Abstract
Objective
Description of surgical technique, complications and outcome of radius/ulna fractures in toy and miniature breed dogs treated with the paraosseous clamp-cerclage stabilisation (PCCS) method.
Study design
Retrospective study.
Methods
Clinical records of small breed dogs with fractures of the radius and ulna were reviewed between January 2011 and January 2016. Inclusion criteria were bodyweight of ≤3.5 kg, fracture of the radius and ulna of one or two limbs without previous repair attempts, available follow-up information, and the use of PCCS for repair of the fracture as the sole method of fixation.
Results
Seventeen fractures in 17 dogs were included in the study. Radiographic union was documented in 13/17 cases. Median time to radiographic union was 13 weeks (range: 5–53 weeks). Major complications occurred in 24 per cent (4/17) due to implant failure, and for revision surgery the PCCS method was chosen in all four cases. Three of four revised fractures healed radiographically. One of the four dogs was lost for radiographic follow-up, but the owner could be contacted for a telephone questionnaire. Eleven of 17 dogs achieved an excellent return to function without any lameness during clinical examination, but 5/17 dogs showed an intermittent mild lameness despite full radiographic union. Routine implant removal was performed in 9/17 dogs. The owners of 15/17 dogs could be contacted for a telephone questionnaire for a long-term follow-up. No further complications were reported.
Conclusions
PCCS is a feasible low-cost internal fixation technique for repairing radial and ulnar fractures in toy breed dogs. Further biomechanical and clinical studies are needed for better evaluation of the PCCS method.
Keywords: Dogs, Fracture management, Surgery, Trauma
Introduction
Fractures of the radius and ulna occur most frequently in the distal radial diaphysis of small breed dogs (Lappin and others 1983, Eger 1990, Muir 1997, Larsen and others 1999, Hamilton and others 2005, McCartney and others 2010, Piras and others 2011, Gibert and others 2015). Non-rigid stabilisation methods like the application of casts or the use of intramedullary pins have a major complication rate of more than 80 per cent (Lappin and others 1983). External skeletal fixation (ESF) (transfixation pins with acrylic cement or circular external fixation) (McCartney and others 2010, Piras and others 2011) or plate osteosynthesis (locking compression plates or conventional plates) (Gibert and others 2015, Ramírez and Macías 2016) achieves good clinical outcomes with a major complication rate of less than 6 per cent (McCartney and others 2010, Piras and others 2011, Gibert and others 2015, Ramírez and Macías 2016).
Paraosseous clamp-cerclage stabilisation (PCCS) is an internal fixation osteosynthesis method that has been developed as a low-cost treatment for simple and comminuted diaphyseal fractures of long bones in dogs and cats (Wanivenhaus 2001). The Arbeitsgemeinschaft für Osteosynthese (AOVET) described PCCS as a rigid fixation method for treatment of tibial fractures (Schwarz 2005). So far only a few studies have been published in which this method has been assessed biomechanically as well as clinically (Bartolomaeus and others 2007, Behrend 2007). The method has already been applied successfully for radial/ulnar fractures in 14 dogs (9 of 14 had distal diaphyseal fractures) and in 8 cats (Wanivenhaus 2001, Graf 2003, Behrend 2007). Fifty of 51 diaphyseal fractures of various bones have been successfully repaired in cats and several dog breeds (Graf 2003).
At the authors’ hospital, the PCCS method has been initially used for radial and ulnar fractures in toy breed dogs after failure of fracture fixation with compression plate or external fixator, and/or for dogs where the owners had financial limitations. During routine check-up, the patients had a low rate of refractures and the authors started to use PCCS routinely.
The aim of this retrospective study was to describe surgical technique, complications, and short-term and long-term outcomes for the treatment of radial and ulnar fractures in toy breed dogs with PCCS.
Materials and methods
Selection criteria
In the database of the small animal hospital, Freie Universität Berlin, clinical records of small and toy breed dogs with surgical treatment of radius/ulna fractures were searched from January 2011 to January 2016. Inclusion criteria were bodyweight of 3.5 kg or less as reported by Hamilton and others (2005), fracture of the radius and ulna of one or two limbs, and repair with open reduction and internal fixation using the PCCS as the sole method of fixation. Dogs with previously failed fracture repair or dogs without any follow-up information were excluded.
Preoperative patient information
The following data were collected from clinical records: signalment, clinical history, cause of the fracture and its duration. Standard radiographic images (mediolateral and craniocaudal) were assessed and the type and location of fracture were documented.
Implant description
For the PCCS apparatus, stainless steel Kirschner wire (0.8–1.4 mm diameter) and stainless steel cerclage wire 0.5–0.8 mm diameter (Königsee Implantate, Allendorf, Germany) were used.
Surgical procedure
Several surgeons with different levels of experience at the small animal hospital of the Freie Universität Berlin, Germany, performed the surgeries. As standard anaesthetic protocol, midazolam (0.5 mg/kg intravenously, Midazolam B Braun) or diazepam (0.5 mg/kg intravenously, Ziapam. Ecuphar) and levomethadone/fenpipramid (0.5/0.025 mg/kg intravenously, L-Polamivet; MSD Animal Health) were used for premedication, and propofol (2–3 mg/kg intravenously, Narcofol; CP-Pharma) was used as induction agent. Anaesthesia was maintained using inhalation anaesthesia with isoflurane (1.5–2 per cent) and oxygen, and the patients were ventilated throughout the procedure. All dogs were given amoxicillin/clavulanic acid (12.5 mg/kg intravenously, AmoxClav; HEXAL) at least 30 minutes preoperatively. The affected limb was clipped circumferentially and the dog was positioned in a metal frame in sternal recumbency with the neck in extension. The limb was prepared aseptically and draped with single-use water-impermeable cloth. A craniomedial approach to the radius was performed and care was taken to preserve the tendon of the abductor pollicis longus muscle.
Each implant was custom-made during the procedure as described by Wanivenhaus and later on by Schwarz in the AO Principles of Fracture Management in the Dog and Cat (Wanivenhaus 2001, Schwarz 2005). Wanivenhaus and Schwarz have used double-loop cerclages for their paraosseous clamps, but the authors preferred a simple twisted cerclage as described in a few cases by Behrend and Graf (Graf 2003, Behrend 2007). This technique is described by the authors for radial and ulnar fractures as follows: The first hole was drilled through the cranial and caudal cortices of the distal radial fragment in a diagonal fashion as far away from the fracture line as possible (Fig 1a). The diameter of the drill bit was chosen according to the size of the selected K-wire. For example, a 1.1 mm drill bit or (1 mm diameter) K-wire was used for drilling holes for clamps assembled with (1 mm diameter) K-wires. A 1.2 mm K-wire was used for drilling holes for clamps assembled with 1.2 mm K-wire and so on. The size of the K-wires used during the surgical procedure did not exceed more than 40 per cent of the diameter of the radial bone on sagittal plane (0.8–1.4 mm diameter). A measuring device was used to measure the depth of each hole. In some cases, intravenous cannulas were used as a template for evaluation of a suitable angle in which the K-wire needed to be bent (Fig 1b). The cannula was inserted into the hole and was bent towards the fracture line so that it could lay parallel to the bone cortex on the same plane as the cortex. Then the distal end of the K-wire was remodelled (with the help of the template) and cut to be 1 mm longer than the measured depth of the hole. The opposite end of the K-wire was bent in a standard angle of 90–110°, and the bent end was shortened to a length that would allow fixation in at least one cortex. The distal end of the clamp was inserted in the distal fragment and the fracture was reduced using two Locke Phalangeal forceps, one on each fragment (Fig 1c). The hole for insertion for the proximal end of the clamp on the cranial surface of the radius was drilled in a similar angle (90–110°) at the selected contact point of the proximal end of the clamp with the radial bone (Fig 1c). Either a pair of Locke Phalangeal forceps or a temporary cerclage made of 2–0 monofilament suture material was used to secure the first clamp to the bone and to keep the fracture temporarily reduced (Fig 1d). The second clamp, which is usually shorter than the first one, was customised to the medial aspect of the radius in a similar fashion (Fig 1d). Due to the small craniocaudal diameter of the radius, the holes for the medial clamp were drilled diagonally from craniomedial into caudolateral direction. The angle between the two planes created by the clamps was approximately 90°. In most cases, one or two simple twisted cerclages were placed around the clamps on the distal fragment, and two or three cerclages were used for the proximal fragment. Cerclage ends were bent over. A tip of a surgical instrument (eg, periosteal elevator) was inserted between clamps in the middle to avoid impingement during tightening of the cerclages. Application of the distal cerclage is difficult due to the conical shape of the distal fourth of the radius. Therefore, in some cases, a hemi-cerclage was applied to reduce the risk of cerclage slipping away (Fig 1e). All implants were reassessed before wound closure and their position was corrected if there were any problems. The wound was closed routinely.
FIG 1:

Anatomical model, SYNBONE AG. (a) Photograph illustrating the diagonal angle for drilling the first hole in the distal radial fragment. (b) An intravenous cannula used as a template for bending the K-wire in the correct angle to create a PCCS clamp. (c) Photograph to demonstrate how the second hole is drilled into the proximal fragment after reduction of the fracture. The K-wire has been inserted into the distal fragment and is held in place by Locke Phalangeal forceps. The point of contact on the proximal fragment is the correct position for the hole. (d) To keep the fracture reduced, temporary suture cerclages are used to aid the first clamp. The second clamp is custom-made in the same manner as the first clamp. (e) Final result of the entire PCCS apparatus. Hemi-cerclages are recommended, in particular short distal fragments. PCCS, paraosseous clamp-cerclage stabilisation.
Postoperative management
A modified Robert Jones bandage was applied for at least a week postoperatively, and further bandage treatment was recommended for up to 3 weeks depending on the surgeon’s preference. The owners were instructed to keep the patient strictly rested with short leash walks three times daily for 5–10 minutes. The bandage was changed on the second postoperative day and bandage changes were continued twice a week. Skin sutures were removed between 10 and 14 days after surgery. NSAIDs were given for 5–7 days, and it was recommended to have the implants surgically removed after fracture healing was completed and the fracture line could not be identified radiographically. Implant removal was planned after radiographic union at a time point convenient for the owners. If owners decided not to have the implants removed, it was recommended to have the limb reassessed at the hospital twice yearly for the first 2 years. At these rechecks, radiographs were taken to assess the bone for osteopenia. After implant removal, a modified Robert Jones bandage was applied for 2 or 3 days, and NSAIDs were given for 5–7 days. It was recommended that the owners restrict dog exercise postoperatively for 3 or 4 weeks. Follow-up data were collected from clinical records, and included postoperative care, complications (considered major if another surgery was needed), any specifics of revision surgery (eg, bone graft), lameness at the time of follow-up, when radiographic union was evident or later if available, clinical outcome, and implant removal (routinely or indicated because of a complication).
Owners were contacted for a telephone questionnaire after a minimum of 3 months after fracture healing or implant removal, and questions included limb function and possible complications.
Surgical procedure and PCCS evaluation
Surgical protocols and postoperative radiographs (mediolateral and craniocaudal) of each case were evaluated. Diameter of K-wires and type of cerclage (whether simple or hemi-cerclage) were recorded. Number of cerclages used, length of the longest clamp compared with the length of the radius and the method of insertion of the clamp (monocortical v bicortical) were documented for each fracture.
Postoperative radiographic follow-up
Fracture reduction was evaluated postoperatively on frontal and sagittal planes and was graded as excellent (≥90 per cent), good (80–89 per cent), fair (70–79 percent) and poor (<70 per cent) with respect to apposition of the fragments. The first recheck with postoperative radiographs was recommended 4–6 weeks after surgery, and thereafter every 4 weeks until the fracture had healed. The fracture was considered radiographically healed if the fracture line was not visible anymore. After fracture healing, possible complications such as radioulnar synostosis and osteopenia were documented.
Moreover, radiographs (craniocaudal as well as mediolateral planes) were used to determine limb alignment (Fox and others 2006). For this purpose, the following angles were measured. On frontal plane, medial proximal radial angle (MPRA), lateral distal radial angle (LDRA) and frontal plane alignment (FPA) were calculated. FPA is the absolute difference between MPRA and LDRA angles. On sagittal plane, proximal cranial radial angle and distal caudal radial angle were calculated, and finally sagittal plane alignment (SPA) was determined as the angular difference between the elbow and the carpal lines.
The measurements of both planes were compared with standard data that have been described in the literature previously (Fox and others 2006, Piras and others 2011). The authors also categorised measurements: excellent=no malalignment, good=<5° (minimal) malalignment and satisfactory=5–20° malalignment, from the standard values published by Fox and others, FPA (range: 0–8°) and SPA (range: 8–35°).
Results
Dog population
Twenty-six dogs had a PCCS fixation between January 2011 and January 2016. Of the 26 dogs, 22 dogs were toy breed dogs with a weight of 3.5 kg or less. Four dogs were excluded because of previous repair using other fixation methods. One dog was excluded because of the lack of follow-up information. Seventeen fractures of 17 dogs were included in the study (Table 1). The following breeds were included: four chihuahuas, four Prague ratters, one pomeranians, two Miniature Pinschers, two Miniature Pinscher mixes, one toy fox terrier, one Russkiy toy, one Papillon and one Italian greyhound.
Table 1:
Case summary of radial and ulnar fractures treatment with paraosseous clamp-cerclage stabilisation technique
| Case no. |
Breed | Age (m) |
Weight (kg) |
Location of the distal radial fracture | K-wire used (mm diameter) cranial/medial | Number/diameter (mm) of cerclage(s) in proximal fragment |
Number and diameter of cerclage(s) in distal fragment | Major complication | Revision surgery | Radial radiographic outcome | Ulnar radiographic outcome | Implant removal |
| 1 | Russkiy toy | 16 | 2.50 | Distal fourth | 1/1 | 2/0.5 | 2/0.5 | Healed | Healed | |||
| 2 | Toy fox terrier | 5 | 3.00 | Distal third | 1.2/1 | 2/0.6 | 1/0.5 | Healed | Healed | Done | ||
| 3 | Chihuahua | 8 | 2.30 | Distal fourth | 1/1 | 2/0.5 | 1/0.5 | Healed | Healed/Synostosis | Done | ||
| 4 | Miniature Pinscher mix | 20 | 2.60 | Mid-shaft | 1/1 | 2/0.5 | 2/0.5 | Healed | Healed/Distal osteopenia | |||
| 5 | Italian greyhound | 24 | 3.3 | Distal third | 1.4/1.4 | 2/0.8 | 2/0.8 | Healed | Healed | |||
| 6 | Prague ratters | 7 | 1.80 | Distal third | 1/1 | 2/0.5 | 1/0.5 | Healed | Healed | Done | ||
| 7 | Chihuahua | 17 | 2.30 | Distal fourth | 1.4/1.4 | 3/0.5 | 2/0.5 | Healed | Atrophic non-union | Done | ||
| 8 | Chihuahua | 5 | 1.20 | Distal fourth | 0.8/0.8 | 3/0.5 | 1/0.5 | Healed | Healed/Synostosis | Done | ||
| 9 | Miniature Pinscher mix | 7 | 1.00 | Distal third | 1/1 | 3/0.5 | 2/0.5 | Healed | Distal resorption | Done | ||
| 10 | Prague ratters | 6 | 1.4 | Distal fourth | 1.2/1.2 | 2/0.5 | 1/0.5 | Healed | Healed | |||
| 11 | Miniature Pinscher | 16 | 1.10 | Distal third | 1/1 | 2/0.5 | 2/0.5 | Healed | Distal resorption | |||
| 12 | Prague ratters | 7 | 1.3 | Distal third | 1.2/1.2 | 2/0.6 | 1/0.6 | Healed | Healed | |||
| 13 | Papillon | 12 | 2.9 | Distal fourth | 1.2/1.2 | 2/0.5 | 2/0.7–0.5 | Healed | Healed/Synostosis | |||
| 14 | Miniature Pinscher | 49 | 2.40 | Distal fourth | 1/0.8 | 2/0.5 | 1/0.5 | Implant failure (broken 1 mm K-wire) after 4 weeks | PCCS with 2×1.2 mm clamps and 2×0.8 mm cerclages proximally and 1×0.6 mm distally | Healed | Healed | Done |
| 15 | Pomeranian | 9 | 1.90 | Distal fourth | 1.2/1 | 2/0.5 | 2/0.5 | Implant failure (distal cerclage instability) and malunion after 11 weeks | PCCS with 2×1 mm clamps and 2×0.5 mm cerclages proximally and 2×0.5 distally (one hemi-cerclage) | Healed | Healed/Synostosis | Done |
| 16 | Prague ratters | 8 | 1.80 | Distal fourth | 1.2/1.2 | 4/0.5 | - | Implant failure after 4 weeks, cause of missing distal cerclage | PCCS, 1×0.6 mm distal hemi-cerclage was added; one proximal cerclage was removed |
Healed | Healed/Synostosis | Done |
| 17 | Chihuahua | 12 | 1.40 | Distal fourth and proximal third | 0.8/0.8 | 3/0.5 | 1/0.5 | Implant failure after 3 weeks (clamp, bending), | PCCS with 2×1 mm clamps and 3×0.6 mm cerclages proximally and 1×0.6 mm hemi-cerclage distally |
Unknown | Unknown |
PCCS, paraosseous clamp-cerclage stabilisation.
Eight dogs were female (six intact, two spayed) and nine dogs were male (six intact, three neutered). The median age was 9 months (range: 5–49 months) and the mean bodyweight was 2.1±0.7 kg (range: 1–3.3 kg). Fractures of the left front leg were reported in 10 dogs and fractures of the right front leg were reported in 7 dogs. None of the fractures were open. All fractures had apparently been caused by minimal trauma: five dogs dropped from the owner’s arm, four dogs were playing with other dogs, and six dogs fell from low height (eg, bed). In two dogs, the cause was not clear. Transverse fractures were observed in 11 dogs, whereas 6 dogs had a slightly oblique fracture. For 15 dogs, the median time from accident to surgery was 1 day, and this ranged from 0 to 3 days. One dog had a healed contralateral radius/ulna fracture with a dynamic compression plate (DCP) in situ. The location of the fracture was on the distal fourth of the radius in 10 dogs, distal third of the radius in 6 dogs and mid-diaphysis in 1 dog.
PCCS stabilisation
In all dogs a total of two clamps were used. The median size of the K-wires was 1 mm (range: 0.8–1.4 mm diameter). In most dogs the same size of K-wires was used on the medial and cranial radial aspect, and only in three dogs two different sizes were chosen for the apparatus (Table 1).
In 4/17 dogs, one end of the assembled clamps was inserted bicortically in each fragment. In 6/17 dogs, three of the four ends of the clamp were inserted bicortically, and in the remaining 7 dogs all ends of both clamps were inserted bicortically.
The longest clamp was 40 per cent of the length of the radial bone in one dog, 50–60 per cent in nine dogs, 70–75 per cent in three dogs and 80–90 per cent in four dogs.
The median size of the cerclage wire used was 0.5 mm (range: 0.5–0.8 mm). Twelve dogs had two cerclage wires (Fig 2), four dogs had three cerclage wires and one dog had four cerclage wire on the proximal fragment. Ten dogs had one cerclage wire on the distal fragment, eight dogs had two cerclage wires and one had no cerclage wire. A hemi-cerclage wire was used on the distal fragment of six dogs.
FIG 2:
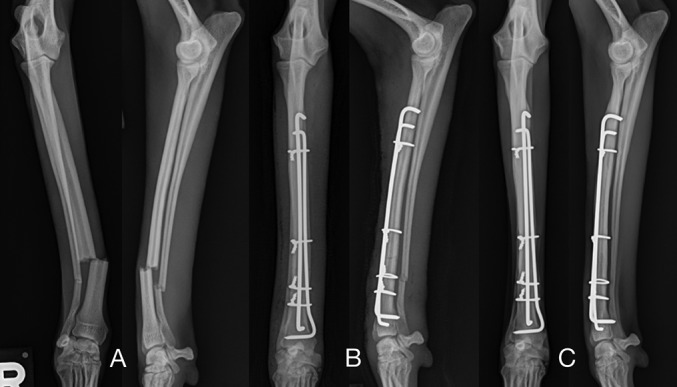
Craniocaudal and mediolateral radiographs of case 5 of the right antebrachium (24-month old Italian greyhound, 3.3 kg). (a) Simple transverse fracture of the radius and ulna. (b) Immediate postoperative radiographs after stabilisation with PCCS (1.4/1.4 mm K-wires). (c) Last postoperative radiographs at 11 months; radial and ulnar fractures are healed, PCCS in situ. PCCS, paraosseous clamp-cerclage stabilisation.
Follow-up information
Excellent fracture reduction and a fracture gap of <1 mm were noted on immediate postoperative radiographs in all cases. For 15/17 dogs, the medical records revealed the duration of postoperative bandage treatment. The median time with a light-modified Robert Jones bandage was 12 days (range: 7–21 days).
Radiographic follow-up of 17 dogs was available; however, time intervals between radiographs varied between cases. For 16 dogs, radiographs were taken between 3 and 11 weeks (median: 5.5 weeks) postoperatively. At this time, four fractures achieved union. Implant failure occurred in three fractures and one fracture developed malunion. All other eight fractures showed different levels of radiographic healing.
For 13/17 dogs without major complications, radiographs were taken between 5 and 53 weeks (median: 13 weeks) postoperatively. At this time, all these 13 fractures showed radiographic union. Callus formation was seen in all dogs at the time of radiographic fracture union.
Minor and major complications
Minor complications occurred during treatment in 3 of 17 dogs. Two dogs developed pressure sores during bandage treatment and another dog had an interphalangeal skin necrosis, which was treated with amoxicillin/clavulanic acid.
Four of 17 (24 per cent) dogs treated in this study had a major complication (Table 1). The median time between the first and second surgery for these four dogs was 4 weeks (range: 3–11 weeks).
Implant failure was detected in three dogs. Fracture instability and non-weightbearing lameness were noticed during clinical examination in these three dogs. In one dog (no. 14) a broken K-wire (1 mm diameter) and bent K-wire (0.8 mm diameter) were noted on the radiographs at 4 weeks postoperatively. During revision surgery, two (1.2 mm diameter) K-wires were chosen and autogenous cancellous bone graft was added at the fracture site. The second (no. 16) dog had no cerclage on the distal fragment by surgical error (the patient was unstable during anaesthesia) and the distal fragment was displaced at 4-week follow-up. During revision surgery, a 0.6 mm diameter hemi-cerclage was used on the distal fragment. Two 0.8 mm diameter K-wires were bent at the level of the fracture line of the third dog (no. 17) after 3 weeks. This dog had a fracture in the distal fourth and another one on the proximal third of the radius, which occurred during the first surgery due to surgical error. At revision surgery, two 1 mm K-wires were used. Malunion was documented in the fourth dog after 11 weeks because of distal cerclage failure. Limb deformity was corrected using PCCS with two 1 mm K-wires and autogenous cancellous bone graft. Swabs for bacterial culture were taken in two dogs during revision surgery and were negative. After revision surgery, three of four dogs achieved radiographic union at a median of 7 weeks (7–17 weeks). The owners of the remaining dog could be contacted by telephone and they reported a mild persistent lameness 1 year postsurgery.
Further follow-up
Thirteen of 16 ulnar fractures achieved radiographic union. In one dog, non-union of the ulna was present and two other dogs had mild bone resorption of the ulna (Figs 3 and 4). In two cases, there was mild osteopenia of the distal part of the ulnar bone. Five of 16 dogs developed a radioulnar synostosis (two of these were revision surgeries).
FIG 3:
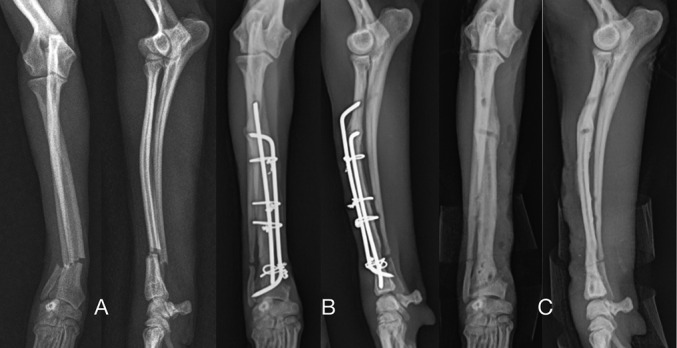
Craniocaudal and mediolateral radiographs of case 7 of the right antebrachium (17-month-old chihuahua, 2.3 kg). (a) Short oblique fracture of the radius and ulna. (b) 7 weeks’ postoperative radiographs after stabilisation with PCCS (1.4/1.4 mm K-wires); radial and ulnar fractures are healing. (c) Radiographs after implant removal at 4 months postoperatively. Notice the ulnar non-union. PCCS, paraosseous clamp-cerclage stabilisation.
FIG 4:
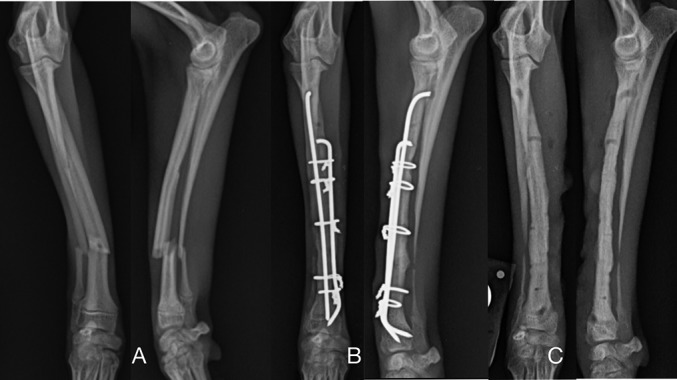
Craniocaudal and mediolateral radiographs of case 9 of the right antebrachium (7-month-old Miniature Pinscher mix, 1 kg). (a) Short oblique fracture of the radius and ulna. (b) 5 weeks’ postoperative radiographs after stabilisation with PCCS (1/1 mm K-wires); radial fracture is healing. (c) Radiographs after implant removal at 2 months. Notice the ulnar resorption. PCCS, paraosseous clamp-cerclage stabilisation.
Long-term radiographic follow-up was available for four cases without implant removal (one dog with revision surgery) at a median of 17 months (range: 11–26 months). No signs of radial osteopenia were noticed in any of the four cases.
Implant removal was carried out in nine dogs (three dogs with revision surgery) between 2 and 21 months (median: 4 months) after fracture repair. Small pieces of the clamps or cerclage wire could not be removed in two of these nine dogs. The median time between radiographic healing and implant removal was 4 weeks (range: 0–80 weeks).
The mean FPA for 16 dogs after fracture healing was 5.6±3° (range: 0–13°) and the median SPA was 8° (range: 7–20°). Comparing with Fox and others, FPA was excellent in 14 of 16 dogs and good in 2. In 14 of 16 dogs, SPA was excellent in 14 and good in 2 dogs.
Final clinical examination was performed in 16 of 17 dogs between 2 and 26 months (median: 5 months) after surgery. Eleven dogs regained normal function of their limb, while five dogs had mild intermittent lameness. Carpal flexion angle was available for nine dogs and was greater than 110°.
Fifteen dog owners were available for telephone follow-up 5–66 months (median: 17 months) after surgery (in nine dogs at a minimum of 3 months after implant removal). No further complication was reported at that time.
Discussion
The results of the present study confirm that the PCCS technique can be applied for the treatment of radius and ulna fractures in toy and miniature breed dogs. In previous publications several types of fractures of various bones have been stabilised with two clamps (Wanivenhaus 2001, Schwarz 2005). However, the PCCS method with a single clamp has been successful in small breed dogs and cats with radial/ulnar and tibial fractures due to the small size of the bones (Wanivenhaus 2001, Graf 2003). The authors have chosen two clamps for every patient in this study.
The PCCS method with two double-loop cerclages in the proximal fragment and one double-loop cerclage in the distal fragment has been described in previous studies (Wanivenhaus 2001, Schwarz 2005). A minimum of one cerclage per fragment is needed in order to achieve stability (Wanivenhaus 2001, Behrend 2007). The double-loop cerclage has better tension and load resistance compared with the twisted cerclage technique (Roe 1997). However, simple twisted cerclages have been used successfully in cases with metacarpal or metatarsal or tibial fractures in cats and were chosen due to the small size and weight of the patients (Graf 2003, Behrend 2007). The authors have used simple twisted cerclage in all cases. The objective was to use the least amount of implant material possible to avoid disturbing bone blood supply. Two or three simple twisted cerclages were applied to the proximal fragment and one or two twisted cerclages to the distal fragment in each of the patients. For the present study, patients with a low bodyweight were selected. Other studies applied the PCCS method for various patient sizes (range: 2.4–45 kg) (Wanivenhaus 2001, Schwarz 2005).
The stiffness of the PCCS apparatus during torsion has been biomechanically tested at the authors’ hospital in vitro on cat’s tibiae in a model with a 5 mm fracture gap (Behrend 2007). In this research, the torsional stiffness of the PCCS apparatus was compared with the torsional stiffness of an external fixator type Ia and type II. The torsional stiffness of PCCS was comparable with the torsional stiffness of an external fixator type Ia, which was about half of the stiffness of an external fixator type II. However, in this in vitro study, only one double-loop cerclage wire was used on each fragment (Behrend 2007), and therefore it is difficult to compare the results of the biomechanical study with these clinical cases. The authors believe that using additional cerclages will give more stability to the PCCS apparatus. Another biomechanical study has compared the bending stiffness of PCCS and DCP in vitro with a 10 mm fracture gap. The DCP had a higher bending stiffness than the PCCS (Bartolomaeus and others 2007). In the authors’ opinion, the lower rigidity of PCCS might be an advantage in antebrachial fractures in toy breeds because it might avoid bone stress protection and the resulting osteopenia of the radial bone.
Ulna resorption has been described in one study in 7 of 20 fractures (Piras and others 2011) and in 10 of 15 fractures in a second study (Hamilton and others 2005). Stress protection is a possible cause for ulna resorption (Hamilton and others 2005). In the present study, two cases of ulna resorption and one of ulna non-union were noticed. In these cases, the authors also assumed that stress protection was preventing the healing process of the ulna. The authors think that the rigidity of PCCS was high. In these three cases, clamp length was more than 80 per cent in comparison with the length of the radius, and three cerclages were applied to the proximal fragment and two cerclages to the distal fragment in each case.
Radiographic union was achieved at a median time of 13.5 weeks (range: 5–53 weeks) in the present study. This means that healing takes longer compared with other studies in small breed dogs with locking compression plates (mean: 6.9±2.5 weeks) (Gibert and others 2015) or ring external fixation (mean: 10±4 weeks) (Piras and others 2011). However, the authors have been inconsistent with the time periods between radiographic follow-up, and it is possible that this longer healing time is due to longer intervals between radiographs.
In the present study, 4/17 dogs (24 per cent) had major complications because of PCCS implant failure (Table 1). One of the earlier studies described the DCP fixation for distal antebrachial fractures in toy breed dogs with 18 per cent major complications (Larsen and others 1999). A current study reported no major complications with DCP fixation (Ramírez and Macías 2016). Locking compression plates have a low complication rate of 6 per cent (Gibert and others 2015). All cases that needed revision surgery were successfully treated with reapplication of the PCCS method. The authors believe these complications could have been avoided with a better understanding of the PCCS method. Another possible explanation for the complications mentioned might be the various surgeons with different levels of surgical experience and the learning curve all surgeons went through during the time period of the study. Currently there is not much literature available describing the PCCS method and its possibilities for application.
One 1 mm K-wire broke in one dog at the level of the fracture line 4 weeks after surgery (Fig 5). The PCCS apparatus might have been unstable due to distal cerclage movement and that micromovement at the fracture line could have caused implant failure.
FIG 5:

Craniocaudal and mediolateral radiographs of case 14 of the left antebrachium (49-month-old Miniature Pinscher, 2.4 kg). (a) Implant failure after 1 mm clamp breakage, 4 weeks after surgery. (b) Immediate postoperative radiographs (revision) after stabilisation with PCCS (1.2/1.2 mm K-wires). (c) 4 weeks’ postoperative radiographs after stabilisation with PCCS; radial and ulnar fractures are healing. (d) Radiographs after implant removal at 21 months. The radial and ulnar fractures are healed. PCCS, paraosseous clamp-cerclage stabilisation.
In a second dog, no cerclage was placed around the distal fragment, and implant failure occurred due to the unstable distal fracture fixation.
Radiographic follow-up showed two bent clamps (2×0.8 mm diameter) in a third dog 3 weeks after surgery. In this dog, a second proximal radial fracture occurred intraoperatively during drilling. Probably, the use of an inadequate K-wire with a thin diameter (0.8 mm) was a technical error in this case, which led to failure of the clamp. The use of thin K-wires (0.8 mm diameter) makes intraoperative clamp assembly easier, but stiffness might be inadequate.
In another dog, both cerclages around the distal fragment slipped, which led to a radial malunion. Possibly these distal cerclages were not tightened enough or they were difficult to tighten due to the conical shape of the distal fourth of the radius. To avoid this complication hemi-cerclages were used during revision surgery in this dog.
Due to small distal bone size in small breed dogs, revision surgeries after failed fixation for radial fractures are technically challenging. The possible alternatives for redirecting or repositioning screws, even in acute fractured bone, are difficult in bone plate fixation of these cases (Waters and others 1993). However in other studies, revision surgery with bone plate fixation was chosen after failure of previous stabilisation with external coaptation, intramedullary pinning, ESF or after first non-successful plating (Muir 1997, Larsen and others 1999, Hamilton and others 2005).
In the four revision cases included in this study, drilling of new holes was technically achievable because small (1–1.2 mm diameter) K-wires were used.
The authors decided in most cases to remove the implants a few weeks after bone union was apparent on radiographs. In 3 of 10 cases, it was not possible to remove the entire implant apparatus as pieces of the clamp or cerclages were covered with callus. Removal of these pieces would have been possible, but traumatic so it was decided to leave them in situ. In all other cases, implant removal was simple and without any complications. The authors believe that the patients will benefit from routine implant removal in the long term, due to the limited amount of soft tissue coverage at this fracture location. There is not much information in the literature about outcome after implant removal in cases where plates were used for repair of antebrachial fractures (Larsen and others 1999, Hamilton and others 2005, Gibert and others 2015, Ramírez and Macías 2016). In the authors’ opinion, the risk of radial and ulnar refracture post implant removal, especially after plate fixation, in toy breeds is a well-known but rarely described complication (Waters and others 1993, Muir 1997). However, stress fractures through implant holes after external fixator or plate removal have been described in toy breeds (McCartney and others 2010, Baltzer and others 2015).
This study has its limitations; it is a retrospective study with a small sample size and there were variations in the data available in the medical records. However, PCCS is a well-established osteosynthesis method at the authors’ hospital, and the use of PCCS is limited to a small percentage (6 per cent) of the orthopaedic caseload (mainly toy breeds and cats). Various surgeons with different levels of surgical experience were involved in this study, and this resulted in a great deal of variability in how these cases were managed.
In conclusion, PCCS in radial and ulnar fractures of toy breed dogs is a feasible, low-cost and alternative surgical technique compared with other fixation methods. However, a major complication rate of 24 per cent is high. The lack of clinical and biomechanical studies describing the technique and possible errors limit the use of the technique. In the authors’ opinion, the use of (1 mm diameter) K-wire, double simple-twisted cerclage in each fragment with one cerclages at the distal fragment as a hemi-cerclage might reduce the complication rate of PCCS in radial and ulnar fractures in toy breed dogs.
Acknowledgments
The authors acknowledge support from the Open Access Publication Funds of the Freie Universität Berlin.
Footnotes
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: No additional data are available.
References
- Baltzer W. I., Cooley S., Warnock J. J., Nemanic S., Stieger-Vanagas S. M (2015) Augmentation of diaphyseal fractures of the radius and ulna in toy breed dogs using a free autogenous omental graft and bone plating. Veterinary and Comparative Orthopaedics and Traumatology 28, 131–139 doi:10.3415/VCOT-14-02-0020 [DOI] [PubMed] [Google Scholar]
- Bartolomaeus E., Niebauer G. W., Schmiedmayer H. B., Windischbauer G (2007) Comparison of a Paracortical-Clamp-Cerclage and a 3.5 mm dynamic compression plate regarding bending stiffness and strength. Wiener Tierärztliche Monatsschrift 94, 184–191 [Google Scholar]
- Behrend A. Surgical treatment of diaphyseal long bone fracture of the cat: a biomechanical and clinical study (Dissertation). Department of Veterinary Medicine. Freie Universität Berlin; Berlin, 2007:1-128. [Google Scholar]
- Eger C. E. (1990) A technique for the management of radial and ulnar fractures in miniature dogs using translation pins. Journal of Small Animal Practice 31, 377–381 doi:10.1111/j.1748-5827.1990.tb00484.x [Google Scholar]
- Fox D. B., Tomlinson J. L., Cook J. L., Breshears L. M (2006) Principles of uniapical and biapical radial deformity correction using dome osteotomies and the center of rotation of angulation methodology in dogs. Veterinary Surgery 35, 67–77 doi:10.1111/j.1532-950X.2005.00114.x [DOI] [PubMed] [Google Scholar]
- Gibert S., Ragetly G. R., Boudrieau R. J (2015) Locking compression plate stabilization of 20 distal radial and ulnar fractures in toy and miniature breed dogs. Veterinary and Comparative Orthopaedics and Traumatology 28, 441–447 doi:10.3415/VCOT-15-02-0042 [DOI] [PubMed] [Google Scholar]
- Graf G. (2003)Evaluation of clinical application of the paraosseous clamp-cerclage-Stabilization technique in dogs and cats(Dissertation) Vetnerary Medicine University, Wien,1-77. [Google Scholar]
- Hamilton M. H., Langley Hobbs S. J., Hobbs S. L (2005) Use of the AO veterinary mini ‘T’-plate for stabilisation of distal radius and ulna fractures in toy breed dogs. Veterinary and Comparative Orthopaedics and Traumatology : V.C.O.T 18, 18–25 [PubMed] [Google Scholar]
- Lappin M, Aron D, Herron H, et al. . Fractures of the radius and ulna in the dog. The Journal of the American Animal Hospital Association 1983;19:643–50. [Google Scholar]
- Larsen L. J., Roush J. K., McLaughlin R. M (1999) Bone plate fixation of distal radius and ulna fractures in small- and miniature-breed dogs. Journal of the American Animal Hospital Association 35, 243–250 doi:10.5326/15473317-35-3-243 [DOI] [PubMed] [Google Scholar]
- McCartney W., Kiss K., Robertson I (2010) Treatment of distal radial/ulnar fractures in 17 toy breed dogs. Veterinary Record 166, 430–432 doi:10.1136/vr.b4810 [DOI] [PubMed] [Google Scholar]
- Muir P. (1997) Distal antebrachial fractures in toy-breed dogs. Compendium on Continuing Education for the Practicing Veterinarian 19, 137–145 [Google Scholar]
- Piras L., Cappellari F., Peirone B., Ferretti A (2011) Treatment of fractures of the distal radius and ulna in toy breed dogs with circular external skeletal fixation: a retrospective study. Veterinary and Comparative Orthopaedics and Traumatology 24, 228–235 doi:10.3415/VCOT-10-06-0089 [DOI] [PubMed] [Google Scholar]
- Ramírez J. M., Macías C (2016) Conventional bone plate fixation of distal radius and ulna fractures in toy breed dogs. Australian Veterinary Journal 94, 76–80 doi:10.1111/avj.12408 [DOI] [PubMed] [Google Scholar]
- Roe S. C. (1997) Mechanical characteristics and comparisons of cerclage wires: introduction of the double-wrap and loop/twist tying methods. Veterinary Surgery 26, 310–316 doi:10.1111/j.1532-950X.1997.tb01503.x [DOI] [PubMed] [Google Scholar]
- Schwarz G. (2005) Fractures of the Tibial Diaphysis in (AO Principles of Fracture Management in the Dog and Cat. Thieme, NY:AO Publishing; 319–331 [Google Scholar]
- Wanivenhaus G. (2001) Paraossäre Klammer-Cerclage-Stabilisierung: eine Biologische osteosynthesemethode. Wiener Tierärztliche Monatsschrift 88, 123–128 [Google Scholar]
- Waters D, Breur G, Toombs J. Treatment of common forelimb fractures in miniature-and toy-breed dogs. Journal of the American Animal Hospital Association 1993;29:442–8. [Google Scholar]


