Abstract
Background
The benefits of work for physical, psychological, and financial wellbeing are well documented. Return to work (RTW) after unintentional injury is often delayed, and psychological morbidity may contribute to this delay. The impact of psychological morbidity on RTW after a wide range of unintentional injuries in the UK has not been adequately quantified.
Aim
To quantify the role of psychological factors, including anxiety, depression, and post-traumatic distress, on RTW following unintentional injuries.
Design and setting
A longitudinal multicentre prospective study was undertaken in Nottingham, Bristol, Leicester, and Guildford, UK.
Method
Participants (n = 273) were 16–69-year-olds admitted to hospital following unintentional injury, who were in paid employment prior to injury. They were surveyed at baseline, then at 1, 2, 4, and 12 months following injury; demographic data were collected along with injury characteristics, psychological morbidity, and RTW status. Associations between demographic, injury and psychological factors, and RTW between 2 and 12 months after injury were quantified using random effects logistic regression.
Results
The odds of RTW between 2 and 12 months after injury reduced as depression scores early in the recovery period (1 month after injury) increased (odds ratio [OR] 0.87, 95% confidence interval [CI] = 0.79 to 0.95) and as length of hospital stay increased (OR 0.91, 95% CI] = 0.86 to 0.96). For those experiencing threatening life events following injury (OR 0.27, 95% CI = 0.10 to 0.72) and with higher scores on the Crisis Support Scale (OR 0.93, 95% CI] = 0.88 to 0.99), the odds of RTW between 2 and 12 months after injury were lower. Multiple imputation analysis found similar results, but those relating to crisis support did not remain statistically significant.
Conclusion
Primary care professionals can identify patients at risk of delayed RTW who may benefit from management of psychological morbidity and support to RTW.
Keywords: cohort study, injuries, mental health, psychological factors, work
INTRODUCTION
Being in work benefits physical and mental health,1 while being out of work can have negative financial, physical, and psychological consequences.2 The importance of identifying modifiable factors that, if addressed, may help individuals to remain in work was highlighted by the 2008 report, Working for a Healthier Tomorrow.2
In England in 2014–2015, 319 000 adults aged 16–69 years were admitted to hospital with traumatic injuries or poisoning (external cause codes V01–X59).3 The annual NHS costs of care in the first 12 months after such injuries has recently been estimated at £1.53 billion.4 Hospital-treated injuries result in substantial health-related work absence, with 17% of emergency department attenders and 43% of people admitted to hospital not having returned to work 4 months post-injury.5 Injuries also account for 10% of sick notes in the UK2 and 14% of benefit claimants.6
Depression,7–11 anxiety,12 and post-traumatic stress disorder (PTSD)13 are common after traumatic injury; for example, a review focusing on road traffic injuries estimated that, at 1 year, prevalence ranged from 21–67% for depression, 4–87% for anxiety, and 0–100% for PTSD.14 These conditions have a negative impact on an individual’s ability to return to work (RTW);8,13,15–20 this has been illustrated in a study by Ching et al, who found that fewer patients with depression (52%) or PTSD (47%) were working 6 months after injury than those without depression (73%) or PTSD (78%).20
As depression, anxiety, and PTSD are detectable and treatable, it is important to quantify their impact on RTW among injured working-age adults in the UK. This article reports the findings on psychological morbidity and RTW from the Impact of Injuries Study, to inform the identification and management of these diagnoses post-injury in primary care and in other services, such as occupational health.
METHOD
Elements of the study method are outlined below; a full description is available in the published protocol.21
Study design
This research involved a multicentre longitudinal cohort study undertaken in four NHS acute hospital trusts with emergency departments in Nottingham, Bristol, Leicester, and Guildford, UK. These sites were chosen due to their having prior experience of recruiting to similar studies.
How this fits in
Injuries are common in working-age adults, resulting in a delayed return to work (RTW) for many. This is of concern as the benefits of work for physical, psychological, and financial wellbeing are well documented. Depression that occurs early in the recovery period, threatening life events after the injury, and a longer stay in hospital significantly reduce the odds of RTW between 2 and 12 months after injury. Primary care professionals can identify patients at risk of delayed RTW, detect and manage psychological morbidity, and provide RTW support.
Participants
Participants were recruited from June 2010 until June 2012 within 3 weeks of hospital admission for unintentional injury. Those aged 16–70 years with a fixed address (to enable follow-up) were eligible. Those with loss of consciousness, amnesia, or a Glasgow Coma Scale score of <15 at presentation were excluded due to difficulty distinguishing between head injury sequelae and psychological morbidity.22
Participants were recruited face to face and by post. Quota sampling by injury type was used from June 2010 until May 2011; subsequently, due to slow recruitment, all eligible patients could participate.
The sample for this analysis comprised participants who were in paid employment at baseline, and returned the 1-month questionnaire and at least one subsequent follow-up questionnaire (at 2, 4, or 12 months).
Data collection
Participants completed self-administered questionnaires at recruitment (baseline) and at 1, 2, 4, and 12 months post-injury. Baseline questionnaires assessed:
sociodemographic characteristics (age, marital status, ethnicity, employment status, and area-level deprivation based on the 2010 indices of multiple deprivation);23
injury details;
long-term health conditions (longstanding illness, past psychiatric diagnoses, and pain);
anxiety and depression;24
alcohol problems;25
substance use;26 and
social functioning.27
Injury severity was assessed from medical records based on the most severe injury for participants with multiple injuries, and using the Abbreviated Injury Scale (AIS).28 The following categories were used:
minor (AIS score: 1);
moderate (AIS score: 2); and
serious or worse (AIS score: ≥3–6).
Follow-up questionnaires included questions on:
time off work since injury;
self-reported recovery;29
post-traumatic distress;30
threatening life events related to the injury;31
social support;32
positive and negative changes in outlook;33 and
legal proceedings or compensation claims due to injury.
More information about the scale that was used to measure each variable is given in Table 1.
Table 1.
Description and reliability scores of scales used
| Variable | Scale | Description | Cronbach’s α | |
|---|---|---|---|---|
| Items, n | Score | |||
| Anxiety and depression | Hospital Anxiety and Depression Scale | 14: 7 depression, 7 anxiety | 0–21 for each subscale (higher scores indicate higher severity of anxiety and depression) | 0.80 (anxiety) 0.70 (depression) 0.83 (overall) |
| Alcohol problems | Alcohol Use Disorders Identification Test |
10 | 0–40 (higher scores indicate higher levels of excessive or harmful drinking) | 0.79 |
| Substance use | Drug Abuse Screening Test | 10 | 0–10 (higher scores indicate higher levels of abuse of substances other than alcohol) | 0.67 |
| Social functioning | Social Functioning Questionnaire |
8 | 0–24 (higher scores indicate greater social dysfunction) | 0.72 |
| Post-traumatic distress | Impact of Events Scale | 15: 7 on intrusion, 8 on avoidance symptoms | 0–75 (higher scores indicate greater severity of post-traumatic symptoms) | 0.89 (intrusion) 0.84 (avoidance) 0.92 (overall) |
| Social support | Crisis Support Scale | 6 | 6–42 (higher scores indicate higher social support) | 0.76 |
| Positive and negative changes in outlook | Changes in Outlook Questionnaire |
10: 5 on positive change, 5 on negative change | 5–30 for each subscale (higher scores indicate respective greater positive and negative changes) | 0.78 (negative) 0.87 (positive) |
Researchers administered structured clinical interviews34 to measure psychological morbidity for all participants at baseline.
Outcomes
The primary outcome was whether a participant reported returning to work. This was a binary outcome at each time point (1, 2, 4, and 12 months post-injury). RTW was defined as being in full- or part-time paid employment, working at the specific time point, and not being prevented from working since the previous follow-up because of the injury sustained.
Statistical analyses
Baseline characteristics were described and compared between the sample described above (responders) and those employed at baseline who returned the 1-month questionnaire only (non-responders). Categorical data were compared using χ2 tests, and continuous data using t-tests or Mann–Whitney U tests, dependent on distributions.
Proportions of participants who had returned to work were calculated, and an RTW trajectory was developed.35 Non-responders and those with missing RTW data were categorised as ‘unknown’.
Univariate and multivariable odds ratios (ORs) with 95% confidence intervals (CIs) were estimated for RTW using random effects logistic regression to account for repeated measures of RTW at 2, 4, and 12 months. Linearity of continuous predictors was assessed, and non-linear predictors were categorised into quintiles. Models were built using predictors described in Box 1.
Box 1. Predictors and potential predictors of return to work included in multivariable model building.
|
Block 1 (a-priori predictors) Age, sex, study centre, and time |
|
Block 2 (psychological predictors at 1 month) HADS-A, HADS-D, IES-A, IES-I, AUDIT and DAST |
|
Block 3 (potential predictors at baseline) Number of past psychiatric diagnoses, HADS-A, HADS-D, AUDIT, DAST, longstanding illness, work status, ethnicity, deprivation, marital status, length of hospital stay, injury characteristics (severity, number, body part, mechanism, and location) |
|
Block 4 (potential predictors at 1 month) Social functioning, social support, changes in outlook (positive and negative), threatening life events since injury, pain visual analogue scale, compensation, and litigation |
AUDIT = Alcohol Use Disorders Identification Test. DAST = Drug Abuse Screening Test. HADS-A = Hospital Anxiety and Depression Scale — anxiety. HADS-D = Hospital Anxiety and Depression Scale — depression. IES-A = Impact of Events Scale avoidance. Impact of Events Scale-I = IES intrusion.
Block 2 psychological predictors at 1 month were added to Block 1 in order of statistical significance on univariate analysis, and retained if the likelihood ratio test (LRT) P-value was <0.05. Correlations between predictors in Blocks 3 and 4 with psychological predictors of Block 2 were assessed. Those with correlation coefficients of ≥0.5 or ≤−0.5 were excluded from the analysis.
Block 3 predictors were added and retained in the model if the LRT was P<0.05 or if their removal resulted in a >10% change in the 1-month psychological predictor OR. Block 4 predictors were added and retained as for Block 3. Interactions between psychological predictors at 1 month and age, sex, and follow-up time were assessed based on an LRT P-value of <0.01.
Collinearity was assessed by the covariance correlation matrix and variance inflation factors. Model assumptions were checked using deviance residuals. Multiple imputation with chained equations was used to impute missing data for all participants employed at baseline. The imputation model included all predictors in the univariate analysis and the outcome (RTW at 2, 4, and 12 months). Ten datasets were created and combined using Rubin’s rules.36,37
RESULTS
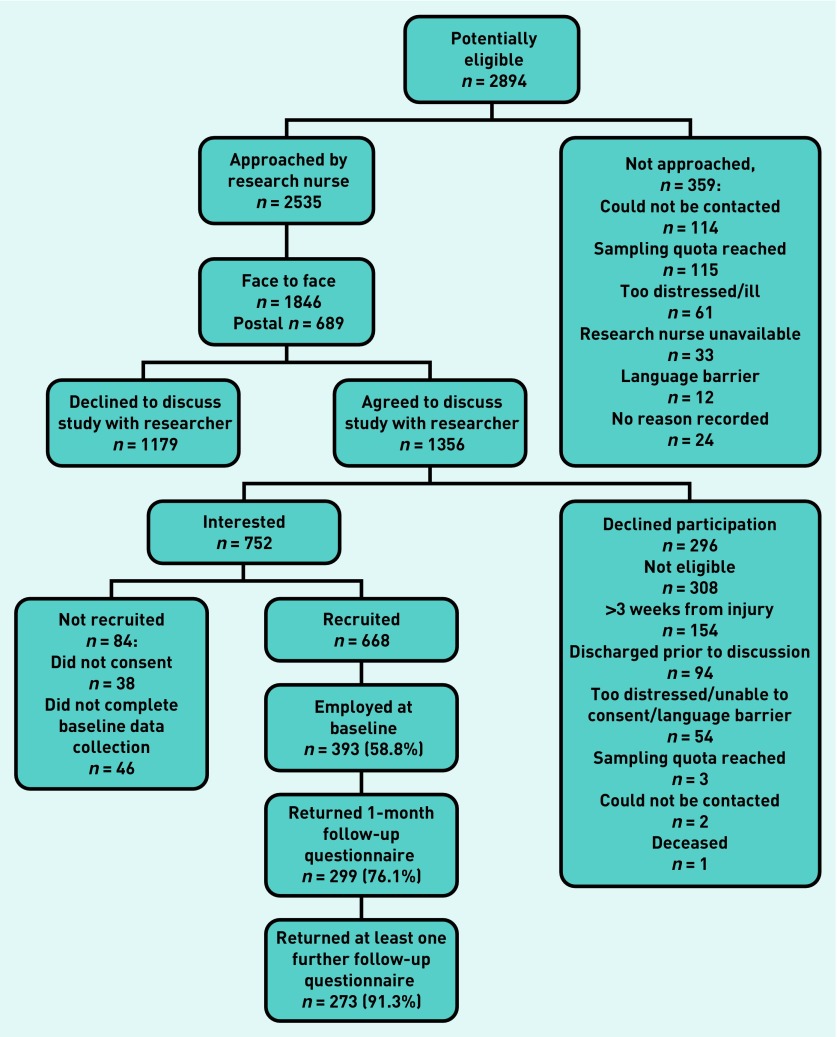
Figure 1 shows the flow of participants in the Impact of Injury Study. Almost three-fifths (n = 393, 58.8%) of the total 668 study participants were employed at the time of injury. Of these, 299 (76.1%) returned the 1-month follow-up questionnaire and 273 (91.3%) also returned at least one subsequent follow-up questionnaire, thereby forming the sample for the analyses presented here.
Figure 1.
Impact of Injury Study recruitment process.
Table 2 shows baseline characteristics of the study sample, and indicates that: 51.7% were male; ages ranged from 16–69 years, with 53.1% aged 45–64 years; 75.7% had an injury of moderate severity; 42.9% reported single injuries; 62.3% had an injury of the lower limb; and injuries most commonly occurred at work (30.4%), and were most frequently caused by falls (58.2%).
Table 2.
Participants’ baseline characteristics (n = 273)
| Characteristic | Participantsa |
|---|---|
| Study site, n (%) | |
| Nottingham | 99 (36.3) |
| Leicester | 74 (27.1) |
| Bristol | 71 (26.0) |
| Guildford | 29 (10.6) |
|
| |
| Age, years, n (%) | |
| 16–24 | 29 (10.6) |
| 25–44 | 92 (33.7) |
| 45–64 | 145 (53.1) |
| 65–69 | 7 (2.6) |
|
| |
| Sex, n (%) | |
| Female | 132 (48.4) |
| Male | 141 (51.7) |
|
| |
| Ethnic group, n (%) | |
| White | 265 (97.1) |
| Black or ethnic minority | 8 (2.9) |
|
| |
| Deprivation | |
| IMD score, median (IQR) [3]b | 12 (7–20) |
|
| |
| Marital status, n (%) | |
| Single | 74 (27.1) |
| Married/partnership | 164 (60.1) |
| Divorced/widowed | 35 (12.8) |
|
| |
| Longstanding illness, n (%) [1]b | |
| No | 230 (84.3) |
| Yes | 42 (15.4) |
|
| |
| Past psychiatric diagnoses (obtained from SCID), n (%) | |
| 0 | 237 (86.8) |
| 1 | 27 (9.9) |
| ≥2 | 9 (3.3) |
|
| |
| HADS-A score, median (IQR) [1]b | 2 (0–4) |
|
| |
| HADS-D score, median (IQR) [1]b | 0 (0–2) |
|
| |
| AUDIT score, median (IQR) [5]b | 4 (2–6) |
|
| |
| DAST score, median (IQR) [2]b | 0 (0–0) |
|
| |
| Social functioning score, median (IQR) | 1 (0–3) |
|
| |
| Pain visual analogue scale score, median (IQR) [1]b | 0 (0–2) |
|
| |
| Nights in hospital, median (IQR) [11]b | 5.5 (3–8) |
|
| |
| Injury severity, n (%) [1]b | |
| Minor (AIS = 1) | 15 (5.5) |
| Moderate (AIS = 2) | 206 (75.7) |
| Serious or worse (AIS ≥3) | 51 (18.8) |
|
| |
| Injuries, n (%) | |
| 1 | 117 (42.9) |
| 2 | 91 (33.3) |
| ≥3 | 65 (23.8) |
|
| |
| Body part injured, n (%) | |
| Other | 28 (10.3) |
| Upper limb | 49 (18.0) |
| Lower limb | 170 (62.3) |
| Upper and lower limbs | 26 (9.5) |
|
| |
| Injury mechanism, n (%) | |
| Other | 28 (10.3) |
| Falls | 159 (58.2) |
| Traffic | 63 (23.1) |
| Struck | 23 (8.4) |
|
| |
| Place of injury, n (%) [1]b | |
| Other | 42 (15.4) |
| Home | 39 (14.3) |
| Work | 83 (30.4) |
| Road | 29 (10.6) |
| Countryside | 38 (13.9) |
| Sports facilities | 41 (15.0) |
Participants employed at baseline who returned 1-month questionnaire and at least one follow-up questionnaire.
[missing]. AIS = Abbreviated Injury Scale. AUDIT = Alcohol Use Disorders Identification Test. DAST = Drug Abuse Screening Test. HADS-A = Hospital Anxiety and Depression Scale — anxiety. HADS-D = Hospital Anxiety and Depression Scale — depression. IMD = Index of Multiple Deprivation. IQR = interquartile range. SCID = structured clinical interview.
Few participants returning follow-up questionnaires had returned to work at 1 month (13.2%), 23.4% had done so at 2 months, 52.4% at 4 months, and two-thirds (67.0%) at 12 months. Only 6.6% of participants had fully returned to work at all time points; 3.7% initially returned to work, but had not returned to work at a later time point. More than half (52.5%) of participants had a delayed RTW, 8.0% had not returned to work at any time point, and 29.4% had insufficient information to categorise RTW over the full 12-month period.
Univariate and multivariable associations with RTW are shown in Tables 3 and 4 respectively. In the final model, a one-unit increase in the Hospital Anxiety and Depression Scale — depression (HADS-D) score reduced the odds of RTW by 13.0% (OR 0.87, 95% CI = 0.79 to 0.95), a one-unit increase in the number of nights in hospital reduced the odds of RTW by 9.2% (OR 0.91, 95% CI = 0.86 to 0.96), the odds of RTW reduced by 6.7% per unit increase in crisis support (OR 0.93, 95% CI = 0.88 to 0.99), and by 72.7% for those experiencing threatening life events since the injury (OR 0.27, 95% CI = 0.10 to 0.72). Social functioning and negative changes in outlook were excluded due to high correlations with the HADS-D at 1 month. No statistically significant interactions between depression at 1 month and age, sex, and time were found. Variance inflation factors ranged from 1.03 to 3.08 (data not shown).
Table 3.
Potential factors associated with return to work
| Variable | Unadjusted OR (95% CI) |
|---|---|
| Location | |
| Centre | |
| Nottingham | 1.00 |
| Leicester | 0.82 (0.51 to 1.31) |
| Bristol | 0.92 (0.57 to 1.48) |
| Guildford | 1.96 (1.00 to 3.84) |
|
| |
| Age, years | |
| 16–24 | 1.00 |
| 25–44 | 1.29 (0.67 to 2.51) |
| 45–64 | 0.95 (0.51 to 1.76) |
| 65–69 | 0.65 (0.19 to 2.28) |
|
| |
| Sex | |
| Female | 1.00 |
| Male | 1.04 (0.71 to 1.51) |
|
| |
| Follow-up time, months | |
| 2 | 1.00 |
| 4 | 11.72 (6.06 to 22.70) |
| 12 | 77.39 (30.91 to 193.77) |
|
| |
| Psychological predictors at 1 month post-injury | |
| HADS-A | 0.92 (0.88 to 0.97) |
| HADS-D | 0.92 (0.88 to 0.96) |
| IES-A | 0.96 (0.93 to 0.98) |
| IES-I | 0.96 (0.94 to 0.99) |
| AUDIT scale, quintile | |
| 1 (0)a | 1.00 |
| 2 (1.0–2.0) | 1.08 (0.64 to 1.83) |
| 3 (2.2–3.0) | 1.73 (0.95 to 3.16) |
| 4 (3.3–6.0) | 2.12 (1.19 to 3.76) |
| 5 (7.0–25.0) | 1.16 (0.65 to 2.05) |
| DAST scale | 1.08 (0.69 to 1.67) |
|
| |
| Psychological predictors at baseline | |
| Past psychiatric diagnoses (obtained from SCID) | |
| 0 | 1.00 |
| 1 | 0.88 (0.46 to 1.68) |
| ≥2 | 0.27 (0.09 to 0.80) |
| HADS-A | 0.99 (0.93 to 1.05) |
| HADS-D | 0.94 (0.85 to 1.04) |
| AUDIT scale | 1.00 (0.96 to 1.04) |
| DAST scale | 0.92 (0.61 to 1.37) |
|
| |
| Longstanding illness | |
| No | 1.00 |
| Yes | 0.76 (0.46 to 1.27) |
|
| |
| Ethnic group | |
| White | 1.00 |
| Black or minority ethnic group | 0.43 (0.12 to 1.48) |
|
| |
| Deprivation (IMD) | 0.98 (0.97 to 1.00) |
|
| |
| Marital status | |
| Single | 1.00 |
| Married/partnership | 1.43 (0.92 to 2.22) |
| Divorced/widowed | 1.17 (0.62 to 2.20) |
|
| |
| Nights in hospital | 0.93 (0.90 to 0.97) |
|
| |
| Injury severity | |
| Minor (AIS = 1) | 1.00 |
| Moderate (AIS = 2) | 0.73 (0.32 to 1.63) |
| Serious or worse (AIS ≥3) | 0.42 (0.17 to 1.02) |
|
| |
| Number of injuries | |
| 1 | 1.00 |
| 2 | 1.12 (0.73 to 1.72) |
| ≥3 | 0.60 (0.38 to 0.97) |
|
| |
| Body part injured | |
| Other | 1.00 |
| Upper limb | 0.95 (0.46 to 1.96) |
| Lower limb | 0.55 (0.29 to 1.04) |
| Upper and lower limbs | 0.45 (0.19 to 1.03) |
|
| |
| Injury mechanism | |
| Other | 1.00 |
| Falls | 1.00 (0.54 to 1.84) |
| Traffic | 0.75 (0.38 to 1.49) |
| Struck | 1.10 (0.47 to 2.57) |
|
| |
| Place of injury | |
| Other | 1.00 |
| Home | 0.63 (0.32 to 1.22) |
| Work | 0.70 (0.40 to 1.24) |
| Road | 0.90 (0.44 to 1.85) |
| Countryside | 1.28 (0.64 to 2.55) |
| Sports facilities | 0.61 (0.31 to 1.17) |
|
| |
| Other predictors at 1 month post-injury | |
| Social functioning scale, quintile | |
| 1 (0–4.6)a | 1.00 |
| 2 (5–6.9) | 0.42 (0.24 to 0.73) |
| 3 (7–8) | 0.31 (0.18 to 0.54) |
| 4 (9–10) | 0.29 (0.16 to 0.52) |
| 5 (10.3–18.3) | 0.23 (0.13 to 0.42) |
| CCS | 1.00 (0.97 to 1.04) |
| CiOQ-P scale | 0.96 (0.94 to 0.98) |
| CiOQ-N scale | 0.97 (0.93 to 1.01) |
|
| |
| Threatening life events since injury | |
| No | 1.00 |
| Yes | 0.38 (0.22 to 0.66) |
|
| |
| Pain visual analogue scale | 0.98 (0.98 to 0.99) |
|
| |
| Seeking compensation | |
| No | 1.00 |
| Yes | 0.59 (0.38 to 0.90) |
|
| |
| Involved in litigation | |
| No | 1.00 |
| Yes | 0.57 (0.35 to 0.94) |
Figures in brackets represent the range for each quintile. AIS = Abbreviated Injury Scale. AUDIT= Alcohol Use Disorders Identification Test. CiOQ-N = Changes in Outlook Questionnaire (negative). CiOQ-P = Changes in Outlook Questionnaire (positive). CSS = Crisis Support Scale. DAST = Drug Abuse Screening Test. HADS-A = Hospital Anxiety and Depression Scale — anxiety. HADS-D = Hospital Anxiety and Depression Scale — depression. IES-A = Impact of Events Scale avoidance. IES-I = Impact of Events Scale intrusion. IMD = Index of Multiple Deprivation. IQR = interquartile range. OR = odds ratio. SCID = structured clinical interview.
Table 4.
Psychological and other predictors associated with return to work at 1 month post-injury
| Final model (complete case analysis) | Final model (multiple imputation analysis) | |
|---|---|---|
|
| ||
| Characteristic | OR (95% CI) | OR (95% CI) |
| Location | ||
| Centre | ||
| Nottingham | 1.00 | 1.00 |
| Leicester | 0.86 (0.40 to 1.85) | 0.90 (0.48 to 1.71) |
| Bristol | 0.68 (0.31 to 1.48) | 0.95 (0.52 to 1.73) |
| Guildford | 2.62 (0.92 to 7.50) | 1.97 (0.81 to 4.80) |
|
| ||
| Age, years | ||
| 16–24 | 1.00 | 1.00 |
| 25–44 | 1.13 (0.39 to 3.29) | 0.95 (0.44 to 2.08) |
| 45–64 | 0.44 (0.16 to 1.24) | 0.60 (0.27 to 1.31) |
| 65–69 | 0.27 (0.04 to 1.99) | 0.31 (0.06 to 1.68) |
|
| ||
| Sex | ||
| Female | 1.00 | 1.00 |
| Male | 0.73 (0.39 to 1.34) | 0.79 (0.45 to 1.38) |
|
| ||
| Follow-up time, months | ||
| 2 | 1.00 | 1.00 |
| 4 | 10.80 (5.62 to 20.76) | 7.16 (3.61 to 14.19) |
| 12 | 72.17 (29.02 to 179.45) | 31.78 (13.87 to 72.81) |
|
| ||
| Psychological predictors at 1 month post-injury | ||
| HADS-D | 0.87 (0.79 to 0.95) | 0.91 (0.85 to 0.99) |
|
| ||
| Psychological, sociodemographic, and injury characteristics at baseline | ||
| Nights in hospital | 0.91 (0.86 to 0.96) | 0.92 (0.88 to 0.97) |
|
| ||
| Other predictors at 1 month post-injury | ||
| CSS | 0.93 (0.88 to 0.99) | 0.97 (0.92 to 1.03) |
| Threatening life events since injury | ||
| No | 1.00 | 1.00 |
| Yes | 0.27 (0.10 to 0.72) | 0.42 (0.19 to 0.92) |
CSS = Crisis Support Scale. HADS-D = Hospital Anxiety and Depression Scale — depression. OR = odds ratio.
Non-responders were statistically significantly younger (P<0.001), more likely to be male (P<0.001), single (P<0.001), live in disadvantaged areas (P<0.001), and have scores indicating greater problems with alcohol (P = 0.001) and drug use (P = 0.01) than responders (data not shown). Results from the multiple imputation analysis (Table 4) were similar to the complete case analysis. Associations between depression at 1 month (OR 0.91, 95% CI = 0.85 to 0.99), nights in hospital (OR 0.92, 95% CI = 0.88 to 0.97), and threatening life events (OR 0.42, 95% CI = 0.19 to 0.92) remained statistically significant. Crisis support no longer remained statistically significantly associated with RTW (OR 0.97, 95% CI = 0.92 to 1.03).
DISCUSSION
Summary
One-third of participants had not returned to work at 12 months post-injury. An increased depression score at 1 month post-injury, increased hospital stay, subsequent threatening life events, and increased Crisis Support Scale score were associated with significantly lower odds of RTW after injury. Other sociodemographic and injury characteristics, such as age, sex, body part injured, or injury severity, were not independently associated with RTW status. Findings for depression, length of hospital stay, and threatening life events remained statistically significant in multiple imputation analyses.
Strengths and limitations
One strength of this study is that it is the first prospective, multicentre, UK study to quantify the impact of early psychological morbidity on RTW in adults aged 16–69 years, who were admitted to hospital following a range of injuries. It also addressed some limitations of previous studies by including a general injury population with injuries of varying levels of severity, measuring a series of psychological predictors of RTW, and adjusting for several potential confounders. Despite responders differing from non-responders on a range of characteristics, multiple imputation analyses showed that most of the findings were robust to missing data. Follow-up rates were higher than, or comparable with, those of studies that used similar recruitment methods.38–42
Limitations include a potential selection bias: 30% of eligible patients who were approached took part, and participants and non-participants may have differed in terms of their likelihood of returning to work. It was also not possible to explore the impact of injuries on changes to jobs and hours of work; further work is required to address this.
The number of participants with some types of injuries (for example, penetrating injuries or over-exertion injures such as sprains) was small, limiting analyses to broad injury groupings. The upper limb, lower limb, upper and lower limbs, and other injuries categories were chosen because limb injuries are a major cause of work disability43–45 and the groups were consistent with a systematic review of prognostic factors associated with RTW post-injury.46 Similarly, small numbers required broad grouping of injury mechanisms.
Study sites were in the Midlands and southern England. Occupations vary across the country and ‘blue-collar work’ (for example, manual labour or work paid by the hour) has previously been associated with lower rates of RTW post-injury;46 as such, some care should be taken in generalising the findings to the north of the country.
Black and minority ethnic groups were under-represented, potentially limiting the generalisability of these findings.
Injuries that take place at work are likely to have poorer work-related outcomes than those occurring elsewhere;42,47,48 this may be partly explained by depression and PTSD, which may be more common after occupational injuries.8,49–51 With only 83 participants who suffered work-related injuries, the predictors and RTW were not explored in this group as this study was underpowered to detect significant associations between predictors and RTW in this group.
The finding of lower odds of RTW with increasing crisis support was unexpected, although the scale used measured support provided in a crisis, not longer-term social support. Higher levels of crisis support may reflect greater emotional distress or physical impairment, both of which could reduce the odds of RTW. In addition, the short-term nature of crisis support may not provide the buffering effect on depression often seen with longer-term social support.
Comparison with existing literature
Non-UK studies show post-injury depression and PTSD are associated with delayed RTW,19,52,53 but differences in occupations, benefits, and compensation systems limit comparability with the UK. A 2010 systematic review of RTW prognostic factors after acute orthopaedic trauma46 included only two small UK studies; the authors of the research presented here have not found any more recent UK studies.
One cohort study from 2002 recruited 154 injured males admitted to hospital and found greater PTSD symptoms were associated with a reduced odds of RTW 18 months post-injury (regression coefficient Impact of Event Scale-R avoidance subscale 0.47, 95% CI not reported, P<0.001).42 Another study, from 1992 — a review of the records of 101 patients receiving compensation having sustained injury in road traffic accidents — found that undefined psychological problems (regression coefficient 3.24, standard error [SE] 1.54) and older age (regression coefficient −0.77, SE 0.39) were associated with a reduced likelihood of RTW.54 In the study presented here, no association between PTSD symptoms and RTW was found, once depression was in the multivariable model. This may be explained by the fact that depression and PTSD often coexist.55 Most (81%) of the current study’s participants with moderate or severe PTSD met borderline or case criteria for depression and/or anxiety. Injuries due to assaults42 and road traffic accidents54 were more frequent than in the study presented here, and PTSD may be more common after such injuries.
Differences in study populations may explain the variation between the findings presented here and those of other studies in relation to sex42 and age;54 the larger sample size of this study may explain the statistically significant finding for length of hospital stay.
Implications for research and practice
Patients consult frequently in primary care after injury,5 hence a range of primary care professionals, including GPs, are well placed to identify psychological morbidity post-injury. Most injured patients have not returned to work 1 month after injury and would be eligible for the Fit for Work service, according to guidance from the UK government.56 This service provides occupational health assessments and develops an RTW plan with patients; the findings presented here suggest assessments should include identifying, and responding to, psychological morbidity.
This study identified a small number of key factors — depression, longer in-patient stays, threatening life events subsequent to injury, and greater crisis support — that predicted longer work absence. GPs, occupational health services, and the Fit for Work service can use these findings to identify those patients who may benefit from additional help with returning to work.
Some GPs may regard depressive symptoms almost as ‘normal’ after an injury and are reluctant to ‘medicalise unhappiness’.57 Watchful waiting may be appropriate for short-lived symptoms, but this study shows the negative impact of depressive symptoms that last for 1 month or more post-injury. The National Institute for Health and Care Excellence (NICE) guideline on recognising and managing depression in adults with chronic physical health problems highlights the high risk of depression where functional impairment is present.58 Thus, as traumatic injuries requiring hospital admission frequently result in functional impairments for many months,41,59 these NICE guidelines should be applied.
Traumatic injuries present additional challenges for GPs in terms of managing depression, such as impaired mobility, which can limit access to group-based peer support, talking therapies, or undertaking physical activity; analgesics and adjuvant pain medications may also interact with antidepressants.
Further work exploring GPs’ perceptions of psychological problems post-injury, the extent and ways in which they identify, manage, and coordinate care for these patients, and barriers and facilitators to doing so would be useful. Longitudinal studies assessing the impact of psychological problems on RTW after acute traumatic occupational injuries would also be beneficial, as this group may be at particular risk of experiencing psychological problems.
Funding
This study was funded by the National Institute for Health Research (NIHR) Collaboration for Leadership in Applied Health Research and Care (CLAHRC) Nottinghamshire, Derbyshire, and Lincolnshire. Richard Morriss is currently funded by NIHR CLAHRC East Midlands. The views expressed are those of the authors and not necessarily of the NHS, NIHR, or the Department of Health.
Ethical approval
Ethical approval for the study was provided by Nottingham Research Ethics Committee 1 (ref. 09/H0407/29).
Provenance
Freely submitted; externally peer reviewed.
Competing interests
The authors have declared no competing interests.
Discuss this article
Contribute and read comments about this article: bjgp.org/letters
REFERENCES
- 1.Waddell G, Burton AK. Is work good for your health and well-being? An evidence review. Norwich: TSO; 2006. https://www.gov.uk/government/publications/is-work-good-for-your-health-and-well-being (accessed 16 May 2017) [Google Scholar]
- 2.Black C. Working for a healthier tomorrow. Dame Carol Black’s review of the health of Britain’s working age population. London: TSO; 2008. https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/209782/hwwb-working-for-a-healthier-tomorrow.pdf (accessed 16 May 2017) [Google Scholar]
- 3.NHS Digital Hospital Episode Statistics, Admitted Patient Care — England, 2014–15. http://content.digital.nhs.uk/searchcatalogue?productid=19420&q=title%3a%22Hospital+Episode+Statistics%2c+Admitted+patient+care+-+England%22&sort=Relevance&size=10&page=1#top (accessed 16 May 2017)
- 4.Kellezi B, Baines DL, Coupland C, et al. The impact of injuries on health service resource use and costs in primary and secondary care in the English NHS. J Public Health (Oxf) 2015;ii:fdv173. doi: 10.1093/pubmed/fdv173. [DOI] [PubMed] [Google Scholar]
- 5.Kendrick D, Vinogradova Y, Coupland C, et al. Getting back to work after injury: the UK Burden of Injury multicentre longitudinal study. BMC Public Health. 2012;12:584. doi: 10.1186/1471-2458-12-584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Black C, Frost D. Health at work: an independent review of sickness absence. London: TSO; 2011. https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/181060/health-at-work.pdf (accessed 19 May 2017) [Google Scholar]
- 7.Bültmann U, Franche R-L, Hogg-Johnson S, et al. Health status, work limitations, and return-to-work trajectories in injured workers with musculoskeletal disorders. Qual Life Res. 2007;16(7):1167–1178. doi: 10.1007/s11136-007-9229-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Carnide N, Franche R-L, Hogg-Johnson S, et al. Course of depressive symptoms following a workplace injury: a 12-month follow-up update. J Occup Rehabil. 2016;26(2):204–215. doi: 10.1007/s10926-015-9604-3. [DOI] [PubMed] [Google Scholar]
- 9.Lin KH, Shiao JS, Guo NW, et al. Long-term psychological outcome of workers after occupational injury: prevalence and risk factors. J Occup Rehabil. 2014;24(1):1–10. doi: 10.1007/s10926-013-9431-3. [DOI] [PubMed] [Google Scholar]
- 10.Vles WJ, Steyerberg EW, Essink-Bot ML, et al. Prevalence and determinants of disabilities and return to work after major trauma. J Trauma. 2005;58(1):126–135. doi: 10.1097/01.ta.0000112342.40296.1f. [DOI] [PubMed] [Google Scholar]
- 11.Wall CL, Ogloff JRP, Morrissey SA. Psychological consequences of work injury: personality, trauma and psychological distress symptoms of noninjured workers and injured workers returning to, or remaining at work. Int J Disability Management. 2007;2(2):37–46. [Google Scholar]
- 12.Noble J, Gomez M, Fish JS. Quality of life and return to work following electrical burns. Burns. 2006;32(2):159–164. doi: 10.1016/j.burns.2005.08.022. [DOI] [PubMed] [Google Scholar]
- 13.Zatzick D, Jurkovich G, Rivara FP, et al. A national US study of posttraumatic stress disorder, depression, and work and functional outcomes after hospitalization for traumatic injury. Ann Surg. 2008;248(3):429–437. doi: 10.1097/SLA.0b013e318185a6b8. [DOI] [PubMed] [Google Scholar]
- 14.Blaszczynski A, Gordon K, Silove D, et al. Psychiatric morbidity following motor vehicle accidents: a review of methodological issues. Compr Psychiatry. 1998;39(3):111–121. doi: 10.1016/s0010-440x(98)90069-4. [DOI] [PubMed] [Google Scholar]
- 15.Ash P, Goldstein SI. Predictors of returning to work. Bull Am Acad Psychiatry Law. 1995;23(2):205–210. [PubMed] [Google Scholar]
- 16.Franche RL, Carnide N, Hogg-Johnson S, et al. Course, diagnosis, and treatment of depressive symptomatology in workers following a workplace injury: a prospective cohort study. Can J Psychiatry. 2009;54(8):534–546. doi: 10.1177/070674370905400806. [DOI] [PubMed] [Google Scholar]
- 17.Matthews LR. Work potential of road accident survivors with post-traumatic stress disorder. Behav Res Ther. 2005;43(4):475–483. doi: 10.1016/j.brat.2004.03.008. [DOI] [PubMed] [Google Scholar]
- 18.Opsteegh L, Reinders-Messelink HA, Schollier D, et al. Determinants of return to work in patients with hand disorders and hand injuries. J Occup Rehabil. 2009;19(3):245–255. doi: 10.1007/s10926-009-9181-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Tøien K, Skogstad L, Ekeberg Ø, et al. Prevalence and predictors of return to work in hospitalised trauma patients during the first year after discharge: a prospective cohort study. Injury. 2012;43(9):1606–1613. doi: 10.1016/j.injury.2011.03.038. [DOI] [PubMed] [Google Scholar]
- 20.Ching AC, Wessler L, Blizzard SR, et al. The relation between depression, PTSD and the likelihood of returning to work after spine trauma. Spine J. 2014;14(11):S6. [Google Scholar]
- 21.Kendrick D, O’Brien C, Christie N, et al. The impact of injuries study. Multicentre study assessing physical, psychological, social and occupational functioning post injury — a protocol. BMC Public Health. 2011;11(1):963. doi: 10.1186/1471-2458-11-963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Jacobson RR. The post-concussional syndrome: physiogenesis, psychogenesis and malingering. An integrative model. J Psychosom Res. 1995;39(6):675–693. doi: 10.1016/0022-3999(95)00006-5. [DOI] [PubMed] [Google Scholar]
- 23.Department for Communities and Local Government. English Indices of Deprivation 2010. London: Department for Communities and Local Government; 2011. https://www.gov.uk/government/statistics/english-indices-of-deprivation-2010 (accessed 15 May 2017) [Google Scholar]
- 24.Bjelland I, Dahl AA, Haug TT, Neckelmann D. The validity of the Hospital Anxiety and Depression Scale: an updated literature review. J Psychosom Res. 2002;52(2):69–77. doi: 10.1016/s0022-3999(01)00296-3. [DOI] [PubMed] [Google Scholar]
- 25.Saunders JB, Aasland OG, Babor TF, et al. Development of the Alcohol Use Disorders Identification Test (AUDIT): WHO Collaborative Project on Early Detection of Persons with Harmful Alcohol Consumption-II. Addiction. 1993;88:791–804. doi: 10.1111/j.1360-0443.1993.tb02093.x. [DOI] [PubMed] [Google Scholar]
- 26.Maisto SA, Carey MP, Carey KB, et al. Use of the AUDIT and the DAST-10 to identify alcohol and drug use disorders among adults with a severe and persistent mental illness. Psychol Assess. 2000;12(2):186–192. doi: 10.1037//1040-3590.12.2.186. [DOI] [PubMed] [Google Scholar]
- 27.Tyrer P, Nur U, Crawford M, et al. The Social Functioning Questionnaire: a rapid and robust measure of perceived functioning. Int J Soc Psychiatry. 2005;51(3):265–275. [PubMed] [Google Scholar]
- 28.Association for the Advancement of Automotive Medicine. Abbreviated Injury Scale (AIS) 2005 — update 2008. 2008. https://www.aaam.org/abbreviated-injury-scale-ais/ (accessed 24 May 2017) [PMC free article] [PubMed]
- 29.Harms L. After the accident: survivors’ perceptions of recovery following road trauma. Aust Soc Work. 2004;57(2):161–174. [Google Scholar]
- 30.Horowitz M, Wilner N, Alvarez W. Impact of Event Scale: a measure of subjective stress. Psychosom Med. 1979;41(3):209–218. doi: 10.1097/00006842-197905000-00004. [DOI] [PubMed] [Google Scholar]
- 31.Brugha T, Bebbington P, Tennant C, Hurry J. The list of threatening experiences: a subset of 12 life event categories with considerable long-term contextual threat. Psychol Med. 1985;15(1):189–194. doi: 10.1017/s003329170002105x. [DOI] [PubMed] [Google Scholar]
- 32.Joseph S, Andrews B, Williams R, Yule W. Crisis support and psychiatric symptomatology in adult survivors of the Jupiter cruise ship disaster. Br J Clin Psychol. 1992;31(Pt 1):63–73. doi: 10.1111/j.2044-8260.1992.tb00968.x. [DOI] [PubMed] [Google Scholar]
- 33.Joseph S, Linley PA, Andrews L, et al. Assessing positive and negative changes in the aftermath of adversity: psychometric evaluation of the changes in outlook questionnaire. Psychol Assess. 2005;17(1):70–80. doi: 10.1037/1040-3590.17.1.70. [DOI] [PubMed] [Google Scholar]
- 34.First MB, Gibbon M, Spitzer RL, Williams JBW. User’s guide for the structured clinical interview for DSM-IV-TR axis I disorders — research version. New York, NY: Biometrics Research, New York State Psychiatric Institute; 2002. [Google Scholar]
- 35.Harcombe H, Langley J, Davie G, Derrett S. Functional status following injury: what recovery pathways do people follow? Injury. 2015;46(7):1275–1280. doi: 10.1016/j.injury.2015.04.004. [DOI] [PubMed] [Google Scholar]
- 36.Rubin DB. Multiple imputation for nonresponse in surveys. New York, NY: John Wiley & Sons; 2004. [Google Scholar]
- 37.Royston P. Multiple imputation of missing values. Stata Journal. 2004;4(3):227–241. [Google Scholar]
- 38.Polinder S, van Beeck EF, Essink-Bot ML, et al. Functional outcome at 2.5, 5, 9, and 24 months after injury in the Netherlands. J Trauma. 2007;62(1):133–141. doi: 10.1097/TA.0b013e31802b71c9. [DOI] [PubMed] [Google Scholar]
- 39.Wilson R, Hansen P, Langley J, Derrett S. A comparison of injured patient and general population valuations of EQ-5D health states for New Zealand. Health Qual Life Outcomes. 2014;12:21. doi: 10.1186/1477-7525-12-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kendrick D, Vinogradova Y, Coupland C, et al. Recovery from injury: the UK burden of injury multicentre longitudinal study. Inj Prev. 2013;19(6):370–381. doi: 10.1136/injuryprev-2012-040658. [DOI] [PubMed] [Google Scholar]
- 41.Meerding WJ, Looman CWN, Essink-Bot M-L, et al. Distribution and determinants of health and work status in a comprehensive population of injury patients. J Trauma. 2004;56(1):150–161. doi: 10.1097/01.TA.0000062969.65847.8B. [DOI] [PubMed] [Google Scholar]
- 42.Mason S, Wardrope J, Turpin G, Rowlands A. Outcomes after injury: a comparison of workplace and nonworkplace injury. J Trauma. 2002;53(1):98–103. doi: 10.1097/00005373-200207000-00019. [DOI] [PubMed] [Google Scholar]
- 43.MacKenzie EJ, Bosse MJ, Kellam JF, et al. Early predictors of long-term work disability after major limb trauma. J Trauma. 2006;61(3):688–694. doi: 10.1097/01.ta.0000195985.56153.68. [DOI] [PubMed] [Google Scholar]
- 44.Pichora D, Grant H. Upper extremity injured workers stratified by current work status: an examination of health characteristics, work limitations and work instability. Int J Occup Environ Med. 2010;1(3):124–131. [PubMed] [Google Scholar]
- 45.Read KM, Kufera JA, Dischinger PC, et al. Life-altering outcomes after lower extremity injury sustained in motor vehicle crashes. J Trauma. 2004;57(4):815–823. doi: 10.1097/01.ta.0000136289.15303.44. [DOI] [PubMed] [Google Scholar]
- 46.Clay FJ, Newstead SV, McClure RJ. A systematic review of early prognostic factors for return to work following acute orthopaedic trauma. Injury. 2010;41(8):787–803. doi: 10.1016/j.injury.2010.04.005. [DOI] [PubMed] [Google Scholar]
- 47.Schneider JC, Bassi S, Ryan CM. Employment outcomes after burn injury: a comparison of those burned at work and those burned outside of work. J Burn Care Res. 2011;32(2):294–301. doi: 10.1097/BCR.0b013e31820aaf56. [DOI] [PubMed] [Google Scholar]
- 48.Lilley R, Davie G, Langley J, et al. Do outcomes differ between work and nonwork-related injury in a universal injury compensation system? Findings from the New Zealand Prospective Outcomes of Injury Study. BMC Public Health. 2013;13:995. doi: 10.1186/1471-2458-13-995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Kim J. Depression as a psychosocial consequence of occupational injury in the US working population: findings from the medical expenditure panel survey. BMC Public Health. 2013;13:303. doi: 10.1186/1471-2458-13-303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Ghisi M, Novara C, Buodo G, et al. Psychological distress and post-traumatic symptoms following occupational accidents. Behav Sci. 2013;3(4):587–600. doi: 10.3390/bs3040587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Buodo G, Novara C, Ghisi M, Palomba D. Posttraumatic and depressive symptoms in victims of occupational accidents. Depress Res Treat. 2012;2012:184572. doi: 10.1155/2012/184572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Zatzick D, Jurkovich GJ, Rivara FP, et al. A national US study of posttraumatic stress disorder, depression, and work and functional outcomes after hospitalization for traumatic injury. Ann Surg. 2008;248(3):429–437. doi: 10.1097/SLA.0b013e318185a6b8. [DOI] [PubMed] [Google Scholar]
- 53.Richmond TS, Amsterdam JD, Guo W, et al. The effect of post-injury depression on return to pre-injury function: a prospective cohort study. Psychol Med. 2009;39(10):1709–1720. doi: 10.1017/S0033291709005376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Cornes P. Return to work of road accident victims claiming compensation for personal injury. Injury. 1992;23(4):256–260. doi: 10.1016/s0020-1383(05)80011-7. [DOI] [PubMed] [Google Scholar]
- 55.O’Donnell ML, Creamer M, Pattison P. Posttraumatic stress disorder and depression following trauma: understanding comorbidity. Am J Psychiatry. 2004;161(8):1390–1396. doi: 10.1176/appi.ajp.161.8.1390. [DOI] [PubMed] [Google Scholar]
- 56.Department for Work and Pensions. Fit for work: guidance for GPs. 2015. https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/458954/gp-fit-for-work-gps.pdf (accessed 19 May 2017)
- 57.Christie N, Beckett K, Earthy S, et al. Seeking support after hospitalisation for injury: a nested qualitative study of the role of primary care. Br J Gen Pract. 2016. DOI: https://doi.org/10.3399/bjgp15X688141. [DOI] [PMC free article] [PubMed]
- 58.National Institute for Health and Care Excellence. Depression in adults with a chronic physical health problem: recognition and management. CG91. London: NICE; 2009. https://www.nice.org.uk/guidance/cg91 (accessed 5 Jun 2017) [Google Scholar]
- 59.Holbrook TL, Anderson JP, Sieber WJ, et al. Outcome after major trauma: 12-month and 18-month follow-up results from the Trauma Recovery Project. J Trauma. 1999;46(5):765–771. doi: 10.1097/00005373-199905000-00003. discussion 771–773. [DOI] [PubMed] [Google Scholar]