Abstract
Background
Preterm birth and small for gestational age (SGA) are strong indicators of neonatal adverse outcomes. With the growing importance of preterm SGA infants, we aim to evaluate the prevalence and risk factors for preterm SGA in China.
Method
We analyzed the data of parents and infants from a population-based cohort research of the free National Pre-pregnancy Checkups Project (NPCP) in rural China. Only singleton live births that occurred between 24 weeks +0 days and 36 weeks +6 days of pregnancy were included in this study. SGA was defined as birth weight less than the 10th percentile of the reference birth-weight-for-gestational-age population. A multiple logistic regression model was built using the statistically significant variables from the 371 variables in the questionnaire.
Results
A total of 11,474 singleton, preterm, live-birth infants were included. Of the total infants, 317 (2.77%) were preterm SGA infants. A higher risk of preterm SGA infants was observed among mothers who were on oral contraceptives (OR: 8.162, 95% CI: 1.622–41.072), mothers who had syphilis (OR: 12.800, 95% CI: 1.250–131.041), and mothers with a high eosinophil percentage (OR: 13.292, 95% CI: 1.282–135.796). Maternal intake of folic acid at least 3 months before pregnancy (OR: 0.284, 95% CI:0.124–0.654) and paternal intake of egg and meat (OR: 0.097,95% CI:0.030–0.315) were protective factors. Compared with North China, the incidence of preterm SGA infants was higher in South China.
Conclusion
Preterm SGA infants were associated with both maternal and paternal factors.
Keywords: Preterm delivery, Small for gestational age, Folic acid supplementation, Oral contraceptive
Background
Gestational age and birth weight are two of the most important factors for evaluating the prognosis of infants. Small for gestational age (SGA) infants may show a decrease in their growth due to intrauterine growth restriction. Limitations in fetal growth affect the development of the cardiovascular system or other organs, which can have life-long effects on an individual [1]. Preterm birth is a significant causative factor of infant and child morbidity and mortality. Preterm birth complications are estimated to be the second most common cause of death in children under 5 years old [2]. In addition to its contribution to mortality, preterm birth has lifelong effects, and increased risk of neurodevelopmental disorders and chronic diseases in adulthood [3]. There is a growing consensus on the differentiation of preterm SGA from term SGA infants from both the clinical and research perspectives [4]. In particular, preterm SGA infants have a 10–40 times greater risk of dying in the first month of life than term appropriate for gestational age (AGA) infants [5]. Further, preterm SGA infants have a relatively low body fat percentage and would experience a postnatal catchup growth. Many epidemiological studies have demonstrated that the catch-up growth is associated with cardiovascular diseases, obesity, hypertension, type-2 diabetes, and metabolic syndrome in later life [6]. Few studies have evaluated the risk factors of preterm SGA infants [7, 8]. The purpose of present study is to identify the risk factors of preterm small-for-gestational age infants. The knowledge gained from this study will be crucial in prevention and treatment of preterm SGA.
Methods
Subjects
A population-based retrospective cohort study was performed on 248,501 couples and their children who were part of the free National Pre-pregnancy Checkups Project (NPCP) in 220 pilot counties in 30 provinces in China between January 2010 and December 2012. The project was implemented by the Chinese National Health and Family Planning Commission and Ministry of Finance with aim of preventing birth defects in China, it is the largest pregnancy retrospective cohort study of the preconception stage in China. It covered all volunteer couples who planned to conceive within the next 6 months. The clinical data were collected during the preconception medical examination. Information on socioeconomic background, reproductive history and history of illness, lifestyle, and dietary habits was carefully collected through face-to-face interviews by qualified nurses. Physical examinations and biochemical studies were also carried out by medical staff at the same time [9].
SGA was defined by a 1995 WHO expert committee as infants with body weight below the 10th percentile of a birth-weight-for-gestational-age, using the gender-specific reference population with the local growth standards of Li Zhu et al. [10] Zhu’s neonatal growth standards were derived from birth weight data obtained from a nationwide neonatology network of 161,420 live births in China from 2011 to 2014. Preterm SGA infants in our study were defined as infants born small for gestational age between 24 weeks + 0 days and 36 weeks +6 days of gestation.
The inclusion and exclusion criteria are shown in Fig. 1. A couple and their children was considered as a single subject. We included a total of 11,474 subjects.
Fig. 1.
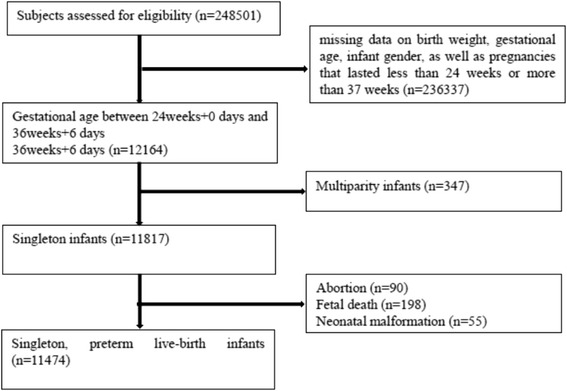
Participant flow chart
Design and setting
Data collection
A structured questionnaire was constructed by well-trained investigators; the questionnaire included 371 variables from the National Free Preconception Health Examination Project [9, 11]. As the adverse effect of preterm large-for-gestational age (LGA) infants is controversial [12, 13], we compared preterm SGA infants with preterm non-SGA infants including the preterm AGA and LGA infants. We divided China into North and South region by the Qinling Mountain-Huaihe River Line and we compared the prevalence of preterm SGA infants in both regions. We also assessed the risk factors of preterm SGA infants.
Selection of risk factors
The questionnaire involves 19 aspects including baseline characters of couples, physical examination, laboratory examination family history of couples etc. We chose the variables with a high data integrity over 80%. Among these variables, 38 variables were statistically significant exposures in univariate analysis including education level of the parents, maternal preconception intake of narcotics and paternal second-hand smoking, maternal intake of eggs and meat, the beginning time of maternal intake of folic acid, paternal intake of eggs and meat and paternal intake of vegetables, tense maternal and paternal relationship with relatives and co-workers, paternal exposure to heavy metals, organic solutes and vibrations, maternal syphilis and Candida infection, maternal drug use, pet exposure and influenza virus infection during pregnancy, maternal medical history of diabetes mellitus (DM), maternal medical history of hepatitis B, maternal oral contraceptive use, maternal family history of neonatal death, paternal hepatitis B vaccination and paternal family history of DM, maternal height (meter), maternal weight (kilogram), maternal BMI (kg/m2), maternal red blood cell count (109/L), maternal eosinophil percentage, maternal blood glucose level (mmol/L) and paternal height. It also included the presence of maternal HBe antibodies, maternal rubella virus IgG antibodies, maternal CMV IgG antibodies, maternal toxoplasma IgG antibodies, paternal HBs antibodies. The folic acid supplementation, the preconception habits and socioeconomic status of the parents were based on self-report. The location was classified as North or South region of China by the Qinling Mountain-Huaihe River Line.
Statistical analysis
All risk factor variables were first examined by univariate analysis to assess the importance of each of them on preterm SGA. We used chi-square test for analysis of categorical variables, and the Mann-Whitney U test for analysis of continuous variables with a skewed distribution as all of continuous variables were of skewed distribution in this cohorts examined by Kolmogorov-Smirnov test. The continuous skewed variables were expressed in the form of mid-values (25th percentile, 75th percentile). When a variable was found to be significant at the 0.1 level, it was entered into the multivariate model. Stepwise logistic regression was used to examine the correlation between risk factors and preterm SGA. In logistic regression, p < 0.05 was considered statistical significance. The results were presented using the OR and 95% CI values. The analyses were performed with SPSS (version 19.0; SPSS Inc., Chicago, IL, USA).
Results
Baseline characteristics of SGA and non-SGA
A total of 248,501 infants were recruited in our database, of which 12,164 were preterm infants (5.63%). The preterm neonatal mortality was 1.69% in our study. The mean weight of 11,474 preterm singleton live-birth infants was 3104.87 ± 636.03 g, 6307 infants of them were male (54.97%). Among them, 317 (2.77%) were preterm singleton live-birth SGA infants. The mean weight of them was 1778.26 ± 438.58 g, 189 of them were male (59.62%). 11,157 of them were preterm singleton live-birth non-SGA infants, the mean weight was 3141.73 ± 595.51 g, 6118 of them were male (54.84%).
Univariate analysis
The following tables show the risk factors in preterm SGA deliveries. Table 1 indicates that maternal intake of narcotics lead to a higher risk of preterm SGA. Nutrition status is also described in Table 1. Parents who did not consume enough vegetables, eggs or meat were more likely to deliver preterm SGA infants, which reflects the paternal level of essential vitamin and proteins. Starting time of maternal folic acid supplement is described in Table 1. Mothers who used folic acid at least 3 months before last menstrual period (LMP) had a lower risk of giving birth to preterm SGA infants. We also noticed that a total of 3701 women (32.6%) in our study did not take folic acid before or after their pregnancy, even though it is routinely recommended by their health care providers.
Table 1.
The univariate analysis of risk factors of preterm SGA infants (categorical variables)
| Risk factors | Number of SGA | Number of Non-SGA | P value |
|---|---|---|---|
| Maternal Education years | |||
| 0 | 2 | 27 | 0.000 |
| 0–6 | 19 | 444 | |
| 6–9 | 181 | 7743 | |
| 9–12 | 71 | 1713 | |
| 12–16 | 38 | 966 | |
| > 16 | 1 | 6 | |
| Paternal Education years | |||
| 0 | 1 | 13 | 0.008 |
| 0–6 | 13 | 337 | |
| 6–9 | 189 | 7464 | |
| 9–12 | 70 | 1922 | |
| 12–16 | 33 | 1066 | |
| > 16 | 0 | 10 | |
| Maternal intake of narcotics | |||
| Yes | 4 | 29 | 0.012 |
| No | 208 | 10,782 | |
| Paternal second-hand smoking | |||
| Regular | 13 | 358 | 0.091 |
| Occasional | 90 | 3732 | |
| No | 191 | 6089 | |
| Maternal intake of eggs and meat | |||
| No | 9 | 155 | 0.045 |
| Yes | 292 | 10,675 | |
| Maternal intake of vegetable | |||
| No | 10 | 94 | 0.000 |
| Yes | 290 | 10,737 | |
| Maternal intake of folic acid from at least 3 months before LMP | |||
| Yes | 73 | 3448 | 0.003 |
| No | 241 | 7584 | |
| Paternal intake of eggs or meat | |||
| No | 8 | 125 | 0.003 |
| Yes | 286 | 10,073 | |
| Paternal intake of vegetables | |||
| No | 5 | 81 | 0.094 |
| Yes | 289 | 10,104 | |
| Maternal tense relationship with relatives and co-workers | |||
| No | 272 | 10,098 | 0.000 |
| Low | 29 | 597 | |
| Moderate | 0 | 143 | |
| High | 2 | 3 | |
| Paternal tense relationship with relatives and co-workers | |||
| No | 261 | 9403 | 0.075 |
| Low | 2 | 627 | |
| Moderate | 4 | 162 | |
| High | 0 | 5 | |
| Paternal exposure to heavy metals | |||
| Yes | 4 | 28 | 0.011 |
| No | 313 | 11,489 | |
| Paternal exposure to organic solutes | |||
| Yes | 5 | 528 | 0.006 |
| No | 312 | 10,989 | |
| Paternal exposure to vibrations | |||
| Yes | 4 | 54 | 0.076 |
| No | 313 | 11,463 | |
| Maternal syphilis infection | |||
| Yes | 4 | 29 | |
| No | 293 | 10,656 | |
| Maternal Candida infection | |||
| Yes | 2 | 80 | 0.003 |
| No | 269 | 10,138 | |
| Maternal HBe antibodies | |||
| Positive | 31 | 770 | 0.024 |
| Negative | 255 | 9855 | |
| Maternal rubella virus IgG antibodies | |||
| Positive | 136 | 4114 | 0.022 |
| Negative | 153 | 6355 | |
| Maternal CMV IgG antibodies | |||
| Positive | 79 | 2312 | 0.068 |
| Negative | 204 | 8022 | |
| Maternal toxoplasma IgG antibodies | |||
| Positive | 9 | 148 | 0.052 |
| Negative | 273 | 10,190 | |
| Paternal HBs antibodies | |||
| Positive | 83 | 2555 | 0.077 |
| Negative | 198 | 7413 | |
| Maternal medication us after LMP | |||
| Yes | 20 | 274 | 0.000 |
| No | 294 | 10,758 | |
| Maternal pet exposure after LMP | |||
| Yes | 11 | 171 | 0.018 |
| No | 305 | 10,942 | |
| Maternal influenza virus infection after LMP | |||
| Yes | 9 | 92 | 0.002 |
| No | 305 | 11,021 | |
| Maternal medical history of hepatitis B | |||
| Yes | 4 | 51 | 0.076 |
| No | 299 | 10,811 | |
| Maternal oral contraceptive use | |||
| Yes | 4 | 56 | |
| No | 300 | 10,732 | |
| Maternal family history of neonatal death | |||
| Yes | 2 | 4 | 0.010 |
| No | 300 | 10,846 | |
| Paternal hepatitis B vaccination | |||
| Yes | 66 | 2980.017 | |
| No | 230 | 7273 | |
| Paternal family history of DM | |||
| Yes | 4 | 47 | 0.055 |
| No | 292 | 10,716 | |
| Location | |||
| North | 60 | 3671 | 0.000 |
| South | 257 | 7486 | |
Paternal exposure to heavy metals, organic solutes and vibrations were associated with a higher incidence of preterm SGA. Parental infections were also identified as important risk factors. Syphilis, Candida infection, rubella virus infection, CMV infection, toxoplasma infection were associated with higher rate of preterm SGA. Hepatitis B is common in China. Positive maternal HBe antibodies is associated with higher prevalence of preterm SGA. Moreover, maternal family history of hepatitis B was associated with higher rate in preterm SGA infants while paternal hepatitis B vaccination was associated with lower rate in preterm SGA infants.
Mothers who were taking medications, came into contact with pets or had influenza virus infection were more likely to have preterm SGA infants. With regard to the medical history of the parents, maternal family history of neonatal death were associated with a higher rate of preterm SGA.
The Qinling Mountain-Huaihe River Line is an important demarcation line of climate, hydrology, and topography in China [14]. The North China has a lower rate of preterm SGA rate (1.61% vs. 3.32%). The mean birth weight of preterm live-birth was 3188.58 ± 650.67 g in North China and 3061.78 ± 636.03 g in South China.
As expected, the parental weight, height and BMI were associated with preterm SGA as shown in Table 2. The median values were used for risk factors that showed skewed distribution. The maternal weight, height, BMI and paternal height were significantly lower and the maternal eosinophil ratio was higher in preterm SGA group.
Table 2.
The univariate analysis of risk factors of preterm SGA infants (continuous variables)
| Risk factors | SGA Median(quartile) | Non-SGA Median(quartile) | P value |
|---|---|---|---|
| Maternal age | 24.00 (22.00–27.00) | 24.00 (22.00–27.50) | 0.571 |
| Maternal height (meter) | 159.00 (156.00–161.00) | 160.00 (156.00–162.00) | 0.081 |
| Maternal weight (kilogram) | 52.00 (48.00–56.00) | 52.00 (49.00–57.00) | 0.027 |
| Maternal BMI before LMP (kg/m2) | 20.32 (18.89–22.31) | 20.70 (19.38–22.38) | 0.063 |
| Maternal red blood cell count (109/L) | 4.22 (3.90–4.51) | 4.13 (3.80–4.48) | 0.005 |
| Maternal eosinophil percentage | 2.00 (0.73–3.48) | 1.10 (0.10–2.50) | 0.017 |
| Maternal blood glucose level (mmol/L) | 4.90 (4.39–5.50) | 4.82 (4.30–5.30) | 0.018 |
| Paternal height (meter) | 170.00 (168.00–173.25) | 171.00 (169.00–175.00) | 0.031 |
Multivariable analysis
Table 3 shows the results of multiple logistic regression of preterm SGA. Higher risks of preterm SGA infants were observed among women who took oral contraceptives (OR: 8.162, 95% CI: 1.622–41.072), women with higher eosinophil percentage (OR: 1.067, 95% CI: 1.010–1.127) and women with syphilis infection (OR: 13.292, 95% CI: 1.282–135.796). Frequent intake of meat and egg of father (OR: 0.097, 95% CI: 0.030–0.315) was found to be a protective factor for infants. Comparing with women who did not use folic acid or started using folic acid after 3 months before LMP, intake of folic acid from 3 months before LMP (OR: 0.284, 95% CI:0.124–0.654) was also a protective factor for preterm SGA infants. It is well accepted that maternal BMI before LMP is related to the rate of preterm and SGA. So we put the maternal BMI before LMP (OR: 0.945, 95% CI: 0.828–1.709) in the regression model although it was not statistically significant. Moreover, the confidence intervals are wide for some of the factors in the logistic model may due to the small sample size of preterm SGA.
Table 3.
Multiple logistic regression of preterm SGA infants
| Risk factors | B | P value | OR | 95% C.I. for OR | |
|---|---|---|---|---|---|
| Lower | Upper | ||||
| Maternal intake of folic acid from at least 3 months before LMP | −1.257 | 0.003 | 0.284 | 0.124 | 0.654 |
| Maternal oral Contraceptive use | 2.100 | 0.011 | 8.162 | 1.622 | 41.072 |
| Maternal eosinophil percentage | 0.064 | 0.021 | 1.067 | 1.010 | 1.127 |
| Maternal syphilis infection | 2.580 | 0.030 | 13.191 | 1.281 | 135.796 |
| Paternal intake of egg and meat | −2.336 | 0.000 | 0.097 | 0.030 | 0.315 |
| Maternal BMI before LMP | −0.056 | 0.403 | 0.945 | 0.828 | 1.709 |
| Constant | 1.357 | 0.401 | 3.886 | ||
Discussion
Birth weight and gestational age are considered as strong predictors of short-term and long-term prognosis of infants. Given the growing attention paid to preterm SGA infants, our study attempted to determine the incidence of the preterm SGA infants and the risk factors associated with delivering preterm SGA infants.
A major strength of this study is its large sample size and the large number of variables analyzed. To the best of our knowledge, this is the most extensive multi-center study in China to evaluate the risk factors associated with preterm SGA infants. The large number of variables allows us to analyze more risk factors than previous studies on preterm SGA infants. The effect of paternal factors on preterm SGA infants, for example, the maternal eosinophil percentage has rarely been reported before.
This database has several unique features. Compared with earlier study, the mortality rate of preterm infants in our study (5.63%) was lower than the average rate reported for eastern Asia (7.2% (5.4–9.0)) [15]. With economic growth and improvements in perinatal care, the neonatal mortality rate has decreased by 59.3% from 2000 to 2010 in China [16], which could be due to lower rate of preterm SGA. With regard to the low prevalence of preterm SGA infants in the North China, it could be explained by the significant difference in body weight and height between the Northern and Southern Han Chinese. It also fit the Bergmann’s rule as body mass increases with colder climate [17, 18]. The greater weight and height of parents in the North could explain the lower incidence of preterm SGA in North China.
In our study, we discovered a gender-based difference in the incidence of preterm SGA infants in China; 59.62% of preterm SGA infants were male. It has been reported that boys are more likely to be born before term in a different of populations [19]. A possible explanation is that in preterm infants, the growth-promoting effect of androgen is not obvious. Moreover, the male preterm infants were more likely to meet the preterm SGA criteria, as the weight standard for males is higher than that for females.
Folic acid
Insufficient periconceptional folic acid intake is associated with a number of birth defects that may also be related to genetic and environmental factors before conception or during early pregnancy [20]. Recent study has shown that supplementation of folic acid could protect against preterm birth. This study also suggests that the duration of folic acid supplementation may be as important as the dose. The risk of spontaneous preterm birth was inversely related to the duration of folic acid supplementation, and was lowest in women who reported using folic acid supplementation for more than a year prior to conception [21]. However, it is controversial whether folic acid supplementation influence the incidence of low birth weight or SGA [21–23]. In our study, taking folic acid supplementation more than 3 months before LMP was associated with a significant reduction in incidence of preterm SGA. As mentioned before, 32.6% of the women in this study did not take folic acid before or during pregnancy, even it is routinely recommended. Considering the large percentage of subjects were from rural areas with relatively poor nutrition status, we think that health care providers in these areas, in particular, should emphasize on folic acid supplementation before pregnancy.
Oral contraceptive
Oral contraceptives use is one of the most popular reversible methods of contraception. However, the adverse effects of oral contraceptives on fetal development are unclear. Previous studies have reported the association of oral contraceptive use and preterm birth and low birth weight [24, 25]. It should be noted that oral contraceptive use is rare in China compared to developed countries; only 1.31% of women who delivered preterm SGA infants and 0.47% of women who delivered preterm non-SGA infants used oral contraceptives. In contrast, it was reported that oral contraceptive account for 79% of all contraception in America for the same period [26]. Nonetheless, we observed that the use of oral contraceptives was associated with preterm SGA infants. A possible explanation is that increased levels of estrogen at the time of blastocyst implantation may contribute to an increased risk of preterm birth, which has been shown in women undergoing fresh embryo-based transfer for in vitro fertilization [27, 28]. It is undeniable that oral contraceptives have many advantages in birth control and regulating the menstrual cycle, but physicians should be aware of its potential side effects of delivering preterm SGA infants.
Maternal eosinophil percentage
Eosinophils have been shown to be a significant cellular infiltrate of the placenta and uterus, including the infiltration and degranulation of eosinophils in the cervix of pregnant humans [29]. The roles of eosinophils in preterm delivery or SGA remains unknown. Elevation of the eosinophil level is associated with chronic inflammation or enhanced immune reactions, which may associate with preterm SGA infants. As the eosinophil percentage is not routinely determined in pregnancy, further research needs to be conducted to explore the relationship between the eosinophil percentage and pregnancy.
Infection of syphilis
Despite being easily detectable and treatable during pregnancy, syphilis remains an important cause of adverse pregnancy outcomes [30]. Syphilis in pregnancy may lead to severely adverse pregnancy outcome such as abortion, prematurity, neonatal death and congenital syphilis in the newborn [31]. In China, the incidence of congenital syphilis has increased at an alarming rate of 71.9% per year from 0.01 to 19.68 cases per 100,000 live births from 1997 to 2005 [32]. A study released in 2013 indicated that total incidence of maternal syphilis in China was estimated as 0.30% (95% CI: 0.28–0.32) [32]. In our study, the incidence of maternal syphilis was 1.35% in women who delivered preterm SGA infants, which was much higher than the incidence in women who delivered preterm non-SGA infants (0.271%). Unless testing and treatment of syphilis during pregnancy are made universally available, over half of the pregnancies in women with syphilis will have adverse outcome [33]. Primary prevention and prenatal care are needed to be addressed to reduce the incidence of syphilis associated preterm SGA infants.
Nutrition status of father
Our study showed that diet containing egg and meat of the father, which reflected the paternal nutritional status, particularly protein intake, was significantly associated with lower incidence of preterm SGA infants. Animal studies have demonstrated that all stages of gamete maturation and preimplantation embryo development are influenced directly by parental nutrition and hormonal status [34]. Moreover, an animal model showed that the diet during the preconception period and pregnancy of the males and females differentially affects embryonic growth and fatty acid content [35]. Also, there is an animal study showed that paternal nutrition can influence the amount of seminiferous tissue, spermatogenic capacity and spermatogenic efficiency [36]. However, our understanding of the influence of paternal nutritional status on human offspring is still limited.
Limitation
The primary limitation of our study is that several risk factors such as the beginning time of maternal folic acid intake, the paternal intake of egg and meat, and the use of oral contraceptive were based on self-report of the parents. More quantitative variables are needed in our questionnaire. With the large number of subjects, it is difficult to assure the completeness of data. This study identified several factors that are associated with preterm SGA, due to diverse culture and social economic status of these subjects, some confounding factors might be overlooked.
Conclusion
Our results show that preterm SGA infants were associated with both maternal and paternal factors. Maternal use of oral contraceptives, maternal syphilis infection, maternal higher eosinophil percentage, maternal folic acid intake less than 3 months before pregnancy and paternal low protein diet were associated with preterm SGA.
Acknowledgments
We thank all the participants in this research and all the medical staffs in the 220 counties for their hard work in NFPC. We also gratefully thank the valuable support of Xu Ma (National Research Institute for Family Planning, No. 12, Dahuisi Road, Haidian District, Beijing 100081, China), QiaoMei WANG, HaiPing SHEN and YiPING ZHANG (National health and family planning commission of the people’s republic of China).
Funding
This study was supported by the “Five-twelfth” National Science and Technology Support Program (No.2012BAI41B08, No.2013BAI12B01) and the National Natural Science Foundation (No.41401469), People’s Republic of China.
Availability of data and materials
The datasets during the current study are available from the corresponding author on reasonable request.
Abbreviations
- AGA
Appropriate for gestational age
- DM
Diabetes mellitus
- LGA
Large for gestational age
- LMP
Last menstrual period
- SGA
Small for gestational age
Authors’ contributions
SC data analysis and drafting of manuscript. RZ data analysis and drafting of manuscript. HZ paper review and analysis of data. HY acquisition and interpretation of data and paper review. FG study design and drafting of manuscript. LW technical support, acquisition of data and paper review. YJ acquisition and interpretation of data and drafting of manuscript. BQL data analysis and paper review. CY acquisition and interpretation of data and drafting of manuscript. JL acquisition of data, technical support and paper review. QW acquisition of data, technical support and paper review. SZ study design and paper review. HP paper review and study supervision. All authors read and approved the final manuscript.
Ethics approval and consent to participate
The study was approved by the medical ethics committee of the Peking Union Medical College Hospital. Informed consent was obtained from all NFPC participants.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Shi Chen, Email: cspumch@163.com.
Rong Zhu, Email: seth_zhu@163.com.
Huijuan Zhu, Email: shengxin2004@163.com.
Hongbo Yang, Email: hongbo.yang7@gmail.com.
Fengying Gong, Email: fygong@sina.com.
Linjie Wang, Email: eileenwood@163.com.
Yu Jiang, Email: wingedsky@gmail.com.
Bill Q. Lian, Email: qylian@yahoo.com
Chengsheng Yan, Email: fyycs@sina.com.
Jianqiang Li, Email: lijianqiang@bjut.edu.cn.
Qing Wang, Email: qing.wang@tsinghua.edu.cn.
Shi-kun Zhang, Email: shikun888@sina.com.
Hui Pan, Phone: 86-10-69155845, Email: panhui20111111@163.com.
References
- 1.Sochet AA, Ayers M, Quezada E, et al. The importance of small for gestational age in the risk assessment of infants with critical congenital heart disease. Cardiol Young. 2013;23:896–904. doi: 10.1017/S1047951113001960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Liu L, Johnson HL, Cousens S, Perin J, et al. Global, regional, and national causes of child mortality: an updated systematic analysis for 2010 with time trends since 2000. Lancet. 2012;379:2151–2161. doi: 10.1016/S0140-6736(12)60560-1. [DOI] [PubMed] [Google Scholar]
- 3.Mwaniki MK, Atieno M, Lawn JE, Newton CR. Long-term neurodevelopmental outcomes after intrauterine and neonatal insults: a systematic review. Lancet. 2012;379:445–452. doi: 10.1016/S0140-6736(11)61577-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Crispi F, Llurba E, Dominguez C, Martin-Gallan P, Cabero L, Gratacos E. Predictive value of angiogenic factors and uterine artery Doppler for early- versus late-onset pre-eclampsia and intrauterine growth restriction. Ultrasound Obstet Gynecol. 2008;31:303–309. doi: 10.1002/uog.5184. [DOI] [PubMed] [Google Scholar]
- 5.Katz J, Lee ACC, Kozuki N, et al. Mortality risk in preterm and small-for-gestational-age infants in low-income and middle-income countries: a pooled country analysis. Lancet. 2013;382:417–425. doi: 10.1016/S0140-6736(13)60993-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Okada T, Takahashi S, Nagano N, Yoshikawa K, Usukura Y, Hosono S. Early postnatal alteration of body composition in preterm and small-for-gestational-age infants: implications of catch-up fat. Pediatr Res. 2015;77:136–142. doi: 10.1038/pr.2014.164. [DOI] [PubMed] [Google Scholar]
- 7.Ota E, Ganchimeg T, Morisaki N, et al. Risk factors and adverse Perinatal outcomes among term and preterm infants born small-for-gestational-age: secondary analyses of the WHO multi-country survey on maternal and newborn health. PLoS One. 2014;9:e105155. doi: 10.1371/journal.pone.0105155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zeitlin JA, Ancel PY, Saurel-Cubizolles MJ, Papiernik E. Are risk factors the same for small for gestational age versus other preterm births? Am J Obstet Gynecol. 2001;185:208–215. doi: 10.1067/mob.2001.114869. [DOI] [PubMed] [Google Scholar]
- 9.Wang Y, Cao Z, Peng Z, et al. Folic acid supplementation, preconception body mass index, and preterm delivery: findings from the preconception cohort data in a Chinese rural population. BMC Pregnancy Childbirth. 2015;15:336. doi: 10.1186/s12884-015-0766-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zhu L, Zhu R, Zhang S, et al. Chinese neonatal birth weight curve for different gestational age. Chin J Pediatr. 2015;53:97–103. [PubMed] [Google Scholar]
- 11.Liu J, Zhang S, Wang Q, et al. Seroepidemiology of hepatitis B virus infection in 2 million men aged 21–49 years in rural China: a population-based, cross-sectional study. Lancet Infect Dis. 2016;16:80–6. [DOI] [PubMed]
- 12.Mardones F, Marshall G, Viviani P, et al. Estimation of individual neonatal survival using birthweight and gestational age: a way to improve neonatal care. J Health Popul Nutr. 2008;26:54–63. [PMC free article] [PubMed] [Google Scholar]
- 13.Wennerstrom EC, Simonsen J, Melbye M. Long-term survival of individuals born small and large for gestational age. PLoS One. 2015;10:e0138594. doi: 10.1371/journal.pone.0138594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Fang J, Song Y, Liu H, Piao S. Vegetation-climate relationship and its application in the division of vegetation zone in China. Acta Bot Sin. 2002;44:1105–1122. [Google Scholar]
- 15.Blencowe H, Cousens S, Oestergaard MZ, et al. National, regional, and worldwide estimates of preterm birth rates in the year 2010 with time trends since 1990 for selected countries: a systematic analysis and implications. Lancet. 2012;379:2162–2172. doi: 10.1016/S0140-6736(12)60820-4. [DOI] [PubMed] [Google Scholar]
- 16.Feng J, Yuan X, Zhu J, et al. Under-5-mortality rate and causes of death in China, 2000 to 2010. Chin J Epidemiol. 2012;33:558–561. [PubMed] [Google Scholar]
- 17.Ma L, Cao Y, Xu J, He J. The relationship between the stature and the geo-environmental factors of 102 populations in China. Acta Anthropologica Sinica. 2008;27:223–231. [Google Scholar]
- 18.Li Y, Zheng L, Xi H, et al. Body weight difference in Han Chinese populations. Acta Anatomica Sinica. 2015;46:270–274. [Google Scholar]
- 19.Zeitlin J, Saurel-Cubizolles MJ, De Mouzon J, Rivera L, et al. Fetal sex and preterm birth: are males at greater risk? Hum Reprod. 2002;17:2762–2768. doi: 10.1093/humrep/17.10.2762. [DOI] [PubMed] [Google Scholar]
- 20.De-Regil LM, Fernandez-Gaxiola AC, Dowswell T, Pena-Rosas JP. Effects and safety of periconceptional folate supplementation for preventing birth defects. Cochrane Database Syst Rev. 2010;6:CD007950. [DOI] [PMC free article] [PubMed]
- 21.Bukowski R, Malone FD, Porter FT, et al. Preconceptional folate supplementation and the risk of spontaneous preterm birth: a cohort study. PLoS Med. 2009;6:e1000061. doi: 10.1371/journal.pmed.1000061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kim MW, Ahn KH, Ryu KJ, et al. Preventive effects of folic acid supplementation on adverse maternal and fetal outcomes. PLoS One. 2014;9:e97273. doi: 10.1371/journal.pone.0097273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Central Technical Co-ordinating Unit ITC-oUI Multicentric study of efficacy of periconceptional folic acid containing vitamin supplementation in prevention of open neural tube defects from India. Indian J Med Res. 2000;112:206–211. [PubMed] [Google Scholar]
- 24.Jensen ET, Daniels JL, Sturmer T, et al. Hormonal contraceptive use before and after conception in relation to preterm birth and small for gestational age: an observational cohort study. BJOG. 2015;122:1349–1361. doi: 10.1111/1471-0528.13114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Chen XK, Wen SW, Sun LM, Yang Q, Walker MC, Krewski D. Recent oral contraceptive use and adverse birth outcomes. Eur J Obstet Gynecol Reprod Biol. 2009;144:40–43. doi: 10.1016/j.ejogrb.2008.12.016. [DOI] [PubMed] [Google Scholar]
- 26.Mucci LA, Lagiou P, Hsieh CC, et al. A prospective study of pregravid oral contraceptive use in relation to fetal growth. BJOG. 2004;111:989–995. doi: 10.1111/j.1471-0528.2004.00232.x. [DOI] [PubMed] [Google Scholar]
- 27.Pelkonen S, Koivunen R, Gissler M, Nuojua-Huttunen S, et al. Perinatal outcome of children born after frozen and fresh embryo transfer: the Finnish cohort study 1995-2006. Hum Reprod. 2010;25:914–923. doi: 10.1093/humrep/dep477. [DOI] [PubMed] [Google Scholar]
- 28.Marino JL, Moore VM, Willson KJ, et al. Perinatal outcomes by mode of assisted conception and sub-fertility in an Australian data linkage cohort. PLoS One. 2014;9:e80398. doi: 10.1371/journal.pone.0080398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Jacobsen EA, Helmers RA, Lee JJ, Lee NA. The expanding role(s) of eosinophils in health and disease. Blood. 2012;120:3882–3890. doi: 10.1182/blood-2012-06-330845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Temmerman M, Gichangi P, Fonck K, et al. Effect of a syphilis control programme on pregnancy outcome in Nairobi, Kenya. Sex Trans Infect. 2000;76:117–121. doi: 10.1136/sti.76.2.117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Costa MC, Bornhausen Demarch E, Azulay DR, Perisse AR, Dias MF, Nery JA. Sexually transmitted diseases during pregnancy: a synthesis of particularities. An Bras Dermatol. 2010;85:767–782. doi: 10.1590/S0365-05962010000600002. [DOI] [PubMed] [Google Scholar]
- 32.Qin JB, Feng TJ, Yang TB, Hong FC, Lan LN, Zhang CL. Maternal and paternal factors associated with congenital syphilis in Shenzhen, China: a prospective cohort study. Eur J Clin Microbiol Infect Dis. 2014;33:221–232. doi: 10.1007/s10096-013-1948-z. [DOI] [PubMed] [Google Scholar]
- 33.Gomez GB, Kamb ML, Newman LM, Mark J, Broutet N, Hawkes SJ. Untreated maternal syphilis and adverse outcomes of pregnancy: a systematic review and meta-analysis. Bull World Health Organ. 2013;91:217–226. doi: 10.2471/BLT.12.107623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Sinclair KD, Watkins AJ. Parental diet, pregnancy outcomes and offspring health: metabolic determinants in developing oocytes and embryos. Reprod Fertil Dev. 2013;26:99–114. doi: 10.1071/RD13290. [DOI] [PubMed] [Google Scholar]
- 35.Otero-Ferrer F, Izquierdo M, Fazeli A, Holt WV. Sex-specific effects of parental diet during pregnancy on embryo development in the long snout seahorse. Reprod Fertil Dev. 2014;27:153. doi: 10.1071/RDv27n1Ab122. [DOI] [Google Scholar]
- 36.Martin GB, Blache D, Miller DW, Vercoe PE. Interactions between nutrition and reproduction in the management of the mature male ruminant. Animal. 2010;4:1214–1226. doi: 10.1017/S1751731109991674. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets during the current study are available from the corresponding author on reasonable request.


