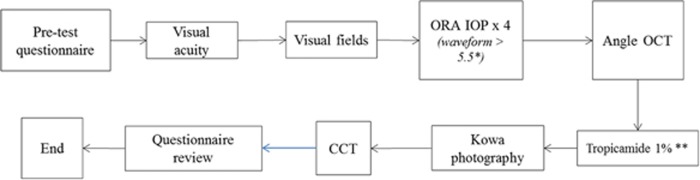
Patients attending the service are seen by three ophthalmic trained technicians who performed tests in a streamlined manner (see Figure 1). Acuities are measured using COMPlog (Version 1.3.60, COMPlog Clinical Vision Measurement Systems Ltd, London, UK). The Humphrey Field Analyzer (Carl-Zeiss Meditec, CA, USA) SITA 24-2 standard test strategy is used to assess VFs. IOP is measured using the Reichert Ocular Response Analyzer (ORA; Ametek, Inc. and Reichert, Inc., Depew, NY, USA); both IOPg and IOPcc are recorded. Angle assessment is performed with a temporal and nasal line scan using the Topcon 3D 2000 optical coherence tomographer (Topcon Corporation, Tokyo, Japan). Disc imaging is performed using the Kowa non-mydriatic WX3D stereo-fundus camera (Kowa Company Ltd., Nagoya, Japan); two fundus images are taken in each eye: one a stereo-image of the optic disc and the second a wider field monosopic image of the disc and macula. Central corneal thickness is measured using an ultrasound pachymeter (DGH Pachmate, DGH Technology, Inc., Exton, PA, USA). A questionnaire enquiring about the presence of any systemic risk factors, medication details, previous ocular or other operations, family history, and driving status is administered on arrival and answers confirmed by the technician before the patient leaves the clinic. Patients who have an IOP >32 mm Hg on the day of their screening visit are taken to a consultant delivered clinic on the same day. Patients are advised upon leaving the service that they will receive a letter advising the outcome within 2 weeks of their appointment.
Figure 1.
Flow-through GSC. Journey times from start to finish are collected on a paper proforma. Key: *, the ORA waveform score indicates the quality of measurement, thus only scores >5.5 (out of a possible 9) are acceptable; **, tropicamide would only be instilled if the angle measured >25° CCT, central corneal thickness, measured following instillation of one drop of topical anaesthetic.
Data are entered into the patient’s electronic patient record (OpenEyes; www.openeyes.org) and patients are ‘referred’ to the ‘virtual clinic’ list. When the reviewing consultant logs into their OpenEyes page, they are directed to the ‘virtual clinic’ and a list of all patients seen in the GSC are available to view. The consultant has a laptop with a stereo-monitor (LG A520-3D; LG Computing, Seoul, Korea); thus, all reviews are performed remotely without the need for paper notes. The consultant has one 3.5 h session per week to review referrals. Since November 2015, the service is operating at 12 patients per 3.5 h session, 2 sessions per week.
On review of the data, the consultant chooses two outcomes: discharge from the service or follow-up in the outpatient clinic. The outcomes of those patients attending for a second, face-to-face, consultation were collected in order to determine the false positive rate of the GSC.
False negative audit
From November 2014, the clinic administrator was asked to randomly select one patient discharged from each GSC to bring back for a face-to-face consultant review within 8 weeks of being discharged. Patients were suitable to be booked into any glaucoma outpatient clinic excluding that led by the GSC reviewing consultant. These audit patients were advised that attendance was voluntary, and that the exercise was part of the hospital’s ongoing quality assurance programme.
Results
Between 1 March 2014 and 31 March 2016, 1,532 patients were booked into the GSC. One hundred and fifty two patients (10%) failed to attend their appointment. The average (SD) journey time in the clinic was 58 (16) min. The majority of patients were reviewed by a single consultant (JB; 1097 patients, 79%), with leave cover by other glaucoma consultants. The average (SD) time from patient attendance to consultant virtual review was 4 (4) days. The number of patients discharged following consultant virtual review was 855 (62%).
Of the remaining 525 patients, 16 patients (1%) required same-day doctor assessment, as they presented with elevated IOP. Ninety one (6%) patients were booked for a follow-up in the Glaucoma Monitoring Service, the service’s sister virtual clinic for stable OHT, glaucoma suspect, or early-to-moderate glaucoma patients.20 The diagnoses of the 418 patients who were referred for face-to-face outpatient review are presented in Table 1.
Table 1. Outcomes of the 418 patients who were referred for face-to-face consultation.
| Diagnosis | Number (%) |
|---|---|
| OHT (monitor) | 47 (11) |
| OHT (treat) | 25 (6) |
| Glaucoma suspect (monitor) | 155 (37) |
| Glaucoma (treat) | 75 (18) |
| Non-occludable narrow angles (monitor) | 7 (2) |
| Occludable, narrow angles (intervention required) | 20 (5) |
| Discharged | 64 (15) |
| Did not attend/awaiting appointment | 25 (6) |
Abbreviations: CI, confidence intervals; GSC, Glaucoma Screening Clinic.
The positive predictive value of the GSC was 83.7% (95% CI=79.9–87.2%).
False negative audit
Between 10 November 2014 and 14 March 2016, 157 (18%) patients discharged from the GSC following virtual review were invited to re-attend for a face-to-face ophthalmologist consultation; 82 patients (9%) accepted the invitation and were reviewed in clinic. Sixty-six patients were discharged following consultation, in agreement with the virtual review; this equates to a GSC false-negative rate of 20%. The negative-predictive value (NPV) of the GSC was 79% (95% CI=68.1–87.5%)
The diagnosis of the 16 patients in whom the face-to-face consultation disagreed with the decision of the virtual review are detailed in Table 1. For the majority of patients, no treatment was instigated at the face-to-face appointment, but instead they were kept under clinic review. However, only three patients required medical intervention, equivalent to a ‘significant’ false-negative rate of 4%, or a revised NPV of 96.3% (95% CI=89.7–99.2%). Two of these patients were diagnosed as being ocular hypertensives; one required treatment based on the NICE guidelines, whereas the second presented at the face-to-face review with an IOP level twice that found both at the GSC visit and in the original referral letter. One patient was diagnosed as having occludable angles requiring prophylactic laser iridotomy, but had no evidence of glaucoma Table 2.
Table 2. Outcomes of the 16 patients who were initially discharged following their GSC appointment, but deemed to require further management at their face-to-face visit.
| Diagnosis | Management | Number of patients |
|---|---|---|
| OHT | Monitor | 3 |
| OHT | Treat | 2 |
| Glaucoma suspect: suspicious discs | Monitor | 6 |
| Unreliable visual fields | Monitor | 2 |
| Non-occludable, narrow anglesa | Monitor | 1 |
| Occludable anglesa | Treat | 1 |
| Angle recession | Monitor | 1 |
Abbreviation: GSC, Glaucoma Screening Clinic.
For both these patients, the original referral letter indicated a grade 4 Van Herick angle.
Discussion
This study reports the outcomes of an in-house, ophthalmic technician-delivered ‘virtual’ glaucoma referral triaging service for new optometrist or GP-initiated glaucoma suspect referrals into a specialist ophthalmic hospital in London. The service was successful at reducing the number of onward referrals to the glaucoma outpatient clinic by over 60%. The false-positive rate of onward referrals to the outpatient service was 15% and a ‘glaucoma miss rate’ of 4% for a sub-group assessed later and found to require medical intervention.
There are a number of established optometrist-delivered referral refinement schemes across the UK, with those based in Manchester,11 Huntingdon,14 Cambridge,17 Cardiff,15 and Bexley13 having published their experiences. In these schemes, the decision of whether the patient is ‘normal’ or ‘suspect’ is made by a suitably trained optometrist with appropriate in-house equipment. Another model is the virtual clinic model proposed by Trikha et al,21 whereby community-based optometrists collect clinical information, but the decision of ‘normal’ or ‘suspect’ is made by a consultant ophthalmologist. Optometrists are ideally placed to deliver community refinement, as they possess the equipment23 and clinical expertise for assessments. However, although many community optometrists may wish to have a more extended role in primary care, the remuneration to participate in such schemes is often insufficient for the optometry practice business model.24 We would propose that in areas where uptake of community refinement is low or where there are scant resources to initiate these schemes, which include the training and education of personnel, our technician-delivered virtual glaucoma refinement model may be a suitable alternative.
The positive-predictive value of the GSC was~84%, which is comparable to the optometrist refinement schemes in Manchester11 Huntingdon,14 and Carmarthenshire,15 and the Portsmouth community optometrist virtual clinic model.21 On first review, our false-negative rate of 20% may be a cause of concern. However, on further inspection, if we assess the number of patients requiring an intervention who were missed by the GSC, this falls to 4%. The Carmarthenshire scheme estimated a false-negative rate of between 3 and 10% based on consultant review of optic disc photographs.15 In Huntingdon, a recent evaluation of community optometrists participating in the CHANGE scheme revealed a false negative rate of 15%, but a 0% ‘glaucoma miss rate’ that is, no patients discharged by the community optometrist required treatment following consultant review. In a recent report of the Cambridge community optometrist refinement scheme, a 5% false-negative rate was found following consultant face-to-face review of a proportion of patients discharged following community refinement.17 In our study, 3 (4%) of the patients brought back for the false negative audit were deemed to require treatment and 13 (16%) were kept under the HES for observation. It is recognised that very early glaucoma is challenging to detect.5 Furthermore, it is well known that expert clinicians exhibit a wide range of agreement with each other, and even themselves, when diagnosing or managing the condition.25, 26, 27 It is our policy to advise all patients who are discharged from the GSC to visit their optometrist for annual or biennial eye exams in the future. If this advice is followed, we hope that any abnormality that was missed the first time would be detected at subsequent examinations, particularly if the physical signs become more pronounced. However, this remains unproven. The fact that two patients with narrow angles were ‘missed’ despite anterior segment imaging does raise some concerns. We have taken the view that angle-closure suspect referrals are not suitable for the clinic and it should be noted that in both cases, the optometrist referral letter indicate wide open angle on Van Herick’s assessment. In both cases, the anterior segment OCT showed no evidence of irido-trabecular contact. Studies suggest that anterior segment OCT tends to ‘overcall’ closed angles28 and assessment of drainage angle width is exquisitely dependent on the lighting conditions and examination technique, especially in borderline cases.29 Of the three patients who required intervention, none were given a diagnosis of glaucoma. Referral refinement services are put in place to improve the quality of referrals and not miss disease, and our service did not miss any cases of glaucoma. We should also put our findings into perspective; our false-negative rate of 4% is better than that reported by some screening programmes for breast and cervical cancer, which report false-negative rates of up to 34 and 58%, respectively.30 However, we are looking for ways of improving the service and will soon be introducing optical coherence disc imaging as the standard method of optic disc assessment.
Another potential criticism of our service is that it is not in line with NICE guidelines, which recommend that referral refinement schemes use Van Herick’s method for angle assessment and applanation tonometry for IOP measurement;4 we used neither. In designing the clinic, we had to decide upon what was practical and maintain a balance between quality and efficiency. There are a number of reports that highlight the imprecision of applanation tonometry31, 32 and a recent NIHR Health Technology Assessment report concluded that, based on current evidence, Goldmann applanation tonometry may not be the most appropriate reference standard for IOP measurement.33 Based on our experience,34 we felt that the ORA was an acceptable alternative to use. In addition, the training and time required to undertake Van Herick assessment was felt to be outweighed by the simplicity of using an objective method, which provides a documentary record of angle status.35 Emerging evidence suggests that implementation of NICE guidelines for glaucoma and OHT monitoring is not always feasible36 or cost-effective37 within most NHS HES departments. Year on year, data from NHS England shows that the use of hospital outpatient services for ophthalmology rank second in the country, with orthopaedics and trauma topping the list (7.07 million versus 7.52 million outpatient appointments in 2014–15, respectively, from http://www.hscic.gov.uk/home); we are in the midst of a capacity crisis.38, 39, 40, 41 Thus, we need to be open to new models of service delivery if we are to cope42 and be pragmatic about the tests we need to conduct to detect sight-threatening disease.37 Our GSC has freed up 24 face-to-face new patient slots per week, allowing more complex-needs patients to be assessed by a consultant team. As such, we feel that the model is a successful one and it is being expanded.
Our choice of developing the service in-house was primarily for convenience. As Trikha et al21 have shown, it is possible to have virtual refinement services in the community. Our model could be transferred to GP practices or even non-NHS organisations, such that patient data is collected in a location convenient to the patient, but clinical decision-making and the overall responsibility for the patient lay with the secondary care consultant. However, this type of virtual refinement model relies on a solid IT infrastructure and the ability to securely share information between different healthcare providers. Up until now, it has been impossible to share electronic information, such as digital VF and optic disc imaging data, between non-NHS and NHS settings without incurring the considerable expense of installing an N3 line.43 It is hoped that the new Health and Social Care Network programme will better facilitate the secure sharing of medical information between different healthcare settings.44
In summary, our novel technician-delivered glaucoma referral triaging service with consultant virtual review offers an alternative model for evaluating new glaucoma suspect referrals that is successful at reducing the number of onward referrals into the standard outpatient clinic. The service may be a useful alternative for Trusts where there are difficulties in implementing other community based referral refinement schemes. Further work will examine the cost comparisons between this model of service compared to other models of care, including the standard out-patient service.
Acknowledgments
We thank Mr Ananth Viswanathan, Mr Ahmed Elkarmouty, and Mr Jonathan Clarke for reviewing patients in the GSC, and all the technicians involved in running the service. Dr Kotecha and Professor Foster receive a proportion of their funding from the Department of Health’s National Institute for Health Research Biomedical Research Centre for Ophthalmology at Moorfields Eye Hospital NHS Foundation Trust and the UCL Institute of Ophthalmology.
Footnotes
The authors declare no conflict of interest.
References
- Tham YC, Li X, Wong TY, Quigly HA, Aung T, Cheng CY. Global prevalence of glaucoma and projections of glaucoma burden through 2040: a systematic review and meta-analysis. Ophthalmology 2014; 121: 2081–2090. [DOI] [PubMed] [Google Scholar]
- Department of Work and Pensions. Focus on Older People. Office of National Statistics, 2005. Available from: http://www.statistics.gov.uk/cci/nugget.asp?id=1352 (accessed 14 January 2015).
- Tuck MW, Crick RP. The projected increase in glaucoma due to an ageing population. Ophthalmic Physiol Opt 2003; 23(2): 175–179. [DOI] [PubMed] [Google Scholar]
- NICE. National Institute of Clinical Excellence (NICE) Guidance CG85 Glaucoma: Diagnosis and Management of Chronic Open Angle Glaucoma and Ocular Hypertension. April 2009; Available from: http://guidance.nice.org.uk/CG85.
- National Eye Care Service Steering Group. First Report of the National Eye Care Services Steering Group. 2004. Available from: http://webarchive.nationalarchives.gov.uk/20130107105354/http://www.dh.gov.uk/prod_consum_dh/groups/dh_digitalassets/@dh/@en/documents/digitalasset/dh_4080999.pdf (accessed 6 June 2015).
- Edgar DF, Romanay T, Lawrenson J, Myint J. Referral behaviour among optometrists: increase in the number of referrals from optometrists following the publication of the April 2009 NICE guidelines for the diagnosis and management of coag and oht in england and wales and its implications. Optometry Practice 2010; 11(1): 33–38. [Google Scholar]
- Ratnarajan G, Newson W, French K, Kean J, Chang L, Parker M et al. The impact of glaucoma referral refinement criteria on referral to, and first-visit discharge rates from, the hospital eye service: the Health Innovation & Education Cluster (HIEC) Glaucoma Pathways project. Ophthalmic Physiol Opt 2013; 33(2): 183–189. [DOI] [PubMed] [Google Scholar]
- Shah S, Murdoch IE. NICE—impact on glaucoma case detection. Ophthalmic Physiol Opt 2011; 31(4): 339–342. [DOI] [PubMed] [Google Scholar]
- de Silva SR, Riaz Y, Purbrick RM, Salmon JF. There is a trend for the diagnosis of glaucoma to be made at an earlier stage in 2010 compared to 2008 in Oxford, United Kingdom. Ophthalmic Physiol Opt 2013; 33(2): 179–182. [DOI] [PubMed] [Google Scholar]
- NICE. Quality Standard, Cost Impact and Commissioning Assessment: Quality Standard for Glaucoma, March 2011 (updated March 2012). National Institute for Health and Clinical Excellence. Available from: https://www.nice.org.uk/guidance/qs7/resources/cost-impact-and-commissioning-assessment-quality-standard-for-glaucoma-252279325 (accessed August 2016).
- Henson DB, Spencer AF, Harper R, Cadman EJ. Community refinement of glaucoma referrals. Eye 2003; 17(1): 21–26. [DOI] [PubMed] [Google Scholar]
- Syam P, Rughani K, Vardy SJ, Rimmer T, Fitt A, Husain T et al. The Peterborough scheme for community specialist optometrists in glaucoma: a feasibility study. Eye (Lond) 2010; 24(7): 1156–1164. [DOI] [PubMed] [Google Scholar]
- Parkins DJ, Edgar DF. Comparison of the effectiveness of two enhanced glaucoma referral schemes. Ophthalmic Physiol Opt 2011; 31(4): 343–352. [DOI] [PubMed] [Google Scholar]
- Bourne RR, French KA, Chang L, Borman AD, Hingorani M, Newsom WD. Can a community optometrist-based referral refinement scheme reduce false-positive glaucoma hospital referrals without compromising quality of care? The community and hospital allied network glaucoma evaluation scheme (CHANGES). Eye (Lond) 2010; 24(5): 881–887. [DOI] [PubMed] [Google Scholar]
- Devarajan N, Williams GS, Hopes M, O’Sullivan D, Jones D. The Carmarthenshire Glaucoma Referral Refinement Scheme, a safe and efficient screening service. Eye (Lond) 2011; 25(1): 43–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ratnarajan G, Newsom W, Vernon SA, Fenerty C, Henson D, Spencer F et al. The effectiveness of schemes that refine referrals between primary and secondary care—the UK experience with glaucoma referrals: the Health Innovation & Education Cluster (HIEC) Glaucoma Pathways Project. BMJ Open 2013; 3: 7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keenan J, Shahid H, Bourne RR, White AJ, Martin KR. Cambridge community optometry glaucoma scheme. Clin Experiment Ophthalmol 2015; 43(3): 221–227. [DOI] [PubMed] [Google Scholar]
- Roberts HW, Rughani K, Syam P, Dhingra S, Ramirez-Florez S. The Peterborough scheme for community specialist optometrists in glaucoma: results of 4 years of a two-tiered community-based assessment and follow-up service. Curr Eye Res 2015; 40(7): 690–696. [DOI] [PubMed] [Google Scholar]
- Wright HR, Diamond JP. Service innovation in glaucoma management: using a web-based electronic patient record to facilitate virtual specialist supervision of a shared care glaucoma programme. Br J Ophthalmol 2015; 99(3): 313–317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kotecha A, Baldwin A, Brookes J, Kotecha A. Experiences with developing and implementing a virtual clinic for glaucoma care in an NHS setting. Clin Ophthalmol 2015; 9: 1915–1923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trikha S et al. The Portsmouth-based glaucoma refinement scheme: a role for virtual clinics in the future? Eye (Lond) 2012; 26(10): 1288–1294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rathod D, Win T, Pickering S, Austin M. Incorporation of a virtual assessment into a care pathway for initial glaucoma management: feasibility study. Clin Exp Ophthalmol 2008; 36(6): 543–546. [DOI] [PubMed] [Google Scholar]
- Dabasia PL, Edgar DF, Garway-Heath DF, Lawrenson JG. A survey of current and anticipated use of standard and specialist equipment by UK optometrists. Ophthalmic Physiol Opt 2014; 34(5): 592–613. [DOI] [PubMed] [Google Scholar]
- Konstantakopoulou E, Harper RA, Edgar DF, Lawrenson JG et al. A qualitative study of stakeholder views regarding participation in locally commissioned enhanced optometric services. BMJ Open 2014; 4(5): e004781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weinreb RN. Clinical decision-making in cyberspace. J Glaucoma 1997; 6(1): 1–2. [PubMed] [Google Scholar]
- Murdoch I, Johnston RL. Consultant clinical decision making in a glaucoma clinic. Eye (Lond) 2010; 24(6): 1028–1030. [DOI] [PubMed] [Google Scholar]
- van der Schoot J, Reus NJ, Garway-Heath DF, Saarela V, Anton A, Bron AM et al. Accuracy of matching optic discs with visual fields: the European Structure and Function Assessment Trial (ESAFAT). Ophthalmology 2013; 120(12): 2470–2475. [DOI] [PubMed] [Google Scholar]
- Nolan WP, See JL, Chew PT, Friedman DS, Smith SD, Radhakrishnan S et al. Detection of primary angle closure using anterior segment optical coherence tomography in Asian eyes. Ophthalmology 2007; 114(1): 33–39. [DOI] [PubMed] [Google Scholar]
- Foster PJ, Aung T, Nolan WP, Machin D, Baasanhu J, Khaw PT et al. Defining 'occludable' angles in population surveys: drainage angle width, peripheral anterior synechiae, and glaucomatous optic neuropathy in east Asian people. Br J Ophthalmol 2004; 88(4): 486–490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petticrew MP, Sowden AJ, Lister-Sharp D, Wright K. False-negative results in screening programmes: systematic review of impact and implications. Health Technol Assess 2000; 4(5): 1–120. [PubMed] [Google Scholar]
- Whitacre MM, Stein R. Sources of error with use of Goldmann-type tonometers. Survey Ophthalmol 1993; 38(1): 1–30. [DOI] [PubMed] [Google Scholar]
- Ajtony C, Elkarmouty A, Barton K, Kotecha A. Applanation tonometry: interobserver and prism agreement using the reusable Goldmann applanation prism and the Tonosafe disposable prism. Br J Ophthalmol 2016; 100(6): 848–853. [DOI] [PubMed] [Google Scholar]
- Burr JM, Botello-Pinzen P, Takwoingi Y, Hernandez R, Vasquez-Montes M, Elders A et al. Surveillance for ocular hypertension: an evidence synthesis and economic evaluation. Health Technol Assess 2012; 16(29): 1–271, iii-iv. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kotecha A, White E, Schlottmann PG, Garway-Heath DF. Intraocular pressure measurement precision with the Goldmann applanation, dynamic contour, and ocular response analyzer tonometers. Ophthalmology 2010; 117(4): 730–737. [DOI] [PubMed] [Google Scholar]
- Campbell P, Redmond T, Agarwal R, Marshall LR, Evans BJ. Repeatability and comparison of clinical techniques for anterior chamber angle assessment. Ophthalmic Physiol Opt 2015; 35(2): 170–178. [DOI] [PubMed] [Google Scholar]
- Malik R, Baker H, Russell RA, Crabb DP. A survey of attitudes of glaucoma subspecialists in England and Wales to visual field test intervals in relation to NICE guidelines. BMJ Open 2013; 3: 5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hernandez R, Burr JM, Vale L, Azuara-Blanco A, Cook JA, Banister K et al. Monitoring ocular hypertension, how much and how often? A cost-effectiveness perspective. Br J Ophthalmol 2015; 100: 1263–1268. [DOI] [PubMed] [Google Scholar]
- Chalk D, Smith M. Guidelines on glaucoma and the demand for services. Br J Healthcare Management 2013; 19(10): 476–481. [Google Scholar]
- RNIB. Saving Money, Losing Sight. RNIB Campaign Report November 2013. Available from: http://www.rnib.org.uk/sites/default/files/Saving%20money%20losing%20sight%20Campaign%20report_0.pdf (accessed January 2016).
- Smith R. Our ophthalmology service is ‘failing’, please help! Royal College of Ophthalmologists Professional Standards Committee, 15 August 2013. Available from: https://www.rcophth.ac.uk/2013/08/our-ophthalmology-service-is-failing-please-help/ (accessed March 2016).
- Kotecha A, Turner S, Vasilakis C, Utley M, Fulop N, Azuara-Blanco A et al. Improving care and increasing efficiency-challenges in the care of chronic eye diseases. Eye (Lond) 2014; 28(7): 779–783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sim DA et al. The evolution of teleophthalmology programs in the united kingdom: beyond diabetic retinopathy screening. J Diabetes Sci Technol 2016; 10(2): 308–317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- House of Commons Committee of Public Accounts. The dismantled National Programme for IT in the NHS, 2013. Available from: http://www.publications.parliament.uk/pa/cm201314/cmselect/cmpubacc/294/294.pdf (accessed July 2016).
- Health and Social Care Information Centre. Information and Technology for Better Care, March 2015. Available from: https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/443353/HSCIC-Strategy-2015-2020-FINAL-310315.pdf (accessed August 2016).