Abstract
Background
Spouses’ ability to care for survivors can be particularly challenging because patients and spouses are interdependent and mutually influence one another. Family functioning such as family cohesion and communication may play a primary role in improving the health-related quality of life (HRQOL) of couples, given that cancer can influence family dynamics.
Objective
to investigate the mediating effect of family communication on the relationship between family cohesion and HRQOL and examined the moderating effect of sex on this relationship among cancer survivor-spouse dyads.
Methods
A total of 91 cancer survivors diagnosed with breast, colorectal, or prostate cancer and their spouses were recruited from the University Hospital Registry in Cleveland, Ohio. The dyadic data were analyzed using structural equation modeling with the actor-partner interdependence mediation model.
Results
Findings demonstrated that the spouses’ own perceived family communication mediated the associations between their own family cohesion and physical HRQOL and between the survivors’ family cohesion and physical HRQOL. The spouse actor effects between family communication and HRQOL significantly differed by sex.
Conclusions
Enhancing family cohesion and communication within the family can improve the spouses’ HRQOL. Findings regarding sex differences serve as a rationale for gender-based approaches to improving HRQOL in survivorship care in the family context.
Implications for Practice
Couple- and/or family-based interventions should be designed to enhance family cohesion and improve family communication skills for effective adjustments within couples and families. Supportive care within the family context can be promoted to address the diverse challenges of survivorship care.
INTRODUCTION
Nearly 14.5 million individuals in the United States were living with a history of cancer in 2014.1 Some of these individuals, often called cancer survivors, were diagnosed many years ago and no longer had evidence of cancer. Due to the earlier diagnosis of cancers and improvements in treatment, the 5-year relative survival rate for all cancers increased from 49% in 1975–1977 to 68% in 2004–2010.1 As the number of cancer survivors continues to grow, family caregivers’ ability to care for survivors can be particularly challenging because patients and family caregivers are interdependent and mutually influence one another.2
Generally, family members provide diverse types of support, including emotional, financial, and functional support, while cancer patients are facing cancer and even years after the completion of cancer treatment. Given that the experience of cancer is a long journey, a cancer diagnosis adversely affects not only those diagnosed but also family members, especially spouses who provide primary care. Several studies found that family caregivers show worse health-related quality of life (HRQOL) than normative samples during the treatment phases and even during the survivorship phase.3,4 More specifically, spouses are more likely than other family members to experience greater burden, strain, and distress.5
Previous research has suggested that the HRQOL of one spouse may directly and/or indirectly influence the other spouse throughout all phases of cancer; this phenomenon is known as “spillover”. Because couples tend to react as an emotional unit,2,6 the effect of cancer on a spouse can spill over to affect the other partner and, thus, can affect both the cancer survivors’ and the spouses’ adaptation to cancer-related distress.2,7 Several researchers have demonstrated that couples have a mutual impact on each other’s HRQOL.8,9 These findings suggest that survivors and spouses should address the practical issues that they may face throughout the cancer journey together.10 Thus, the current study focuses on survivor-spouse dyads, rather than the individual experiences of survivors or spouses, to examine couples’ HRQOL after cancer treatment.
Given that cancer is a family illness and can influence family dynamics,11,12 family functioning may play a primary role in improving the HRQOL of couples. Although there is some evidence that spousal support contributes to HRQOL,13 little is known about which aspects within the family system are associated with HRQOL. The current study examines whether an individual’s emotional bond to any other person within the family, called “family cohesion,” is associated with the HRQOL of couples. Family cohesion refers to “the emotional bonding that family members have toward one another”14 and depends on how systems balance their separateness versus togetherness. Members in highly cohesive families tend to unite to resolve their problems and thus provide mutual support; therefore, they expect to experience better HRQOL.15,16 Although positive associations between family cohesion and HRQOL among children with other health conditions are now better understood,17 these associations among cancer survivor-spouse dyads remain unclear.
Family communication, which refers to the way verbal and non-verbal information is exchanged between family members,18 is another important aspect of family functioning that affects the success of the relationship between cancer survivors and their spouses.19 Previous studies have suggested that a family’s clear and open communication during a traumatic event can improve cancer survivors’ HRQOL,20 while cancer survivors who avoided conversation with their spouses showed poorer adjustment.21 According to the Circumplex Model, which focuses on the three dimensions of family systems including family cohesion, flexibility, and communication, communication facilitates family cohesion.22 However, it is not clear how family communication facilitates family cohesion. Nevertheless, we expect that families that are emotionally closer may effectively communicate to cope with stressors and, in turn, improve HRQOL; it indicates the mediating effect of family communication to clarify the nature of the relationship between family cohesion and HRQOL. Previous studies have found that the openness of communication regarding cancer beyond family communication patterns in daily life is associated with better HRQOL.23,24 Thus, in the current study, cancer-related communication was controlled to obtain a full understanding of the impact of family communication.
Although family cohesion and communication are important variables for understanding the dynamics and functioning within the family, survivors and their spouses may have different perceptions of cohesion and communication. Several studies reported that most patients and family caregivers express a desire for better and more concordant communication, indicating that they frequently have conflicting and unmet communication needs within families.24–27 Thus far, researchers have not given sufficient attention to the mutual influences of family cohesion and communication between survivors and spouses. Moreover, the mediating effect of family communication on the relationship between family cohesion and HRQOL among cancer survivor-spouse dyads has rarely been examined.
According to Social Role Theory,28 gender role expectations and cultural norms cause men and women to behave and communicate differently. While sex refers to biological differences, gender describes the characteristics that a society or culture delineate as masculine or feminine.29 Typically, women are interpersonally oriented and pay attention to others’ emotions, while men are task-oriented in their interactions and focus on problem solving.30,31 Given specified male and female roles are thought to contribute directly to most social behavior differences between men and women, that is the stereotypes of their social roles,32 the current study examines sex differences in the relationships among family cohesion, communication, and HRQOL. In addition to sex differences, whether one is the cancer survivor or the spouse can be an important indicator of family cohesion and communication, suggesting that the role of survivor versus spouse, as well as sex, should be considered.33 Lim et al.33 found differences in family communication between male survivor-female partner and female survivor-male partner couples. This study indicated that male survivors tended to avoid initiating discussions about cancer-related issues, while male partners of breast cancer survivors were likely to initiate cancer-related communication to solve problems. Such findings imply that a moderating effect of the role of survivor versus spouse and sex may exist specifically for family communication, suggesting that the relationship between variables including family communication depends on the role or sex. Because the current study addresses the dyadic relationships among family cohesion, family communication, and HRQOL in survivor-spouse couples, the inclusion of the moderating role of sex will simultaneously reflect whether the role of the survivor versus the spouse moderates the relationships among the study variables.
The purpose of the current study is to investigate the mediating effect of family communication on the relationship between family cohesion and HRQOL and to examine the moderating effect of sex on this relationship among cancer survivor-spouse dyads. The Circumplex Model22 helps illustrate why family communication mediates the relationship between family cohesion and HRQOL, and Social Role Theory28 provides the theoretical lends which we study the moderating effect of sex. The primary study intended to investigate the relationships among family resilience, family communication, and coping for European- and African-American cancer survivors diagnosed with breast, colorectal, or prostate cancer and their spouses in Cleveland, Ohio.34 Thus, this study expands upon the primary study by focusing on the family context and sex/gender effect. The current study tests the following hypotheses:
Hypothesis 1 (H1). Own and/or the partner’s higher perceived family cohesion is related to one’s and/or the partner’s higher perceived family communication, which is, in turn, positively associated with one’s own and/or the partner’s HRQOL.
Hypothesis 2 (H2). The dyadic relationships among family cohesion, family communication, and HRQOL differ by sex.
METHODS
Data Source and Participants
The current study is a secondary analysis of data gathered for a cross-sectional study entitled “Promoting family resilience among cancer survivors and their partners.” The study was approved by the Institutional Review Board.
The eligibility criteria for cancer survivors included the following: 1) 18 years of age or older at cancer diagnosis; 2) within 1–5 years of breast, colorectal, or prostate cancer diagnosis (stages I–III); 3) completion of active treatment (i.e., surgery, chemotherapy, or radiation therapy); 4) self-identification as European-American or African-American, and 5) living with a spouse who had not been diagnosed with any type of cancer at the time of cancer diagnosis. Survivors with a major disabling medical (e.g., stroke) or psychiatric (e.g., schizophrenia) diagnosis, in stage IV of the disease, or with other cancer diagnoses were not eligible. Spouses who had been living with a cancer survivor at the time of cancer diagnosis, and had not been diagnosed with any type of cancer were eligible.
Data Collection Procedures
Methodological details, such as sampling and data collection procedures, have been reported elsewhere.34 In short, the participants were first identified from the University Hospital Cancer Registry in Cleveland, OH. Potential participants whose contact information was obtained from the registry received invitation letters and were then contacted by an ethnically matched research assistant (RA). The RAs made follow-up calls to confirm potential participants’ interest and to conduct a screening to assess eligibility. If a survivor agreed to invite her/his spouse to participate during the screening process, her/his preferred method for contacting her/his spouse was recorded. If the survivor did not agree to her/his spouse’s participation, the survivor and the partner were not included in the study. Both survivors and spouses who were eligible and agreed to verbally consent to participating in the study over the phone received a questionnaire and a consent form and were asked to return them within 3 weeks. Participants received a $20 gift certificate as compensation.
Instruments
Health-related quality of life (HRQOL)
HRQOL was assessed using the Medical Outcome Study (MOS) SF-36, which is a 36-item self-report HRQOL measure for both ill and healthy populations.35 The SF-36 consists of 8 subscales, including 1) physical functioning, 2) physical limitation, 3) pain, 4) general health perception, 5) vitality, 6) social functioning, 7) emotional limitation, and 8) mental health. Each subscale score was calculated by summing the items and transforming the raw scale scores into standardized scores; higher scores indicate better physical and mental HRQOL. In this study, the two summary scores, the Physical Component Summary (PCS) and the Mental Component Summary (MCS), were used as outcomes. Summary scores were obtained by averaging the corresponding subscales. The reliability coefficients for the subscales ranged from 0.83 to 0.92 for survivors and from 0.83 to 0.90 for spouses.
Family cohesion
The Family Adaptability and Cohesion Evaluation Scales-III(FACES-III) was used to assess family cohesion.14 The FACES-III is a 20-item standardized family functioning instrument that was developed to assess families’ cohesion.36 In the current study, 9 items of the FACES-III family cohesion subscale were used. The family cohesion score was obtained by averaging items, and high scores reflected positive functioning in terms of family cohesion. The reliability coefficients were 0.75 for survivors and 0.79 for spouses.
Family communication
The Family Adaptability and Cohesion Evaluation Scales(FACES-IV)-Family Communication Scale, which was designed to investigate the functionality of communication within the family,37 was used to assess family communication. Responses to this 10-item self-report measure were provided on a 5-point Likert scale. The communication score was obtained by averaging the 10 items; higher scores indicate better family communication. The reliability coefficient was 0.90 for both survivors and spouses.
Cancer-related communication
The Cancer Communication Assessment Tool for Patients and Families (CCAT-PF) was used to assess cancer-related communication. The CCAT-PF was developed to measure the level of communication concordance/discordance between patients and family caregivers.24 The CCAT-PF scores are obtained after combing two components: 1) an 18-item questionnaire completed by the patient (CCAT-P) and 2) an 18-item questionnaire completed by the family (CCAT-F). The respondents rated items on a 5-point Likert scale; higher scores indicate better communication regarding cancer. The CCAT-PF scores, which are calculated from the CCAT-P and the CCAT-F, range from 0 to 90, with higher scores indicating greater conflict. In this sample, the reliability coefficients were 0.73 for survivors and 0.65 for partners.
Demographic and medical characteristics
Demographic and medical characteristics such as age, sex, income, education, cancer type, cancer stage, types of cancer treatment, and comorbidities were obtained using a self-administered questionnaire.
Data Analyses
Power analysis
As measured by the power analysis program,38 the hypothesis-testing framework of the root mean square error of approximation (RMSEA) was used to calculate the power. Given a α = .05, a null hypothesis RMSEA of 0.05, an alternative hypothesis RMSEA of 0.10, and degree of freedom ranging from 20 to 50, the range of statistical power given a sample size of 91 is between 0.82 and 0.89; thus the model showed moderate power.
Preliminary analysis
Descriptive statistics were conducted to describe the sample characteristics. Chi-square tests were used to examine the association between variables, and independent samples t-tests were conducted to investigate the mean differences in variables by sex. Before conducting dyadic analyses, correlation analyses were used to evaluate the degree to which the survivors and spouses within dyads provided similar reports for the study variables. Mean differences in predictor and outcome variables between survivors and spouses were examined by paired-samples t-tests. The analyses were conducted using SPSS 20.0.
Hypotheis 1
The Actor-Partner Interdependence Mediation Model (APIMeM) was performed to assess the mediation effect of family communication on the relationship between family cohesion and HRQOL in the dyadic data.39 The APIMeM examines actor and partner effects. Actor effects are defined as “estimates of an individual’s effects on herself or himself, and partner effects are “the degree to which a person’s outcome is influenced by their partner’s scores on the variable.”39 To test H1, the APIMeM was performed to examine the relationship between family cohesion and HRQOL as mediated by family communication using structural equation modeling (SEM) in AMOS 20.0. The hypothesized model was evaluated using goodness of fit indices, including the chi-square statistic or discrepancy function, the ratio of the discrepancy function to the number of degrees of freedom, RMSEA (acceptable fit≤0.08),40 and the comparative fit index (CFI; acceptable model fit≥0.9).41
Hypothesis 2
The moderating effect of sex was tested to investigate whether the relationships among variables in the dyadic data differ by survivors’ sex (H2) using the SEM multiple group analysis.42,43 Initially, all parameters for male and female groups were unconstrained (i.e., baseline model; two groups will be different). Then, structural paths were constrained to test for structural invariances, which assume that two groups will be equivalent. Two unconstrained and constrained models were compared by computing a chi-square difference test. A significant difference in chi-square values indicates that there are differences in the structural models between male and female survivors. Critical ratios (CRs) for differences tests were conducted to examine differences in all direct effect parameters according to sex.
Methodological issues
To conduct SEM, methodological issues were addressed. First, methods to handle missing values were evaluated. Less than 1% of the values in our dataset were missing. Thus, full information maximum likelihood estimation was used.44 Second, the relationships between variables were specified based on the conceptual model. Third, covariates were determined based on previous studies and findings. Given that family communication is significantly associated with cancer-related communication,45 a cancer-related communication was controlled to investigate the true effect of family communication. Additionally, the survivors’ physical HRQOL was significantly related to the survivors’ number of comorbidities; thus, the number of comorbidities was included as a covariate in the final model. Finally, the corresponding variables between survivors and spouses were allowed to correlate with one another.
RESULTS
Sample Characteristics
Of the 950 potential participants to whom recruitment letters were mailed, 241(25.4%) were not accessible because they did not respond to the letters or follow-up telephone calls or because their contact information was incorrect. Of the 709 accessible survivors approached for this study, 296 refused to participate (41.7%), 109 were not eligible to participate (15.4%), and 35 agreed to participate but did not complete the survey (4.4%). As well, the first and second phone calls failed to reach 166 survivors, and additional calls were not made due to the timeline of the study. Twelve additional survivors were excluded because their spouses did not agree to participate. Thus, a total of 91 couples completed the survey.
The final sample of survivors included 74 European-Americans and 17 African-Americans. The mean age of the participants was 64 years. Approximately 64% of survivors were male. Nearly one-half of the participants were diagnosed with prostate cancer, 31% of the participants had breast cancer, and 20% of the participants had colorectal cancer. The mean time since cancer diagnosis was approximately 3.7 years. Male survivors were more likely than female survivors to be employed, to have been diagnosed with stage II prostate cancer, to have undergone surgery, and to be older.
In terms of the dyadic correlation, couples reported moderate levels of family cohesion, family communication, and HRQOL (0.31≤r≤0.49). For survivors, family cohesion and communication were not significantly associated with HRQOL (0.03≤r≤0.19). For spouses, family communication was significantly associated with HRQOL, while family cohesion was not associated with physical QOL only. A paired-samples t-test showed that family cohesion, family communication, and HRQOL scores were not significantly different between couples.
Hypothesis Testing
The mediating effect of family communication (Hypothesis 1)
For physical HRQOL, both survivor and spouse actor effects between family cohesion and communication were observed, i.e., individuals’ increased perception of family cohesion was related to their own higher perceived family communication. The spouse partner effect was also found, which indicates that the survivors’ increased perception of family cohesion was associated with their spouses’ higher perceived family communication. However, there was no survivor partner effect.
A spouse actor effect was observed in the relationship between family communication and physical HRQOL, indicating that the spouses’ higher perceived family communication was related to their own better physical HRQOL. There were neither survivor nor spouse actor and partner effects in the relationship between family cohesion and physical HRQOL. The family cohesion and communication variables accounted for 24.8% of the variance in the survivors’ physical HRQOL and 10.8% of the variance in the spouses’ physical HRQOL.
The mental HRQOL model was similar to the physical HRQOL model. However, the actor effect between family communication and mental HRQOL was not observed for spouses. The family cohesion and communication variables accounted for 14.8% of the variance in the survivors’ mental HRQOL and 16.3% of the variance in the spouses’ mental HRQOL.
Mediating effects were found for the physical HRQOL only. That is, the spouses’ perceived family communication mediated the association between the survivors’ perceived family cohesion and the spouses’ physical HRQOL. A Sobel test confirmed this mediating effect (z=1.65, p< .05). The spouses’ perceived family communication also mediated the association between their own perceived family cohesion and their own physical HRQOL. A Sobel test confirmed (z=2.11, p< .05) this effect, which indicates that the spouses’ perceived family cohesion improved their abilities to communicate with family members, which, in turn, improved their physical HRQOL.
The moderating effect of sex (Hypothesis 2)
The model in which the structural paths differ by sex supported our hypothesis. For physical HRQOL, differences between the baseline model and the constrained structural path model were found at p< .01(ΔX2(15)=34.39), which suggests that family cohesion affects physical HRQOL through family communication differently for the two groups. In terms of mental HRQOL, there were statistically significant differences between the baseline model and the constrained structural path model at p< .01(ΔX2(15)=28.61).
In both the physical and mental HRQOL models, the spouse actor effects between family communication and HRQOL did not significantly differ by sex (Physical HRQOL: CR=−2.88, p< .01; Mental HRQOL: CR=−3.41, p< .01). That is, the positive perception of family communication for spouses of male survivors was associated with their own improved physical HRQOL, while the perception of family communication for spouses of female survivors was not associated with their own physical HRQOL. Additionally, male spouses’ own positive perception of family communication was related to their own decreased mental HRQOL.
DISCUSSION
The current study aimed to investigate the relationships among family cohesion, family communication, and HRQOL in couples dealing with cancer. More specifically, the mediating effects of family communication and the moderating effects of sex were tested. The study findings indicate that mediating effects of family communication were found for physical HRQOL only. The moderating effect of sex was demonstrated, indicating that the spouse actor effects between family communication and HRQOL significantly differed by sex. Thus, our hypotheses were partially supported in this study.
First, cancer survivors reported levels of perceived family cohesion, family communication, and HRQOL that were comparable with those of their spouses, showing that there are no significant differences in such outcomes. Previous studies have suggested that disagreement between patients and spouses are associated with worse HRQOL,46 and couple congruence is an important component of the adjustment to cancer.47 Based on the findings, we can expect that couples that participated in this study are likely to positively adjust to cancer. In fact, dyadic data, which require the participation of both members of couples, are likely to show similar findings in other studies46,48 because couples who participate in research together tend to have good relationships. Future study needs to further investigate the relationships among the study variables for both healthy and unhealthy couples using a large population-based study.
Second, the current study found positive relationships between family cohesion and communication, regardless of the type of HRQOL (physical versus mental), indicating that individuals’ increased perception of family cohesion was associated with their own higher perceived family communication. As the Circumplex Model suggested,22 our finding demonstrates that family communication may facilitate family cohesion, which, in turn, improves HRQOL. Generally, family cohesion is associated with healthy and positive interactions among family members.49 Individuals who live in a cohesive environment also tend to support each other and help each other cope with stress, protecting family members against psychological maladjustment.50 Thus, the finding that individuals in cohesive families openly and effectively communicate within the family seems to be reasonable.
Additionally, our findings demonstrated that the survivors’ increased perception of family cohesion is related to the spouses’ higher perceived family communication. This result indicates that spouses may consider their loved ones’ family involvement as a factor that affects their own ability to actively communicate and cope with stressful situations. For example, a spouse may not feel burdened by communicating with a cancer survivor about daily life or cancer issues if the spouse feels that the cancer survivor attempts to positively interact with other family members. In fact, both cancer survivors and their spouses experience communication difficulties,51 and a spouse’s unwillingness to communicate may make it more difficult for the other spouse to express her/his emotions.33 This result suggests that the participation of spouses in communication within the family may be influenced by how cancer survivors are actively engaged in household activities.
Meanwhile, survivors’ family communication was not influenced by their spouses, showing that there was no survivor partner effect in the relationship between family cohesion and communication. This result seems to be consistent with the result of a dyadic study on the relationship between resilience and psychological distress.34 Generally, cancer survivors may be overwhelmed by cancer treatment and self-management after cancer and, thus, may not pay attention to their spouses’ changes in roles and status within the family. This result contributes to the literature by providing reasons for the levels of family communication that may be expressed by both the survivors and the spouses.
In terms of the relationship between family communication and HRQOL, only a spouse actor effect was observed for physical HRQOL. Thus, the current study demonstrated the mediating role of family communication in the relationship between family cohesion and physical HRQOL for spouses. Family communication in survivorship care is an important and complex process that involves diverse types of content and interactions and, ultimately, influences HRQOL.52 Thus, a direct impact of family communication on survivors’ HRQOL might not be found because other factors that influence survivors’ HRQOL, including physical condition, side effects, and the relationships between survivors and physicians, may affect the relationship between family communication and HRQOL. Nevertheless, in the current study, we found that spouses’ perception of their own family communication, which is influenced by both the survivors’ and the spouse’s family cohesion, is directly associated with their physical HRQOL. This result may indicate that spouses’ physical health is influenced by their loved ones’ attitudes and involvement within the family. In fact, it is well known that family caregivers have higher levels of depression and worse physical health compared with non-caregivers.53 The current finding suggests that effective and good communication within the family, as well as the active engagement of cancer survivors, can improve spouses’ physical HRQOL. Future study is required to further investigate other factors that influence the relationship between family communication and HRQOL among cancer survivors.
The current study demonstrated the moderating effect of sex, indicating that the relationships among family cohesion, family communication, and HRQOL vary by sex, which is consistent with other studies.33,54 More specifically, female spouses’ own positive perception of family communication was associated with their own improved physical HRQOL, while male spouses’ own perception of family communication was not associated with their own physical HRQOL. Generally, it is recognized that men tend to communicate to solve problems and negotiate or maintain their status, with a focus on problem solving and task-oriented talk.55 Thus, high-quality family communication might not influence male spouses’ HRQOL. Meanwhile, if female spouses feel that they communicate well with family members, including cancer survivors, the burden of caring for their loved one may be reduced and, thus, their physical HRQOL may be improved. This finding seems to reflect established female communication patterns, such as emotion-focused and interpersonally oriented talk.31 The study findings imply that perspectives or standards of family communication may differ by gender such that men’s and women’s satisfaction with family communication may vary. Meanwhile, we did not find sex differences in survivor effects; thus, the effect of the “sick role” beyond sex/gender needs to be further investigated.
The current study has several limitations. First, the obtained data were self-reported; thus, recall bias and social desirability might have occurred. Second, the findings may not be generalizable to all cancer survivors and spouses due to the small sample size and low response rate. More specifically, the response rate of the current study was lower than that of other studies with cancer survivor dyads.47,56 Our stringent eligibility criteria, i.e., both the survivor and the spouse should participate together as a dyadic unit and survivors are currently cancer-free, and the inclusion of ethnic minorities such as African Americans might limit our ability to recruit samples. Methods for recruiting cancer survivors and collecting dyadic data in the community need to be systemically developed, and representative samples should be recruited to improve the generalizability of the results. Third, the current study has a potential selection bias based on the principle of voluntary participation and the characteristics of dyadic data (i.e., couples may have good relationships). This potential bias could lead to an underestimation of HRQOL and family functioning, including family communication and cohesion. Finally, the current study utilized a cross-sectional design; thus, causality cannot be assumed. Therefore, the findings should be interpreted with caution.
In conclusion, the current study provides valuable information regarding the relationships among family cohesion, family communication, and HRQOL in cancer survivor-spouse couples. Enhancing the family cohesion and communication of cancer survivors and their spouses can improve the spouses’ HRQOL. Our findings highlight the importance of understanding different paths in the relationships among family cohesion, communication, and HRQOL according to sex. Evidence that sex differences in the relationships among family cohesion, communication, and HRQOL exist serves as a rationale for gender-based approaches to improving HRQOL in survivorship care in the family context. Our findings also suggest the need for couple- and/or family-based interventions that are designed to enhance family cohesion and improve family communication skills that reinforce effective adjustments within couples and families. Additionally, behavioral interventions for couples and family members that address challenges related to psychosocial problems, health risk behaviors, cancer-related side effects, and self-management can aid in successfully preparing families for survivorship care. Thus, supportive care within the family context can be promoted to address the diverse challenges of survivorship care.
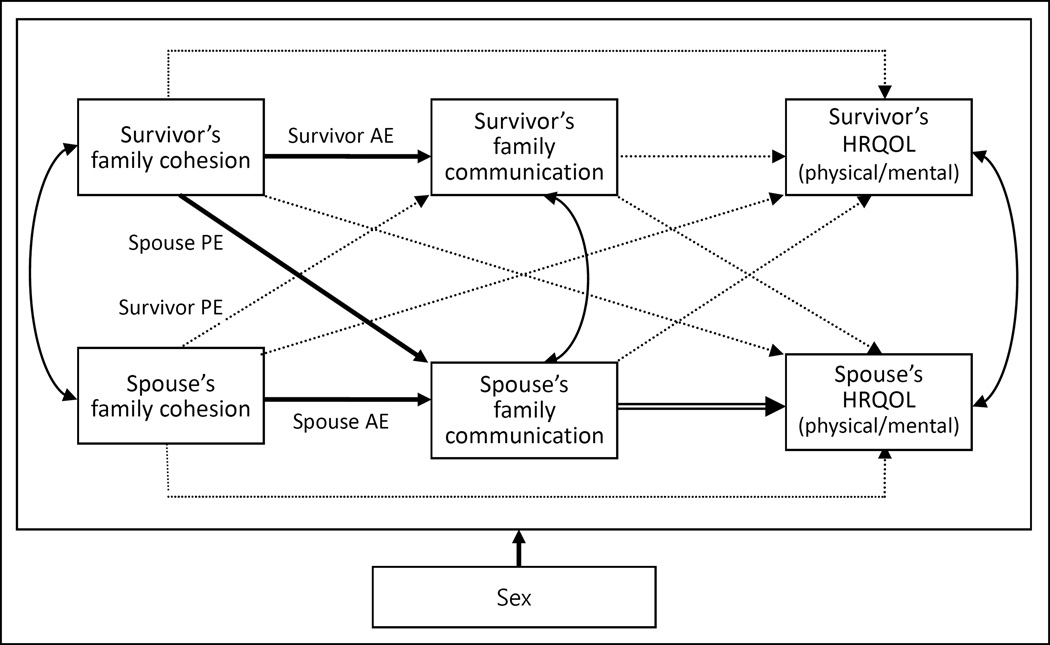
Figure. The Dyadic Model of Family Cohesion, Communication, and HRQOL: the Moderating Effect of Sex.
Note. Solid lines refer to significant paths at p<0.05; dotted lines refer to non-significant paths at p<0.05; double line refers to a different result by sex;
Abbreviations: AE, Actor effect; PE, Partner effect; Survivor PE, a survivor’s outcome is influenced by his/her partner’s scores; Spouse PE, a spouse’s outcome is influenced by his/her partner (survivor)’s scores.
Table 1.
Demographic and Medical Characteristics of Cancer Survivors by Sex (N=91)
| Variables | Male (n=58) | Female (n=33) | X2 |
|---|---|---|---|
| N(%) | |||
| Household income | |||
| <$25,000 | 7(12.7) | 3(9.7) | 0.30 |
| $25,001–$45,000 | 12(21.8) | 8(25.8) | |
| $45,001–$75,000 | 11(20.0) | 6(19.4) | |
| >$75,000 | 25(45.5) | 14(45.2) | |
| Employment | |||
| Unemployed | 3(5.2) | 8(24.2) | 0.20a |
| Employed | 55(94.8) | 25(75.8) | |
| Ethnicity | |||
| European-American | 47(81.0) | 27(81.8) | 0.01 |
| African-American | 11(19.0) | 6(18.2) | |
| Education | |||
| <High school | 4(6.9) | 1(3.0) | 0.63 |
| High school graduate | 11(19.0) | 7(21.2) | |
| >High school | 43(74.1) | 25(75.8) | |
| Cancer type | |||
| Breast | 1(1.7) | 27(81.8) | 69.52b |
| Colorectal | 12(20.7) | 6(18.2) | |
| Prostate | 45(77.6) | 0 | |
| Stage of diagnosis | |||
| I | 5(8.8) | 18(54.5) | 23.94b |
| II | 48(84.2) | 15(45.5) | |
| III | 4(7.0) | 0 | |
| Types of Cancer Treatment(yes) | |||
| Surgery | 37(67.3) | 33(100) | 13.58b |
| Radiation | 30(51.7) | 23(69.7) | 2.79 |
| Chemotherapy | 9(15.8) | 18(54.5) | 14.95b |
| Mean(SD) | t | ||
| Age | 67.9(8.5) | 57.6(10.4) | 5.13b |
| Years since diagnosis | 3.7(1.0) | 3.8(2.9) | −0.34 |
| Survivor-partner differences in cancer communication (CCAT-PF) |
19.8(6.6) | 19.1(7.7) | 0.48 |
| Current comorbidities | 3.0(3.1) | 3.4(3.3) | −0.64 |
p<.05
p<.001;
Table 2.
Inter-correlations, Means, and SDs of the Study Variables
| Variables | 1 | 2 | 3 | 4 |
|---|---|---|---|---|
| 1.Family cohesion | .49*** | .56*** | .16 | .35** |
| 2.Family communication | .56*** | .38*** | .28** | .33** |
| 3.Physical HRQOL | .03 | .13 | .32** | .69*** |
| 4.Mental HRQOL | .19 | .18 | .71*** | .31** |
| Mean(SD) | ||||
| Survivors | 32.9(5.5) | 3.8(0.8) | 68.9(24.9) | 75.0(19.9) |
| Spouses | 33.7(6.5) | 4.0(6.5) | 68.8(23.3) | 72.1(21.3) |
| Paired t | −1.81 | −1.15 | 0.06 | 1.23 |
p<.05,
p<.01,
p<.001; correlation coefficients above each diagonal correspond to spouses, and coefficients below each diagonal correspond to survivors.
Table 3.
Dyadic Effects of Family Cohesion and Communication in Predicting HRQOL
| Standardized Beta Coefficients |
Male Survivors | Female Survivors |
Critical Ratios for differences |
||
|---|---|---|---|---|---|
| Standardized Beta Coefficients |
Standardized Beta Coefficients |
||||
| Predicting physical HRQOL | |||||
| Cohesion → family communication |
Survivor AE | 0.512e | 0.438e | 0.648e | 1.736 |
| Spouse AE | 0.503e | 0.496e | 0.515d | 0.854 | |
| Survivor PE | 0.106 | 0.204 | −0.070 | −1.072 | |
| Spouse PE | 0.196c | 0.266c | 0.031 | −1.006 | |
| Family communication→ physical HRQOL |
Survivor AE | 0.081 | 0.224 | −0.025 | −1.169 |
| Spouse AE | 0.304c | 0.547e | −0.250 | −2.883a | |
| Survivor PE | 0.091 | 0.282b | −0.141 | −1.892 | |
| Spouse PE | −0.048 | −0.104 | 0.314 | 1.505 | |
| Cohesion → physical HRQOL |
Survivor AE | −0.051 | −0.077 | −0.111 | −0.279 |
| Spouse AE | −0.083 | −0.148 | 0.053 | 0.599 | |
| Survivor PE | −0.046 | −0.168 | 0.044 | 0.793 | |
| Spouse PE | 0.153 | 0.144 | −0.155 | −0.968 | |
| Covariates | CCAT→survivor’s com | −0.108 | −0.143 | −0.093 | 0.287 |
| CCAT→partner’s com | 0.023 | −0.134 | 0.260b | 2.267a | |
| Comorbidity→PHRQOL | −0.487e | −0.357d | −0.761e | −2.977a | |
| Predicting mental HRQOL | |||||
| Cohesion → family communication |
Survivor AE | 0.509e | 0.429e | 0.647e | 1.727 |
| Spouse AE | 0.497e | 0.490e | 0.532d | 1.022 | |
| Survivor PE | 0.112 | 0.215b | −0.071 | −1.117 | |
| Spouse PE | 0.196c | 0.264c | 0.021 | −1.046 | |
| Family communication→ mental HRQOL |
Survivor AE | 0.083 | 0.136 | 0.091 | −0.275 |
| Spouse AE | 0.188 | 0.452d | −0.438c | −3.409a | |
| Survivor PE | 0.116 | 0.120 | 0.056 | −0.270 | |
| Spouse PE | −0.075 | −0.103 | 0.354 | 1.718 | |
| Cohesion → mental HRQOL |
Survivor AE | 0.104 | 0.222 | −0.203 | −1.538 |
| Spouse AE | 0.182 | 0.068 | 0.487c | 1.747 | |
| Survivor PE | −0.049 | −0.175 | 0.269 | 1.676 | |
| Spouse PE | 0.157 | 0.157 | −0.325 | −1.689 | |
| Covariates | CCAT→survivor’s com | −0.107 | −0.142 | −0.095 | 0.269 |
| CCAT→partner’s com | 0.019 | −0.138 | 0.259 | 2.293a | |
| Comorbidity→MHRQOL | −0.318e | −0.214b | −0.519e | −1.447 | |
Note.
the critical ratio for differences meeting or exceeding ±1.96 were considered statistically significant at a p<.05.
p<.1
p<.05
p<.01
p<.001
Abbreviations: AE, Actor Effect; CCAT, The Cancer Communication Assessment Tool for Patients and Families; MHRQOL, Mental health-related quality of life; PE, Partner Effect; PHRQOL, Physical health-related quality of life.
Acknowledgments
Funding: This work was funded through the National Institute of Nursing Research (1P30NR011907).
Footnotes
Conflicts of Interest: The authors have no conflicts of interest to disclose.
Contributor Information
Jung-won Lim, College of Social Welfare, Kangnam University, Gyeonggi-do, Korea.
En-jung Shon, Mandel School of Applied Social Sciences, Case Western Reserve University, Cleveland, USA.
References
- 1.American Cancer Society. Cancer Facts & Figures 2015. Atlanta, GA: American Cancer Society; 2015. [Google Scholar]
- 2.Northouse LL, Katapodi MC, Schafenacker AM, Weiss D. The impact of caregiving on the psychological well-being of family caregivers and cancer patients. Semin. Oncol. Nurs. 2012;28:236–245. doi: 10.1016/j.soncn.2012.09.006. [DOI] [PubMed] [Google Scholar]
- 3.Goren A, Gilloteau I, Lees M, DaCosta DM. Quantifying the burden of informal caregiving for patients with cancer in Europe. Supp Car Cancer. 2014;22:1637–1646. doi: 10.1007/s00520-014-2122-6. [DOI] [PubMed] [Google Scholar]
- 4.Kim Y, Spillers RL, Hall DL. Quality of life of family caregivers 5 years after a relative's cancer diagnosis: follow-up of the national quality of life survey for caregivers. Psychooncology. 2012;21:273–281. doi: 10.1002/pon.1888. [DOI] [PubMed] [Google Scholar]
- 5.Litzelman K, Yabroff KR. How are spousal depressed mood, distress, and quality of life associated with risk of depressed mood in cancer survivors? Longitudinal findings from a national sample. Cancer Epidemiol Biomarkers Prev. 2015;24(6):969–977. doi: 10.1158/1055-9965.EPI-14-1420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hodges LJ, Humphris GM, Macfarlane G. A meta-analytiic investigation of the relationship between the psychological distress of cancer patients and their carers. Soc Sci Med. 2005;60(1):1–12. doi: 10.1016/j.socscimed.2004.04.018. [DOI] [PubMed] [Google Scholar]
- 7.Bodenmann G. Dyadic coping and its significant for marital functioning. In: Revenson T, Kayser K, Bodenmann G, editors. Couples coping with stress: emerging perspectives on dyadic coping. Washington DC: American Psychological Association; 2005. pp. 33–50. [Google Scholar]
- 8.Li Q, Loke AY. A literature review on the mutual impact of the spousal caregiver-cancer patients dyads: "communication," "reciprocal influence," and "caregiver-patient congruence". European Journal of Oncology Nursing. 2014;18:58–65. doi: 10.1016/j.ejon.2013.09.003. [DOI] [PubMed] [Google Scholar]
- 9.Litzelman K, Green PA, Yabroff KR. Cancer and quality of life in spousal dyads: spillover in couples with and without cancer-related health problems. Supportive Care Cancer. 2015 doi: 10.1007/s00520-015-2840-4. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dankoski ME, Pais S. What's love got to do with it? Couples, illness, and MFT. Journal of Couple and Relationships Therapy. 2007;6:31–43. [Google Scholar]
- 11.Powazki RD. The family conference in oncology: Benefits for the patient, family, and physician. Semin Oncol Nurs. 2011;38(3):407–412. doi: 10.1053/j.seminoncol.2011.03.011. [DOI] [PubMed] [Google Scholar]
- 12.Lim JW, Paek MS. The relationship between communication and health-related quality of life in survivorship care for Chinese-American and Korean-American breast cancer survivors. Supp Car Cancer. 2013;21:1157–1166. doi: 10.1007/s00520-012-1641-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kim Y, Given BA. Quality of life of family caregivers of cancer survivors. Cancer. 2008;112(S11):2556–2568. doi: 10.1002/cncr.23449. [DOI] [PubMed] [Google Scholar]
- 14.Olson DH, Portner J, Bell RQ. FACES II. Family Adaptability and Cohesion Evaluation Scales. Minnesota: Family Social Science, University of Minnesota; 1982. [Google Scholar]
- 15.Olson DH. Circumplex model of marital and family systems. J Fam Ther. 2000;22:144–167. doi: 10.1111/j.1545-5300.1983.00069.x. [DOI] [PubMed] [Google Scholar]
- 16.Northouse L. A longitudinal study of the adjustment of patients and husbands to breast cancer. Oncol Nurs Forum. 1989;16(4):221–225. [PubMed] [Google Scholar]
- 17.Moreira H, Frontini R, Bullinger M, Canavarro MC. Family cohesion and health-related quality of life of children with type 1 diabetes: The mediating role of parental adjustment. J Child Fam Stud. 2014;23:347–359. [Google Scholar]
- 18.Epstein NB, Bishop D, Ryan C, Keitner G. The McMaster Model View of Healthy Family Functioning. In: Walsh F, editor. Normal Family Processes. New York/London: The Guilford Press; 1993. pp. 138–160. [Google Scholar]
- 19.Shin DW, Shin J, Kim SY, et al. Family avoidance of communication about cancer: A dyadic examination. Cancer Res Treat. 2015 doi: 10.4143/crt.2014.280. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Black K, Lobo M. A conceptual review of family resilience factors. Journal of Family Nursing. 2008;14:33–55. doi: 10.1177/1074840707312237. [DOI] [PubMed] [Google Scholar]
- 21.Shin DW, Cho J, Yang HK, Kim SY, Park B. Oncologists' experience with patients with second primary cancer and the attitudes toward second primary cancer screening: a nationalwide survey. Cancer Research and Treatment. 2015 doi: 10.4143/crt.2014.162. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Olson DH. Circumplex model of marital and family systems. Journal of Family Therapy. 2000;22:144–167. [Google Scholar]
- 23.Shin DW, Shin J, Kim SY, et al. Family avoidance of communication about cancer: a dyadic examination. Cancer Research and Treatment. 2015 doi: 10.4143/crt.2014.280. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Siminoff LA, Zyzanski SJ, Rose JH, Zhang AY. The Cancer Communication Assessment Tool for Patients and Families (CCAT-PF): A new meausre. Psychooncology. 2008;17(12):1216–1224. doi: 10.1002/pon.1350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Fried TR, Bradley EH, O'Leary JR. Unmet desire for caregiver-patient communication and increased caregiver burden. Journal of American Geriatrics. 2005;53:59–65. doi: 10.1111/j.1532-5415.2005.53011.x. [DOI] [PubMed] [Google Scholar]
- 26.Santos FR, Kozasa EH, Chauffaille ML. Psychosocial adaptation and quality of life among Brazilian patients with different hematological malignancies. J. Psychosom. Res. 2006;60:505–511. doi: 10.1016/j.jpsychores.2005.08.017. [DOI] [PubMed] [Google Scholar]
- 27.Mols F, Vingerhoets AJ, Coebergh JW, Van de Poll-Franse LV. Quality of life among long-term breast cancer survivors: a systematic review. Eur. J. Cancer. 2005;41(17):2613–2619. doi: 10.1016/j.ejca.2005.05.017. [DOI] [PubMed] [Google Scholar]
- 28.Eagly AH, Wood W, Diekman AB. Social role theory of sex differences and similarities: a current appraisal. In: Eckes T, editor. The developmental social psychology of gender. Mahwah, NJ: Lawrence Erlbaum Associates Publishers; 2000. pp. 123–174. [Google Scholar]
- 29.Archer J. Sex differenes in social behavior: Are the social role and evolutionary explanations compatible? Am. Psychol. 1996;51:909–917. doi: 10.1037//0003-066x.51.9.909. [DOI] [PubMed] [Google Scholar]
- 30.Culp LN, Beach SRH. Marriage and depressive symptoms. Psychology of Women Quarterly. 1998;22:647. [Google Scholar]
- 31.Powell GN, Greenhaus JH. Sex, gender, and the work-to-family interface: exploring negative and positive interdependencies. Acad. Manage. J. 2010;53:513–534. [Google Scholar]
- 32.Eagly AH. Sex differences in social behavior: a social-role interpretation. Hillsdale, NJ, England: Lawrence Erlbaum Associates, Inc; 1987. [Google Scholar]
- 33.Lim JW, Paek MS, Shon EJ. Gender and role differences in couples' communication during cancer survivorship. Cancer Nurs. 2015;38(3):51–60. doi: 10.1097/NCC.0000000000000191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lim JW, Shon EJ, Paek M, Daly B. The dyadic effects of coping and resilience on psychological distress for cancer survivor couples. Supportive Care Cancer. 2014;22(12):3209–3217. doi: 10.1007/s00520-014-2334-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ware JE, Snow KK, Kosinski M, Gandek B. SF-36 health survey: manual and interpretation guide. Boston: Health Institute, New England Medical Center; 1993. [Google Scholar]
- 36.Olson DH. Circumplex Model VII: Validation studies and FACES III. Fam. Process. 1986;25(3):337–351. doi: 10.1111/j.1545-5300.1986.00337.x. [DOI] [PubMed] [Google Scholar]
- 37.Olson DH, Gorall DM, Tiesel JW. FACES IV Package. Minneapolis, MN: Life Innovations; 2004. [Google Scholar]
- 38.MacCallum RC, Bronwe MW, sugawara HM. Power analysis and determination of sample size for covariance modeling. Psychological Methods. 1996;1(2):130–149. [Google Scholar]
- 39.Ledermann T, Macho S, Kenny DA. Assessing mediation in dyadic data using the actor-partner interdependence model. Structural Equation Modeling. 2011;18:595–612. [Google Scholar]
- 40.Steiger JH. Structural model evaluation and modification: An interval estimation approach. Multivariate Behavioral Research. 1990;25:173–180. doi: 10.1207/s15327906mbr2502_4. [DOI] [PubMed] [Google Scholar]
- 41.Bentler PM. Comparative fit indexes in structural models. Psychol. Bull. 1990;107(2):238–246. doi: 10.1037/0033-2909.107.2.238. [DOI] [PubMed] [Google Scholar]
- 42.Bollen KA. Structural equations with latent variables. New York, NY: John Wiley & Sons, Inc; 1989. [Google Scholar]
- 43.Kline RB. Principles and practice of structural equation modeling. New York: Guilford Press; 1998. [Google Scholar]
- 44.Enders C, Bandalos D. The relative performance of full information maximum likelihood estimation for missing data in structural equation models. Structural Equation Modeling. 2001;8(3):430–457. [Google Scholar]
- 45.Lim JW, Ashing-Giwa K. Is family functioning and communication associated with health-related quality of life for Chinese- and Korean-American breast cancer survivors? Qual. Life Res. 2013;22:1319–1329. doi: 10.1007/s11136-012-0247-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Merz E, Malcarne V, Ko CM, et al. Dyadic concordance among prostate cancer patients and their partners and health-related quality of life: Does it matter? Psychology & Health. 2011;26(6):651–666. doi: 10.1080/08870441003721251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Drabe N, Wittmann L, Zwahlen D, Buchi S, Jenewein J. Changes in colose relationships between cancer patients and their partners. Psychooncology. 2013;22:1344–1352. doi: 10.1002/pon.3144. [DOI] [PubMed] [Google Scholar]
- 48.Song L, Northouse LL, Zhang L, et al. Study of dyadic communication in couples managing prostate cancer: a longitudinal perspective. Psychooncology. 2012;21(1) doi: 10.1002/pon.1861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Field C, Duchoslav R. Family influence on adolescent treatment outcomes. In: O'Donohue WT, Tolle LW, editors. Behavioral approaches to chronic disease in adolescence. New York: Springer; 2009. pp. 47–54. [Google Scholar]
- 50.Coyne JC, Downey G. Social factors and psychopathology: stress, social support, and coping processes. Annu. Rev. Psychol. 1991;42:401–425. doi: 10.1146/annurev.ps.42.020191.002153. [DOI] [PubMed] [Google Scholar]
- 51.Boehmer U, Clark JA. Communication about prostate cancer between men and their wives. The Journal of Family Practice. 2001;50(3):226–231. [PubMed] [Google Scholar]
- 52.Rim SH, Hall IJ, Fairweather ME, et al. Considering racial and ethnic preferences in communication and interactions among the patient, family member, and physician following diagnosis of localized prostate cancer: study of a US population. Internal Journal General Medicine. 2011;4:481–486. doi: 10.2147/IJGM.S19609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Pinquart M, Sorensen S. Ethnic differences in stressors, resources, and psychological outcomes of family caregiving: A Meta-Analysis. the Gerontologist. 2005;45(1):90–106. doi: 10.1093/geront/45.1.90. [DOI] [PubMed] [Google Scholar]
- 54.Walsh SR, Manuel JC, Avis NE. The impact of breast cancer on younger women's relationships with their partner and children. Families, Systems & Health: The Journal of Collaborative Family Health Care. 2005;23:80–93. [Google Scholar]
- 55.Tannen D. You just don't understand: Women and men in conversation. New York: Quill; 2001. [Google Scholar]
- 56.Kim Y, Carver CS, Spillers RL, Crammer C, Zhou ES. Individual and dyadic relations between spiritual well-being and quality of life among cancer survivors and their spousal caregivers. Psychooncology. 2011;20:762–770. doi: 10.1002/pon.1778. [DOI] [PubMed] [Google Scholar]