Abstract
Background
Dysplasia may progress because of a loss to follow-up after an abnormal cervical cytology. Approximately 18% of Danish women postpone the recommended follow-up, which depends on the cytology results.
Aim
To investigate if a reminder to the GP about missed follow-up could reduce the proportion of women who fail to act on a recommended follow-up, and to analyse the effect on sociodemographic and general practice variations.
Design and setting
A national electronic GP reminder system was launched in Denmark in 2012 to target missed follow-up after screening, opportunistic testing, or surveillance indication. The authors compared follow-up proportions in a national observational before–after study.
Method
From national registries, 1.5 million cervical cytologies (from 2009 to 2013) were eligible for inclusion. Approximately 10% had a recommendation for follow-up. The proportion of cervical cytologies without follow-up was calculated at different time points. Results were stratified by follow-up recommendations and sociodemographic characteristics, and changes in practice variation for follow-up were analysed.
Results
Fewer women with a recommendation for follow-up missed follow-up 6 months after a GP reminder. Follow-up improved in all investigated sociodemographic groups (age, ethnicity, education, and cohabitation status). Interaction was found for age and cohabitation status. Variation between practices in loss to follow-up was significantly reduced.
Conclusion
An electronic GP reminder system showed potential to improve the quality of cervical cancer screening through reduced loss to follow-up.
Keywords: early detection of cancer, general practice, mass screening, quality of health care, uterine cervical neoplasms
INTRODUCTION
Successful prevention of cervical cancer depends on follow-up of abnormalities after cervical cytology testing.1,2 Nevertheless, women without follow-up are a persisting problem in many Western countries.3–5 Lack of follow-up has been associated with both patient-6–8 and system-related barriers.3,9,10 In Denmark, a GP is usually involved in securing follow-up.5,11 Consequently, since 2012, GPs have received an electronic reminder if appropriate follow-up was not duly registered.11
Four other studies have addressed the effect of a GP reminder as a single intervention in cervical cancer screening follow-up. However, two of the studies lacked a control group,12,13 and a before–after study did not find more women with follow-up when comparing before and after in an unadjusted analysis, though the study may have been underpowered.14 A Dutch intervention study improved follow-up. However, in this setting it was necessary to generate a GP reminder for 45% of all women in need of follow-up and, despite this, 19% of intervention women missed follow-up 1 year after cervical cytology requisition.15 In Denmark, 18% of women with a cervical cytology and a recommendation for follow-up are without follow-up 12 weeks after recommended follow-up.5,11 This number is relatively low compared with studies in other countries.3 Therefore, evidence about the effects of a GP reminder in a clinical setting with better follow-up is needed. It could be expected that the remaining 18% of women without follow-up may face more complex barriers and could thus be more reluctant to attend follow-up.16 Additionally, no studies have described the effect of GP reminders on social inequality17 or variation among GP practices.
The authors aimed to evaluate the effect of GP reminders on women without follow-up, on sociodemographic differences, and on variation between GP practices.
METHOD
In a large observational study, the authors compared the proportions of follow-up before and after the implementation of a national electronic reminder system for GPs.
Setting
All Danish women aged 23–50 years are invited to cervical cancer screening every third year, and women aged 50–64 years are invited every fifth year. The women are identified through national databases and are encouraged to book an appointment free of charge with their general practice. All samples are sent to a pathology department for diagnosis. If necessary, a recommendation for follow-up is also applied — that is, either within 3 months (referral to a gynaecologist) or in 3, 6, or 12 months, depending on the current and former cervical cytology results. Results and follow-up recommendation are transferred to the electronic patient record in the general practice. GPs convey results to women either face-to-face, or by phone, or by e-mail.11 Before the implementation of GP reminders, no other national system initiatives were performed in Denmark to support women or GPs in remembering follow-up.11 Approximately 99% of all Danish women are listed with a specific GP practice.18
How this fits in
A review found that up to 12% of cancers arise due to failure in follow-up, and is the third most common reason for cancer development. Strategies to improve follow-up are thus crucial. As the sample taker, the GP plays a pivotal role in securing follow-up. This study found that a GP reminder almost halved the proportion of women without follow-up, had effect across sociodemographic groups, and decreased the variation in loss to follow-up among GPs.
Intervention
The reminder system was launched nationwide in Denmark on 18 January 2011 under the auspices of the Danish Pathology Data Bank (DPDB). The reminder system was fully operational on 2 February 2012 after a run-in period.4 Cervical cytologies with a recommendation of follow-up within 3 months (referral to gynaecologist) generated a GP reminder if no new cervical cytology or histology was registered in the DPDB 1 month after the follow-up was due. Cytology results with a recommendation of follow-up in 3, 6, or 12 months generated a reminder 3 months after recommended date of follow-up. It was anticipated that, after receiving the electronic reminder from the DPDB, GPs would initiate contact with the woman, and encourage her to return for the required follow-up. However, there was no protocol for how or when GPs should act on reminders and no additional resources were given to the GPs.
Study participants
All cervical cytology samples (Systematized Nomenclature of Medicine [SNOMED code: T8X310]) performed during 1 January 2009 to 5 August 2013 for women with a follow-up recommendation were identified, regardless of test indication (screening, opportunistic testing, or surveillance for earlier abnormality). The authors aimed to study follow-up adherence 6 months after the reminder (that is, 7 months after a recommendation for follow-up within 3 months, and 9 months after recommendations for follow-up in 3, 6, or 12 months), as the reminder was generated 1 or 3 months after the date of recommended follow-up. Data regarding follow-up were retrieved on 30 May 2014. Therefore, the authors only included cervical cytologies with a recommended follow-up date 7 or 9 months earlier than 30 May 2014. The authors excluded cytologies of women with unknown diagnosis or carcinoma, women who died or emigrated from Denmark in the study period, women with identification errors, and women who participated in the intervention arm of a randomised study targeted to improve follow-up.
Before–after exposure groups
The authors calculated a GP reminder date for all included cervical cytologies. They divided the study population into a before group (with a simulated reminder date before activation of the reminder system) and an after group (with an actual reminder date after activation). The before group consisted of women with a simulated reminder date before 18 July 2010 (that is, 6 months before the system was launched on 18 January 2011). The after group consisted of women with a reminder date after 2 February 2012 (when the system was fully operational). The transition group consisted of women with a GP reminder date generated during the run-in period (between 19 July 2010 and 2 February 2012). This period ensured a fully functioning reminder system in the after group and gave the GPs time to adapt to the new procedures.
Data
Data regarding cervical cytology and histology were retrieved from the nationwide DPDB. This register contains records on diagnosis and dates of all pathological material evaluated in Denmark since 1997, from all settings and regardless of indication. All cytologies are assigned codes from the Danish version of the SNOMED.19 National standards from 2007 prescribe classification of results in accordance with the Bethesda Classification for Cervical Cytology 2001 and encourage inclusion of follow-up recommendation (specific SNOMED codes).20,21
Information on sociodemographic characteristics was obtained through Statistics Denmark (on 1 January in the year preceding the cytology), and all data were linked using the unique Danish civil registration number of each woman. Educational level was categorised, according to the UNESCO classification, as low (≤10 years), middle (11–15 years), or higher education (>15 years).22 Cohabitation was categorised as married/cohabiting or living alone. Ethnicity was categorised according to the definition applied by Statistics Denmark as:
Danish;
immigrant or descendant from Western countries; or
immigrant or descendant from non-Western countries.23
Age was calculated by subtracting the woman’s date of birth from the cytology requisition date.
Statistical analysis
Follow-up proportions were calculated for each follow-up recommendation (that is, within 3, or in 3, 6, or 12 months) with all women needing follow-up as the denominator at four time points. Follow-up proportions in before-and-after groups were compared through odds ratios (OR) for the likelihood of not having a follow-up, and stratified according to type of follow-up recommendation.
The unit of analysis was the individual cervical cytology. The authors calculated ORs using multilevel mixed-effects logistic regression with random effects to correct for clustering of measurements within each woman, and for clustering of women within GP practices.24
Kaplan–Meier plots displayed the time from date of initial cervical cytology to date of follow-up, or censoring due to missed follow-up, at the end of the observation period, whichever came first.
To determine if the GP reminder effect was modified by the sociodemographic characteristics of the women, follow-up proportions 7 or 9 months after the recommended date of follow-up (that is, 6 months after a reminder for the after group) between before and after groups were compared in a stratified analysis. Associations between follow-up status and sociodemographic factors were estimated as described above and adjusted for age (as a continuous variable) and type of follow-up recommendation. Effect on GP practice variation was explored by calculating follow-up proportions 7 or 9 months after the recommended date of follow-up (that is, 6 months after a reminder for the after group) for each practice before and after implementation of the reminder system. To ensure high statistical precision, only GP practices with four or more cervical cytologies in need of follow-up were included. The proportions were listed according to order of practice proportions in scatterplots, and the interquartile range was estimated. Pitman’s test for comparing variances of follow-up proportions of paired GP practices was additionally used (Stata command: sdpair).25 Only practices that were active both before and after were included in this test. All statistical analyses were conducted using Stata version 14.
RESULTS
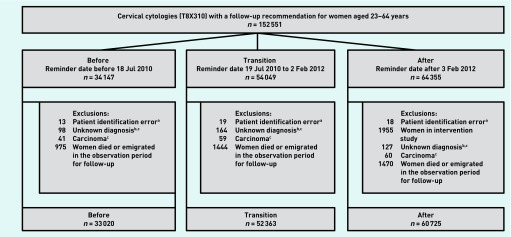
In the study period, 1 487 155 cervical cytologies were performed in general practice. Of these, 1 321 846 (88.9%) had no follow-up recommendation, and 12 758 (0.8%) had less than 6 months to observe follow-up adherence after the GP reminder. This left 152 551 (10.3%) eligible women in the study period. The authors included 33 020 cervical cytologies (from 29 978 women) before, and 60 725 cytologies (from 49 981 women) after the implementation in the analyses (Figure 1). Table 1 shows the baseline characteristics of the included women and cytologies. Follow-up recommendations and types of diagnosis differed between the before and after groups.
Figure 1.
Flow chart of number of cervical cytologies. aWomen without a unique Danish civil registration number. bUnknown diagnosis or potential uncertainty about follow-up recommendations. c Diagnosis formed according to information available from the authors upon request.
Table 1.
Characteristics of the 146 108 cervical cytologies and the 124 244 women before, in the transition period, and after implementation of GP reminders
| Before, n (%) | Transition, n (%) | After, n (%) | |
|---|---|---|---|
| Total number of cervical cytologies | 33 020 | 52 363 | 60 725 |
|
| |||
| Total number of general practices | 2093 | 2174 | 2176 |
|
| |||
| 10th–90th centile in number of cytologies per practice | 2–36 | 3–56 | 3–68 |
|
| |||
| Number of general practices with >4 cytologies | 1692 | 1943 | |
|
| |||
| Total number of women | 29 978 (100) | 44 285 (100) | 49 981 (100) |
| Number of women with 1 cytology | 27 044 (90) | 36 779 (83) | 40 098 (80) |
| Number of women with 2 cytologies | 2828 (9) | 6964 (16) | 9085 (18) |
| Number of women with ≥3 cytologies | 106 (0) | 542 (1) | 798 (2) |
|
| |||
| Diagnosisa | |||
| Normal | 4237 (13) | 16 248 (31) | 17 182 (28) |
| Inadequate | 10 308 (31) | 11 240 (21) | 11 440 (19) |
| ASC-US, ASC-H, AGC | 8034 (24) | 10 840 (21) | 12 367 (20) |
| LSIL | 6399 (19) | 9720 (19) | 14 730 (24) |
| HSIL, AIS | 4042 (12) | 4315 (8) | 5006 (8) |
|
| |||
| Follow-up recommendationa | |||
| Before 3 months (reminder after 4 months) | 11 957 (36) | 13 887 (27) | 17 673 (29) |
| 3 months (reminder after 6 months) | 10 222 (31) | 10 817 (21) | 10 854 (18) |
| 6 months (reminder after 9 months) | 6986 (21) | 8890 (17) | 9683 (16) |
| 12 months (reminder after 15 months) | 3855 (12) | 18 769 (36) | 22 515 (37) |
|
| |||
| Regiona | |||
| Capital Region of Denmark | 6297 (19) | 8532 (16) | 10 868 (18) |
| Region Zealand | 7134 (22) | 11 872 (22) | 13 048 (21) |
| Central Denmark Region | 9527 (29) | 15 247 (29) | 16 848 (28) |
| North Denmark Region | 3462 (10) | 6837 (13) | 8656 (14) |
| Region of Southern Denmark | 6598 (20) | 9875 (19) | 11 305 (19) |
| Missing | 2 | 0 | 0 |
|
| |||
| Median age of women (25th–75th centile)b | 36 (29–44) | 36 (29–44) | 36 (29–45) |
|
| |||
| Ethnicityb | |||
| Danish | 27 493 (93) | 40 764 (93) | 45 891 (93) |
| Western immigrants/descendants | 684 (2) | 991 (2) | 1289 (3) |
| Non-Western immigrants/descendants | 1266 (4) | 1892 (4) | 2139 (4) |
| Missing | 535 | 638 | 662 |
|
| |||
| Cohabitation statusb | |||
| Married/cohabiting | 18 308 (62) | 27 058 (62) | 29 601 (60) |
| Living alone | 11 140 (38) | 16 596 (38) | 19 724 (40) |
| Missing | 530 | 631 | 656 |
|
| |||
| Education (years)b | |||
| ≤10 | 5689 (20) | 8349 (19) | 9219 (19) |
| >10 to <15 | 15 624 (54) | 22 888 (53) | 25 318 (53) |
| >15 | 7663 (26) | 11 658 (27) | 13 656 (28) |
| Missing | 1002 | 1390 | 1788 |
Numbers per cervical cytology.
Numbers per women at time of first cervical cytology. AGC = atypical glandular cells. AIS = adenocarcinoma in situ. ASC-H = atypical squamous cells of undetermined significance. ASC-US = atypical cells of undetermined significance. HSIL = high-grade squamous intraepithelial lesion. LSIL = low-grade squamous intraepithelial lesion.
Table 2 presents the likelihood of not being followed-up, stratified by type of follow-up recommendation. Follow-up recommendations roughly corresponded to certain diagnoses. As indications for follow-up recommendations might have changed over time, sensitivity analyses were performed with adjustments for diagnoses, but this did not change the results substantially (further information is available from the authors on request).
Table 2.
Associations (odds ratios)a of cervical cytologies without follow-up, stratified by follow-up recommendation
| Before % without follow-up | After % without follow-up | After versus before (ref) OR (95% CI) | |
|---|---|---|---|
| Recommended follow-up in 12 months, n | 3855 | 22 515 | |
| At recommended follow-up date | 78.0 | 72.8 | 0.87 (0.83 to 0.91) |
| 3 months after recommended follow-up b | 48.8 | 48.0 | 1.00 (0.96 to 1.06) |
| 6 months after recommended follow-up | 36.0 | 18.6 | 0.54 (0.50 to 0.58) |
| 9 months after recommended follow-up | 28.4 | 11.7 | 0.44 (0.39 to 0.50) |
|
| |||
| Recommended follow-up in 6 months, n | 6986 | 9683 | |
| At recommended follow-up date | 64.8 | 62.0 | 0.94 (0.90 to 0.97) |
| 3 months after recommended follow-up b | 28.4 | 28.0 | 0.99 (0.96 to 1.03) |
| 6 months after recommended follow-up | 18.5 | 10.9 | 0.73 (0.69 to 0.76) |
| 9 months after recommended follow-up | 14.8 | 7.0 | 0.62 (0.56 to 0.69) |
|
| |||
| Recommended follow-up in 3 months, n | 10 222 | 10 854 | |
| At recommended follow-up date | 62.6 | 60.1 | 0.94 (0.90 to 0.97) |
| 3 months after recommended follow-up b | 34.3 | 32.4 | 0.94 (0.91 to 0.98) |
| 6 months after recommended follow-up | 25.5 | 15.0 | 0.64 (0.59 to 0.70) |
| 9 months after recommended follow-up | 21.5 | 10.6 | 0.60 (0.55 to 0.67) |
|
| |||
| Recommended follow-up within 3 months, n | 11 957 | 17 673 | |
| At recommended follow-up date | 16.3 | 16.2 | 0.99 (0.95 to 1.02) |
| 1 month after recommended follow-up b | 9.7 | 10.4 | 1.04 (0.99 to 1.08) |
| 4 months after recommended follow-up | 4.4 | 3.9 | 0.93 (0.88 to 0.99) |
| 7 months after recommended follow-up | 3.3 | 2.5 | 0.87 (0.81 to 0.94) |
Multilevel mixed-effect logistic regression, with correction for random-effect clusters at the level of GPs and women.
The date a GP reminder was generated for the after group. CI = confidence interval. OR = odds ratio. Ref = reference.
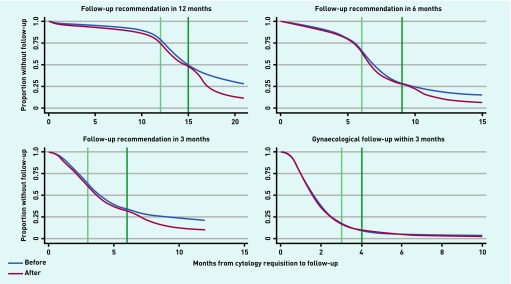
Figure 2 shows a marked temporal reduction in no follow-up when a GP reminder was generated for the after group, most markedly for those with a recommendation of follow-up in 12 months, and less markedly for those with a recommendation of follow-up within 3 months.
Figure 2.
Proportion of cervical cytologies without follow-up before and after implementation of reminders, stratified by follow-up recommendation.aaFirst vertical line is the time point for recommended follow-up. Second vertical line is the time point when a reminder was generated for the after group. Follow-up recommendations within 3 months (needing to consult a gynaecologist) had a GP reminder 1 month after recommended date of follow-up (that is, after 4 months), whereas recommendations for follow-up in 3, 6, or 12 months had a GP reminder 3 months after date of recommended follow-up (that is, after 6, 9, or 15 months).
Table 3 shows that follow-up was most complete for women ≥35 years, ethnic Danes, and women who are highly educated. The proportion without follow-up decreased significantly from before to after implementation in all sociodemographic groups. The effect was lowest among younger women (aged 23–34 years) and women living alone.
Table 3.
Association (odds ratios) between no follow-upa and sociodemographic status
| Before | After | After versus before (ref) | ||||
|---|---|---|---|---|---|---|
|
| ||||||
| n (% without follow-up)b | OR (95% CI)c | n (% without follow-up)b | OR (95% CI)c | OR (95% CI)c | Pd | |
| Age group, years | ||||||
| 23–34 | 15 650 (14.8) | 1 (ref) | 27 905 (9.2) | 1 (ref) | 0.53 (0.49 to 0.57) | |
| 35–44 | 9793 (14.1) | 0.79 (0.72 to 0.85) | 17 588 (7.5) | 0.63 (0.57 to 0.70) | 0.44 (0.40 to 0.48) | 0.001 |
| 45–54 | 5227 (12.7) | 0.66 (0.59 to 0.74) | 10 207 (6.5) | 0.49 (0.43 to 0.55) | 0.43 (0.37 to 0.48) | 0.003 |
| 55–64 | 2350 (15.5) | 0.79 (0.69 to 0.89) | 5025 (7.2) | 0.56 (0.48 to 0.66) | 0.36 (0.30 to 0.43) | 0.005 |
|
| ||||||
| Ethnicity | ||||||
| Non-Western | 1374 (22.0) | 1 (ref) | 2507 (12.6) | 1 (ref) | 0.46 (0.36 to 0.55) | |
| Western | 746 (18.1) | 0.86 (0.67 to 1.11) | 1548 (10.7) | 0.87 (0.66 to 1.14) | 0.48 (0.34 to 0.62) | 0.833 |
| Danish | 30 323 (13.7) | 0.58 (0.49 to 0.68) | 55 937 (7.7) | 0.50 (0.42 to 0.59) | 0.47 (0.44 to 0.49) | 0.644 |
|
| ||||||
| Education, years | ||||||
| <10 | 6267 (17.3) | 1 (ref) | 11 072 (10.3) | 1 (ref) | 0.47 (0.42 to 0.53) | |
| >10 to <15 | 17 321 (13.6) | 0.72 (0.66 to 0.79) | 30 970 (7.3) | 0.60 (0.54 to 0.66) | 0.44 (0.40 to 0.47) | 0.301 |
| >15 | 8348 (12.6) | 0.66 (0.60 to 0.74) | 16 592 (7.1) | 0.59 (0.52 to 0.66) | 0.47 (0.42 to 0.52) | 0.962 |
|
| ||||||
| Cohabitation | ||||||
| Living alone | 12 450 (12.8) | 1 (ref) | 24 441 (7.8) | 1 (ref) | 0.52 (0.48 to 0.57) | |
| Married/cohabiting | 19 999 (15.0) | 1.03 (0.95 to 1.11) | 35 559 (8.1) | 0.93 (0.86 to 1.01) | 0.44 (0.41 to 0.47) | 0.002 |
Follow-up proportions were studied 6 months after a GP reminder — that is, 7 months after recommended date of follow-up for women with a recommendation for gynaecological follow-up within 3 months, and 9 months after date of recommended follow-up for women with a recommendation for follow-up in 3, 6, or 12 months.
Numbers per cervical cytology. Numbers vary due to missing data.
Adjusted for type of follow-up recommendation. Ethnicity, education, and cohabitating status also adjusted for age.
Test for interaction showing if effects of reminders were modified by sociodemographic factors. CI = confidence interval. OR = odds ratio. Ref = reference.
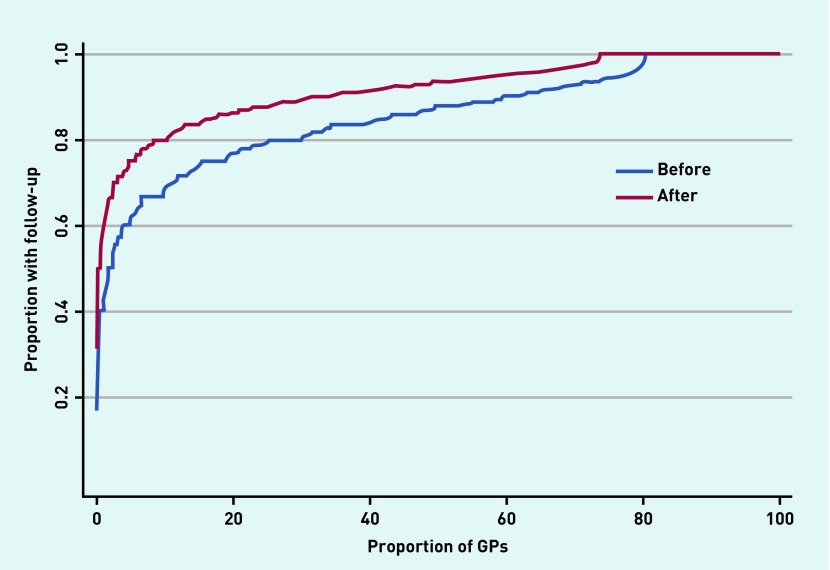
The interquartile interval of follow-up proportions among GP practices in the before group ranged from 79% to 94% (interquartile range [IQR] 15). Comparable estimates for the after group were 88% to 100% (IQR 12). The variation between follow-up proportions decreased significantly from before to after among the 1527 paired practices (ratio of standard deviations 0.67, 95% confidence interval [CI] = 0.63 to 0.70), visualised by a more horizontal after line compared with the before line (Figure 3).
Figure 3.
GP variations in cervical cytology follow-up proportions. Proportions of 1692 GP practices before, and 1943 GP practices after, listed according to proportion of women with follow-up. Observation of follow-up adherence ended 6 months after a GP reminder was generated to the after group. This entailed 7 months after recommended date of follow-up for women with a ’recommendation for follow-up within 3 months’, and 9 months for women with a ’recommendation for follow-up in 3, 6, or 12 months’.
DISCUSSION
Summary
The proportion of women without follow-up was almost halved following the implementation of the reminder system. It had a positive effect in all sociodemographic groups and reduced the variation in follow-up proportions among GP practices. The quality of the screening programme was thus improved. However, 2.5% to 11.7% of cervical cytologies had no follow-up 6 months after a GP reminder, depending on the type of follow-up recommendation.
Strengths and limitations
The risk of selection bias was reduced as the authors used prospectively collected national data from the DPDB. These records have been almost complete since 2005.26 The study enjoyed high statistical precision from the large number of included cervical cytologies and general practices. Misclassification due to ambiguous or imprecise coding was minimised as national standards for SNOMED coding of diagnoses and follow-up were adopted in Denmark in 2007.
A weakness of this observational study is the before–after design, as other changes may have caused the effects. For instance, small improvements were observed for the after group even before the introduction of the reminders, but the largest effects began to show at the exact time of the reminder introduction. The authors excluded women with identification errors as it was not possible in registries to study their follow-up. However, these women may be at greater risk of not returning for follow-up, therefore prevalence of follow-up proportions may be underestimated, though the authors do not expect it to affect the associations.
Differences in the distribution of follow-up recommendations persisted between before and after groups. This was expected, because of the design of the study. In particular, cytologies with late follow-up recommendation were more likely to receive a reminder (and be included in the after group) than those with a short follow-up recommendation. Therefore, all analysis of follow-up proportions were stratified by type of follow-up recommendation. Distribution of diagnoses also differed from before to after within each type of follow-up recommendation group (further information is available from the authors upon request). This may have been a consequence of introducing human papilloma virus (HPV) triage and a change to liquid-based screening techniques in pathology departments during the study period.11,20 Even though adjusting for diagnosis did not alter associations much, confounding may persist (further information is available from the authors upon request).
Comparison with existing literature
Other studies found varying improvement in follow-up using GP reminders,13–15 but these did not investigate effects on sociodemographic variations. In this study, the reminder improved follow-up in all social groups. However, 6.5% to 12.6% of the women were not followed up, particularly younger and low-educated women with non-Western ethnicity. Other studies have found similar inequalities.6,27 Inequalities persisted with reminders, and as the reminders had a smaller relative effect among women living alone and younger women, relative inequalities may thereby increase, even though the absolute differences in these groups were reduced.
The most profound effect of reminders was found for cervical cytologies with a recommendation of follow-up in 12 months. Approximately 80% of these cytologies were normal but still needed follow-up, for example, due to surveillance for earlier dysplasia (further information is available from the authors upon request). Normal test results are generally excluded from studies on follow-up,13–15 even though it is assumed that 8% of women develop new pre-cancerous dysplasia after cone biopsy treatment, and 80% within 2 years.28 Additionally, incidence rate ratios of cervical cancer are increased for up to 15.5 years after an abnormal cytology.29 Some of these women are followed in general practice.11 A smaller, significant effect was found among women with a recommendation of follow-up within 3 months. Approximately 30% of these have a high-grade squamous intraepithelial lesion (HSIL) diagnosis (further information is available from the authors upon request). However, as almost 30% of women with cervical squamous intraepithelial neoplasia (CIN) III are expected to receive a cancer diagnosis if no subsequent adequate treatment is performed,30 even small improvements for this group may be important. For women with a recommendation for follow-up in 3 months, 95% and 99% of results were inadequate in the before and after study populations, respectively (further information is available from the authors upon request). Women with this type of follow-up recommendation also improved follow-up, but do not necessarily have an increased risk of cancer.
Implications for practice
Reminders improved the follow-up of women participating in cervical cancer screening, regardless of sociodemographic characteristics. The effect was seen in a healthcare system with a relatively high follow-up rate, which proves that the GP reminder intervention delivers strong results. However, challenges with follow-up and social inequalities persist, and this finding needs further consideration. Electronic reminders are currently sent to the general practice that performed the cytology and thus not necessarily to the woman’s current GP. In Denmark, 23% of the population aged 18–30 years change GP practice each year, whereas the corresponding figure is only 4% for women aged ≥50.31 Thus, reminders may address social inequality among the young if sent to the woman’s current GP or to the woman herself. The intervention decreased the variation in follow-up proportions between GPs. This implies that the GP reminder served as a supportive tool for GPs, as follow-up of women now depends to a lesser extent on individual GPs.
Funding
The study was financially supported by the Danish foundation TrygFonden (grant number: 7.12.0836), the Health Science Research Foundation of the Central Denmark Region, and the Health Foundation (grant number: 20128125).
Ethical approval
None required.
Provenance
Freely submitted; externally peer reviewed.
Competing interests
The authors have declared no competing interests.
Discuss this article
Contribute and read comments about this article: bjgp.org/letters
REFERENCES
- 1.Leyden WA, Manos MM, Geiger AM, et al. Cervical cancer in women with comprehensive health care access: attributable factors in the screening process. J Natl Cancer Inst. 2005;97(9):675–683. doi: 10.1093/jnci/dji115. [DOI] [PubMed] [Google Scholar]
- 2.Spence AR, Goggin P, Franco EL. Process of care failures in invasive cervical cancer: systematic review and meta-analysis. Prev Med. 2007;45(2–3):93–106. doi: 10.1016/j.ypmed.2007.06.007. [DOI] [PubMed] [Google Scholar]
- 3.Yabroff KR, Washington KS, Leader A, et al. Is the promise of cancer-screening programs being compromised? Quality of follow-up care after abnormal screening results. Med Care Res Rev. 2003;60(3):294–331. doi: 10.1177/1077558703254698. [DOI] [PubMed] [Google Scholar]
- 4.Steering Committee for the Danish Cervical Cancer Screening Programme. Annual report 2014. The Danish Clinical Registries (RKKP); 2014. [In Danish]. [Google Scholar]
- 5.Lynge E, Rygaard C, Baillet MV, et al. Cervical cancer screening at crossroads. APMIS. 2014;122(8):667–673. doi: 10.1111/apm.12279. [DOI] [PubMed] [Google Scholar]
- 6.Elit L, Krzyzanowska M, Saskin R, et al. Sociodemographic factors associated with cervical cancer screening and follow-up of abnormal results. Can Fam Physician. 2012;58(1):e22–e31. [PMC free article] [PubMed] [Google Scholar]
- 7.Ibfelt EH, Kjaer SK, Hogdall C, et al. Socioeconomic position and survival after cervical cancer: influence of cancer stage, comorbidity and smoking among Danish women diagnosed between 2005 and 2010. Br J Cancer. 2013;109(9):2489–2495. doi: 10.1038/bjc.2013.558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ibfelt E, Kjaer SK, Johansen C, et al. Socioeconomic position and stage of cervical cancer in Danish women diagnosed 2005 to 2009. Cancer Epidemiol Biomarkers Prev. 2012;21(5):835–842. doi: 10.1158/1055-9965.EPI-11-1159. [DOI] [PubMed] [Google Scholar]
- 9.Yabroff KR, Zapka J, Klabunde CN, et al. Systems strategies to support cancer screening in US primary care practice. Cancer Epidemiol Biomarkers Prev. 2011;20(12):2471–2479. doi: 10.1158/1055-9965.EPI-11-0783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bastani R, Yabroff KR, Myers RE, Glenn B. Interventions to improve follow-up of abnormal findings in cancer screening. Cancer. 2004;101(5 Suppl):1188–1200. doi: 10.1002/cncr.20506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Danish National Board of Health. Cervical cancer screening — recommendations 2012. Copenhagen: Sundhedsstyrelsen; 2012. [In Danish]. [Google Scholar]
- 12.Mitchell H, Medley G. Adherence to recommendations for early repeat cervical smear tests. BMJ. 1989;298(6688):1605–1607. doi: 10.1136/bmj.298.6688.1605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wagner E, Duggan MA. Effectiveness of follow up-letters to health care providers in triggering follow-up for women with abnormal results on Papanicolaou testing. CMAJ. 2001;164(2):207–208. [PMC free article] [PubMed] [Google Scholar]
- 14.Dupuis EA, White HF, Newman D, et al. Tracking abnormal cervical cancer screening: evaluation of an EMR-based intervention. J Gen Intern Med. 2010;25(6):575–580. doi: 10.1007/s11606-010-1287-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hermens RP, Siebers BG, Hulscher ME, et al. Follow-up of abnormal or inadequate cervical smears using two guidance systems: RCT on effectiveness. Prev Med. 2005;41(5–6):809–814. doi: 10.1016/j.ypmed.2005.08.002. [DOI] [PubMed] [Google Scholar]
- 16.Burger EA, Kim JJ. The value of improving failures within a cervical cancer screening program: an example from Norway. Int J Cancer. 2014;135(8):1931–1939. doi: 10.1002/ijc.28838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Eggleston KS, Coker AL, Das IP, et al. Understanding barriers for adherence to follow-up care for abnormal pap tests. J Womens Health (Larchmt) 2007;16(3):311–330. doi: 10.1089/jwh.2006.0161. [DOI] [PubMed] [Google Scholar]
- 18.Pedersen KM, Andersen JS, Sondergaard J. General practice and primary health care in Denmark. J Am Board Fam Med. 2012;25(Suppl 1):S34–S38. doi: 10.3122/jabfm.2012.02.110216. [DOI] [PubMed] [Google Scholar]
- 19.Erichsen R, Lash TL, Hamilton-Dutoit SJ, et al. Existing data sources for clinical epidemiology: the Danish National Pathology Registry and Data Bank. Clin Epidemiol. 2010;2:51–56. doi: 10.2147/clep.s9908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Danish National Board of Health. Cervical cancer screening — recommendations 2007. Copenhagen: Sundhedsstyrelsen; 2007. [In Danish]. [Google Scholar]
- 21.Solomon D, Davey D, Kurman R, et al. The 2001 Bethesda System: terminology for reporting results of cervical cytology. JAMA. 2002;287(16):2114–2119. doi: 10.1001/jama.287.16.2114. [DOI] [PubMed] [Google Scholar]
- 22.UNESCO ISCED International Standard Classification of Education. 2011. http://uis.unesco.org/sites/default/files/documents/international-standard-classification-of-education-isced-2011-en.pdf (accessed 3 Jul 2017)
- 23.Statistics Denmark. Documentation of statistics. Copenhagen: Statistics Denmark.; http://www.dst.dk/en/Statistik/dokumentation/documentationofstatistics/immigrants-and-descendants (accessed 3 Jul 2017) [Google Scholar]
- 24.Donner A, Klar N. Design and analysis of cluster randomization trials in health research. London: Arnold; 2000. [Google Scholar]
- 25.Lee J. Comparison of variance between correlated samples. Comput Appl Biosci. 1992;8(4):405–406. doi: 10.1093/bioinformatics/8.4.405. [DOI] [PubMed] [Google Scholar]
- 26.Dugue PA, Lynge E, Bjerregaard B, Rebolj M. Non-participation in screening: the case of cervical cancer in Denmark. Prev Med. 2012;54(3–4):266–269. doi: 10.1016/j.ypmed.2012.01.012. [DOI] [PubMed] [Google Scholar]
- 27.Lindau ST, Basu A, Leitsch SA. Health literacy as a predictor of follow-up after an abnormal Pap smear: a prospective study. J Gen Intern Med. 2006;21(8):829–834. doi: 10.1111/j.1525-1497.2006.00534.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.van Hamont D, van Ham MA, Struik-van der Zanden PH, et al. Long-term follow-up after large-loop excision of the transformation zone: evaluation of 22 years treatment of high-grade cervical intraepithelial neoplasia. Int J Gynecol Cancer. 2006;16(2):615–619. doi: 10.1111/j.1525-1438.2006.00404.x. [DOI] [PubMed] [Google Scholar]
- 29.Wang J, Andrae B, Sundström K, et al. Risk of invasive cervical cancer after atypical glandular cells in cervical screening: nationwide cohort study. BMJ. 2016 doi: 10.1136/bmj.i276. DOI: https://doi.org/10.1136/bmj.i276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.McCredie MR, Sharples KJ, Paul C, et al. Natural history of cervical neoplasia and risk of invasive cancer in women with cervical intraepithelial neoplasia 3: a retrospective cohort study. Lancet Oncol. 2008;9(5):425–434. doi: 10.1016/S1470-2045(08)70103-7. [DOI] [PubMed] [Google Scholar]
- 31.Drachmann TT, Storgaard L, Olesen F. Is change of general practitioners more frequent among patients diagnosed with cancer or other serious diseases? [In Danish] Ugeskr Laeger. 2003;165(27):2743–2746. [PubMed] [Google Scholar]