Abstract
Background and aims
There are significant gaps in knowledge regarding the role of childhood adversity, interpersonal violence, and suicidal behavior in hypersexual disorder (HD). The aim of this study was to investigate interpersonal violence in hypersexual men compared with healthy volunteers and the experience of violence in relation to suicidal behavior.
Methods
This case–control study includes 67 male patients with HD and 40 healthy male volunteers. The Childhood Trauma Questionnaire – Short Form (CTQ-SF) and the Karolinska Interpersonal Violence Scale (KIVS) were used for assessing early life adversity and interpersonal violence in childhood and in adult life. Suicidal behavior (attempts and ideation) was assessed with the Mini-International Neuropsychiatric Interview (version 6.0) and the Montgomery–Åsberg Depression Rating Scale – Self-rating.
Results
Hypersexual men reported more exposure to violence in childhood and more violent behavior as adults compared with healthy volunteers. Suicide attempters (n = 8, 12%) reported higher KIVS total score, more used violence as a child, more exposure to violence as an adult as well as higher score on CTQ-SF subscale measuring sexual abuse (SA) compared with hypersexual men without suicide attempt.
Discussion
Hypersexuality was associated with interpersonal violence with higher total scores in patients with a history of suicide attempt. The KIVS subscale exposure to interpersonal violence as a child was validated using the CTQ-SF but can be complemented with questions focusing on SA for full assessment of early life adversity.
Conclusion
Childhood adversity is an important factor in HD and interpersonal violence might be related to suicidal behavior in hypersexual men.
Keywords: interpersonal violence, suicidal behavior, hypersexual disorder, childhood trauma
Introduction
Hypersexual disorder (HD) was proposed as a diagnosis in DSM-5 with the suggested conceptualization as a non-paraphilic sexual desire disorder with components of impulsivity, addiction, and compulsivity (Kafka, 2010). However, concerns were raised about the gaps in knowledge, including epidemiology, pathophysiology, and validity of the proposed disorder (Marshall & Briken, 2010; Moser, 2013; Piquet-Pessôa, Ferreira, Melca, & Fontenelle, 2014; Wakefield, 2012; Winters, 2010), and HD was finally not included as a diagnosis in the DSM-5.
During the last decade, several reviews have explored and updated the current knowledge about the proposed models behind the disorder including compulsivity, impulsivity, and behavioral addiction. However, to this day, it is still unclear how to best define and categorize people with excessive sexual behavior as there is insufficient evidence for any of the suggested models (Aaron, 2012; Blum, Badgaiyan, & Gold, 2015; Kaplan & Krueger, 2010; Kor, Fogel, Reid, & Potenza, 2013; Leeman & Potenza, 2013; Stein, 2008). Kraus, Voon, and Potenza (2016) found that recent research show some overlapping features between excessive sexual behavior and substance use disorder including common neurotransmitter systems and dysregulated hypothalamic–pituitary–adrenal axis function. However, significant gaps in understanding still exist and should be further investigated before any conclusions about classification can be made and the authors highlight that more research is needed (Kraus et al., 2016).
Early life adversity is a known risk factor for several psychiatric disorders including substance use disorders, anxiety, and mood disorders (Sachs-Ericsson, Cromer, Hernandez, & Kendall-Tackett, 2009; Teicher & Samson, 2013). Persons with childhood adversity also present more comorbidity and have a greater risk of suicide (Teicher & Samson, 2013). Research suggests that there may be a connection between early life adversity and HD with Långström and Hanson (2006) reporting that individuals with hypersexuality had more often adverse family backgrounds. Especially, sexual abuse (SA) appears to be related to hypersexuality (Aaron, 2012; Kuzma & Black, 2008; Widom, Czaja, & Dutton, 2008). In a recent study, patients with hypersexuality reported significantly higher rates of childhood adversity including SA as well as physical abuse (PA) and emotional abuse (EA) compared with healthy volunteers (Chatzittofis et al., 2016).
Persons with hypersexuality have also reported high rates of psychiatric comorbidity such as mood disorders, substance use disorders, and anxiety disorders (Black, Kehrberg, Flumerfelt, & Schlosser, 1997; Raymond, Coleman, & Miner, 2003) as well as high rates of past suicide attempts (Black et al., 1997).
Childhood adversity is related to suicidality and suicide attempters when compared with healthy volunteers reported more exposure to violence in childhood and experience of violence as an adult measured using Karolinska Interpersonal Violence Scale (KIVS) (Jokinen et al., 2010). Moreover, research has shown an association between the experiences of violence measured using KIVS and increased risk of suicidal behavior in different patient populations including patients with alcohol dependence (Khemiri, Jokinen, Runeson, & Jayaram-Lindström, 2016).
KIVS measures exposure to violence and expression of violent behavior in both childhood and as an adult. In the publication of the KIVS, the Buss–Durkee Hostility Inventory, “Urge to act out hostility” subscale from the Hostility and Direction of Hostility Questionnaire, and the “Early Experience Questionnaire” were used for validation of the new rating scale. The KIVS subscale exposure to interpersonal violence as a child has not been validated against the Childhood Trauma Questionnaire (CTQ), which is the gold standard to measure early life adversity. How experience of violence correlates with HD is not known.
The main aim of this study was to investigate if men with hypersexuality reported more interpersonal violence compared with healthy volunteers and if experience of violence was associated with suicidal behavior in the same group. Since childhood adversity is a proposed indicator for the development of hypersexuality, our first hypothesis was that men with hypersexuality would report more exposure to interpersonal violence in childhood measured using KIVS than healthy volunteers. Moreover, since impulsivity/aggressivity is part of the endophenotype of suicidal behavior, our second hypothesis was that hypersexual men with a history of suicide attempts would report more interpersonal violence compared with hypersexual men without suicidal behavior.
Specific research questions were to investigate the self-reported interpersonal violence in men with hypersexuality and in healthy volunteers, to validate the items in KIVS measuring exposure to violence in childhood using CTQ – Short Form (CTQ-SF), and to investigate if there is an association between experience of interpersonal violence in hypersexual men with a history of suicidal behavior compared with hypersexual men without such a history.
Methods
This study is a case–control study investigating biological markers for hypersexual behavior (Chatzittofis et al., 2016).
Participants
Patients with hypersexual behavior and healthy volunteers were recruited at the Center for Andrology and Sexual Medicine (CASM) at the Karolinska University Hospital to participate in a study of biological markers for hypersexual behavior. A detailed description of the study can be found in Chatzittofis et al. (2016).
Patients
Patients were recruited through advertising in media as well as referrals to the CASM at the Karolinska University Hospital. A total of 67 men with HD were included in this study. The mean age of the patients was 39.2 years (range: 19–65). Inclusion criteria were, besides meeting the diagnosis criteria of HD, an age of 18 years or older and available contact information. Exclusion criteria were alcohol and drug abuse, current psychotic illness, and severe psychiatric disorder that would require immediate treatment and advanced physical illness.
Since HD is not included in DSM-5, patients were diagnosed with HD using the proposed diagnostic criteria proposed by Kafka (2010). Patients had to meet four out of five criteria to be diagnosed with HD.
Healthy volunteers
Forty male healthy volunteers were recruited from the Karolinska Trial Alliance database with efforts performed to match regarding age. The mean age of the healthy volunteers was 37.5 years (range: 21–62). Healthy volunteers were physically healthy with no serious illnesses, no previous or ongoing psychiatric illness, no first-degree relative with schizophrenia, bipolar disorder, or completed suicide, and no previous exposure to serious trauma (assault, natural disasters that required treatment or caused disability). One of the volunteers had a deviant laboratory result in his blood sample and was excluded from the main study. However, since he was not shown to have any psychiatric psychopathology, the assessments were included in this study.
Characteristics of patients with HD and healthy volunteers are shown in Table 1.
Table 1.
Characteristics of patients with HD and healthy volunteers
| Patients (n = 67) | Healthy volunteers (n = 40) | Statistics (Kruskal–Wallis test) p value | ||
|---|---|---|---|---|
| Age | Mean (SD) | 39.2 (11.5) | 37.5 (11.9) | .45 |
| Range | 19–65 | 21–62 | ||
| Civil status | Married | 40 (59.70%) | 19 (47.50%) | .22 |
| In a relationship | 15 (22.39%) | 8 (20%) | ||
| Single | 12 (17.91%) | 13 (32.5%) | ||
| Education | University | 41 (61.19%) | 32 (80%) | .12 |
| Upper secondary | 24 (35.82%) | 7 (17.5%) | ||
| Nine-year compulsory school or less | 2 (2.99%) | 1 (2.5%) | ||
| Employment | Working, studying or parental leave, pension | 64 (95.52%) | 36 (90%) | .52 |
| Unemployed | 2 (2.99%) | 3 (7.5%) | ||
| Long-term sick leave or disability pension | 1 (1.49%) | 1 (2.5%) | ||
| Sexual behavior HD:CAS | Mean (SD) | 10.3 (5.4) | 0.38 (0.88) | <.001 |
| Range | 1–22 | 0–4 |
Note. The Hypersexual Disorder: Current Assessment Scale (HD:CAS) is a dimensional measurement of hypersexual behavior in the recent 2-week time (six questions: 0–4; total scores: 0–24).
Measures
The Mini-International Neuropsychiatric Interview (M.I.N.I., version 6.0) is a validated, structured, diagnostic clinical interview for assessing psychopathology along the Axis I (Sheehan et al., 1998). Patients who reported committing a self-destructive act with some degree of intent to die were regarded as suicide attempters. Interrupted or aborted suicidal acts were also regarded as suicide attempts. The assessment was based on the patient’s reports in M.I.N.I. with further evaluation in the clinical interview.
The following self-rated scales were administrated by the web-based platform.
The Montgomery–Åsberg Depression Rating Scale – Self-rating (MADRS-S) includes nine questions on depressive symptoms to measure the severity of depression. Each question is scored between 0 and 6 points. One question measures zest of life, where 4 points correspond to active suicidal ideation and 6 points to active suicide plans and preparations (Svanborg & Åsberg, 2001). This question will be referred as MADRS-S suicide item.
The KIVS contains four rating scales assessing exposure to violence and expressed violent behavior in childhood (between 6 and 14 years of age) and during adult life (15 years or older). The items are scored between 0 and 5 for each subscale. The KIVS has previously been shown to have high interrater reliability as well as validity (Jokinen et al., 2010; Khemiri et al., 2016).
The CTQ-SF was used for self-assessment of childhood trauma. It has five subscales measuring PA, EA, SA, physical neglect (PN), and emotional neglect (EN). Each subscale includes five items and is scored 5–25. Three additional items constitute a minimization/denial scale to identify individuals that might be underreporting adversity (Bernstein et al., 2003).
The Swedish version of CTQ-SF is shown to have the same construct validity and internal consistency as the original CTQ and giving support for the subscales used in this study measuring childhood abuse (Bernstein & Fink, 1998; Gerdner & Allgulander, 2009).
Procedure
The patients and healthy volunteers were after initial contact with the study coordinators asked to log into a web-based platform, leave their preliminary informed consent to participate in this study, and complete their personal information as well as the self-rated questionnaires. Subsequently, all participants were evaluated in a face-to-face interview by a trained psychiatrist and a psychologist using the M.I.N.I. (Sheehan et al., 1998) to establish psychiatric diagnoses and the diagnosis of HD. According to the inclusion and exclusion criteria, eligible patients and healthy volunteers were enrolled after signing a final written informed consent. Individuals screened positive for pedophilic disorder were also excluded.
Statistical analysis
Initial analyses were carried out to evaluate skewness and kurtosis of the distributions with Shapiro–Wilk test. CTQ total scores and the EA, PA, SA, EN, PN subscale scores were skewed. Group differences were assessed with Wilcoxon test in continuous variables. Tests of non-parametric correlations were performed using Spearman’s rho. The effect sizes were calculated using Cohen’s d (Cohen, 1992). All statistical tests were two-tailed.
The α was set at .05. The Statistical Package JMP 12.1.0 software (SAS Institute, Inc., Cary, NC, USA) was used for all statistical analyses.
Ethics
The study procedures were carried out in accordance with the guidelines of Declaration of Helsinki. The study protocols were approved by the Regional Ethical Review Board in Stockholm (Dnrs: 2013/1335-31/2) and the participants gave their written informed consent to this study.
Results
Interpersonal violence in men with HD and healthy volunteers
The patients had significantly higher scores in the KIVS rating scale measuring exposure to violence in childhood compared with healthy volunteers. The mean value of KIVS subscale exposure to interpersonal violence as a child was 1.45 in patients and 0.8 in healthy controls (HC; z = −2.92, p = .0035, Cohen’s d = 0.6).
The patients also reported significantly more violent behavior as an adult and had a significantly higher total experience of violence measured using KIVS compared with healthy volunteers (z = −2.67, p = .008; z = −2.45, p = .014). There were no significant differences in expression of violence as a child or exposure to violence as an adult between the two groups. The mean values of KIVS subscales for patients and healthy volunteers are presented in Table 2. The correlations of different KIVS subscales of exposure to and expression of violence in patients with HD are reported in Table 3.
Table 2.
Karolinska Interpersonal Violence Scale (KIVS) ratings in 67 patients and 40 healthy volunteers
| Patients (n = 67) | Healthy volunteers (n = 40) | Statistics (Kruskal–Wallis test), p value | Cohen’s d | ||
|---|---|---|---|---|---|
| KIVS total (total experience of violence) | Mean (SD) | 3.84 (2.79) | 2.58 (2.54) | .0143 | 0.472 |
| Range | 0–10 | 0–10 | |||
| KIVS used as a child | Mean (SD) | 0.78 (0.78) | 0.58 (0.59) | .2244 | 0.289 |
| Range | 0–4 | 0–2 | |||
| KIVS used as an adult | Mean (SD) | 0.64 (0.92) | 0.25 (0.54) | .0076 | 0.517 |
| Range | 0–5 | 0–2 | |||
| KIVS exposure as a child | Mean (SD) | 1.45 (1.17) | 0.80 (0.99) | .0035 | 0.599 |
| Range | 0–4 | 0–4 | |||
| KIVS exposure as an adult | Mean (SD) | 0.97 (1.09) | 0.95 (1.15) | .8469 | 0.017 |
| Range | 0–4 | 0–4 |
Table 3.
Correlations between the Karolinska Interpersonal Violence Scale (KIVS) subscales measuring exposure to violence and expression of violent behavior in hypersexual men (n = 67)
| Used violence as a child | Exposure to violence as an adult | Used violence as an adult | |
|---|---|---|---|
| Exposure to violence during childhood | 0.23 | 0.41** | 0.36* |
| Used violence as a child | 0.46** | 0.33* | |
| Exposure to violence as an adult | 0.45** |
p < .01.
p < .001.
Correlation between exposure to violence in childhood measured using KIVS and CTQ-SF in HD
There was a significant correlation between the total value of CTQ-SF and KIVS measuring exposure to violence in childhood in hypersexual patients (p < .01, ρ = 0.36). The CTQ-SF subscales measuring EA and PA showed a significant positive correlation with KIVS measuring exposure to violence in childhood in patients with HD (p < .01; Table 4). The correlations between CTQ-SF measuring SA and KIVS childhood exposure to interpersonal violence were not significant.
Table 4.
Correlations between the Karolinska Interpersonal Violence Scale (KIVS) subscales measuring exposure to violence during childhood and the Childhood Trauma Questionnaire – Short Form (CTQ-SF) subscales measuring abuse in HD (n = 65)
| CTQ-SF total | CTQ EA | CTQ PA | CTQ SA | |
|---|---|---|---|---|
| KIVS, exposure to violence during childhood | 0.36* | 0.32* | 0.32* | 0.13 |
p < .01.
Association between experience of violence and suicidal behavior in hypersexual men
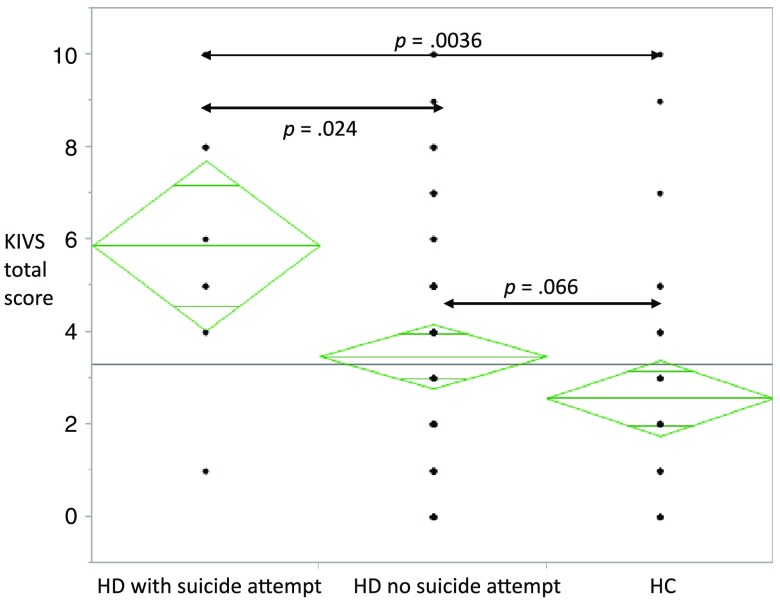
There were no suicide attempts among HC. Eight patients (12%) reported previous suicide attempts and were compared with the remaining cohort of hypersexual men. Suicide attempters reported significantly higher scores on KIVS subscales measuring expression of violence in childhood and exposure to violence as an adult (z = 2.61, p = .0091; z = 2.40, p = .016; Table 5). Furthermore, suicide attempters had significantly higher KIVS total score, representing total experience of violence (z = 2.20, p = .028), as well as higher score on CTQ-SF subscale measuring SA in childhood (z = 2.31, p = .021, Cohen’s d = 0.584). Figure 1 shows KIVS total score in hypersexual men with and without suicide attempt and in HC.
Table 5.
Karolinska Interpersonal Violence Scale (KIVS) ratings in hypersexual men with and without earlier suicide attempt
| Hypersexuality with suicide attempt (n = 8) | Hypersexuality without suicide attempt (n = 59) | Statistics (Kruskal–Wallis test), p value | Cohen’s d | ||
|---|---|---|---|---|---|
| KIVS total (total experience of violence) | Mean (SD) | 5.88 (2.80) | 3.56 (2.69) | .028 | 0.845 |
| Range | 1–10 | 0–10 | |||
| KIVS used as a child | Mean (SD) | 1.63 (1.19) | 0.66 (0.63) | .0091 | 1.018 |
| Range | 0–4 | 0–2 | |||
| KIVS used as an adult | Mean (SD) | 0.75 (0.89) | 0.63 (0.93) | .61 | 0.132 |
| Range | 0–2 | 0–5 | |||
| KIVS exposure as a child | Mean (SD) | 1.5 (1.07) | 1.45 (1.19) | .86 | 0.044 |
| Range | 0–3 | 0–4 | |||
| KIVS exposure as an adult | Mean (SD) | 2.0 (1.41) | 0.83 (0.97) | .016 | 0.967 |
| Range | 0–4 | 0–4 |
Figure 1.
KIVS total score in hypersexual men with and without suicide attempt and in healthy controls (HC)
There were no significant differences between the groups in CTQ-SF total score or in the subscales measuring PA (Cohen’s d = 0.187), EA (Cohen’s d = 0.331), PN (Cohen’s d = 0.230), and EN (Cohen’s d = 0.154 and −0.028). There were no significant differences between the groups in regard or exposure to violence as a child (Cohen’s d = 0.038) or expression of violent behavior as an adult (Cohen’s d = 0.132) measured using KIVS.
Six men with HD scored 4 points in MADRS-S suicide item, the rest of the cohort reporting lower values. There were significant correlations between MADRS-S suicide item and the total score of CTQ-SF as well as with the CTQ-SF subscale measuring SA (ρ = 0.25, p = .048; ρ = 0.27, p = .029). There was no significant correlation between MADRS-S suicide item and KIVS and its subscales, neither with CTQ-SF subscales measuring PA or EA.
Discussion
Regarding the first part of this study, as hypothesized, the patients with HD reported significantly higher rates of exposure to violence during childhood measured using KIVS. Using the same instrument, KIVS, the same result was reported in patients with alcohol dependence (Khemiri et al., 2016). These findings are in line with the literature reporting childhood adversity as a potential risk factor for developing mental health problems as an adult (Aaron, 2012; Sachs-Ericsson et al., 2009; Teicher & Samson, 2013) and increasing the risk of the development of risky sexual behavior (Aaron, 2012). Previous studies have reported high levels of childhood adversity, especially SA in HD (Black et al., 1997; Chatzittofis et al., 2016).
In this study, we also found that persons with HD had expressed more violent behavior as adults and had a higher total experience of violence compared with healthy volunteers. The mean level of used adult violence in men with HD was somewhat higher than recently reported among alcohol-dependent patients (Khemiri et al., 2016). This may be explained by impulsivity component related to HD maybe leading also to aggression dyscontrol or by the fact that the study of Khemiri and coworkers included even women with alcohol dependence and we studied only men with HD. Impulsivity traits are related to addictive behaviors, even incorporated in the definition of HD as well as violent behavior. Since impulsivity is strongly related to genetic factors, it might also explain higher levels of interpersonal violence in men with HD. Unfortunately, we did not have assessment of impulsivity in this study to enable us to do mediation analysis to investigate if impulsivity would be a common factor underlying both interpersonal violence and hypersexual behaviors.
There were significant correlations between the KIVS subscales measuring exposure to violence during childhood and exposure to violence as adult fitting well with findings of earlier studies observing revictimization (Widom et al., 2008). Exposure to violence in childhood correlated with violent behavior as an adult in hypersexual patients and is in line with the literature regarding childhood adversity as a mediating risk factor for later aggressive or violent behavior (Jaffee, Caspi, Moffitt, & Taylor, 2004).
We have already reported (Chatzittofis et al., 2016) that men with HD had significantly higher scores of childhood trauma measured using CTQ-SF compared with healthy volunteers. In this study, the CTQ-SF subscales measuring abuse were used for validation of the KIVS subscale measuring exposure to interpersonal violence during childhood. The correlations between exposure to interpersonal violence in childhood measured using KIVS and CTQ subscales measuring PA and EA were significant in hypersexual patients. The correlation with CTQ total score and KIVS was also significant, indicating that KIVS subscale measuring exposure to violence in childhood has validity as a clinical tool assessing PA and EA.
The correlation between CTQ measuring SA and KIVS was not significant. The CTQ-SF has five questions addressing SA such as “I believe that I was sexually abused” and “someone threatened to hurt me or tell lies about me unless I did something sexual with them” whereas the simple statement “sexually abused” in KIVS could be regarded less sensitive in assessing molestation as well as non-physical SA. This is important to notice and it is thus suggested that KIVS subscale measuring exposure to violence in childhood should be complemented with the questions regarding SA in CTQ for a full evaluation of childhood abuse and especially SA.
Suicide attempters within men with HD reported significantly higher scores on KIVS subscales measuring expression of violence in childhood, exposure to violence as an adult and total experience of violence, as well as higher score on CTQ-SF subscale measuring SA in childhood compared with hypersexual men without suicide attempt. The suicide attempters did not report more exposure to violence in childhood measured using KIVS. Both early life adversity and violent behavior have been repeatedly associated with suicidal behavior (Jokinen et al., 2010; Turecki, Ota, Belangero, Jackowski, & Kaufman, 2014). The suicide attempters in men with HD reported significantly higher values in KIVS total score. The mean total KIVS score of 5.88 among men with HD and suicidal behavior in this study is consistent with mean levels reported in two Swedish follow-up studies of suicide attempters, both reporting mean total KIVS score of 6 (Haglund et al., 2016; Jokinen et al., 2010). This fits also well with findings of Khemiri et al. (2016) on patients with alcohol dependence with suicidal behavior reporting more interpersonal violence compared with patients with alcohol dependence without proneness to suicidality. Furthermore, the KIVS total score was shown to predict completed suicide in previous suicide attempters (Jokinen et al., 2010).
Regarding up to date suicidality measured using MADRS-S in hypersexual men, our results are suggesting a correlation with childhood adversity assessed as CTQ-SF total score. The CTQ subscale measuring SA was also significantly correlated with present suicidal thoughts. These findings could indicate that childhood adversity and especially SA are important factors in suicide risk assessments among men with hypersexuality. However, this correlation has to be replicated and validated with other clinical tools measuring current suicidality before any conclusions can be made about SA in childhood being an indicator of up to date suicidality.
There are a number of limitations that have to be pointed out. First, the childhood abuse measures were through self-report and retrospective, hence depend on the memory of the subjects and possibly could bias the results. We did not control for previous treatments such as 12-step programs that would made individuals more sensitive to identify previous trauma and violence. A third comparison group with addiction (e.g., alcohol) would be of help. Second, the limited number of subjects with suicide attempts (n = 8) and the study design with the use of cross-sectional data does not allow for causal conclusions. The lack of a clinical assessment of personality disorders and the adjustment for comorbidity or other possible confounding factors such as impulsivity traits suggest that the findings should be interpreted with caution until replicated. Furthermore, the size of the HC group was small mainly due to the main research question being stress-related biomarkers, which have been reported earlier (Chatzittofis et al., 2016). For the research questions concerning behavioral measures of interpersonal violence and suicidal behavior in this explorative study, it can be seen as a convenience control group. Despite the fact that the sociodemographic variables did not differ on group level, it would have strengthened the design if more variables in matching the control group had been used.
The age-matched control group of healthy volunteers was screened for absence of present or past psychiatric disorders as well as family history of major psychiatric disorders and major previous traumatic experiences, which can be seen as a strength as well as the careful and thorough diagnostics of the patients with HD and the use of multiple dimensional rating scales.
In conclusion, hypersexual men as hypothesized had significantly more exposure to violence in childhood. They also reported more violent behavior as adults and more total experience of violence measured using KIVS compared with healthy volunteers. EA and PA scales of CTQ-SF and the total value of CTQ-SF showed a significant positive correlation with exposure to violence in childhood measured using KIVS and the KIVS was validated using the CTQ-SF. Suicide attempters reported significantly higher KIVS total score, more expression of violence in childhood, more exposure to violence as an adult as well as higher score on CTQ-SF subscale measuring SA in childhood.
Funding Statement
Funding sources: Funding for this study was provided by the Swedish Research Council (Project numbers: K2009-61P-21304-04-4 and K2009-61X-21305-01-1) and through the Regional Agreement on Medical Training and Clinical Research (ALF) between Stockholm County Council and Karolinska Institutet.
Authors’ contribution
AC, SA, PN, and JJ conceptualized this study. All the authors were responsible for the design of this study. AC, KÖ, and JH were responsible for the data collection and SA coordinated and supervised data collection. AC, JS, and JJ carried out the statistical analyses and were responsible for the interpretation of the data. AC and JS wrote the first draft of the manuscript. All authors revised the paper critically for important intellectual content and gave final approval of the version to be published.
Conflict of interest
The authors declare no conflict of interest.
References
- Aaron M. (2012). The pathways of problematic sexual behavior: A literature review of factors affecting adult sexual behavior in survivors of childhood sexual abuse. Sexual Addiction & Compulsivity: The Journal of Treatment & Prevention, 19(3), 199–218. doi:10.1080/10720162.2012.690678 [Google Scholar]
- Bernstein D. P., Fink L. (1998). Childhood Trauma Questionnaire: A retrospective self-report manual. San Antonio, TX: The Psychological Corporation. [Google Scholar]
- Bernstein D. P., Stein J. A., Newcomb M. D., Walker E., Pogge D., Ahluvalia T., Stokes J., Handelsman L., Medrano M., Desmond D., Zule W. (2003). Development and validation of a brief screening version of the Childhood Trauma Questionnaire. Child Abuse & Neglect, 27(2), 169–190. doi:10.1016/S0145-2134(02)00541-0 [DOI] [PubMed] [Google Scholar]
- Black D. W., Kehrberg L. L., Flumerfelt D. L., Schlosser S. S. (1997). Characteristics of 36 subjects reporting compulsive sexual behavior. American Journal of Psychiatry, 154(2), 243–249. doi:10.1176/ajp.154.2.243 [DOI] [PubMed] [Google Scholar]
- Blum K., Badgaiyan R. D., Gold M. S. (2015). Hypersexuality addiction and withdrawal: Phenomenology, neurogenetics and epigenetics. Cureus, 7(10), e348. doi:10.7759/cureus.348 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chatzittofis A., Arver S., Öberg K., Hallberg J., Nordström P., Jokinen J. (2016). HPA axis dysregulation in men with hypersexual disorder. Psychoneuroendocrinology, 63, 247–253. doi:10.1016/j.psyneuen.2015.10.002 [DOI] [PubMed] [Google Scholar]
- Cohen J. (1992). A power primer. Psychological Bulletin, 112(1), 155–159. doi:10.1037/0033-2909.112.1.155 [DOI] [PubMed] [Google Scholar]
- Gerdner A., Allgulander C. (2009). Psychometric properties of the Swedish version of the Childhood Trauma Questionnaire – Short Form (CTQ-SF). Nordic Journal of Psychiatry, 63(2), 160–170. doi:10.1080/08039480802514366 [DOI] [PubMed] [Google Scholar]
- Haglund A., Lindh A. U., Lysell H., Renberg E. S., Jokinen J., Waern M., Runeson B. (2016). Interpersonal violence and the prediction of short-term risk of repeat suicide attempt. Scientific Reports, 6(1), 36892. doi:10.1038/srep36892 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jaffee S. R., Caspi A., Moffitt T. E., Taylor A. (2004). Physical maltreatment victim to antisocial child: Evidence of an environmentally mediated process. Journal of Abnormal Psychology, 113(1), 44–55. doi:10.1037/0021-843X.113.1.44 [DOI] [PubMed] [Google Scholar]
- Jokinen J., Forslund K., Ahnemark E., Gustavsson J. P., Nordstrom P., Åsberg M. (2010). Karolinska Interpersonal Violence Scale predicts suicide in suicide attempters. Journal of Clinical Psychiatry, 71(8), 1025–1032. doi:10.4088/JCP.09m05944blu [DOI] [PubMed] [Google Scholar]
- Kafka M. P. (2010). Hypersexual disorder: A proposed diagnosis for DSM-V. Archives of Sexual Behavior, 39(2), 377–400. doi:10.1007/s10508-009-9574-7 [DOI] [PubMed] [Google Scholar]
- Kaplan M. S., Krueger R. B. (2010). Diagnosis, assessment, and treatment of hypersexuality. The Journal of Sex Research, 47(2–3), 181–198. doi:10.1080/00224491003592863 [DOI] [PubMed] [Google Scholar]
- Khemiri L., Jokinen J., Runeson B., Jayaram-Lindström N. (2016). Suicide risk associated with experience of violence and impulsivity in alcohol dependent patients. Scientific Reports, 6(1), 19373. doi:10.1038/srep19373 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kor A., Fogel Y., Reid R. C., Potenza M. N. (2013). Should hypersexual disorder be classified as an addiction? Sexual Addiction & Compulsivity, 20(1–2), 27–47. doi:10.1080/10720162.10722013.10768132 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kraus S. W., Voon V., Potenza M. N. (2016). Should compulsive sexual behavior be considered an addiction? Addiction, 111(12), 2097–2106. doi:10.1111/add.1329710.1111/add.13297 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuzma J. M., Black D. W. (2008). Epidemiology, prevalence, and natural history of compulsive sexual behavior. Psychiatric Clinics of North America, 31(4), 603–611. doi:10.1016/j.psc.2008.06.005 [DOI] [PubMed] [Google Scholar]
- Långström N., Hanson R. K. (2006). High rates of sexual behavior in the general population: Correlates and predictors. Archives of Sexual Behavior, 35(1), 37–52. doi:10.1007/s10508-006-8993-y [DOI] [PubMed] [Google Scholar]
- Leeman R. F., Potenza M. N. (2013). A targeted review of the neurobiology and genetics of behavioural addictions: An emerging area of research. Canadian Journal of Psychiatry, 58(5), 260–273. doi:10.1177/070674371305800503 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marshall L. E., Briken P. (2010). Assessment, diagnosis, and management of hypersexual disorders. Current Opinion in Psychiatry, 23(6), 570–573. doi:10.1097/YCO.0b013e32833d15d1 [DOI] [PubMed] [Google Scholar]
- Moser C. (2013). Hypersexual disorder: Searching for clarity. Sexual Addiction & Compulsivity, 20(1–2), 48–58. doi:10.1080/10720162.2013.775631 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Piquet-Pessôa M., Ferreira G. M., Melca I. A., Fontenelle L. F. (2014). DSM-5 and the decision not to include sex, shopping or stealing as addictions. Current Addiction Reports, 1(3), 172–176. doi:10.1007/s40429-014-0027-6 [Google Scholar]
- Raymond N. C., Coleman E., Miner M. H. (2003). Psychiatric comorbidity and compulsive/impulsive traits in compulsive sexual behavior. Comprehensive Psychiatry, 44(5), 370–380. doi:10.1016/S0010-440X(03)00110-X [DOI] [PubMed] [Google Scholar]
- Sachs-Ericsson N., Cromer K., Hernandez A., Kendall-Tackett K. (2009). A review of childhood abuse, health, and pain-related problems: The role of psychiatric disorders and current life stress. Journal of Trauma Dissociation, 10(2), 170–188. doi:10.1080/15299730802624585 [DOI] [PubMed] [Google Scholar]
- Sheehan D. V., Lecrubier Y., Sheehan K. H., Amorim P., Janavs J., Weiller E., Hergueta T., Baker R., Dunbar G. C. (1998). The Mini-International Neuropsychiatric Interview (M.I.N.I.): The development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. Journal of Clinical Psychiatry, 59(Suppl. 20), 22–33; quiz 34–57. [PubMed] [Google Scholar]
- Stein D. J. (2008). Classifying hypersexual disorders: Compulsive, impulsive, and addictive models. Psychiatric Clinics of North America, 31(4), 587–591. doi:10.1016/j.psc.2008.06.007 [DOI] [PubMed] [Google Scholar]
- Svanborg P., Åsberg M. (2001). A comparison between the Beck Depression Inventory (BDI) and the self-rating version of the Montgomery Åsberg Depression Rating Scale (MADRS). Journal of Affective Disorders, 64(2–3), 203–216. doi:10.1016/S0165-0327(00)00242-1 [DOI] [PubMed] [Google Scholar]
- Teicher M. H., Samson J. A. (2013). Childhood maltreatment and psychopathology: A case for ecophenotypic variants as clinically and neurobiologically distinct subtypes. American Journal of Psychiatry, 170(10), 1114–1133. doi:10.1176/appi.ajp.2013.12070957 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turecki G., Ota V. K., Belangero S. I., Jackowski A., Kaufman J. (2014). Early life adversity, genomic plasticity, and psychopathology. Lancet Psychiatry, 1, 461–466. doi:10.1016/S2215-0366(14)00022-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wakefield J. C. (2012). The DSM-5’s proposed new categories of sexual disorder: The problem of false positives in sexual diagnosis. Clinical Social Work Journal, 40(2), 213–223. doi:10.1007/s10615-011-0353-2 [Google Scholar]
- Widom C. S., Czaja S. J., Dutton M. A. (2008). Childhood victimization and lifetime revictimization. Child Abuse & Neglect, 32(8), 785–796. doi:10.1016/j.chiabu.2007.12.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Winters J. (2010). Hypersexual disorder: A more cautious approach. Archives of Sexual Behavior, 39(3), 594–596. doi:10.1007/s10508-010-9607-2 [DOI] [PubMed] [Google Scholar]