Introduction
Rural adults suffer disproportionately poorer health and worse health outcomes compared with urban-dwelling adults (Jaffe, 2015). Limited resources and access to care impact rural adults ability to receive timely management for both chronic and acute conditions (Gamm et al., 2002). Currently, only 10% of physicians practice in rural areas, while almost 20% of Americans live in these underserved rural areas (Barley, Reeves, O’Brien-Gonzales, & Westfall, 2001; US Census Bureau Geography, 2010). Additionally, lack of accessible specialists (Barley et al., 2001; Gamm et al., 2002) may lead to delayed detection of subtle health changes in rural older adults. The combination of higher prevalence of risk factors and limited access to care emphasizes the importance of early detection and diagnosis of specialist-managed health changes in this population.
Among older adults, changes in cognition represent a prime example of a health status alteration that may go undiagnosed or be diagnosed at later stages, particularly because late life cognitive changes may not initially appear to directly affect daily living. Specifically, early cognitive changes associated with Mild Cognitive Impairment (MCI) or early-stage Alzheimer’s disease (AD) may ensue insidiously, worsen over time and, ultimately, have profound implications for affected individuals’ ability to carry out daily activities. MCI is considered a likely prodromal state for dementia (e.g. AD, Petersen et al., 2001). A diagnosis of MCI is typically established in a specialty setting and 1) involves decline in at least one cognitive domain, 2) requires maintenance of near normal functional activities, and 3) requires that the degree of cognitive impairment is not sufficient to warrant a diagnosis of AD or related dementia (Gauthier et al., 2006; Petersen et al., 2001). While older adults with MCI are at greater risk than those without MCI for developing dementia, it is not clear that everyone who develops dementia passes through a well demarcated clinical syndrome of MCI (Mitchell & Shiri-Feshki, 2008, 2009).
Both those with MCI and early stage AD may benefit from early detection of cognitive decline. In the case of MCI, early detection of symptoms may trigger referral to a specialist for further evaluation and monitoring for evidence of progression to dementia. In the case of early AD, early detection is needed to ensure prompt access to current approaches in treatment which focus on maintenance of mental function, management of behavioral symptoms, and slowing or delaying the symptoms of disease (“About Alzheimer’s Disease: Treatment | National Institute on Aging,” n.d.).
Health status, including cognitive functioning, is widely recognized to be influenced by a host of factors, including social determinants of health (The Vision, Mission, and Goals of Healthy People 2020, 2011). Such factors may be of particular importance to rural-dwelling persons affected by MCI and early stage dementia. A systematic review examining factors contributing to missed and delayed diagnosis of dementias in primary settings found patient-related factors, as well as resource and financial system-related factors, to be significant contributors (Bradford et al., 2009).
The identification of perceived determinants of health may help promote identification of early cognitive changes and facilitate lifestyle modifications in underserved populations such as rural communities. For example, given emerging research on the potential cognitive benefits of diets like the Dietary Approaches to Stop Hypertension (DASH) eating plan (Appel LJ, Moore TJ, Obarzanek E, Vollmer WM, Svetkey LP, Sacks FM, Bray GA, Vogt TM, Cutler JA, Windhauser MM, Lin P-H, 1997), individuals who consume excessive quantities of saturated fats and processed foods may benefit from dietary modifications. Additionally, social support and family participation in daily life for one individual may promote an earlier diagnosis compared to someone with limited interactions with their community or family. In rural communities, identification of specific social determinants that may contribute to cognitive health in rural-dwelling adults may provide critical information for improving the long-term cognitive health of this already underserved group. The purpose of this study was to explore perceived social determinants of health among older, rural-dwelling adults with early-stage cognitive impairment.
Methods
Participants
Participants were drawn from a longitudinally followed cohort at an Alzheimer’s Disease Research Center (ADRC, P50 AG005133 PI: O. Lopez, MD). Inclusion criteria for the ADRC study were: >30 years of age, English speaker, >7 years of education, adequate visual and auditory acuity to complete neuropsychological testing, and a reliable care partner who is capable of providing information about the participant’s clinical symptoms. Additional inclusion criteria for the current study were ≥65 years of age and a current diagnosis of either 1) mild cognitive impairment (MCI) diagnosis based on Petersen et al. (2001) and Lopez et al. (2003) or 2) Probable Alzheimer’s disease (AD) diagnosis based on McKhann et al. (1984) with a Mini Mental Status Exam score of 18 or higher. This approach helped minimize the possibility that participants may have advanced cognitive symptoms, which may have impeded their ability to share their perceptions of social determinants of cognitive health. Purposive sampling was used to promote heterogeneity. Specifically, participant characteristics such as sex, degree of rurality, and relative degree of cognitive impairment were considered during recruitment to maximize diversity within the sample (Glaser & Strauss, 1967). United States Department of Agriculture Rural-Urban Commuting Areas Codes (RUCAs) were used to classify ZIP codes using codes from 1–10, where rural included primary RUCA codes 4–10 and included “micropolitan”, “small town”, and “rural areas” (US Department of Agriculture Economic Research Service, 2013). A list of identified rural ZIP codes across four states was provided to the ADRC coordinator, who identified individuals meeting the study inclusion criteria and then called to ask if they would be interested in participating in the study. If they agreed to be contacted by the study, the participant was then called by the study PI to present the study in greater detail. Family care partners of the participants with MCI or early-stage AD were concurrently recruited and invited to consent to the study and participate in the interviews. There were no exclusion criteria for care partners. Previous participation in ADRC activities helped promote trust in this sample beginning at first contact with the investigator.
The ADRC secures written informed consent from all participants for communication between annual visits, including permission for the ADRC recruitment coordinator to contact individuals via telephone about other ancillary studies. Once the ADRC coordinator identified potential participants, the investigator introduced this ancillary study to eligible participants and their care partners over the phone. Those participants who expressed interest in the study were scheduled for a home visit where the study was presented in detail and written informed consent was obtained from both participants with cognitive impairment and their care partners. Capacity to consent was assessed using questions from the University of California, San Diego Brief Assessment of Capacity to Consent (UBACC, Jeste et al., 2007). There were no indications of a lack of decisional capacity based on the UBACC during the consent process. University of Pittsburgh Institutional Review Board approved all procedures.
Design & Data Collection
Qualitative description (Sandelowski, 2000, 2010) was used to explore social determinants of health among older, rural-dwelling adults with early-stage cognitive impairment. The purpose of this approach was to explore beliefs and behaviors of individuals belonging to this culture-sharing group, older, rural-dwelling adults, and identify perceived social determinants of health for this population. We conducted semi-structured interviews in each participant’s home environment with the participant’s care partner present and participating in the interview. Prolonged engagement through home visits and extended interview length were used to cultivate a trusting relationship and meaningful data collection. Care partners were encouraged to participate in the interviews. In one interview, two care partners, husband and daughter, participated in the interview. While data from both of those care partners were included in the analysis, data from the corresponding participant was excluded. During the first 30 minutes of the interview the participant appeared to be confused and displayed frustration and distress requiring the interviewer to stop directing questions to her.
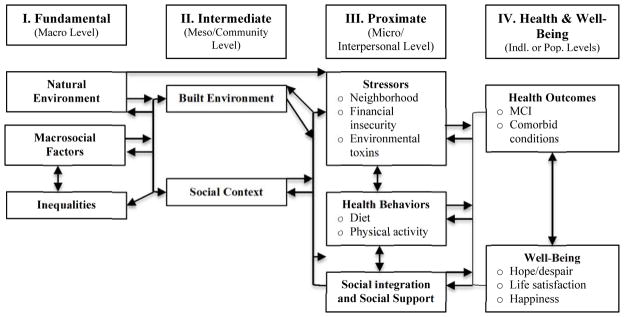
The interview guide consisted of fourteen semi-structured interview questions and was designed to allow for open dialogue among participants, care partners, and the investigator. The Social Determinants of Health and Environmental Health Promotion (SDH) Model proposed by Schulz and Northridge (2004) provided the scaffolding framework to guide interviews and participant observations, with a particular focus on gaining participant perspectives on promoting health at the community, interpersonal, and individual levels (as depicted by shading in Figure 1). Within the model, there are key factors contributing to health promotion including: environment, social context, health behaviors, social integration and support, and well-being. Four of the fourteen interview guide questions directly addressed concepts presented in the SDH model, and this was intentional as the guide wanted to refrain from leading participants to discuss the factors that may have been expected based on the model.
Figure 1.
Social Determinants of Health and Environmental Health Promotion Model
Adapted from Schulz and Northridge (2004)
Recorded interviews lasted 80 ± 9 minutes and ranged from 66–95 minutes in length; length of the individual home visit lasted 110 ± 23 minutes and ranged from 84–160 minutes. Interviews continued until data saturation, which included a total of nine interviews with participant-care partner dyads in Spring of 2015. One investigator interviewed all dyads and made observations before, during, and following the interviews. The investigator kept a reflexive journal to document decisions, processes, and reflections over the course of the study (Erlandson, 1993). Bracketing was acknowledged by the investigator from the beginning of study development through dissemination to separate individual biases or opinion from that which is actually observed (Sandelowski, 1986).
In addition, multiple data collection methods were applied to gain insight into cultural and social nuances that may not be captured in dialogue alone. Observations of both participants and their surroundings were used for the purpose of making a qualitative assessment of the social setting of the participant’s home and surrounding environment (Lofland, 1971). Through observation, the researcher observed what went on, who or what was involved, when and where things happened, how they occurred, and why things happened (Jorgensen, 1989; Malinowski, 1978). Events surrounding the interview, such as introductions and other observations, were captured by investigator home visit notes during and after the interview as described by (Pelto & Pelto, 1978). To ensure credibility (Beck, 1993), home visit notes from these interactions were reviewed and expanded to enhance recall following the interviews. Interviews and visit notes were transcribed and transcripts verified by a different person than the transcriptionist. Furthermore, the primary investigator listened to every tape and read all transcripts to ensure accurate transcription and checking.
Between interviews, comparative analyses were performed. Analysis of participant responses led to changes in the order of interview questions and the approach to asking the questions. Additionally, the investigator’s own actions, interactions, and behaviors were documented promptly following the interview, and reflexive journaling by the primary investigator was used to document these modified approaches to interviews and communication with participants.
Data Analysis
All transcribed data were transferred from a word processing program to Atlas.ti® (version 4.2, Scientific Software Development, Berlin). Data analysis used multiple techniques: line-by-line coding of transcriptions, data reduction (Huberman & Miles, 1998), data display (Miles & Huberman, 1994), emerging theme identification, and conclusion drawing/verification (Erlandson, 1993). First, the primary investigator (MM) line-by-line coded all interviews and three other independent researchers (JL, MN, & LH) line-by-line coded up to four interviews each. Consensus between investigators was reached for codes that emerged within each interview and among interviews. Following line-by-line coding consensus, categorized data were displayed in matrices so that the research team could examine potential patterns, regularities, or irregularities that point toward possible themes and relationships (Miles & Huberman, 1994). After categories were reduced and displayed, a team of four interdisciplinary investigators (MM, JL, AH, & AD), three from nursing and one from social work, met in-person to discuss themes and sub-themes, verify findings, and draw conclusions. It is important to note that the SDH model was not used to guide coding or category identification, but was later used as a way of organizing the themes and conclusions.
Results
Participants (n=9) with cognitive impairment were 73.7 ± 6.0 years of age with 14.2 ± 3.1 years of education; Mini-Mental State Examination 44.4% were female, 100% white, 88.9% married, and 100% lived with someone. Care partners (n=10) were 70.9 ± 7.4 years of age with 15.6 ± 2.3 years of education; 70% were female, 100% white, 80% married, and 90% lived with someone, specifically their care partner. Eight of the ten care partners were spouses (80%), one was a daughter, and one was a friend of over 30 years of the participant. In-home interviews took place across four states with RUCA codes across “micropolitan”, “small town”, and “rural areas” (RUCA codes 4.0, 4.2, 5.2, 7.4, 8.0, & 10.0).
Six themes emerged from the semi-structured interviews with the dyads: Staying active, Eating well, Living with cognitive changes, Living rural, Connecting with neighbors and community, and Relying on children. Of the 9 dyads, 4–8 contributed to each theme, with at least one counter example noted for each theme. Before describing the six themes, it is important to note that across eight of the nine interviews, conversation directing by members of the dyad was used to help guide conversation. Conversation directing refers to either 1) the participant or care partner’s attempt to redirect conversation back to the interview questions or away from certain topics or 2) allowing the other member of the dyad to contribute to the interview. Redirection by loved ones contributed to maintaining an open interview environment, and provided a buffer by which the interview could remain focused on the topics of interest. Examples of redirection back to interview questions include: “We better get back to the questions” and “Why don’t we get back to what we’re supposed to be doing?” Similarly, care partners would try and encourage the participant to talk or respond to prompts. For example, “What do you think? [The researcher] wants to know what you think.”
Staying Active
Staying active emerged as a major theme across eight of the nine interviews, and the value participants and care partners placed on staying active, whether in the context of growing older or in light of their diagnosis, was striking. Within the theme, Staying active, there also were two subthemes identified: staying physically active and staying mentally active. One subtheme, staying physically active, focused on physical ability and desire to be active. For example, a 65-year-old female care partner said of her husband with MCI, “He’s very – he’s very physical. He’s always doing something. He’s not the one to sit around and not do anything…anything he can go to when he’s home, he does...” Activities mentioned by participants ranged from taking walks alone to structured group classes at a local YMCA. On the other hand, a few care partners also shared concern that they believed either they or their loved one weren’t being physically active: “Sometimes it’s motivation or whatever and it’s stickin’ to it. And it’s easier not to bother” (68-year-old female care partner). Overall, a sense of personal responsibility and self-initiative came out through discussions of exercise by four of nine dyads.
There was also mention of staying mentally active to maintain brain and general health by six of the nine dyads. A 68-year-old female care partner said the dyad placed importance on “keeping interactive [with others].” Another example comes from a 69-year-old female with MCI who spoke about reading, “I read a lot in my book group… I do keep my brain, you know, as… active as I can.” Other activities members of the dyads presented to help promote mental activity included involvement in weekly church activities, puzzles (e.g., word finding and Sudoku), and playing cards. In contrast to these examples, there was a care partner who said keeping the “brain active” was important, but her husband with MCI did not: “And for him to keep his brain active…it’s a fight and I can’t get him to do it.” In the three cases that care partners spoke about lack of their loved one’s or their own mental activity, there was also the direct and indirect acknowledgement that promotion of brain or mental activity is good for one’s health.
Eating Well
Eating Well was identified as another major theme in interviews with two subthemes: 1) making healthy food selections and 2) avoiding chemicals and preservatives, which were typically presented during discussion of brain health. Seven of the nine dyads spoke about making, or trying to make, healthy food choices, and two dyads specifically mentioned how they make efforts to avoid chemicals and preservatives. Making healthy food selections, such as eating fruits and vegetables, was important to participants: “We’re healthy eaters… We try to be healthy eaters…we eat a lot of salads and fruit” (81-year-old male with AD). For one family, they noted that food choices changed after receiving an AD diagnosis: “And since this has happened to us, I’ve gotten into… it more.” Eating habits ranged from making recent efforts to improve food choices to modifying healthy eating habits adopted in the past.
In addition to healthy food choices, the avoidance of chemicals and preservatives in food emerged. A 67-year-old female care partner spoke about how her own health promotion-seeking led her to this decision:
“I was reading about [Alzheimer’s disease] and it said that sometimes it’s the preservatives in your meat, and I thought well we’re going to raise beef…That was just something that was very important to me. That way we know what’s going into them and that they aren’t being filled with preservatives and all the crap that they put in the meat.”
Another female care partner spoke to the maintenance of the family garden, “… we have our own garden and eat stuff that way so I can’t say that they’re necessarily be chemicals…it’s more natural or whatever, our own stuff.” The dyad’s choice to raise their own livestock or maintain a garden demonstrates the efforts undertaken to promote, what they consider to be, an important feature of healthy eating.
Participant’s emphasized healthy daily health behaviors, including staying active and eating well, related to both general and cognitive health. The importance placed on eating well and staying active, both physically and mentally, was apparent throughout interviews and highlights efforts to promote healthy lifestyles.
Living with cognitive changes
The theme, Living with cognitive changes, emerged and is described through three subthemes: loss/stressors, maintaining control, and symptom dismissal. Eight of the 9 dyads contributed to the theme, specifically 8/9 to loss/stressors, 6/9 to maintaining control, and 6/9 to symptom dismissal.
Dyads mentioned familial loss/stressors related to their well-being. One participant noted a current stressor: “My mother has nobody but me. Just me. There’s nobody in the family. I can’t imagine. Back then I didn’t—it didn’t register, what my mother was going through.” A care partner tried to provide some background information on her husband and said, “He lost his daughter, his one daughter…he lost her to cancer in [year]. And he also lost a grandson in a snowmobile accident …” Disclosure of life events and stressors throughout interviews was common and also illustrates the trusting relationship between the dyad and investigator.
Some participants and care partners described maintaining control when discussing their cognitive symptoms, while others reported feeling that their life course was out of their control. One participant presented feelings of control over current circumstances: “…anything I can do to prolong it or make it easier, that’s what I’m trying to do right” (73-year-old male with MCI). On the other hand, a 73-year-old female with MCI shared feelings that the diagnosis was out of her control, “I mean if I got it, I got it, you know? I didn’t ask for it; you know what I’m saying?” A 75-year-old male with AD, shared similar feelings, “We don’t know what caused it, so how could we tell you what we could have done to avoid it now?” Maintaining control was a pervasive theme throughout interviews, as evidenced by the positive health behaviors discussed as well as feelings of control of one’s life.
There also were forthcoming discussions of how to maintain control using available resources to minimize the impact of cognitive symptoms. However, there were two instances presenting concerns with quality and efficiency of medical care, specifically referring to inefficiency and frustration with doctors. During a recent visit to her primary care provider a 69-year-old female with MCI said, “And it was… the care is very frustrating.” On the other hand, resources included examples such as home health aides, family, friends, and adult day health centers.
The third subtheme, symptom dismissal, was highlighted through sarcasm and humor when participants discussed cognitive symptoms or events. For example, one participant made a joke about his memory concerns, and ended with “Well, I’m dying,” followed by laughter. Conversation about cognitive symptoms varied across interviews, however the way in which participants, in particular, dismissed and downplayed their own symptoms or disease trajectory provides insight into possible coping mechanisms for this population. Comments about pending or inevitable death following symptom dismissal jokes point to a viewing death as an inevitability as a potential way to help cope with these cognitive changes. Although participant symptom dismissal was noted across six dyad interviews, there also were a number of counter examples demonstrating participant or care partner acceptance, as presented in maintaining control.
Living Rural
Living rural emerged as another major theme in interviews, with participants consistently emphasizing the advantages over disadvantages of living in a rural area. Living rural was divided into advantages and disadvantages with subthemes for each. Seven of the nine dyads spoke to advantages of living in a rural area, while only two dyads spoke to the disadvantages.
Advantages of living rural
Overall, the majority of dyads spoke about the reasons why living further from the city or in a rural area was advantageous, and there were two subthemes: slower pace of life and a good place to raise children. Speaking to the rural lifestyle, a 67-year-old female care partner stated, “I’ll be perfectly honest with you – you know – you look at the crime rate and the traffic, and we just decided we were much happier at a slower pace.” Participants also spoke to problems with drugs “in town”, which influenced their decision to raise their family outside the city, as well as simply being “a good place to raise my kids” at the time they were married (65-year-old female care partner). Although only mentioned by two dyads, the pride and responsibility of having animals on their land also emerged. Participants shared that they owned and cared for cows on their land or enjoyed preparing food for seasonal hummingbirds. During discussion of caring for animals on their land, three dyads spoke to the “advantage of living where we do” for the outdoor work, green space, and open space.
Disadvantages of living rural
There were two subthemes within disadvantages of living rural: traveling longer distances by car and fracking. Traveling longer distances by car was identified by two participants as a disadvantage of living further away from a city when talking about why their friends do not want to travel to or live in a rural area. One 73-year-old female with MCI said, “…they don’t want to come…nothing going on [laughter], and, it’s like, it’s a wonderful place to live. Why wouldn’t you want to come?” Another 73-year-old female care partner said,
“…a lot of our peers, uhm, they think that [big city] is so far away and if they have to have something done, they would never go to [big city]. They’re afraid of it. They’re afraid of traffic.”
When distance from a city was mentioned, it was during discussion about what “other people” thought about living or visiting rural areas, our participants did not share their own stressors related to residence. There was also no mention by any dyad that traveling long distances in the car was a disadvantage to living in a rural area or a concern for accessing care. Only one dyad mentioned fracking, however the spontaneous mention of the impact of fracking on their immediate environment was notable. A 63-year-old female care partner said,
“… you feel like something is majorly on fire, which is, I mean there is. It’s glowing. You can see it for miles… and I talked to some people who are closer and they said they can actually hear this roaring rush when it’s burning off and it burned for days, week—I don’t know—it seemed forever that it burned. You know, it makes me uneasy…”
Not all dyads resided in areas that may be conducive to fracking, but for this one dyad, its impact was significant in that the care partner had conversations with other people that were also impacted or experienced the effects of fracking on nearby lands.
Relying on Children
The theme, Relying on children, emerged during discussion of daily or weekly activities, focusing on the supporting roles children play in their lives or their lack of involvement within the larger family. Some dyads (5/9) spoke about the reasons for and frequency of family-related events or visits with family. The majority of visits or attended events were with children or grandchildren, and for many dyads, family celebrations were mentioned as a source of joy. A 73-year-old female care partner spoke about her daughters as a resource for caring for her husband with early-stage AD when she had scheduled events to attend, “If I have to be somewhere overnight, one of the girls will come and stay overnight with them, with him [participant with early-stage AD].” Although most dyads with children had at least one child living nearby, one 81-year-old female with AD shared concerns that they did not have assistance from children because of distance: “We don’t have any kids around here to help us with. That’s our problem, see?” Of the two dyads that did not explicitly speak about their children or grandchildren, one was never married nor disclosed she had children, and the other dyad included a child of the participant. For the dyad that included the child, the daughter’s role in providing care to her mother and father was evidenced by the attendance and knowledge of her parent’s doctor’s appointments, coordination of care for her mother with early-stage AD, and concern for her parent’s well-being.
Connecting with Neighbors and Community
The theme, Connecting with neighbors and community, arose through discussion about the role the participant and/or his/her care partner play(s) in the community and identification or use of community resources by four dyads. One of the most striking statements speaking to sense of community was repeated by both members of a married couple who stated, “We have our own community.” Another 81-year-old female with AD spoke about the helpfulness and camaraderie of her neighbors, “all of us on this road are … real friendly and help each other.” There was, however, one counter example of note, a 62-year-old care partner who reported feeling that her family did not have adequate social resources, which she perceived as a disadvantage to the family: “All these people [my parents] took care of for years and years and they’re all gone and there isn’t the resources of people that’ll come.” Three dyads spoke explicitly about relationships with their neighbors or larger community, and there was only one example of a lack of this connection. It was also notable that no participants were currently involved or participating in any AD support groups.
Discussion
Semi-structured interviews with older, rural-dwelling adults with early cognitive changes and their care partners focused on adopting a healthy lifestyle, describing relationships with others, and living in rural areas. Correspondence was noted between many of the emergent themes in the study and those factors outlined in the Social Determinants of Health and Environmental Health Promotion Model (SDH, Schulz & Northridge, 2004), however there were also themes, such as Living with cognitive changes, that were specific to the participants’ current diagnoses and did not clearly correspond with determinants found in the SDH model.
Correspondence with the Social Determinants of Health and Environmental Health Promotion Model
Themes, Staying active and Eating well, that emerged from interviews with dyads highlight the importance of how health behaviors, such as physical/mental activity and eating habits, are related to and promote health and well-being. Both Staying active and Eating well appear in the SDH model under health behaviors as “Dietary practices” and “Physical Activity,” and classified under the interpersonal level or proximate level. Participants and care partners that attend the ADRC receive suggestions and information from the ADRC to promote health and try to reduce AD risk factors, hence, health behaviors mentioned in interviews may reflect information provided to participants during an ADRC visit or subsequent follow-up on their own. A previous study also noted these positive lifestyle changes in self-initiated health behaviors following a cognitive diagnosis (Morgan, Garand, & Lingler, 2012). Although our study did not probe for details about participant or care partner’s nutrition and physical activity, these topics have been explored in the literature. For example, a previous study in a rural and remote memory clinic found that of 260 adults with non-amnestic MCI or amnestic MCI, only about 4% reported exercising the recommended amount and frequency each week and less than a 20% reported meeting Canada’s Food Guide recommendations (Dal Bello-Haas, Connell, & Morgan, 2014). The same study showed that those with AD or other non-AD dementias had higher rates of recommended exercise and nutrition compared to those at earlier stages of cognitive impairment, despite the possibility that those in earlier stages may benefit even more from lifestyle interventions (Dal Bello-Haas et al., 2014). It is encouraging that our participants voiced proactive efforts to improve nutrition and exercise frequency. Follow-up inquiry into quantifiable diet and nutritional intake as well as measured exercise could provide both further clarification as to what it means to “eat healthy” and “stay active.” This is important for practitioners to both 1) know what people perceive as eating healthy and staying active and 2) be able to provide input or guidance for reaching or maintaining balanced energy intake/output.
The theme, Living rural, mirrored the SDH concept of “Built Environment,” and emerged in discussions that emphasized the advantages and downplayed the disadvantages of living in a rural area. Within the SDH model, the built environment includes physical or material buildings or structures, as well as other aspects such as the presence or adoption of a slower or positive environment that were mentioned in the study. The “Built Environment” is considered a community level determinant of health and includes considerations such as land use or transportation systems, which may impact rural residents in particular. For example, the lack of public or private transportation systems needed access to health care providers and services may delay routine medical visits for rural residents, as well as cognitive screenings or follow-up appointments by specialists typically working in city centers (Barley et al., 2001; US Census Bureau Geography, n.d.).
Themes, Connecting with neighbors and community and Relying on children, aligned conceptually with “Social Integration and Support” and highlight the importance of social connectedness. For example, family, community, and church events played a recurring role in weekly activities for most dyads. These interactions and planned events through spending time with friends or family promote feelings of connectedness with others and promote engagement in daily activities (Han, Radel, McDowd, & Sabata, 2015), which may promote cognitive and mental health. A study conducted by DiNapoli, Wu, and Scogin (2014) among older, Appalachian adults found that social isolation, social disconnectedness, and perceived isolation predicted worse cognitive functioning and neuropsychological testing. When distance, time, or circumstance may not permit in-person meetings or events, technology may be a potential accompanying tool to promote social connections in persons living with early cognitive and their care partners.
Stressors
A particularly interesting finding was that there was limited mention of stressors, another key concept in the SDH model, by participants or care partners. The absence of talk concerning stressors was noted to be in direct contrast to frequent and forthcoming discussions of resources and other factors that serve as buffers to the strain imposed by cognitive symptoms during interviews. Although interview questions did not ask explicitly about possible stressors, such as finances, this was something that investigators believed would emerge through prolonged engagement with participants and open discussion about a variety of topics. Instead dyads spoke to how they live with cognitive changes, such as through positive lifestyle changes or attitude. Previous research has presented how certain traits in rural adults, such as stoicism and resilience, which may help explain the absence of mention of stressors and focus on what can be changed for this population (Ford, Wong, Jones, & Steel, 2016).
None of the care partners of family members with AD were attending a formal AD support group. There are several explanations as to why care partners were not currently involved. One reason may be because of the requirement to travel longer distances to meet with other care partners in a group setting, thus limiting face-to-face meetings. Traveling greater distances to access health care has been presented in the literature as an important determinant of health (AHRQ, 2005; Hunter & Wilson, 2012), however, travel was not mentioned as a stressor or limiting factor for receiving medical services or support networks, such as AD support groups, by any participants or care partners. Another reason may be that dyads prefer to retain their privacy within small communities and not share cognitive diagnosis or daily struggles with others who could then share this information within social circles in a small rural community. Finally, there may be a lack of resources to create and maintain formal in-person support groups in rural areas, particularly for individuals with MCI, which is a less commonly applied diagnosis than AD. Connecting with support groups via the Internet have been shown to reduce rural-dwelling caregiver’s feelings of isolation (Blusi, Kristiansen, & Jong, 2015), and should be considered as an option to improve social connections and build support systems where in-person support groups may not be possible or desirable. The Alzheimer’s Association also offers online message boards and chat rooms (Alzheimer’s Association, 2016) that allows for anonymity and accessibility for those with privacy or travel concerns.
One limitation of the study is that there may be selection bias as dyads were recruited from a research center, possibly limiting true purposive sampling of this population and leading to a lack of heterogeneity in the sample. For example, dyads in this study were very highly educated and participants involved in research may be more information seeking than those who do not participate in research. There is likely also variability in the time since diagnosis, which may influence how participants identify their current health state and possibly how they do or do not modify their activities of daily living. However, this study provides unique insight into the perceived social determinants of health as presented by older, rural-dwelling adults with early cognitive impairment and their care partners that may be used to improve cognitive and overall health in this underserved population. Identification of social determinants have policy implications as they provide a target for concentrating resources in efforts to improve health equity for rural-dwelling adults. Findings reinforce the need for a policy change to provide and extend support of much-needed services to rural-dwelling Americans dealing with cognitive concerns through creating awareness, providing access to services, and managing initiatives at a national level.
Conclusion
Through interviews with older, rural-dwelling adults with early cognitive impairment, we identified themes corresponding to social determinants of health, descriptions of how dyads cope with illness, and minimal mention of stressors. Our findings help contribute to creating a better foundation to understand rural health disparities for this population, and further inquiry into rural cognitive health should be explored in greater detail in the future. Specially, future research should consider examining perceived determinants of health prior to cognitive impairment diagnosis, focusing on health behaviors, social integration and support and how these may change after a cognitive impairment diagnosis. This may provide crucial information about where to focus education and intervention work before or at the time of cognitive impairment diagnoses. The emergent themes, specifically those corresponding to established social determinants of health, may be used to promote the adoption of self-management and prevention behaviors, particularly lifestyle changes such as nutrition and exercise. Practitioners may consider providing education and directing resources related to diet and physical activity as well as health-related transport services to dyads dealing with early or possible cognitive changes.
Footnotes
Disclaimer: The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
The Authors declare that there is no conflict of interest.
References
- About Alzheimer’s Disease: Treatment. National Institute on Aging; n.d. Retrieved August 7, 2013, from http://www.nia.nih.gov/alzheimers/topics/treatment. [Google Scholar]
- AHRQ. Fact Sheet, AHRQ Pub No. 05-P022. 2005. Health Care Disparities in Rural Areas Selected Findings From the 2004 National Healthcare Disparities Report. [Google Scholar]
- Alzheimer’s Association. Support Groups. 2016 Retrieved July 19, 2016, from http://www.alz.org/apps/we_can_help/support_groups.asp.
- Appel LJ, Moore TJ, Obarzanek E, Vollmer WM, Svetkey LP, Sacks FM, Bray GA, Vogt TM, Cutler JA, Windhauser MM, Lin P-HKN. A Clinical Trial of the Effects of Dietary Patterns on Blood Pressure. The New England Journal of Medicine. 1997;336(16):1117–1124. doi: 10.1056/NEJM199704173361601. [DOI] [PubMed] [Google Scholar]
- Barley GE, Reeves CB, O’Brien-Gonzales A, Westfall JM. Characteristics of and Issues Faced by Rural Female Family Physicians. Journal of Rural Health. 2001;17(3):251–258. doi: 10.1111/j.1748-0361.2001.tb00962.x. [DOI] [PubMed] [Google Scholar]
- Beck C. Qualitative Research: The evaluation of its credibility, fittingness and auditability. WJNR. 1993;15:263. doi: 10.1177/019394599301500212. [DOI] [PubMed] [Google Scholar]
- Blusi M, Kristiansen L, Jong M. Exploring the influence of Internet-based caregiver support on experiences of isolation for older spouse caregivers in rural areas: a qualitative interview study. International Journal of Older People Nursing. 2015;10(3):211–20. doi: 10.1111/opn.12074. [DOI] [PubMed] [Google Scholar]
- Bradford A, Kunik ME, Schulz P, Williams SP, Singh H, Mph J. Missed and Delayed Diagnosis of Dementia in Primary Care Prevalence and Contributing Factors. Alzheimer Disease & Associated Disorders. 2009;23(4):311–314. doi: 10.1097/WAD.0b013e3181a6bebc. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dal Bello-Haas VPMD, Connell MEO, Morgan DG. Maintaining health and wellness in the face of dementia: an exploratory analysis of individuals attending a rural and remote memory clinic. Rural and Remote Health. 2014;14(3):1–16. [PubMed] [Google Scholar]
- DiNapoli EA, Wu B, Scogin F. Social Isolation and Cognitive Function in Appalachian Older Adults. Research on Aging. 2013;36(2):161–79. doi: 10.1177/0164027512470704. [DOI] [PubMed] [Google Scholar]
- Erlandson D. Quality Criteria fo a Naturalistic Study. In: Erlandson D, editor. Doing Naturalistic Inquiry: A Guide to Methods. London: Sage Publications; 1993. [Google Scholar]
- Ford JA, Wong G, Jones AP, Steel N. Access to primary care for socioeconomically disadvantaged older people in rural areas: a realist review. BMJ Open. 2016;6 doi: 10.1136/bmjopen-2015-010652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gamm L, Hutchison L, Bellamy G, Dabney BJ. Rural Healthy People 2010: Identifying Rural Health Priorities. The Journal of Rural Health. 2002;18(1):9–14. doi: 10.1111/j.1748-0361.2002.tb00869.x. [DOI] [PubMed] [Google Scholar]
- Gauthier S, Reisberg B, Zaudig M, Petersen RC, Ritchie K, Broich K, … Winblad B. Mild cognitive impairment. Lancet. 2006;367:1262–1270. doi: 10.1016/S0140-6736(06)68542-5. [DOI] [PubMed] [Google Scholar]
- Glaser BG, Strauss AL. The Discovery of Grounded Theory: Strategies for Qualitative Research. Chicago: Aldine; 1967. [Google Scholar]
- Han A, Radel J, McDowd JM, Sabata D. Perspectives of People with Dementia About Meaningful Activities: A Synthesis. American Journal of Alzheimer’s Disease and Other Dementias. 2015;98(4) doi: 10.1177/1533317515598857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huberman AM, Miles MB. Collecting and Interpreting Qualitative Materials. Thousand Oaks: Sage Publications; 1998. Data Management and Analysis Methods; pp. 179–210. [Google Scholar]
- Hunter D, Wilson J. Promoting health equity. BMJ. 2012;345(aug08 1):e4881–e4881. doi: 10.1136/bmj.e4881. [DOI] [PubMed] [Google Scholar]
- Jaffe S. Aging in rural America. Health Affairs. 2015;34(!):7–10. doi: 10.1377/hlthaff.2014.1372. [DOI] [PubMed] [Google Scholar]
- Jeste DV, Palmer BW, Appelbaum PS, Golshan S, Glorioso D, Dunn LB, … Kraemer HC. A new brief instrument for assessing decisional capacity for clinical research. Archives of General Psychiatry. 2007;64(8):966–974. doi: 10.1001/archpsyc.64.8.966. [DOI] [PubMed] [Google Scholar]
- Jorgensen D. Participant Observation: A Methodology for Human Studies. Newbury Park: Sage Publications; 1989. [Google Scholar]
- Lofland J. Analzying Social Settings: A Guide to Qualitative Observation and Analysis. Belmont: Wadsworth Publishing Co; 1971. [Google Scholar]
- Lopez OL, Jagust WJ, DeKosky ST, Becker JT, Fitzpatrick A, Dulberg C, … Kuller LH. Prevalence and classification of mild cognitive impairment in the Cardiovascular Health Study Cognition Study: part 1. Archives of Neurology. 2003;60(10):1385–9. doi: 10.1001/archneur.60.10.1385. [DOI] [PubMed] [Google Scholar]
- Malinowski B. Argonauts of the Western Pacific. In: Pelto PJ, Pelto GH, editors. Anthropological Research: The Structure of Inquiry. Cambridge: Cambridge University Press; 1978. p. 68. [Google Scholar]
- McKhann G, Drachman D, Folstein M, Katzman R, Price D, Stadlan EM. Clinical diagnosis of Alzheimer’s disease: report of the NINCDS-ADRDA Work Group under the auspices of Department of Health and Human Services Task Force on Alzheimer’s Disease. Neurology. 1984;34(7):939–944. doi: 10.1212/wnl.34.7.939. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/6610841. [DOI] [PubMed] [Google Scholar]
- Miles MB, Huberman AM. Qualitative Data Analysis: An Expanded Sourcebook. 2. Thousand Oaks: Sage Publications; 1994. [Google Scholar]
- Mitchell AJ, Shiri-Feshki M. Temporal trends in the long term risk of progression of mild cognitive impairment: a pooled analysis. Journal of Neurology, Neurosurgery, and Psychiatry. 2008;79(12):1386–91. doi: 10.1136/jnnp.2007.142679. [DOI] [PubMed] [Google Scholar]
- Mitchell AJ, Shiri-Feshki M. Rate of progression of mild cognitive impairment to dementia - Meta-analysis of 41 robust inception cohort studies. Acta Psychiatrica Scandinavica. 2009;119(4):252–265. doi: 10.1111/j.1600-0447.2008.01326.x. [DOI] [PubMed] [Google Scholar]
- Morgan GH, Garand LI, Lingler JH. Self-initiated health behaviors following a diagnosis of mild cognitive impairment. Research in Gerontological Nursing. 2012;5(2):94–100. doi: 10.3928/19404921-20110831-02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pelto PJ, Pelto GH. Anthropological Research: The Structure of Inquiry. Cambridge: Cambridge University Press; 1978. [Google Scholar]
- Petersen R, Doody R, Kurz A, Mohs R, Morris J, Rabins P, … Wingblad B. Current Concepts in Mild Cognitive Impairment. Arch Neurol. 2001;58:1985–1992. doi: 10.1001/archneur.58.12.1985. [DOI] [PubMed] [Google Scholar]
- Sandelowski M. The problem of rigor in qualitative research. Adv Nurs Sci. 1986;8(3):27–37. doi: 10.1097/00012272-198604000-00005. [DOI] [PubMed] [Google Scholar]
- Sandelowski M. Focus on Research Methods: Whatever Happened to Qualitative Description? Research in Nursing & Health. 2000;23:334–340. doi: 10.1002/1098-240x(200008)23:4<334::aid-nur9>3.0.co;2-g. [DOI] [PubMed] [Google Scholar]
- Sandelowski M. What’s in a name? Qualitative description revisited. Research in Nursing & Health. 2010;33(1):77–84. doi: 10.1002/nur.20362. [DOI] [PubMed] [Google Scholar]
- Schulz A, Northridge ME. Social determinants of health: implications for environmental health promotion. Health Education & Behavior. 2004;31(4):455–71. doi: 10.1177/1090198104265598. [DOI] [PubMed] [Google Scholar]
- The Vision, Mission, and Goals of Healthy People 2020. 2011 Retrieved from http://www.healthypeople.gov/2020/
- US Census Bureau Geography. 2010 Census Urban and Rural Classification and Urban Area Criteria. n.d Retrieved from https://www.census.gov/geo/reference/ua/urban-rural-2010.html.
- US Department of Agriculture Economic Research Service. Rural Urban Commuting Area Codes Data. 2013 Retrieved September 27, 2013, from http://depts.washington.edu/uwruca/ruca-demographics.php.