Abstract
Background and Aims:
It has been reported that clonidine when used as an additive in a dose of 90 μg in adults increases the duration of peripheral nerve blocks. Hence, this study was conducted to evaluate the effect of clonidine in brachial plexus blocks and to compare it with tramadol.
Material and Methods:
Ninety patients posted for upper limb orthopedic surgery were divided randomly into three groups. 40 mL of local anesthetic solution was prepared using 15 mL of 2% lignocaine-adrenaline-sodium bicarbonate solution, 15 mL of 0.5% bupivacaine, and 10 mL distilled water. Patients received a supraclavicular brachial plexus block with 0.7 mL/kg of this solution to which either 1 mg/kg tramadol, 1 μg/kg clonidine, or 1.5 μg/kg clonidine was added. The onset and duration of sensory and motor block and the duration of postoperative analgesia were recorded. Pulse rate, blood pressure, respiratory rate, saturation, sedation, and any side effect were monitored. Results were statistically analyzed using analysis of variance F-test and unpaired t-test.
Results:
There was a statistically significant difference in the onset of both the sensory and motor components of the block with the fastest onset seen when clonidine was used in a dose of 1.5 μg/kg. The block also lasted statistically significantly longer with clonidine as compared with tramadol although there was no statistically significant increase in the duration of the block when a higher dose of clonidine was used. The time for rescue analgesia was the longest in patients who received 1.5 μg/kg of clonidine (491.8 ± 33.9 min). This duration was also statistically significant. Patients who received tramadol reported a statistically significant higher incidence of nausea.
Conclusion:
Clonidine in a dose of 1.5 μg/kg body weight provided the fastest onset of sensory as well as motor block and the longest duration of postoperative analgesia and thus is a good additive to local anesthetic solutions for brachial plexus blocks.
Keywords: Brachial plexus block, bupivacaine, clonidine, lignocaine, tramadol
Introduction
The supraclavicular approach to a brachial plexus block provides optimal anesthesia for forearm surgeries. Clonidine is an alpha-2 receptor agonist that provides analgesia by acting at central and peripheral receptors. Clonidine causes dose-dependent bradycardia, hypotension, and sedation.[1,2,3] Its use in neuraxial blocks is well-studied.[4,5] Various studies have reported that clonidine when used as an additive in a dose of 90 μg in adults or approximately 1.5 μg/kg increases the duration of peripheral nerve blocks.[6,7,8,9,10]
Pöpping et al. reported in their meta-analysis of randomized trials that[6] addition of clonidine to regional nerve blocks increases the duration of the block and provides faster onset. This was further supported by McCartney et al.[7] It has been reported that the duration of peripheral nerve blocks increased when clonidine was used in a dose of 1 μg/kg though a dose-responsiveness has not yet been determined.[6,11,12,13] Tramadol as an adjuvant to local anesthetic solutions also enhances a peripheral nerve block[14,15,16] and is commonly used in our institute. Hence, this randomized clinical trial was conducted to compare the onset and duration of a supraclavicular brachial plexus block when tramadol and clonidine in a dose of 1 and 1.5 μg/kg were added as adjuvants to local anesthetic solution.
Material and Methods
This was a double-blind randomized study conducted over a period of 1 year from August 2011 to August 2012 in a tertiary center. Institutional Ethical Committee approval was taken before conducting the trial. Following ethical committee approval, ninety patients posted for routine or emergency orthopedic forearm and hand surgeries lasting for about 90 min were included in this study. All surgeries were performed under a tourniquet. The patients who belonged to the American Society of Anesthesiologists physical status I or II and were between 18 and 50 years of age were selected for this study. Patients who did not meet the above criteria or patients who had hypersensitivity/allergy to any drug used in the study or those who were on analgesics before the study were excluded from the study. Patients with cardiovascular or respiratory diseases and patients suffering from renal or hepatic derangements or diseases of central nervous system or bleeding disorders were excluded from the study. Each patient was given all information and details about the anesthetic procedure and the drugs used and were freely allowed to clarify any doubt or question they had. A written informed consent in the local language was taken from all the patients. Patients taking part in the study underwent a thorough preoperative assessment including detailed case history, physical examination, and baseline investigations such as hemoglobin, bleeding time, and clotting time.
The patients were randomly assigned to three different groups of thirty each by a computer-generated randomized sheet. Concealment was done using sealed envelopes. No premedication was administered. A stock solution with a volume of 40 mL of local anesthetic solution was prepared as follows:
15 mL of 2% lignocaine adrenaline sodium bicarbonate solution (with adrenaline in a concentration of 5 μg/mL of lignocaine solution and 1.25 mL of 7.5% of sodium bicarbonate per 15 mL of the lignocaine solution); 15 mL of 0.5% bupivacaine; 10 mL distilled water.
Patients received 0.7 mL/kg of the above solution for the supraclavicular block.
Adjuvants were added to the final volume of the local anesthetic to be administered depending on the group;
Group A: These patients received 1 mg/kg tramadol as adjuvant;
Group B: These patients received 1 μg/kg clonidine as adjuvant;
Group C: These patients received 1.5 μg/kg clonidine as adjuvant;
All drug solutions were prepared by an anesthesiologist not involved in the administration of anesthesia, patient care, and data collection.
The patients were administered a brachial plexus block under all aseptic precautions using a nerve locator. The patient was made to lie supine with a pillow below the shoulders with the head turned to opposite side. The arm to be blocked was kept along the side of the body. After sterile preparation of the site, the following landmarks were palpated:
The midpoint of the clavicle
The pulsations of the subclavian artery 1–2 cm above the midpoint and just lateral to outer border of scalenus anterior muscle.
The preprocedural pulse rate, blood pressure, respiratory rate, saturation, and sedation were recorded. Using a nerve locator, an insulated 22-gauge injection needle was introduced just lateral to the pulsating subclavian artery in a downward and posterior direction till motor response of the forearm with flexion of the first, second, third, and fourth fingers was elicited. The drug was injected when motor response was elicited at a current of 0.4 mA. The needle was removed and gentle massage was given manually over the site of injection for 5 min to ensure uniform spread of the drug.[17] Sensory blockade was assessed by sterile pinprick along the sensory distribution of median, radial, and the ulnar nerves every 30 s till the onset of the block and the every 30 min till its offset. The onset of sensory block was defined as the time between administering the drug and the time there was no sensation to a pinprick in the distribution of all three nerves.[18] Motor blockade was evaluated by Bromage scale[9] (0 = normal motor function with full flexion and extension of elbow, wrist, and fingers; 1 = decreased motor function with ability to move the fingers only; 2 = compete motor block with inability to move the fingers) every 1 min till the onset followed by 30 min till its offset. The onset of motor block was defined as the time between administering the drug to the time the Bromage scale was 2. Surgery was started after the onset of both sensory and motor components of the block.
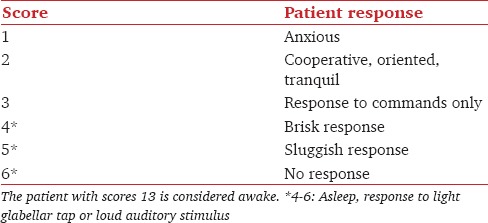
Patients were not given any sedation during the study period. Pulse rate, blood pressure, respiratory rate, saturation, and sedation (evaluated according to The Ramsay sedation scale[19] [Table 1]) were recorded every 15 min for the first hour followed by every 30 min for the next 3 h. Hypotension and bradycardia were defined as a fall in blood pressure and heart rate, respectively, by more than 20% from the preoperative values. In addition, the incidence of nausea, vomiting, and respiratory depression was recorded. Respiratory depression was defined as a decrease in respiratory rate below 10 or a fall in saturation to ≤90%.[20] The time for rescue analgesia, that is, the period from the administration of the block till the time the patient complained of pain was recorded postoperatively in each patient. Injection diclofenac sodium (1.5 mg/kg) was then administered intramuscularly as rescue analgesic.
Table 1.
Ramsay sedation scale
Statistical analysis
Duration of postoperative analgesia was used as the outcome measure to calculate the sample size. The mean and standard deviation of the outcome variable were 450.8 and 40.5 based on a pilot study. It was calculated that with 30 patients in each group, the power of the study is 80% at 0.05 significance level if the difference in the outcome measure between treatments is 30.0 min. The detailed data were entered into the Microsoft Excel sheet. Statistics were represented in terms of mean ± standard division. A null hypothesis was set up stating that there was no difference when different adjuvants were used. Chi-square testing was used for nonquantitative data. Quantitative data were analyzed using analysis of variance (ANOVA)-F test. In case the ANOVA F-test results were significant, the unpaired t-test was used to compare two groups at a time. A P < 0.05 was considered statistically significant and the null hypothesis was then rejected.
Results
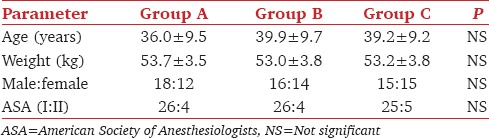
All three groups were demographically comparable [Table 2]. The hemodynamic parameters of patients of all three groups preoperatively were comparable (P = 0.87 and 0.89 for pulse rate and BP, respectively).
Table 2.
Demographics
The time for rescue analgesia was [Figure 1] 313.3 ± 21.4 min in Group A, 470.7 ± 38.6 min in Group B, 491.8 ± 33.9 min in Group C with a P < 0.001. The duration of rescue analgesia was statistically significant between Groups A and B (P < 0.001), Groups A and C (P < 0.001) as well as between Groups B and C (P = 0.028) [Tables 3 and 4].
Figure 1.
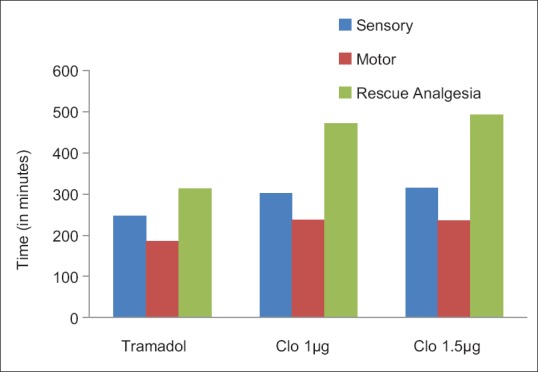
Duration of the block
Table 3.
Onset and duration of the block
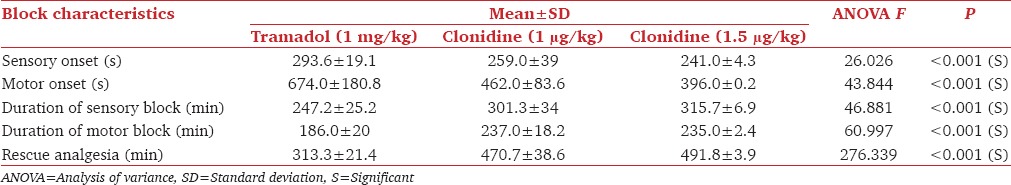
Table 4.
Onset and duration of the block (t-test values with P values)
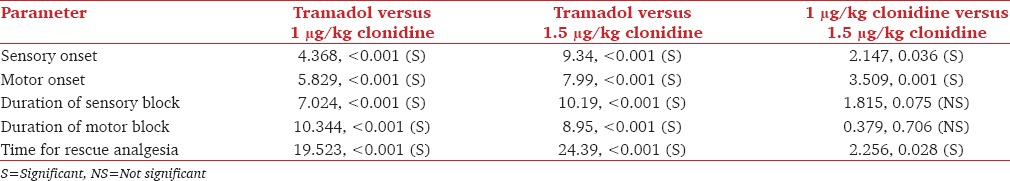
The onset of sensory block was the fastest in Group C as shown in Figure 2. This difference in the onset time was statistically significant between Group A and Group B as well as Group A and Group C. Clonidine also had a statistically significant faster onset of action when used in a dose of 1.5 μg/kg as compared with when used in a dose of 1 μg/kg dose (P = 0.036) [Tables 3 and 4]. Patients who received 1.5 μg/kg clonidine had the shortest time for the onset of motor blockade, i.e. 396.0 ± 60.2 s with a P < 0.01. Figure 1 shows the mean duration of sensory blockade. The difference in the onset time was statistically significant between Group A and Group B, Group A and Group C. However, the difference in the duration was not statistically significant between the two clonidine groups [Tables 3 and 4].
Figure 2.
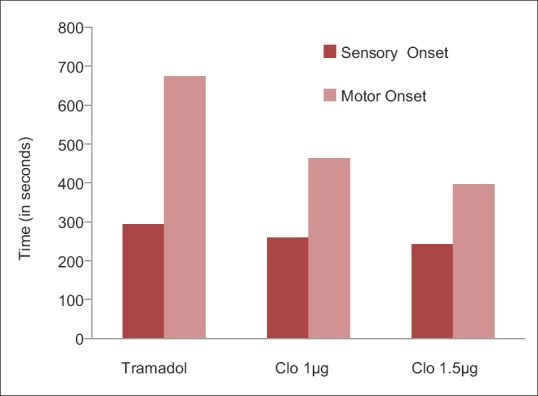
Onset of the block
The mean duration of motor blockade is shown in Figure 1. The duration was longest in Group C. As seen with the duration of sensory blockade, both the clonidine groups had a statistically significant longer duration of motor blockade when compared with tramadol. The difference in the duration of motor blockade was not statistically significant between the two clonidine groups [Tables 3 and 4]. No patient in any group had any hemodynamic instability throughout the study period. There was also no statistically significant change in pulse rate or blood pressure in any patient throughout [Figure 3]. There was no respiratory depression or a clinically significant decrease in saturation seen in any patient in the three groups. Even the larger dose of clonidine did not produce any sedation. A total of 5 patients out of 30 who received tramadol complained of nausea.
Figure 3.
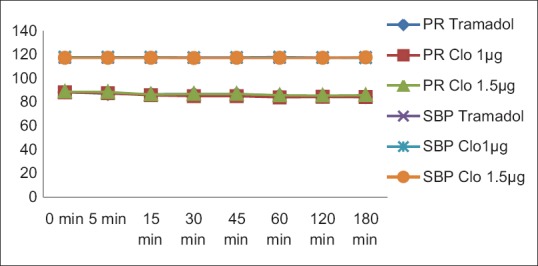
Hemodynamic stability
Discussion
This study was conducted to compare the peripheral nerve block enhancing properties of tramadol and two different doses of clonidine. The time for rescue analgesia was the longest (statistically significant) in patients who received 1.5 μg/kg of clonidine. The increase was by an average of 3 h when compared with tramadol and 21 min when compared with 1 μg/kg clonidine. This dose thus provided the maximum postoperative analgesia out of three doses. A similar result was arrived at by Singelyn et al. in 1996.[12] A meta-analysis of the randomized trials on clonidine in peripheral nerve blocks concluded that addition of clonidine considerably prolonged postoperative analgesia.[6,7] The results of this study are in accordance with the present study. In the present study, a statistically significant earlier onset of sensory and motor block was observed when clonidine was added in a dose of 1.5 μg/kg.
A meta-analysis on previous studies conducted by Pöpping et al.[6] in 2009 on clonidine reported a decrease in onset time of about 2 min with 90 μg of clonidine as compared with controls who did not receive adjuvants. The onset of sensory and motor block in these studies was about 12 and 17 min, respectively. The difference in onset time from our study could be due to the fact that other studies used bupivacaine, ropivacaine, or mepivacaine as local anesthetics. In the present study, a combination of lignocaine-bupivacaine was used. The faster onset of action of lignocaine may be one factor responsible for this difference in onset time. Furthermore, most of the studies included in the meta-analyses used the axillary approach while we used a supraclavicular approach in the present study. Tramadol has been shown to increase the duration of peripheral nerve blocks though the time to onset of the block was not decreased.[14,15,16] In the present study when compared with tramadol, clonidine in either of the two doses resulted in a greater prolongation in the duration of sensory and motor blocks. Clonidine in a dose of 1.5 μg/kg resulted in an average duration of 315.7 ± 26.9 min of sensory block. This is in accordance with other studies and meta-analysis, where 90 μg of clonidine provided an average duration of sensory block of 343 min.
In previous studies, depending on the local anesthetic used the increase in motor blockade ranged from 1.5 to 4 h with the maximum increase seen with bupivacaine.[6,7] A total of 150 μg clonidine were also found to increase the duration of axillary plexus block by Duma et al.[21] In 2005, Iohom et al.[22] found that clonidine added to mepivacaine for axillary brachial plexus block enhances both anesthesia and postoperative analgesia. Interestingly, there are studies which conclude the effect of Clonidine varies depending upon the local anaesthetic used with no effect seen with ropivacaine[23,24]
As far as dose-responsiveness is concerned, in consonance with other studies,[6,11,12,13] the difference in the duration of the block was not statistically significant thus failing to demonstrate a dose-responsiveness.
All patients were hemodynamically stable throughout the study period. No incidence of sedation or respiratory depression was observed in the present study. This is in accordance with most studies state that the ill effects of hypotension, bradycardia, and sedation are limited up to a dose of 150 μg.[6,7]
However, this study was a single-blinded study, so observer bias could have possibly affected the results. The pain was not quantified using a visual analog scale (VAS) score. Any time the patient complained of pain, the rescue analgesic was administered. Ultrasonography assistance was not used for block administration in this study. The use of USG-guided blocks may further validate the result.
Conclusion
From the present study, it can be inferred that when compared with tramadol, the addition of clonidine to a local anesthetic mixture produced a faster onset and prolonged duration of both of the sensory and motor components of a brachial plexus block with fastest onset seen with a dose of 1.5 μg/kg of clonidine. However, there was no significant increase in the duration of the block when a higher dose of clonidine was used. In addition, in a dose of 1.5 μg/kg body weight clonidine provided maximum postoperative analgesia. Patients were hemodynamically stable when 1 or 1.5 μg/kg of clonidine was used. No major side effects were seen. Patients who received clonidine reported a lower incidence of nausea than the patients who received tramadol.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Gaumann DM, Brunet PC, Jirounek P. Clonidine enhances the effects of lidocaine on C-fiber action potential. Anesth Analg. 1992;74:719–25. doi: 10.1213/00000539-199205000-00017. [DOI] [PubMed] [Google Scholar]
- 2.Gaumann DM, Brunet PC, Jirounek P. Hyperpolarizing afterpotentials in C fibers and local anesthetic effects of clonidine and lidocaine. Pharmacology. 1994;48:21–9. doi: 10.1159/000139158. [DOI] [PubMed] [Google Scholar]
- 3.Butterworth JF, 5th, Strichartz GR. The alpha 2-adrenergic agonists clonidine and guanfacine produce tonic and phasic block of conduction in rat sciatic nerve fibers. Anesth Analg. 1993;76:295–301. [PubMed] [Google Scholar]
- 4.Niemi L. Effects of intrathecal clonidine on duration of bupivacaine spinal anaesthesia, haemodynamics, and postoperative analgesia in patients undergoing knee arthroscopy. Acta Anaesthesiol Scand. 1994;38:724–8. doi: 10.1111/j.1399-6576.1994.tb03985.x. [DOI] [PubMed] [Google Scholar]
- 5.Filos KS, Goudas LC, Patroni O, Polyzou V. Hemodynamic and analgesic profile after intrathecal clonidine in humans. A dose-response study. Anesthesiology. 1994;81:591–601. doi: 10.1097/00000542-199409000-00011. [DOI] [PubMed] [Google Scholar]
- 6.Pöpping DM, Elia N, Marret E, Wenk M, Tramèr MR. Clonidine as an adjuvant to local anesthetics for peripheral nerve and plexus blocks: A meta-analysis of randomized trials. Anesthesiology. 2009;111:406–15. doi: 10.1097/ALN.0b013e3181aae897. [DOI] [PubMed] [Google Scholar]
- 7.McCartney CJ, Duggan E, Apatu E. Should we add clonidine to local anesthetic for peripheral nerve blockade? A qualitative systematic review of the literature. Reg Anesth Pain Med. 2007;32:330–8. doi: 10.1016/j.rapm.2007.02.010. [DOI] [PubMed] [Google Scholar]
- 8.Murphy DB, McCartney CJ, Chan VW. Novel analgesic adjuncts for brachial plexus block: A systematic review. Anesth Analg. 2000;90:1122–8. doi: 10.1097/00000539-200005000-00023. [DOI] [PubMed] [Google Scholar]
- 9.Adnan T, Elif AA, Ayse K, Gülnaz A. Clonidine as an adjuvant for lidocaine in axillary brachial plexus block in patients with chronic renal failure. Acta Anaesthesiol Scand. 2005;49:563–8. doi: 10.1111/j.1399-6576.2005.00631.x. [DOI] [PubMed] [Google Scholar]
- 10.Hutschala D, Mascher H, Schmetterer L, Klimscha W, Fleck T, Eichler HG, et al. Clonidine added to bupivacaine enhances and prolongs analgesia after brachial plexus block via a local mechanism in healthy volunteers. Eur J Anaesthesiol. 2004;21:198–204. doi: 10.1017/s0265021504003060. [DOI] [PubMed] [Google Scholar]
- 11.Bernard JM, Macaire P. Dose-range effects of clonidine added to lidocaine for brachial plexus block. Anesthesiology. 1997;87:277–84. doi: 10.1097/00000542-199708000-00014. [DOI] [PubMed] [Google Scholar]
- 12.Singelyn FJ, Gouverneur JM, Robert A. A minimum dose of clonidine added to mepivacaine prolongs the duration of anesthesia and analgesia after axillary brachial plexus block. Anesth Analg. 1996;83:1046–50. doi: 10.1097/00000539-199611000-00025. [DOI] [PubMed] [Google Scholar]
- 13.Singelyn FJ, Dangoisse M, Bartholomée S, Gouverneur JM. Adding clonidine to mepivacaine prolongs the duration of anesthesia and analgesia after axillary brachial plexus block. Reg Anesth. 1992;17:148–50. [PubMed] [Google Scholar]
- 14.Kapral S, Gollmann G, Waltl B, Likar R, Sladen RN, Weinstabl C, et al. Tramadol added to mepivacaine prolongs the duration of an axillary brachial plexus blockade. Anesth Analg. 1999;88:853–6. doi: 10.1097/00000539-199904000-00032. [DOI] [PubMed] [Google Scholar]
- 15.Robaux S, Blunt C, Viel E, Cuvillon P, Nouguier P, Dautel G, et al. Tramadol added to 1.5% mepivacaine for axillary brachial plexus block improves postoperative analgesia dose-dependently. Anesth Analg. 2004;98:1172–7. doi: 10.1213/01.ANE.0000108966.84797.72. [DOI] [PubMed] [Google Scholar]
- 16.Kaabachi O, Ouezini R, Koubaa W, Ghrab B, Zargouni A, Ben Abdelaziz A. Tramadol as an adjuvant to lidocaine for axillary brachial plexus block. Anesth Analg. 2009;108:367–70. doi: 10.1213/ane.0b013e31818e0c6b. [DOI] [PubMed] [Google Scholar]
- 17.Kothari D. Supraclavicular brachial plexus block: A new approach. Indian J Anaesth. 2003;47:287–8. [Google Scholar]
- 18.Lanz E, Theiss D, Jankovic D. The extent of blockade following various techniques of brachial plexus block. Anesth Analg. 1983;62:55–8. [PubMed] [Google Scholar]
- 19.Ramsay MA, Savege TM, Simpson BR, Goodwin R. Controlled sedation with alphaxalone-alphadolone. Br Med J. 1974;2:656–9. doi: 10.1136/bmj.2.5920.656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.American Society of Anesthesiologists Task Force on Neuraxial Opioids. Horlocker TT, Burton AW, Connis RT, Hughes SC, Nickinovich DG, et al. Practice guidelines for the prevention, detection, and management of respiratory depression associated with neuraxial opioid administration. Anesthesiology. 2009;110:218–30. doi: 10.1097/ALN.0b013e31818ec946. [DOI] [PubMed] [Google Scholar]
- 21.Duma A, Urbanek B, Sitzwohl C, Kreiger A, Zimpfer M, Kapral S. Clonidine as an adjuvant to local anaesthetic axillary brachial plexus block: A randomized, controlled study. Br J Anaesth. 2005;94:112–6. doi: 10.1093/bja/aei009. [DOI] [PubMed] [Google Scholar]
- 22.Iohom G, Machmachi A, Diarra DP, Khatouf M, Boileau S, Dap F, et al. The effects of clonidine added to mepivacaine for paronychia surgery under axillary brachial plexus block. Anesth Analg. 2005;100:1179–83. doi: 10.1213/01.ANE.0000145239.17477.FC. [DOI] [PubMed] [Google Scholar]
- 23.Erlacher W, Schuschnig C, Koinig H, Marhofer P, Melischek M, Mayer N, et al. Clonidine as adjuvant for mepivacaine, ropivacaine and bupivacaine in axillary, perivascular brachial plexus block. Can J Anaesth. 2001;48:522–5. doi: 10.1007/BF03016825. [DOI] [PubMed] [Google Scholar]
- 24.Erlacher W, Schuschnig C, Orlicek F, Marhofer P, Koinig H, Kapral S. The effects of clonidine on ropivacaine 0.75% in axillary perivascular brachial plexus block. Acta Anaesthesiol Scand. 2000;44:53–7. doi: 10.1034/j.1399-6576.2000.440110.x. [DOI] [PubMed] [Google Scholar]


