Abstract
Objective
Clinical outcomes in rheumatoid arthritis (RA) are improved if the disease is treated early. However, treatment is often significantly delayed as a result of delayed help-seeking by patients who fail to recognise its symptoms or the need for rapid medical attention. Two studies were conducted to investigate the role of symptom recognition in help-seeking for the symptoms of RA and compared this with angina and bowel cancer.
Methods
A qualitative interview study with 31 individuals and a survey of 1088 members of the general public (all without RA) were conducted. Both studies used vignettes describing the symptoms of RA, bowel cancer and angina. Participants made causal attributions and rated the perceived seriousness of the symptoms and the urgency with which they would seek medical help if confronted with these symptoms.
Results
Only a small proportion of participants in both studies recognised the symptoms of RA, whereas the symptoms of bowel cancer and angina were readily recognised by many participants and considered to be more serious and to require more rapid medical attention (Z values of 14.7 to 34.2, p<.001).
Conclusion
Accurate symptom attribution and the perception that symptoms are indicative of a serious underlying condition are both important drivers for rapid help-seeking. In the case of angina and bowel cancer, recent campaigns have promoted not only recognition of symptoms and their seriousness, but also emphasised the consequences of not seeking timely help. Our results suggest that these consequences should also be addressed in any public health campaign for RA.
Rheumatoid arthritis (RA) is common, with a prevalence of approximately 1%(1). Early treatment reduces the risk of joint damage and disability(2–7), however, the commencement of disease modifying therapy is often delayed(5;8–11). One important source of delay is the patient themselves who often wait many weeks before seeking medical attention(11).
In order for a symptomatic person to seek medical attention they usually need to infer a causal disease for which therapy may be available(12–14). The appraisal of symptoms and subsequent decision-making are influenced by a range of demographic, socio-cultural and psychological factors(15;16) including the knowledge and beliefs that an individual has about a disease(17).
It is known that people often misinterpret the symptoms of RA(18), for example confusing them with those of osteoarthritis or interpreting them as a natural consequence of ageing(17). Lack of awareness of the symptoms of RA, its consequences and the availability of effective disease modifying therapies are possible explanations for patient delay following symptom onset.
Public health campaigns can have a positive impact on symptom recognition and subsequent decisions about seeking medical attention. For example, a UK based ‘Be Clear on Cancer’ (BCOC; Public Health England) campaign targeting bowel cancer via TV, radio and posters(19), resulted in increased knowledge and more rapid help-seeking(20;21). Other recent public health campaigns in the UK include initiatives to raise awareness of ischaemic heart disease(22). In contrast, efforts to increase public awareness of RA symptoms have been limited in the UK(23).
Due to the recent public awareness campaigns for bowel cancer and ischaemic heart disease, we expect that people are more aware of the symptoms of these conditions than those of RA, and that they are more likely to attribute these symptoms to the correct disease, and to seek early medical help. This paper describes two studies designed to assess the role of disease knowledge and symptom recognition in decision-making about help-seeking for the symptoms of RA compared with those of other diseases.
Participants and Methods
Qualitative study: data collection and analysis
Patients from two inner city general practices, aged 18 years and over, without a diagnosis of inflammatory arthritis were sent postal invitations to participate. Participants were purposively sampled from three age groups (18-40, 41-60 and over 61years) to reflect the age distribution for RA onset(24). The study was also advertised using posters at the Universities of Birmingham and Keele.
32 individuals were recruited (31 by post and 1 through poster advertisement). One participant’s data, collected during the only telephone interview conducted, were discarded due to technical problems with the recording. The remaining 31 participants (16 females) were aged between 23 and 84 years; 29 were of white ethnic background (Supplementary Table 1).
Semi-structured interviews were conducted face-to-face (by GS) in the general practices or at the University of Birmingham. Interviews lasted approximately 60 minutes and were guided by an interview schedule developed in collaboration with patient research partners and informed by previous research(17;18). Participants were asked to read and discuss two written vignettes describing what a person with symptoms of early RA may experience (A: ‘Joint pain and stiffness in hands and wrists’ and B: ‘Joint pain, stiffness and swelling in hands and wrists’), and vignettes describing symptoms of bowel cancer and angina (Supplementary Table 2). The order of the vignettes was alternated between interviewees with either the RA vignettes or the bowel cancer and angina vignettes discussed first. Interview questions explored participants’ perceptions of the symptoms, including their seriousness, and participants’ anticipated courses of action if they were to experience such symptoms.
Interviews were audio recorded and transcribed verbatim. Blind coding of five transcripts was undertaken by KK and GS. A few minor coding discrepancies were discussed and resolved before the full coding was undertaken by GS using qualitative data analysis software (NVivo, version 10; QSR International). The data were coded using thematic analysis(25). Data presented in this manuscript focus on themes related to possible causes of symptoms, their perceived seriousness and likely help-seeking after their development.
Quantitative study: data collection and analysis
A survey was mailed to 3400 persons registered with one of four inner-city general practices, who were over 18 years of age, and without a diagnosis of inflammatory arthritis. 1088 people (291 males, 788 females; 9 data not available) aged between 18 and 96 years completed the survey (response rate 32%). The majority (84.5%) of respondents were of a white ethnic background (Supplementary Table 3).
The survey included five vignettes, similar to those used in the qualitative interviews, describing symptoms of; A) RA: joint pain and stiffness in hands and wrists; B) RA: joint pain, stiffness and swelling in hands and wrists; C) RA: joint pain, stiffness and swelling in feet and ankles; D) bowel cancer; and E) angina. The order of these vignettes was fixed in the survey. For each vignette, respondents were asked to rate the seriousness of the symptoms and how quickly they would seek medical help (urgency) using 5-point Likert scales ranging from 1 (Very) to 5 (Not at all).
Respondents were also asked to describe what they thought might have caused the symptoms. These open ended answers were coded according to diagnosis by one coder and checked for accuracy by a second coder; discrepancies were discussed and resolved. These codes were subsequently classified as ‘correct’ (when the cause was identified correctly, e.g. RA, angina/ischaemic heart disease or bowel cancer); ‘approximate’ (when the given cause approximated the correct one, e.g. ‘arthritis’ instead of RA or ‘cancer’ instead of bowel cancer) and ‘incorrect’ (when either an incorrect cause was given (e.g. ‘water retention’) or when the participant indicated that they did not know the answer or left the question blank).
Coded causal attributions were described using percentage distributions and ratings were described using median values and interquartile ranges. Within group comparisons between conditions on the ratings for urgency and seriousness were conducted using nonparametric Friedman tests. Urgency ratings of those respondents who made a correct causal attribution were compared with those who made approximate and incorrect ones using a Kruskal-Wallis test. For both tests built-in post-hoc pairwise multiple comparisons were undertaken based on Dunn's approach with Bonferroni correction(26). Standardised z-values are reported with adjusted p-values. Spearman rank-order correlations were used to describe the relationship between the ratings of seriousness and urgency for each vignette.
Results
Symptom recognition: cause of the symptoms
In both studies participants were asked to assign a possible cause to the symptoms presented in the vignettes. Percentages of survey respondents giving correct, approximate and incorrect causes for each of the vignettes and illustrative interview quotes are shown in Table 1. Additional illustrative quotes can be found in Supplementary Table 4.
Table 1. Causal attribution for symptom vignettes.
Percentage of survey respondents who correctly identified the cause, supplemented with quotes from interviews.
| Vignette | Correctly identified cause % (N) | Approximately identified cause %, (N) | Incorrectly identified cause % (N) |
|---|---|---|---|
| A) RA with joint stiffness and pain | 14% (151) 1) “It’s all down the lines of rheumatics, isn’t it? But, … I’m no expert on rheumatics. I know it can be quite painful, and I know there’s different forms of rheumatics, rheumatoid arthritis, etc.” (p12) |
47% (513) 2) “I would say it sounds like you’d have arthritis…whether there’s any other underlying health problems, maybe, for some people. Maybe it’s part of something else. I’m not sure, really.”(p01) |
39% (424) 3) “Take it for granted it's either lazy bones or … old age really.” (p02) |
| B) RA with joint stiffness, pain and swelling wrists and hands | 16% (169) 4) “Well again I think that’s rheumatism or arthritis but probably at a more advanced stage and those symptoms could just be the start or … maybe just age related but that probably is the beginnings of one or the other, it looks slightly more serious than that.” (p03) |
33% (362) 5) “I’m not certain, actually. I’m not – I wouldn’t know the answer to that. I think any sort of bone aches and pains, you would quite quickly put down to arthritis and, … just age, but with the swelling and the sensitivity … I wouldn’t associate that immediately with arthritis.” (p01) |
51% (557) 6) “I don’t know. I wouldn’t know. Sorry, I’ve no idea.” (p06) |
| C) RA with joint stiffness, pain and swelling feet and ankles | 11% (117) 7) “No, it’s the same thing [arthritic or rheumatoid condition] really”. (p08) |
32% (357) 8) “Well, I know arthritis can – it can affect any joint, can’t it? I would want – as I say, I’d definitely want to get it sorted.” (p27) |
56% (614) |
| D) Bowel Cancer | 47% (515) 9) “Yes I think so, .. obviously it’s better to be safe than sorry … as I said my first impression would be probably bowel cancer …, there are other possibilities … there could be a blood disorder, there could be a lot of other possibilities” (p05) 10) “I’ve been, I’ve been sitting in hospitals, in waiting rooms, and I’ve seen big notices in front of me…saying, ‘If you see these things, see your doctor immediately,’ and it is to do with cancer of your stomach or bowel, that’s why” (p21). |
17% (178) 11) Okay, yeah. Well, hopefully you haven’t got cancer. Hopefully it’s, you know, piles or whatever, which can be treated (p06) |
36% (395) 12) I don’t know. I think I would assume I had a bug or something in my stomach (p26) |
| E) Angina | 32% (343) 13) “Well, it looks as though it might be angina or a heart attack. It’s probably angina, with tightness in the chest and shortness of breath.” (p18) |
32% (345) 14) “My initial thoughts are that I might have some heart trouble.” (p09) |
37% (400) 15) “I would think that the shortness of breath and the chest pain was asthma and the light headedness maybe like some kind of anaemia of something. If it was someone else, I would definitely tell them to get checked for diabetes because dizziness – that’s what I associate it with.” (p26) |
RA vignettes
In response to Vignette A (joint pain and stiffness in hands and wrists), interviewees often described ‘arthritis’, ‘old age’ and or ‘wear and tear’ as the likely cause of these symptoms, but were unable to specify a particular type of arthritis (Table 1, Quote 2 (T1Q2) and T1Q3). Frequently, interviewees would respond ‘I have got that’, apparently attributing these symptoms to other forms of arthritis, such as OA, or other causes of musculoskeletal symptoms which they themselves suffered from. Some interviewees did mention RA spontaneously (T1Q1). Others correctly indicated that the symptoms were related to an ‘autoimmune type of arthritis’, although this type of association was mainly made by interviewees with a medical background (see Supplementary Table 1).
For some interviewees, the inclusion of swelling alongside joint pain and stiffness (Vignette B) changed their perception of the possible underlying diagnosis or made them uncertain of the cause (T1Q5). Others saw the addition of swelling as reflecting a progression of the (rheumatoid) arthritis they had previously identified (T1Q4). Several interviewees freely admitted that they struggled to identify the cause (T1Q6).
When the interviewer described the symptoms as occurring in the ‘feet and ankles’, several interviewees recognised that the symptoms of many arthritides could occur in a wide range of joints (T1Q8) and mentioned that the cause of the symptoms was the same for both scenarios (T1Q7) although many still failed to recognise that these were the symptoms of RA.
Only 14% of survey respondents mentioned RA in response to ‘joint stiffness and pain in hands and wrists’, 15% mentioned RA when ‘joint swelling’ was added, and 11% recognised the symptoms as those of RA when they occurred in the ‘feet and ankles’ rather than in the ‘hands and wrists’ (Table 1). Large proportions of respondents approximately identified the cause by mentioning ‘arthritis’ including specific types of arthritis such as gout and OA or ‘inflammation’:48% for ‘joint stiffness and pain in hands and wrists’, 35% when ‘joint swelling’ was also included and 33% for symptoms in ‘feet and ankles’. The remaining respondents did not correctly identify the cause of the symptoms or gave no cause. Incorrect causal attributions included old age, wear and tear, injury, lack of exercise, inappropriate exercise and water retention.
Bowel cancer vignette
Although a few interviewees attributed the bowel symptoms to a minor ailment such as a ‘stomach bug’ (T1Q12), most interviewees identified the cause of these symptoms as bowel cancer (T1Q9) or cancer in general (T1Q11). Several interviewees indicated that they had heard about the symptoms of bowel cancer through the BCOC campaign(19) which had helped them recognise the cause of the symptoms described, their seriousness and the need for rapid help-seeking (T1Q10). Even those who did not name bowel cancer as a cause of the symptoms often mentioned that they knew urgent help was needed as a result of such a campaign. Others mentioned having being invited to send away a stool sample for testing as part of a screening programme (See also Supplementary Table 4).
Similarly, 47% of survey respondents correctly identified bowel cancer (Table 1), 18% approximately identified the cause (i.e. mentioned cancer or Crohn’s disease) and the remaining respondents either did not identify a cause or gave an incorrect cause such as haemorrhoids.
Angina vignette
Although the symptoms of angina were often recognised by the interviewees as related to ‘the heart’ or a ‘heart attack’ (T1Q14), fewer interviewees spontaneously labelled them as the symptoms of angina or ischaemic heart disease (T1Q13). Some interviewees indicated that the severity of the angina symptoms (i.e. the degree of pain/ tightness across the chest) would determine the perceived identity of the disease (i.e. whether they were due to angina or a myocardial infarction). A few interviewees suggested an underlying diagnosis unrelated to heart disease such as asthma (T1Q15).
32% of survey respondents correctly identified the symptoms as angina or a myocardial infarction. 32% approximately identified the cause, and the remaining respondents either gave no cause or an incorrect cause such as asthma or anxiety (Table 1).
Symptom recognition: Seriousness of the symptoms
Illustrative quotes referred to in the text can be found in Table 2 and further illustrative quotes can be found in Supplementary Table 4.
Table 2. Illustrative quotes from participant interviews (symptom seriousness & urgency).
| Quotes illustrating perceived seriousness of RA symptoms | |
|---|---|
| 1 | “Well, 65 plus, if it’s any younger than that, well then it, it’s even more, serious, if serious is the right word to use but something is wrong, and it’s not just, antiquity.” (p04) |
| 2 | “it doesn’t seem to me that this is (serious), this could possibly be, …. I wouldn’t say well that’s something that could be really bad it just sounds like something a lot of people have therefore it would have to be – it would have to be getting progressively worse for me to get medical attention” (p07) |
| Quotes illustrating perceived seriousness of bowel cancer symptoms | |
| 3 | “Well (if) I had blood in, in my toilet, I would think it’s serious” (p29) |
| 4 | “Oh well, …just like a tummy upset or something like that I would rule that out. It’s more serious than that if it’s ongoing. Particularly if I’ve … lost weight and there’s no change in my diet. And I’ve not been in contact with anybody who had an upset stomach” (p24) |
| Quotes illustrating perceived seriousness of angina symptoms | |
| 5 | “Well, I think if it’s your chest or your lungs or whatever, anyway, … it’s pretty serious anyway, isn’t it, …so it’s something that you don’t muck about with really, or it’s things for concern at the end of the day…” (p12). |
| Quotes illustrating perceived urgency of help-seeking for RA symptoms | |
| 6 | “That they (symptoms) are quite common, that they’re not debilitating, there seems to be a condition that you can live with, you should be able to manage quite easy.” (p07) |
| 7 | “I don’t think I would leave that for any, any length of time. If I saw that the joints were swollen I think… I would be concerned, and – I suppose you’d wait, initially, because …you may think, ‘Oh, well, it could have been…a knock’ or whatever it might be. But if you could see…there were various joints affected, then I would be, I think, making an appointment to see the GP (Family practitioner)…” (p11) |
| Quotes illustrating perceived urgency of help-seeking for bowel cancer symptoms | |
| 8 | “No if I saw that this morning I’d be banging on the doctors door.” (p07) |
| 9 | “Well if I notice it for a few days I will go to my GP (Family practitioner) because… it’s, obviously if I want to take my weight that might take me a few weeks to notice change in my …..but if I’m feeling tired, run down, lethargic and there’s a change in my bowel habit with blood in my stool I probably would not wait for the weight loss, I probably would go say look something is going on here, I don’t know what it is” (p05). |
| Quotes illustrating perceived urgency of help-seeking for angina symptoms | |
| 10 | “Well if it was severe I’d pick up the phone and dial 999 or ask somebody else to do it if it was really, really severe, but … I would sort of basically take it easy, I’d sort of relax, put my feet up and sort of monitor the situation … to see how it is, does it seem a little bit better or does it seem it’s …just as bad.” (p14) |
| 11 | “Well it depends as I say how many times, I think probably give it a month maybe, unless they were coming regularly not just a one off every now and again you might put it down to something else.” (p03) |
| Quote illustrating comparison of urgency across conditions | |
| 12 | “So it could have been a month. It could be two months with it (RA Symptoms) …. I don’t think I’d be as quick going as what I would with those...With the cancer and...the heart and the other one. No, I wouldn’t, I wouldn’t be as quick going (with RA symptoms). This would probably – what – about two or three months, I suppose before you’d really … Just how long you could stand the pain for.” (p10) |
P04 refers to participant 4in the interview study
RA vignettes
The perceived seriousness of the symptoms of RA varied considerably amongst interviewees and was often dependent on the causal attribution (i.e. some types of arthritis were considered to be more serious than others). Some felt that joint pain and stiffness was more serious if experienced in younger people (Table 2, Quote 1; T2Q1). Others did not think the symptoms were serious and intended to only take action if symptoms worsened (T2Q2). Many saw the combination of ‘joint pain, swelling and stiffness’ as more serious than ‘joint pain and stiffness’. A sudden onset of symptoms (as opposed to an insidious onset) and having multiple symptomatic joints (as opposed to a single joint) were identified as factors indicative of a more serious underlying diagnosis.
Bowel cancer vignette
Interviewees often referred to the occurrence of blood in the stool as a serious symptom (T2Q3). Perceived seriousness was increased if this symptom occurred on multiple occasions (T2Q4).
Angina vignette
Most interviewees saw the symptoms of angina as being serious and requiring urgent action (T2Q5). Perceived seriousness was also associated with the frequency with which symptoms occurred.
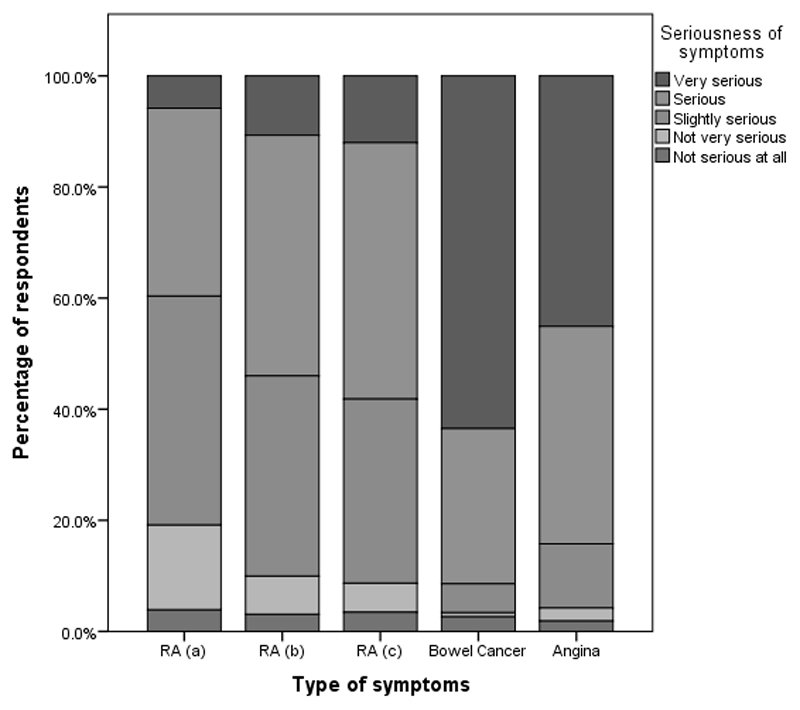
Comparison of seriousness ratings across conditions
Figure 1 illustrates how survey respondents rated the seriousness of each symptom vignette (From ‘not serious at all’ to ‘very serious’). There was a significant difference between rankings for the various vignettes (=2034, p < 0.001). Post-hoc comparisons showed that respondents rated bowel cancer and angina symptoms to be significantly more serious than any of the three combinations of RA symptoms (Z values of 16.3 to 25.3, all p<.001). They also rated the RA vignette with ‘joint pain and stiffness in hands and wrists’ as significantly less serious than either ‘joint pain, stiffness and swelling in hands and wrists’ (Z=9.02, p<.001) or symptoms in the ‘feet and ankles’ (Z=7.75, p<.001). Ratings for the latter two vignettes (hands vs feet) did not differ significantly (Z=1.27, p=1.00). Table 3 gives descriptive statistics for seriousness ratings for each vignette.
Figure 1. Distribution of ratings of seriousness of the symptoms of RA joint pain and joint stiffness in hands and wrists.
(a), RA joint pain, stiffness and swelling in hands and wrists (b), RA joint pain, stiffness and swelling in the feet and ankles (c), bowel cancer and angina by survey respondents
Table 3. Seriousness and urgency ratings.
Median (Interquartile range (IQR)) values shown. Lower scores indicate greater levels of seriousness and urgency.
| Vignette | Rating of | Median (IQR) |
|---|---|---|
| A) Joint stiffness and pain wrists and hands | Seriousness | 3 (1) |
| Urgency | 3 (2) | |
| B) Joint stiffness, pain and swelling wrists and hands | Seriousness | 2 (1) |
| Urgency | 3 (1) | |
| C) Joint stiffness, pain and swelling feet and ankles | Seriousness | 2 (1) |
| Urgency | 2 (1) | |
| D) Bowel cancer | Seriousness | 1 (1) |
| Urgency | 1 (1) | |
| E) Angina | Seriousness | 2 (1) |
| Urgency | 2 (1) |
Perceived urgency of help-seeking
Illustrative quotes referred to in the text can be found in Table 2 and further illustrative quotes can be found in Supplementary Table 4.
RA vignettes
The symptoms of RA described in the vignettes were generally not seen as urgent, and many interviewees indicated that their intention would be to wait for at least a few weeks and up to several months before seeking medical attention. Some interviewees felt that they would be able to live with the symptoms and medical attention was not necessary at all (T2Q6). When swelling was included in the vignette, or when symptoms were described by the interviewer as occurring in multiple joints some interviewees indicated that their intention would be to seek help more urgently (T2Q7). Others felt that in certain circumstances, for example when there was a sudden onset of symptoms, their intention would be to seek help immediately, perhaps making an emergency appointment at their doctors or going to the emergency room.
Bowel cancer vignette
Most interviewees felt that the symptoms of bowel cancer would warrant a visit to the family practitioner within a few days of symptom onset, whereas some indicated their intention to see their doctor immediately (T2Q8). However, none felt that emergency medical attention (e.g. a visit to the A&E department) would be necessary. Interviewees generally reported that they would not wait for weight loss to occur, or let the symptoms persist for a month (as the text in the vignette suggested) before seeking help (T2Q9).
Angina vignette
Interviewees reported the intention to seek help urgently for the symptoms of angina, with several considering contacting the emergency services. Many indicated that their actions would depend on the severity of the symptoms (T2Q10). Some people reported that they would live with the symptoms for as long as the frequency of the attacks or severity of the symptoms would allow them to do so (T2Q11).
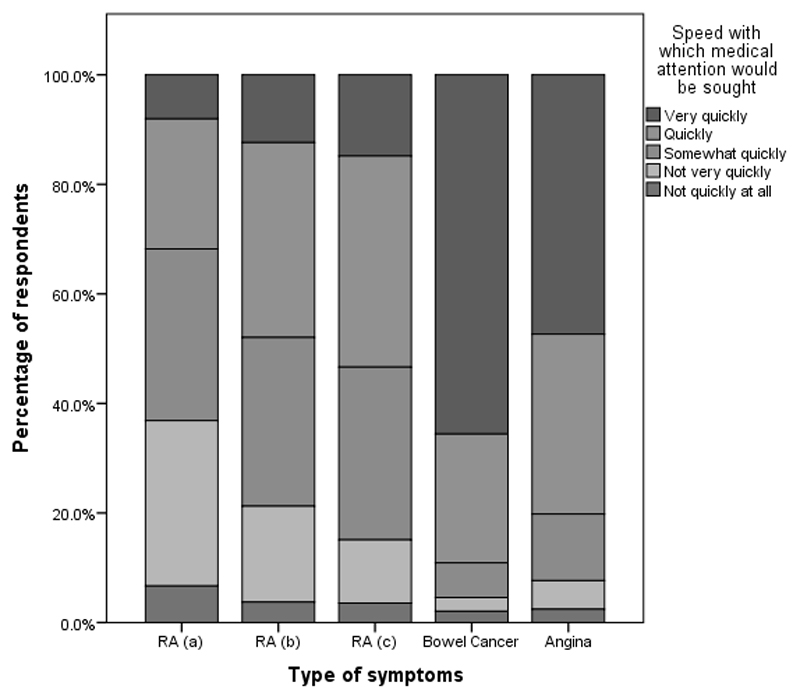
Comparison across vignettes of survey urgency ratings
Several interviewees spontaneously reported the intention to wait far longer with the symptoms of RA compared to the other scenarios before seeking medical attention (T2Q12). The differences between conditions found in the interviews are consistent with the survey results. Figure 2 illustrates the distribution of respondents’ ratings of how quickly they would seek help for each vignette. A significant difference among the ratings for the 5 vignettes was found ( = 2106, p<.001). Survey respondents would seek medical attention significantly more quickly for bowel cancer and angina symptoms than they would for any of the given combinations of RA symptoms (Z values of 14.7 to 34.2, all p<.001). Respondents rated ‘joint pain and stiffness in hands and wrists’ as significantly less urgent compared to either ‘joint pain, stiffness and swelling in hands and wrists’ (Z = 9.3, p<.001,) or symptoms in the ‘feet and ankles’ (Z = 12.5, p<.001). Ratings of the latter two vignettes (hands and wrists vs feet and ankles) also differed significantly (Z = 3.2, p <.05) (see Table 3 for descriptive statistics).
Figure 2. Distribution of ratings of the urgency with which medical attention would be sought for the symptoms of RA joint pain and joint stiffness in hands and wrists.
(a), RA joint pain, stiffness and swelling in hands and wrists (b), RA joint pain, stiffness and swelling in the feet and ankles (c), Bowel Cancer and Angina by survey respondents.
Impact of correct causal attribution on the urgency with which help would be sought
Symptom recognition had a significant impact on the urgency with which survey respondents intended to seek help (Table 4). For all vignettes except for the RA one with ankle and foot involvement, having correct knowledge of the cause of symptoms was associated with significantly higher ratings of perceived urgency compared to incorrect causal attributions. For all vignettes, except for RA with ‘joint pain, stiffness and swelling in the hands and wrists’ and RA with symptoms in the ‘ankles and feet’, having approximate knowledge of the cause was also associated with significantly higher ratings of perceived urgency compared to incorrect causal attributions. These differences where highly significant for both bowel cancer and angina vignettes (p<.001). For the former vignette, there was also a statistically significant difference between urgency ratings for the groups who correctly identify the cause and those who approximated the cause (p<.001).
Table 4. Impact of correct causal attribution on the urgency with which help would be sought.
| Vignette | Kruskal-Wallis Test | 2-way comparison | Dunn’s Test, (Z, p-adj) |
|---|---|---|---|
| A) Joint stiffness and pain | 8.12, 0.02 | Correct vs. Approximate | -0.97,0.99 |
| Approximate vs. Incorrect | 2.23, 0.08 | ||
| Correct vs. Incorrect | 2.49, 0.04 | ||
| B) Joint stiffness, pain and swelling wrists and hands | 6.18, 0.04 | Correct vs. Approximate | -1.57,0.35 |
| Approximate vs. Incorrect | 1.08, 0.84 | ||
| Correct vs. Incorrect | 2.46, 0.04 | ||
| C) Joint stiffness, pain and swelling feet and ankles | 0.70, 0.70 | Correct vs. Approximate | n/a |
| Approximate vs. Incorrect | n/a | ||
| Correct vs. Incorrect | n/a | ||
| D) Bowel Cancer | 81.05, <.001 | Correct vs. Approximate | -2.56,0.03 |
| Approximate vs. Incorrect | 4.50,<.001 | ||
| Correct vs. Incorrect | 8.99,<.001 | ||
| E) Angina | 76.11, <.001 | Correct vs. Approximate | -0.69, 1.0 |
| Approximate vs. Incorrect | 7.11,<.001 | ||
| Correct vs. Incorrect | 7.82,<.001 | ||
Rank-based nonparametric Kruskal-Wallis Test was used to determine if there were significant differences in speed with which help would be sought between groupings of causal attributions; two-way comparisons were subsequently used to directly compare correct attribution with approximate and incorrect attributions. A Bonferroni adjustment has been applied to the p-adj values for the pairwise comparisons.
Impact of seriousness rating on urgency of help-seeking
For all vignettes there was a statistically significant (p<.001) Spearman rank order correlation between ratings of seriousness and urgency. The more serious the symptoms were perceived to be, the more quickly help would be sought.
For the ‘joint pain and stiffness’ vignette, the correlation between seriousness and urgency ratings was 0.729; when ‘swelling’ was added it was 0.811 and for symptoms in ‘feet and ankles’ 0.825. The correlations for bowel cancer and angina were 0.846 and 0.882 respectively.
Discussion
Pelaez and colleagues suggest three trajectories of help-seeking that RA patients might follow depending on whether symptom onset is rapid, oscillating or slow. Oscillating and slow onsets are associated with delayed help-seeking, and help-seeking from non-medical sources, such as social networks(16). The fact that help-seeking would be delayed with slow onset of symptoms is worrying as only a minority of RA patients have an acute onset of symptoms(27). In this study we have sought to understand determinants of the speed of help-seeking in the context of RA in relation to two other common and serious diseases.
Both the interview and survey data showed marked differences between symptom recognition for angina, bowel cancer and RA. Participants were less likely to recognise the symptoms of RA and often assigned these symptoms to less serious or non-modifiable (e.g. ‘old age’) causes. This effect was more pronounced when the symptoms did not include joint swelling. In contrast, the symptoms of bowel cancer and angina were more readily recognised and were considered to be more serious than those of RA with respondents reporting the intention to seek help faster. Correct and approximate causal attributions of symptoms had most effect on perceived urgency of help-seeking for the angina and bowel cancer vignettes. There was a significant correlation between urgency and seriousness ratings for all vignettes, however the correlation for the RA vignettes was slightly lower than for angina or bowel cancer.
As predicted, the interview and survey data show that, accurate symptom recognition and perceived seriousness are associated with the intention to seek help urgently. This was the case for all the symptom vignettes, although the correlations between the urgency and serious ratings were lowest for the RA vignettes. Furthermore, the causal attribution did not have such a clear-cut effect on the urgency of seeking medical attention for RA symptoms compared to bowel cancer and angina. Potential explanations in the context of the RA vignettes are that people may feel that little can be done for these symptoms or that speed is not required despite perceived seriousness due to a perception that the symptoms will not progress rapidly.
The interview data further suggest that specific features related to the onset of RA symptoms (e.g. sudden vs slow; widespread vs localised symptoms) impact on how serious they are considered to be and how urgently help would be sought (e.g. Supplementary Table 4, quote 14). This is consistent with the survey data and with previous research(16;17).
Previous research has shown that health campaigns can aid symptom recognition and increase appropriate help-seeking(19;28). A number of our interviewees spontaneously mentioned having seen the BCOC campaign for bowel cancer and correctly identified the symptoms described in the vignette (see also Supplementary Table 4, quotes 9 and 10).
The current research has a number of limitations. Firstly, as with most biomedical research, only those individuals who consented to participate were included. Research has shown that people take part in health research for a variety of reasons including altruism and a desire to gain more information about the research topic(29). These motivations may influence the types of participant and their responses. For example, the large proportion of participants reporting joint problems themselves might be indicative of a motivation to find out more about arthritis. Secondly, few participants from ethnic minority backgrounds chose to participate. It is well recognized that ethnic minority groups are often under-represented in health studies(30;31). Future research should explore the views of minority groups in the context of the research questions addressed in this paper. Thirdly although in the interviews the ordering of the vignettes was alternated, this was not done in the survey which had a single format. There is the potential that having the RA vignettes first in the survey influenced the subsequent ratings for the non-RA vignettes. Finally, the hypothetical approach taken within these studies (participants were asked to imagine what they would do when encountering certain symptoms) is both a strength and a weakness. Asking members of the general public to react to a number of potential scenarios is as close as we can reasonably get to the experiences of patients who have just started to experience symptoms. This latter group is difficult to access precisely for the reason which inspired the current research; particularly patients with joint symptoms rarely see their GP within weeks of symptom onset(17). Studying intentions is valuable where it is difficult to access actual behavior. However, whether participants’ intended behaviours would translate into actual behaviour if they were ever confronted with any of the symptoms in ‘real life’ depends on many factors including perceived control over situation (32). It was not possible to measure these factors with the current research design.
Our findings extend those previously identified(17;33) and themes found in the qualitative data from the interviews were quantified and supported through the findings of the survey. Although the response rate for the survey was relatively low, the consistency between the quantitative data and the interview data are a good indication that the combined findings reflect the perceptions of the wider general public.
The evidence presented here demonstrates that the general public are less likely to make a correct causal attribution for the symptoms of RA, and less likely to perceive RA symptoms to be serious and to require urgent help compared with other common and serious conditions. This highlights a need to raise awareness about the symptoms of RA, the potential negative impact of RA on quality of life, and the importance of early help-seeking(5;7–10).
Supplementary Material
Significance and Innovations.
Members of the general public in the UK were less likely to make an accurate causal attribution for the symptoms of RA compared to the symptoms of bowel cancer or angina. The general public further perceived RA to be less serious and less urgent than other conditions.
Correct causal attribution had a positive impact on the urgency with which people intended to seek medical attention.
The findings highlight a need to raise public awareness not only about the symptoms of RA but also the need for prompt treatment, and thus the importance of early help-seeking.
Acknowledgments
This research is supported by The Dunhill Medical Trust (grant number R226/1111). The authors also wish to acknowledge the support of the National Institute for Health Research, through the Primary Care Research Network. CDM is funded by the National Institute for Health Research (NIHR) Collaborations for Leadership in Applied Health Research and Care West Midlands, the NIHR School for Primary Care Research and a NIHR Research Professorship in General Practice (NIHR-RP-2014-04-026). The views expressed are those of the author(s) and not necessarily those of the NHS, the NIHR or the Department of Health. The authors would also like to thank the interviewees, survey respondents and the patient research partners who have been involved in the development of the research.
Reference List
- 1.Symmons D, Turner G, Webb R, Asten P, Barrett E, Lunt M, Scott D, Silman A. The prevalence of rheumatoid arthritis in the United Kingdom: new estimates for a new century. Rheumatology (Oxford) 2002;41(7):793–800. doi: 10.1093/rheumatology/41.7.793. [DOI] [PubMed] [Google Scholar]
- 2.Feldman D, Bernatsky S, Beauchamp ME, Abrahamowicz M. Early consultation with a rheumatologist for RA: does it reduce subsequent use of orthopaedic surgery? Rheumatology (Oxford) 2013;52(3):452–9. doi: 10.1093/rheumatology/kes231. [DOI] [PubMed] [Google Scholar]
- 3.Nell V, Machold KP, Eberl G, Stamm T, Uffmann M, Smolen JS. Benefit of very early referral and very early therapy with disease-modifying anti-rheumatic drugs in patients with early rheumatoid arthritis. Rheumatology. 2004;43(7):906–14. doi: 10.1093/rheumatology/keh199. [DOI] [PubMed] [Google Scholar]
- 4.Raza K, Buckley CE, Salmon M, Buckley CD. Treating very early rheumatoid arthritis. Best Pract Res Clin Rheumatol. 2006;20(5):849–63. doi: 10.1016/j.berh.2006.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Raza K, Filer A. The therapeutic window of opportunity in rheumatoid arthritis: does it ever close? Ann Rheum Dis. 2015;74(5):793–4. doi: 10.1136/annrheumdis-2014-206993. [DOI] [PubMed] [Google Scholar]
- 6.Scott D, Hunter J, Deighton C, Scott D, Isenberg D. Treatment of rheumatoid arthritis is good medicine. BMJ. 2011;343(d6962) doi: 10.1136/bmj.d6962. [DOI] [PubMed] [Google Scholar]
- 7.van der Linden M, le Cessie S, Raza K, van der Woude D, Knevel R, Huizinga T, van der Helm-van Mil AH. Long-term impact of delay in assessment of early arthritis patients. Arthritis Rheum. 2010;62(12):3537–46. doi: 10.1002/art.27692. [DOI] [PubMed] [Google Scholar]
- 8.Feldman D, Bernatsky S, Haggerty J, Leffondre K, Tousignant P, et al. Delay in consultation with specialists for persons with suspected new-onset rheumatoid arthritis: a population-based study. Arthritis Rheum. 2007;57(8):1419–25. doi: 10.1002/art.23086. [DOI] [PubMed] [Google Scholar]
- 9.Kiely P, Williams R, Walsh D, Young A. Contemporary patterns of care and disease activity outcome in early rheumatoid arthritis: the ERAN cohort. Rheumatology. 2009;48(1):57–60. doi: 10.1093/rheumatology/ken406. [DOI] [PubMed] [Google Scholar]
- 10.Kumar K, Daley E, Carruthers D, Situnayake D, Gordon C, Grindulis K, et al. Delay in presentation to primary care physicians is the main reason why patients with rheumatoid arthritis are seen late by rheumatologists. Rheumatology. 2007;46(9):1438–40. doi: 10.1093/rheumatology/kem130. [DOI] [PubMed] [Google Scholar]
- 11.Stack RJ, Simons G, Kumar K, Mallen CD, Raza K. Patient delays in seeking help at the onset of rheumatoid arthritis: the problem, its causes and potential solutions. Aging Health. 2013;9(4):425–35. [Google Scholar]
- 12.Andersen BL, Cacioppo J, Roberts DC. Delay in seeking cancer diagnosis: delay stages and psychophysiological comparison processes. Br J Soc Psychol. 1995;34:33–52. doi: 10.1111/j.2044-8309.1995.tb01047.x. [DOI] [PubMed] [Google Scholar]
- 13.de Nooijer J, Lechner L, de Vries H. A qualitative study on detecting cancer symptoms and seeking medical help; an application of Andersen's model of total patient delay. Patient Educ Couns. 2001;42:145–57. doi: 10.1016/s0738-3991(00)00104-x. [DOI] [PubMed] [Google Scholar]
- 14.Safer M, Tharps QJ, Jackson BA, Leventhal H. Determinants of three stages of delay in seeking care at a medical clinic. Med Care. 1979;17:11–29. doi: 10.1097/00005650-197901000-00002. [DOI] [PubMed] [Google Scholar]
- 15.Unger-Saldaña K, Infante-Castañeda CB. Breast cancer delay: A grounded model of help-seeking behaviour. Soc Sci Med. 2011;72(7):1096–104. doi: 10.1016/j.socscimed.2011.01.022. [DOI] [PubMed] [Google Scholar]
- 16.Pelaez I, Infante C, Quintana R. Help-seeking trajectory in patients with rheumatoid arthritis. Clin Rheumatol. 2015;34(suppl 1):17–28. doi: 10.1007/s10067-015-3013-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Simons G, Mallen CD, Kumar K, Stack RJ, Raza K. A qualitative investigation of the barriers to help-seeking among members of the public presented with symptoms of new-onset rheumatoid arthritis. J Rheumatol. 2015;42(4):585–92. doi: 10.3899/jrheum.140913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Stack RJ, Shaw K, Mallen C, Herron-Marx S, Horne R, Raza K. Delays in help seeking at the onset of the symptoms of rheumatoid arthritis: a systematic synthesis of qualitative literature. Ann Rheum Dis. 2012 Apr;71(4):493–7. doi: 10.1136/ard.2011.155416. [DOI] [PubMed] [Google Scholar]
- 19.Moffat J, Bentley A, Ironmonger L, Boughey A, Radford G, Duffy S. The impact of national cancer awareness campaigns for bowel and lung cancer symptoms on sociodemographic inequalities in immediate key symptom awareness and GP attendances. Br J Cancer. 2015;112:14–21. doi: 10.1038/bjc.2015.31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Power E, Wardle J. Change in public awareness of symptoms and perceived barriers to seeing a doctor following Be Clear on Cancer campaigns in England. Br J Cancer. 2015;112:22–6. doi: 10.1038/bjc.2015.32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Pande R, Leung E, McCullough P, Smith S, Harmston C. Impact of the United kingdom national bowel cancer awareness campaign on colorectal services. Dis Colon Rectum. 2014 Jan;57(1):70–5. doi: 10.1097/01.dcr.0000437689.19579.97. [DOI] [PubMed] [Google Scholar]
- 22.British Heart Foundation. British Heart Foundation. 2016 https://www.bhf.org.uk/
- 23.Hardwick CCG. CCG pilots Rheumatoid Arthirits Campaign. Jan 28; http://www.hardwickccg.nhs.uk/news/2015/ccg-pilots-rheumatoid-arthritis-campaign/2015.
- 24.Morse A. London: National Audit Office; 2009. Services for people with rheumatoid arthritis. [Google Scholar]
- 25.Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3:77–101. [Google Scholar]
- 26.Dunn OJ. Multiple Comparisons Using Rank Sums. Technometrics. 1964;6:241–52. [Google Scholar]
- 27.Rindfleisch JA, Muller D. Diagnosis and Management of Rheumatoid Arthritis. Am Fam Physician. 2005;72(6):1037–47. [PubMed] [Google Scholar]
- 28.Hughes-Hallett A, Browne D, Mensah E, Vale J, Mayer E. Assessing the impact of mass media public health campaigns: 'Be Clear on Cancer: Blood in pee' a case in point. BJU Int. 2016;117(4):570–5. doi: 10.1111/bju.13205. [DOI] [PubMed] [Google Scholar]
- 29.Townsend A, Backman CL, Adam P, Li LC. A qualitative interview study: patient accounts of medication use in early rheumatoid arthritis from symptom onset to early postdiagnosis. British Medical Journal Open. 2013;3(2) doi: 10.1136/bmjopen-2012-002164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Redwood S, Gill PS. Under-representation of minority ethnic groups in research--call for action. Br J Gen Pract. 2013;63(612):342–3. doi: 10.3399/bjgp13X668456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Macneill V, Nwokoro C, Griffiths C, Grigg J, Seale C. Recruiting ethnic minority participants to a clinical trial: a qualitative study. British Medical Journal Open. 2013;3(4) doi: 10.1136/bmjopen-2013-002750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ajzen I. The theory of planned behavior. Organ Behav Hum Decis Process. 1991;50:179–211. [Google Scholar]
- 33.Simons G, Mason A, Falahee M, Kumar K, Mallen CD, Raza K, Stack RJ. Qualitative Exploration of Illness Perceptions of Rheumatoid Arthritis in the General Public. Musculoskelet Care. 2016 Feb 1; doi: 10.1002/msc.1135. n/a. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.