The definition of the subscapular bursa (SSB) remains controversial. One researcher demonstrated that SSB was a separate pouch.[1] However, others believed that SSB was actually the superior subscapularis recess (SSR), which is an outpouching of the glenohumeral joint capsule.[2,3,4] Whether or not the SSB and SSR are two different bursae must be confirmed. Furthermore, the fluid in the SSR revealed in magnetic resonance (MR) imaging has been regarded as an indication for a diagnosis of frozen shoulder.[3] Considering that the SSB and SSR are two different structures with a close spatial relationship, recognition of the MR appearance of SSB might have important diagnostic implications. The purposes of this study were to describe the anatomy of the SSB using a three-dimensional (3D) visualization technique based on the Chinese visible human (CVH) and to explore the MR appearance of the SSB.
Sections of eight shoulders were retrieved from four CVH datasets (three females, one male; mean age 26.8 years), and the anatomy of the SSB in each shoulder was observed in the axial view (AV), sagittal oblique view (SOV), and coronal oblique view (COV). Each SSB and its adjacent structures in the SOV sections were then segmented and reconstructed in three dimensions using Amira software version 5.2.2 (TGS, California, USA).
Seven embalmed cadaveric shoulders without visible lesions (five right and two left) were used for this study. Before dissecting them, MR imaging was performed using a 3.0-T system (Spectra; Siemens Medical Solutions, Germany). T2- and T1-weighted tuber spin-echo (TSE) images were obtained in the AV, SOV, and COV planes. After the MR images had been obtained, the cadaveric shoulders were dissected to expose the SSB. Next, a contrast agent was injected into each SSB, and MR imaging was completed using the same MR system. Finally, T1-weighted TSE images were obtained again.
In all eight of the CVH shoulders, the SSB was a flat and irregularly shaped entity located between subscapularis (SSC) and scapula. No connection was found between SSB and glenohumeral articular cavity (GHAC) [Figure 1a and 1b]. In SOV images, the lateral portion of SSB was an irregularly shaped structure; the medial portion of SSB was a saddlebag-shaped entity in close contact with the inferior side of the coracoid process [Figure 1c]; gradually, it presented as a narrow strip between scapula and SSC. In AV and COV images, the SSB presented as an irregular or narrow strip-shaped structure, and the spectrum could be identified between bursa and GHAC [Figure 1e and 1g]. No other bursae were identified between SSC and scapula.
Figure 1.
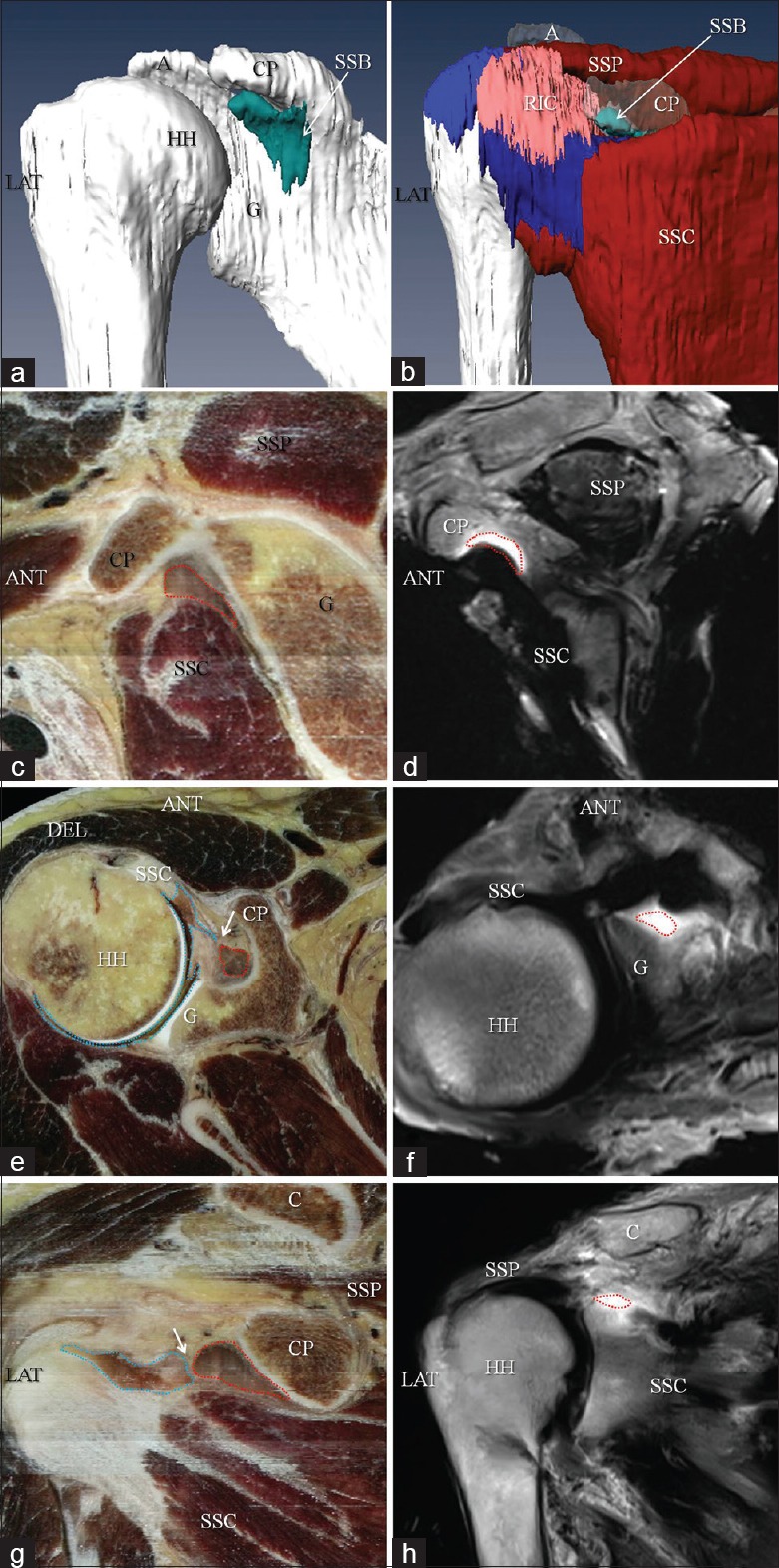
Three-dimensional shape and topographical location of the SSB: Sectional anatomy of SSB and its adjacent structures in the CVH sections and MR images. (a, b) The three-dimensional shape of SSB, the spatial relationship between SSB and its adjacent structures. The SSB are shown in the sagittal oblique CVH (c) and MR images (d); the axial CVH (e) and MR images (f); the coronal oblique CVH (g) and MR images (h). Arrow in e and g: Spectrum separating the SSB and GHAC (in the area marked by blue dashed line) is shown. Area marked by red dashed line: SSB; A: Acromion; ANT: Anterior side; C; Clavicle; CP: Coracoid process; G: Glenoid; GHAC: Anterior part of the glenohumeral articular cavity; HH: Humeral head; LAT: Lateral side; RIC: Rotator interval capsule; SSB: Subscapular bursa; SSC: Subscapularis; SSP: Supraspinatus; SUP: Superior side; MR: Magnetic resonance; CVH: Chinese visible human.
SSB was not identified in the MR images obtained before the dissection. After the SSB had been exposed and filled with contrast agent, the SSB was evident on MR images, and no hyperintensity was observed in GHAC [Figure 1f and 1h]. In SOV MR images, SSB typically appeared as a saddlebag-shaped hyperintense area between the inferior surface of the coracoid process and the superior margin of the SSC [Figure 1d]. In AV and COV MR images, the SSB presented as a narrow strip or an irregular area with high signal intensity [Figure 1d and 1f]. SOV and AV MR images optimized the visualization of SSB; however, it still was not easy to identify SSB on the COV sequences.
SSB was identified as a separate and unique bursa between SSC and scapula in all specimens of this study, which is in line with the results of Colas et al.,[1] who demonstrated that a thin wall was constantly present between GHAC and SSB. However, they only included a textual description of the spatial relationship between the two entities. We illustrated this intimate spatial relationship using a 3D visualization technique based on the CVH sections. Furthermore, CVH sections preferably showed the subtle sectional anatomy of SSB. In addition, the thin spectrum between SSB and GHAC could be easily identified in AV and COV planes in the CVH sections. In terms of its pathologic or functional condition, communication may easily occur through the thin spectrum between SSB and GHAC.[1] Under these circumstances, it would be logical to suppose that the SSB is an outpouching portion of the glenohumeral joint and could be regarded as the SSR.
This study demonstrated that the SSB was visible as a saddlebag-shaped hyperintense area in MR images that was similar to the reported MR appearance of the SSR.[3] SOV MR images optimized the visualization of the SSB, which can also be viewed in the AV images. However, because the slice thickness of the MR images was 3 mm, and SSB is a flat bursa roughly parallel to the COV plane, it was difficult to visualize in the coronal sequences unless it was filled with a large amount of fluid. Based on the sectional anatomy and MR appearance of SSB, the rational appropriate way of confirming SSB effusion is to identify its saddlebag appearance over the SSC using SOV MR images and then to verify that the liquid within SSB is not connected to the fluid in the joint using AV and COV MR images.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
This study was supported by grants from the National Key Research and Development program of China (No. 2016YFC1100503) and Military Youth Science Foundation of China (No. 16QNP100).
Conflicts of interest
There are no conflicts of interest.
Footnotes
Edited by: Ning-Ning Wang
REFERENCES
- 1.Colas F, Nevoux J, Gagey O. The subscapular and subcoracoid bursae: Descriptive and functional anatomy. J Shoulder Elbow Surg. 2004;13:454–8. doi: 10.1016/j.jse.2004.02.001. doi: 10.1016/S1058274604000473. [DOI] [PubMed] [Google Scholar]
- 2.Horowitz MT, Tocantins LM. An anatomical study of the role of the long thoracic nerve and the related scapular bursae in the pathogenesis of local paralysis of the serratus anterior muscle. Anat Rec. 1938;71:375–85. doi: 10.1002/ar.1090710402. [Google Scholar]
- 3.Carbone S, Napoli A, Gumina S. MRI of adhesive capsulitis of the shoulder: Distension of the bursa in the superior subscapularis recess is a suggestive sign of the pathology. Eur J Radiol. 2014;83:345–8. doi: 10.1016/j.ejrad.2013.10.017. doi: 10.1016/j.ejrad.2013.10.017. [DOI] [PubMed] [Google Scholar]
- 4.Petersilge CA, Witte DH, Sewell BO, Bosch E, Resnick D. Normal regional anatomy of the shoulder. Magn Reson imaging Clin N Am. 1993;1:8–9. [PubMed] [Google Scholar]


