Abstract
Acute pulmonary inflammation is characterized by migration of polymorphonuclear neutrophils into the different compartments of the lung. Recent studies showed evidence that the chemokine stromal cell-derived factor (SDF)-1 and its receptors CXCR4 and CXCR7 influence migration of immune cells and their activity was linked to adenosine concentrations. We investigated the particular role of CXCR4- and CXCR7-inhibition and the potential link to the adenosine A2B-receptor, which plays an important anti-inflammatory role in the lung. After LPS-inhalation for 45 minutes, administration of the CXCR4-inhibitor (AMD3100) decreased transendothelial and transepithelial migration, whereas CXCR7-antagonism influenced epithelial migration exclusively. In A2B−/− mice, no anti-inflammatory effects were detectible through either one of the agents. Using chimeric mice, we identified A2B on hematopoietic cells to be crucial for these anti-inflammatory effects of CXCR4/7-inhibition. Both inhibitors decreased TNFα, IL6, CXCL1 and CXCL2/3 levels in the bronchoalveolar lavage of wild type mice, while not influencing the chemokine release in A2B−/− mice. Inflammation augmented the expression of both receptors and their inhibition increased A2B-levels upon inflammation. In vitro assays with human epithelium/endothelium confirmed our in vivo findings. During inflammation, inhibition of CXCR4- and CXCR7-receptors prevented microvascular permeability in wild type but not in A2B−/− mice, highlighting the pivotal role of an active A2B-receptor in this setting. The combination of both inhibitors had a synergistic effect in preventing capillary leakage. In conclusion, we determined the pivotal role of CXCR4- and CXCR7-inhibition in acute pulmonary inflammation, which depended on A2B-receptor signalling.
Acute pulmonary inflammation and its more severe form acute respiratory distress syndrome still have a high mortality around 40%1 and the surviving patients commonly have residual physical limitations and a poor quality of life.2
The innate inflammatory response to pathogens includes the release of chemotactic factors to recruit polymorphonuclear neutrophils (PMNs). Although PMNs are necessary for defense, their excessive migration into inflamed tissue even aggravates tissue damage.3 Thereby, PMNs migrate from the circulation into the lung interstitium passing an endothelial barrier followed by an epithelial barrier into the alveolar space.
Stromal cell-derived factor (SDF)-1 is a chemokine that mediates hematopoietic stem cell mobilization and migration of leukocytes.4, 5 SDF-1 is naturally highly expressed in the bone marrow and acts as a retention factor for neutrophils. During inflammation, the concentration of SDF-1 in the bone marrow decreases and PMNs enter the circulation from where they can migrate to the site of inflammation.6
SDF-1 (CXCL12 in the systematic nomenclature) has two receptors: CXCR4 and CXCR7.7 These receptors seem to play a role in lung emphysema and chronic obstructive pulmonary disease.8
The nucleoside adenosine emerges from the enzymatic degradation of adenosine triphosphate. Four different adenosine receptors exist, whereby the A2B-receptor plays a predominant role in terms of pulmonary inflammation.9, 10 A connection between the A2B-receptor and CXCR4-expression was also found in terms of protection against vascular injury.11
Therefore, we investigated the role of the SDF-1 receptors CXCR4 and CXCR7 concerning the two hallmarks of acute pulmonary inflammation: PMN migration and microvascular permeability. Additionally, we hypothesized that inhibiting CXCR4 and CXCR7 has anti-inflammatory effects and that these effects depend on A2B-receptor signalling.
Results
SDF-1 levels in our model
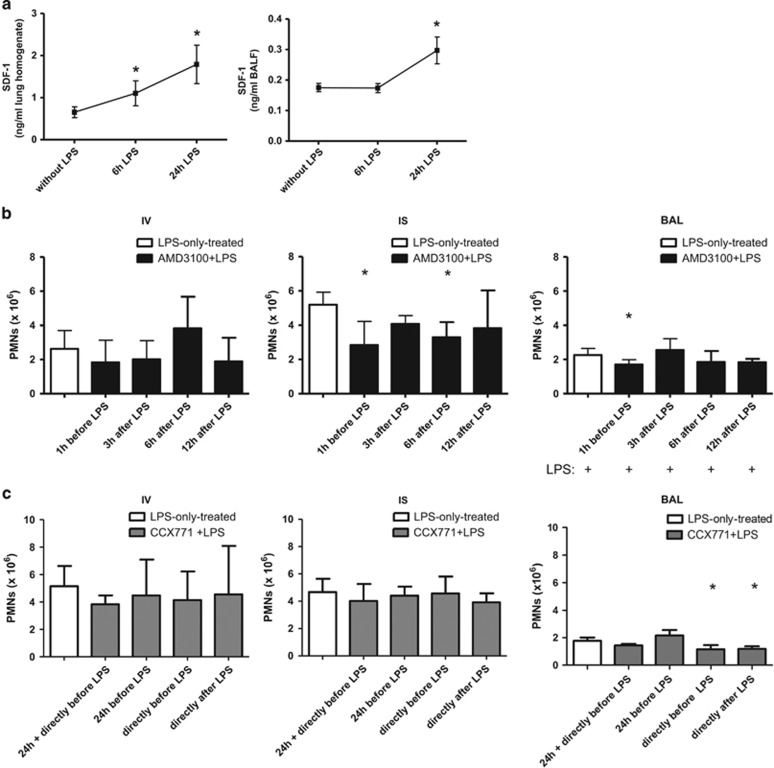
We determined the impact of our model on SDF-1 levels in the lungs of mice and bronchoalveolar lavage (BAL) (Figure 1a). LPS-inhalation significantly increased SDF-1 in the lungs of mice 6 and 24 h after LPS. In the BAL, the significant rise of the chemokine was detectable 24 h after the inflammatory hit.
Figure 1.
Effect of our model on SDF-1 levels in the lungs of mice (a). Mice inhaled LPS and SDF-1 levels were determined in the lungs (n=8) and BAL (n=4). Data are presented as mean ±S.D.; *P<0.05 versus without LPS. Time optimum for the administration of the CXCR4- (b) and CXCR7-antagonist (c). The inhibitors were given at indicated time points and, 24 h after LPS-inhalation, migration of PMNs into the different compartments of the lung (IV=intravascular; IS=interstitial; BAL=bronchoalveolar lavage) was evaluated. Data are presented as mean ±S.D.; n≥4; *P<0.05 versus LPS-only treated
Time-dependent administration of the CXCR4- and CXCR7-antagonist
Based on previously published data, AMD3100 was administered to the animals at different time points12, 13 and all animals inhaled LPS (Figure 1b). There were no differences in PMN counts in the intravascular compartment. In the interstitium of the lung, CXCR4-antagonism was effective in curbing down PMN migration 1 h before LPS and 6 h after the inflammation. One hour before LPS, AMD3100 decreased PMN migration into the alveolar space. Hence, we chose 1 h before LPS as time point for the administration of AMD3100 in all subsequent experiments.
We chose different time points for the administration of CCX771.13, 14 CXCR7-antagonism neither influenced PMN counts intravascular nor interstitial, but reduced migrated PMNs into the alveolar space when injected shortly before or directly after LPS (Figure 1c). Therefore, CCX771 was administered directly after LPS in all following experiments.
The effect of CXCR4- and CXCR7-antagonism in immunohistochemistry
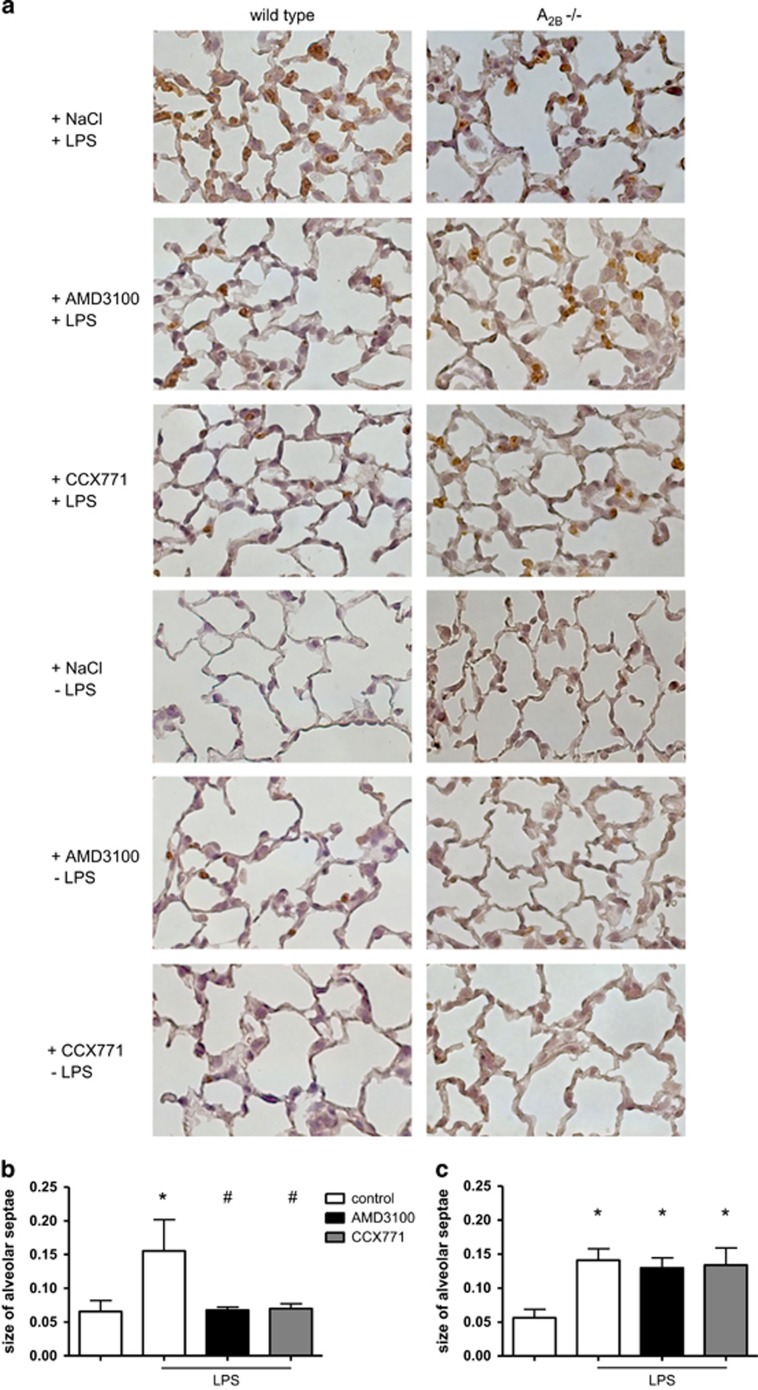
To visualize the effects of inhibiting the SDF-1 corresponding receptors on the architecture of the lung and quantitatively evaluate PMN migration, we prepared slides for immunohistochemistry where PMNs appear brown (Figure 2a). LPS-inhalation increased migrated PMNs and alveolar septae were significantly thickened (Figure 2b). AMD3100 and CCX771 both significantly decreased PMNs and the size of alveolar septae, confirming our results from the in vivo PMN migration assay. Without inflammation, both inhibitors did not affect the size of alveolar septae.
Figure 2.
Impact of AMD3100 and CCX771 on PMN infiltration into the lungs and alveolar thickness identified by immunohistochemistry. Neutrophils were stained with a specific marker and appear brown in histology (rat anti-mouse neutrophil, clone 7/4) (original magnification, × 63). AMD3100 is the specific inhibitor of CXCXR4; CCX771 inhibits CXCR7. All conditions were investigated in wild type (left column) and A2B−/− animals (right column) (a). Images are representatives of n=4 experiments. Alveolar septae of the different conditions were measured in wild type (b) and A2B−/− animals (c). Data are presented as mean ±S.D.; n≥8; *P<0.05 versus control; #P<0.05 versus LPS-treated
Following our hypothesis that an anti-inflammatory effect of CXCR4- and CXCR7-inhibition depends on A2B-receptor signalling, we performed immunohistochemistry slides also in A2B−/− mice. Corresponding to wild type animals, LPS-inhalation increased PMN migration into the lung interstitium and alveolar size rose (Figure 2c). Neither CXCR4- nor CXCR7-antagonism changed PMN counts and alveolar thickness in A2B−/− mice.
In vivo PMN migration assay
To quantitatively determine the effect of AMD3100 and CCX771 on PMN migration, we performed an in vivo PMN migration assay and identified PMNs migrated into the different compartments of the lung by a flowcytometry-based method.
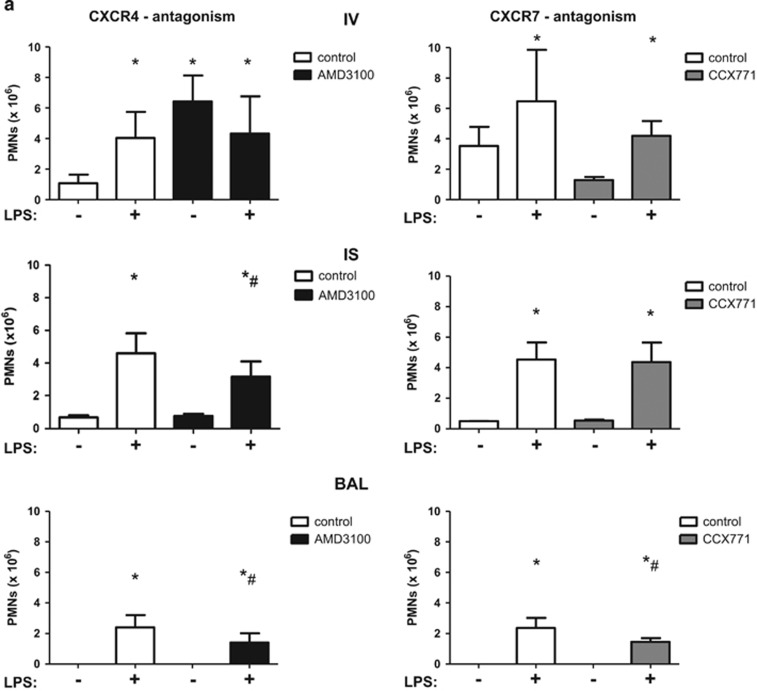
In wild type animals, LPS-inhalation caused a rise of PMNs attached to the endothelium (Figure 3a). SDF-1 keeps PMNs in the bone marrow via CXCR4 and the antagonism of CXCR4 causes a release of neutrophils from the bone marrow in the circulation.15 Therefore, in our model, CXCR4-inhibition increased intravascular PMN counts significantly even without LPS-inhalation. The inhibition of CXCR7 did not lead to any changes in the intravascular compartment. In the interstitium of the lung, LPS caused a rise of PMN influx, whereas AMD3100 decreased migrated PMNs significantly. CCX771 did not influence interstitial PMN counts. In the alveolar space, LPS-inhalation increased migrated PMNs significantly. The reduction of PMN migration by the antagonism of CXCR4 was also apparent in the alveolar space and the inhibition of CXCR7 decreased alveolar PMN reflux.
Figure 3.
Effect of the inhibition of CXCR4 and CXCR7 on PMN migration into the lung. In wild type animals (a) and A2B−/− mice (c), AMD3100 (CXCR4-inhibitor) and CCX771 (CXCR7-inhibitor) were injected and migration of PMNs into the different compartments of the lung without and with LPS (IV = intravascular; IS = interstitial; BAL = alveolar space) quantified. Differential blood counts were performed at indicated time points and total cell counts and also segmented PMNs in wild type animals determined (b) (n≥3). Data are presented as mean ±S.D.; n=4 without LPS; n≥6 with LPS; *P<0.05 versus control; #P<0.05 versus LPS-treated
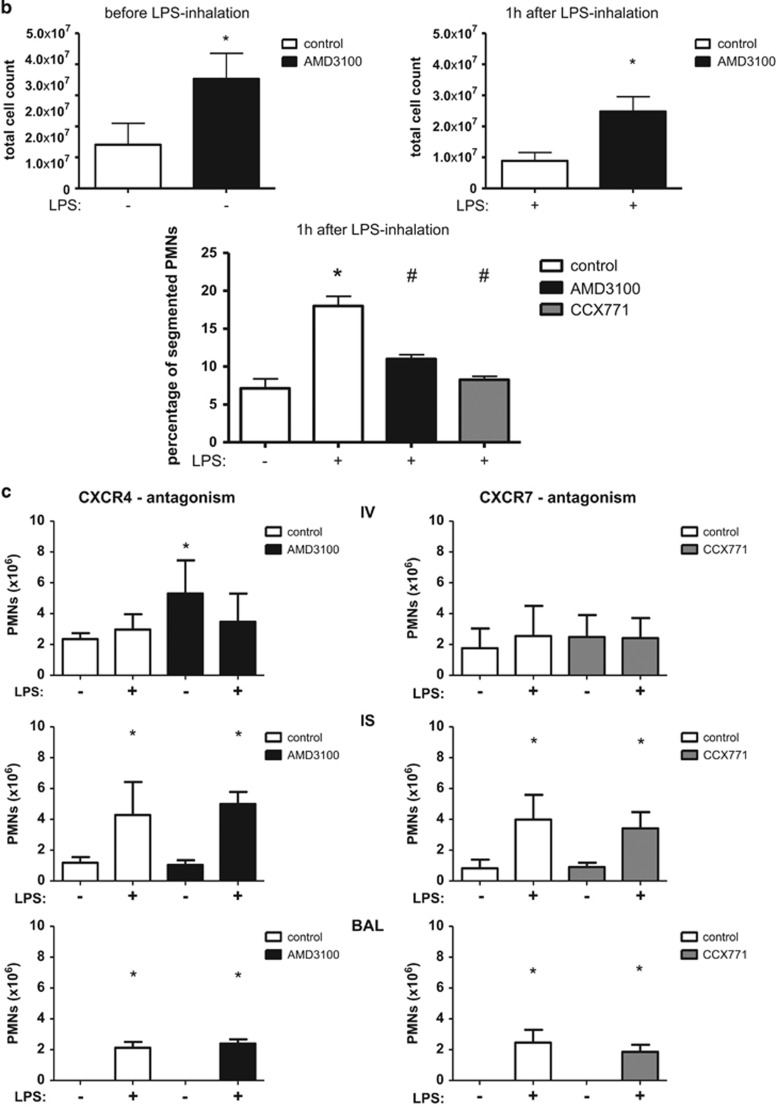
To further investigate the fact that inhibition of CXCR4 increased intravascular PMN counts but, at the same time, reduced migrated PMNs into the lung interstitium and alveolar space, we performed differential blood counts. AMD3100 increased intravascular cell counts significantly even without inflammation, confirming our results from the in vivo migration assay (Figure 3b). LPS-inhalation increased the percentage of segmented and therefore mature PMNs intravascular. These PMNs are known to sequester preferentially into the lung capillaries.6, 16, 17, 18 Differential blood counts further revealed that the percentage of segmented and therefore mature PMNs was significantly decreased in CXCR4- and CXCR7-inhibited animals, explaining the reduced migration of PMNs into the alveolar space and confirming our results from the in vivo transmigration assay.
In A2B−/− mice, CXCR4-antagonism increased PMNs attached to the endothelium without LPS-inhalation (Figure 3c). In the interstitium of the lung, LPS enhanced PMN migration significantly, whereas neither CXCR4- nor CXCR7-inhibition changed these PMN counts. LPS caused a rise of the PMN influx into the alveolar space and, in A2B−/− mice, AMD3100 and CCX771 did not change transepithelial migration, indicating the pivotal role of the A2B−/− receptor in this setting and confirming our findings from immunohistochemistry.
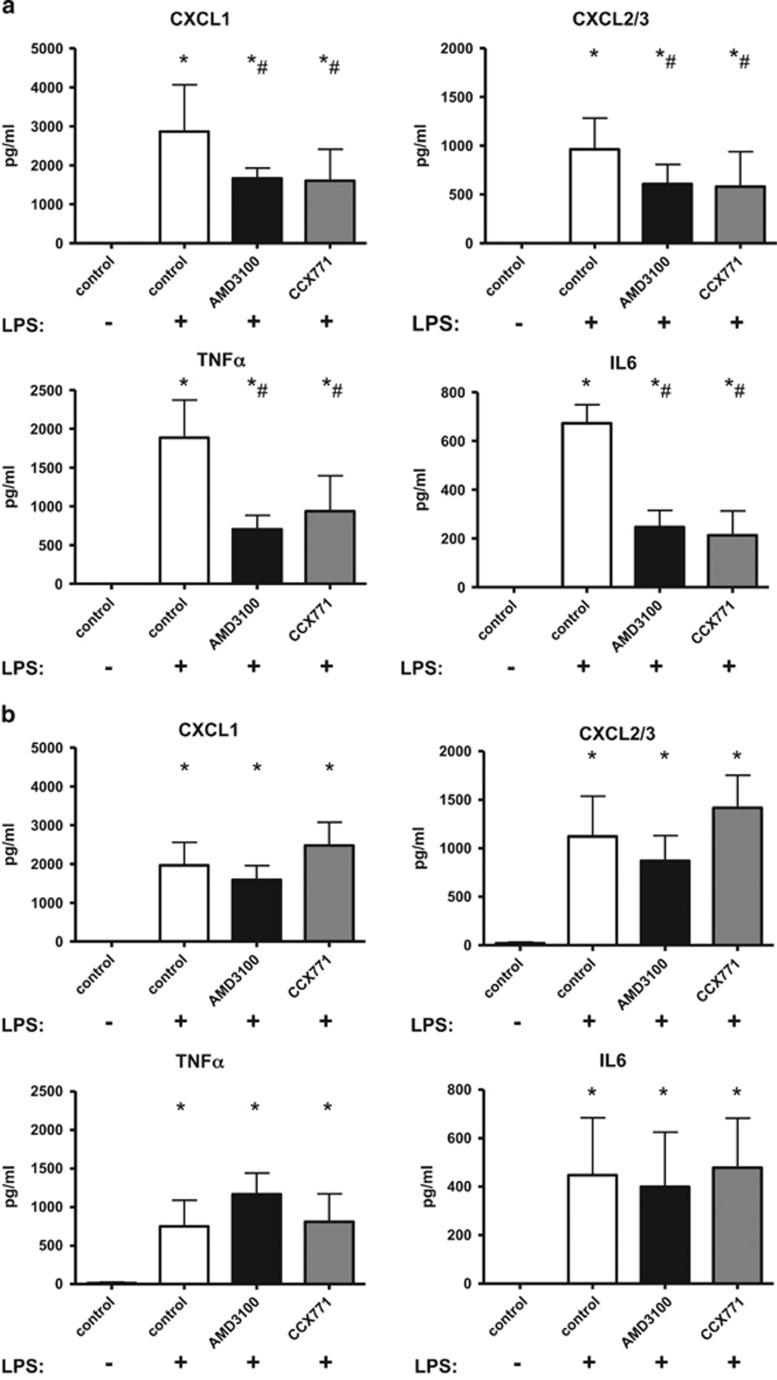
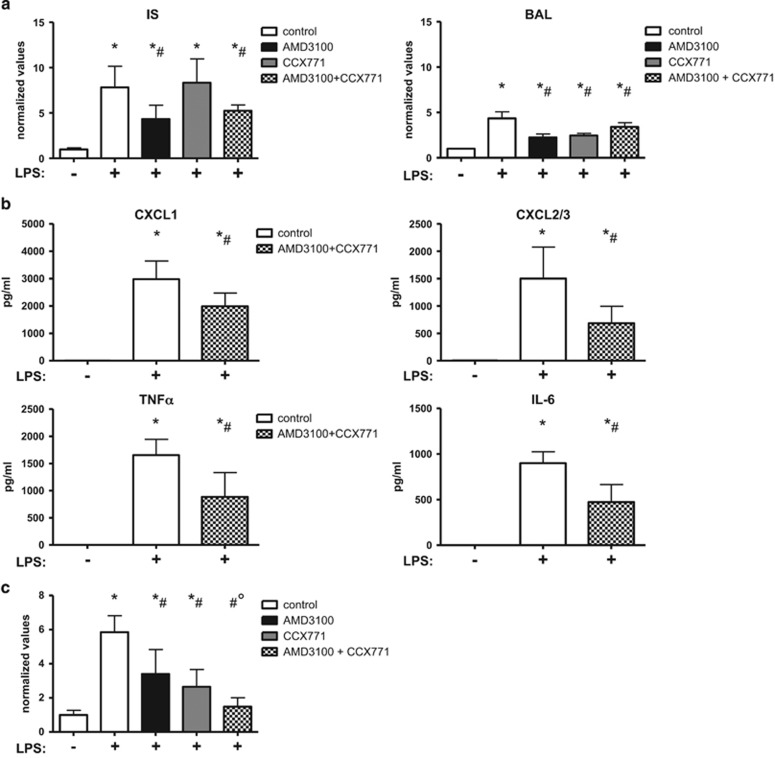
Influence of CXCR4- and CXCR7-antagonism on the release of chemokines
CXCL1 and CXCL2/3 are crucial for PMN migration into inflamed tissue, whereas TNFα and IL6 have a key role in orchestrating complex function and regulation of inflammation.19, 20 LPS caused a rise of all four chemokines in the BAL of mice (Figure 4). In wild type animals, inhibition of CXCR4 and, to a similar amount, CXCR7-antagonism decreased all four chemokines, confirming our results from the PMN migration assay (Figure 4a). In A2B−/− mice, LPS-inhalation significantly increased the chemotactic and inflammatory chemokines (Figure 4b). AMD3100 and CCX771 did not influence any chemokine in these mice, emphasizing again a critical role of the A2B−/− receptor on their mode of action.
Figure 4.
CXCR4- and CXCR7-antagonism and its effects on the release of chemokines. In wild type animals, LPS-inhalation increased all chemokine levels and the administration of both inhibitors decreased this effect (a). In A2B−/− animals, AMD3100 and CCX771 did not influence the release of chemokines (b). Data are presented as mean ±S.D.; n=4 without LPS; n≥7 with LPS; *P<0.05 versus control; #P<0.05 versus LPS-treated
Influence of AMD3100 and CCX771 on different cell types
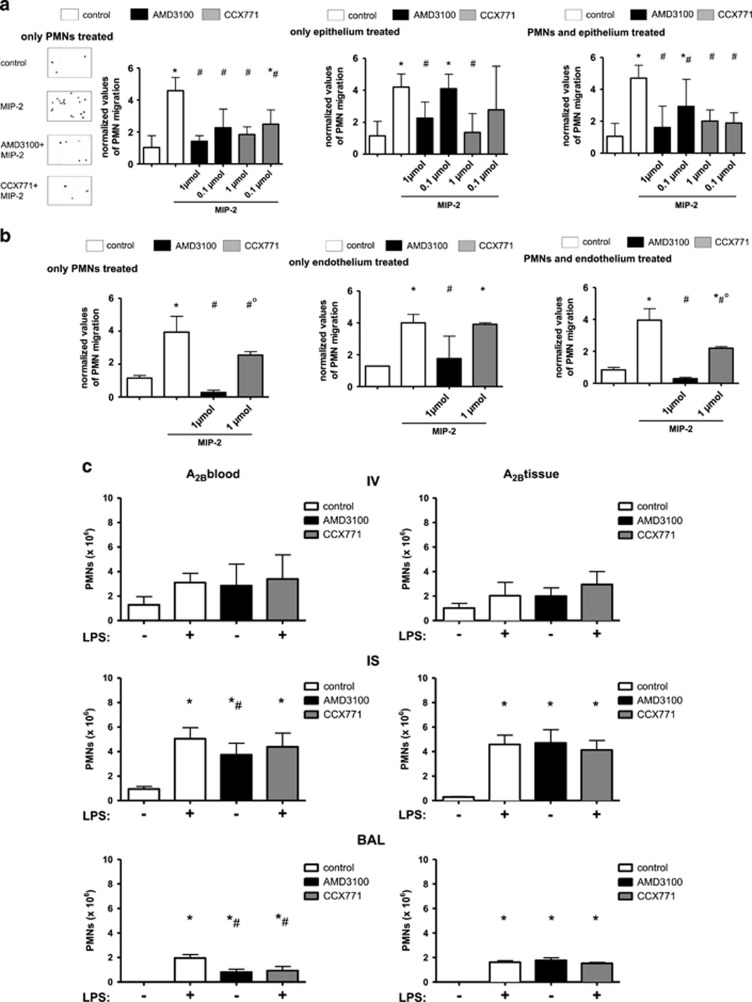
To differentiate between the anti-inflammatory effects of both inhibitors on different cell types, we performed an in vitro PMN transmigration assay. Thereby, freshly isolated human PMNs migrate through a monolayer of human pulmonary epithelial/endothelial cells and can be treated separately.
Isolated treatment of PMNs either with AMD3100 or CCX771 was effective in curbing down PMN migration through a pulmonary epithelial monolayer at two different concentrations (Figure 5a). Thereby, migrated PMNs were quantified by the determination of myeloperoxidase as described later. We added Giemsa-modified stained slides to the first experiment to prove statistical correctness. When only the epithelium was treated, the lower concentrations of both inhibitors were not effective anymore, indicating a distinct role of hematopoietic cells for CXCR4- and CXCR7-antagonism. Combined treatment of PMNs and epithelial cells showed a similar effect compared to PMN-only treatment.
Figure 5.
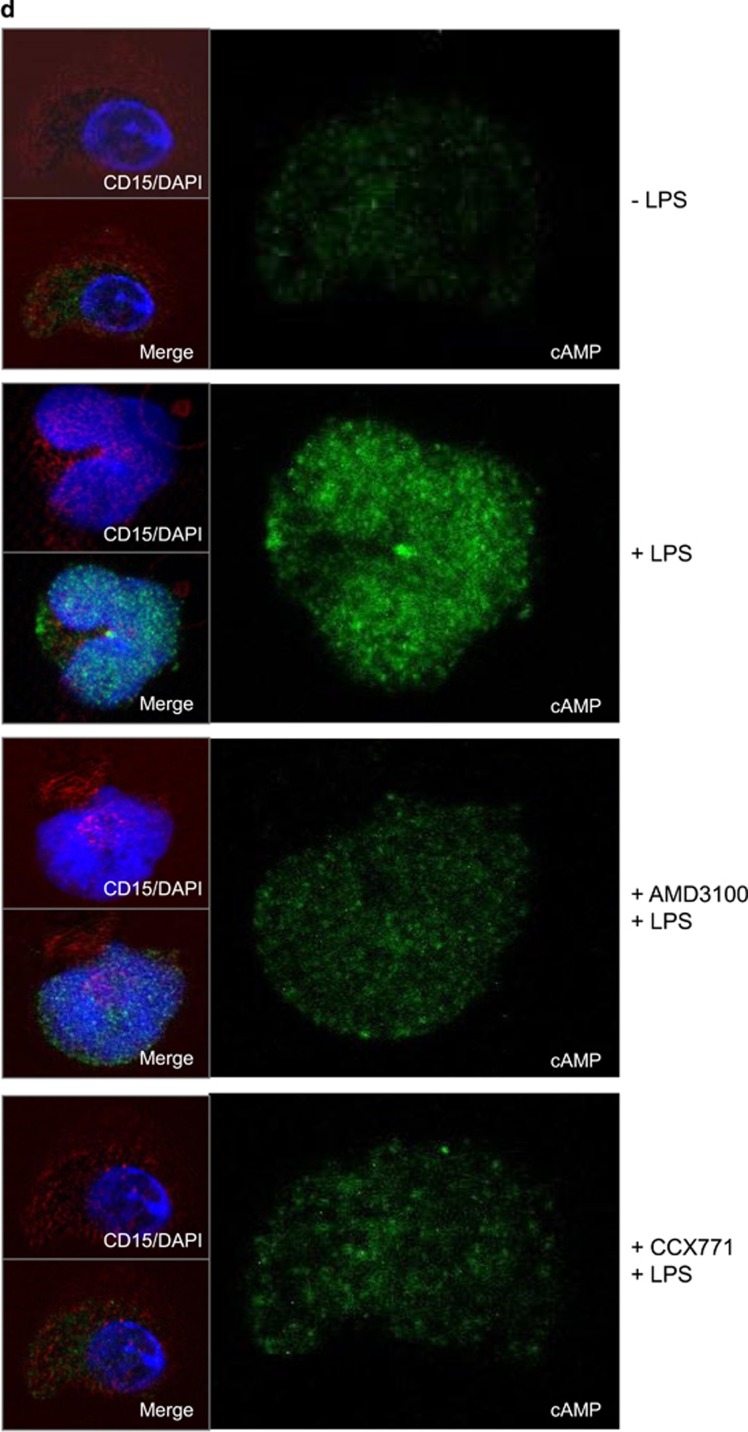
Influence of CXCR4 and CXCR7-inhibion on hematopoietic and non-hematopoietic cells. In vitro transmigration assay of human PMNs through a pulmonary epithelial (a) and endothelial (b) monolayer. PMNs, epithelium or endothelium were treated with CXCR4- (AMD3100) or CXCR7- (CCX771) inhibitors and migration of PMNs through a monolayer of human epithelium/endothelium measured. Migration of PMNs was initiated through the chemokine MIP-2 (CXCL2/3) at indicated wells. Representative pictures of modified Giemsa staining of migrated PMNs were shown to verify results from MPO-measurements (n≥3). Data are presented as mean ±S.D.; (a) n≥3; (b) n≥2; *P<0.05 versus control; #P<0.05 versus MIP-2-treated; °P<0.05 versus AMD3100. In chimeric mice (c), migration of PMNs was determined in the different compartments of the lung (IV = intravascular; IS = interstitial; BAL = alveolar space). A2B−/− mice received bone marrow from wild type mice and possessed the A2B-receptor only on hematopoietic cells (A2Bblood). Wild type mice received bone marrow from A2B−/− and expressed A2B only on non-hematopoietic cells (A2Btissue). Data are presented as mean ±S.D.; n≥3 without LPS; n≥5 with LPS; *P<0.05 versus control; #P<0.05 versus LPS-treated. Cyclic adenosine monophosphate (cAMP) in human PMNs after inflammation and CXCR4/7 treatment (d). Human PMNs were isolated and stimulated as indicated. Images are representatives of four experiments with similar results (original magnification, × 63). cAMP was stained with a specific antibody and appears green, nuclei were stained with DAPI and emerge blue
Both inhibitors were effective in curbing down PMN migration when treated PMNs migrated through pulmonary endothelium (Figure 5b) and, under this condition, AMD3100 was significantly more effective than blocking CXCR7, confirming our in vivo PMN migration results. Corresponding to our results from the in vivo PMN migration assay, treatment with the CXCR7-inhibitor did not show any reduction in terms of PMN migration when only the endothelium was treated. Blocking CXCR4 reduced PMN counts after the endothelium was incubated. The combined treatment of endothelium and PMNs had no additive effect on PMN migration.
The influence of hematopoietic and non-hematopoietic A2B-expression on CXCR4- and CXCR7-antagonism
To further evaluate CXCR4- and CXCR7-inhibition on different cell types, we evaluated their effects in terms of PMN migration in chimeric mice. Wild type mice received bone marrow from A2B−/− and therefore expressed A2B only on non-hematopoietic cells (A2Btissue). A2B−/− mice received bone marrow from wild type mice and possessed the A2B-receptor only on hematopoietic cells (A2Bblood). The in vivo PMN migration assay revealed that the inhibition of CXCR4 and CXCR7 only had anti-inflammatory effects when the A2B-receptor was expressed on hematopoietic cells (A2Bblood) (Figure 5c). Confirming our previous findings from the in vivo migration assay, AMD3100 reduced interstitial and intra-alveolar PMN counts significantly, whereas CCX771 inhibited the PMN-influx into the alveolar system. The expression of the A2B-receptor on non-hematopoietic cells (A2Btissue) led to the same results as in A2B−/− with no anti-inflammatory effects of CXCR4- and CXCR7-inhibition.
Effect of CXCR4/CXCR7-inhibition on the downstream signalling pathway of the A2B-receptor
Changes of cyclic adenosine monophosphate (cAMP) in human PMNs were determined after inflammation and CXCR4/CXCR7-antagonism, to further evaluate the impact of both receptors on the downstream signalling pathway of the A2B-receptor. Inflammation caused an increase of the cAMP level, which was attenuated by the inhibition of CXCR4 and CXCR7, confirming our results with chimeric mice (Figure 5d).
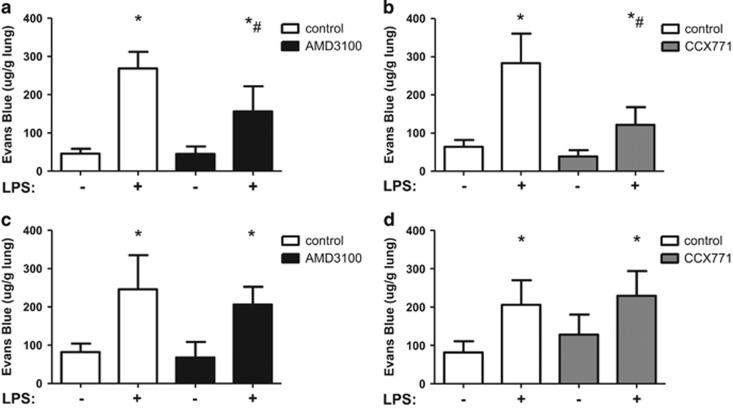
Microvascular permeability
Evans blue extravasation was assessed as an indicator for capillary leakage, since microvascular permeability is the second hallmark of acute pulmonary inflammation besides PMN migration. LPS-treated mice showed a significant increase in capillary leakage (Figure 6). Administration of the specific CXCR4 (Figure 6a) or CXCR7 (Figure 6b) antagonist significantly decreased microvascular permeability, emphasizing their anti-inflammatory potential in stabilizing pulmonary barrier function.
Figure 6.
Microvascular permeability was attenuated by CXCR4- and CXCR7-inhibitors. Six hours after LPS-inhalation, the capillary leakage was assessed by Evans blue extravasation and the influence of CXCR4-antagonism (AMD3100) (a) (respectively CXCR7-antagonism (CCX771) (b)) in wild-type and A2B−/− animals (c, d) investigated. Data are presented as mean ±S.D.; n≥6; *P<0.05 versus control; #P<0.05 versus LPS-treated
In A2B−/− mice, LPS-inhalation increased capillary leakage (Figures 6c and d). AMD3100 (Figure 6c) and CCX771 (Figure 6d) failed to influence microvascular permeability, pointing out again the importance of an A2B−/− receptor signalling for the anti-inflammatory effects of CXCR4- and CXCR7-antagonism.
Combined CXCR4- and CXCR7-inhibition
It has been discussed whether CXCR4 and CXCR7 form a complex and may act additive.14 Therefore, we performed the PMN migration assay and combined the administration of AMD3100 and CCX771 (Figure 7a). The combined treatment showed no synergistic effect and was as effective as AMD3100 alone.
Figure 7.
Combined inhibition of CXCR4 and CXCR7. The effect of simultaneous CXCR4- and CXCR7-antagonism was investigated in terms of PMN migration (IV=intravascular; IS=interstitial; BAL=bronchoalveolar lavage) (a), chemokine release (b) and microvascular permeability (c). There was no additive anti-inflammatory effect concerning PMN migration into the lung, but in terms of stabilizing the capillary leakage. Data are presented as mean ±S.D.; n≥6; *P<0.05 versus control; #P<0.05 versus LPS-treated; °P<0.05 versus single treatment of AMD3100 or CCX771
Confirming our results from the in vivo PMN migration assay and our results from the chemokine assay of the single treatments, additive CXCR4- and CXCR7-inhibition decreased all four chemokines significantly (Figure 7b).
Further on, we investigated the combined treatment in terms of microvascular permeability (Figure 7c). In this setting, simultaneous inhibition of CXCR4 and CXCR7 was significantly more effective compared to the inhibition of each receptor alone and almost completely prevented an increase of capillary leakage after LPS-inhalation.
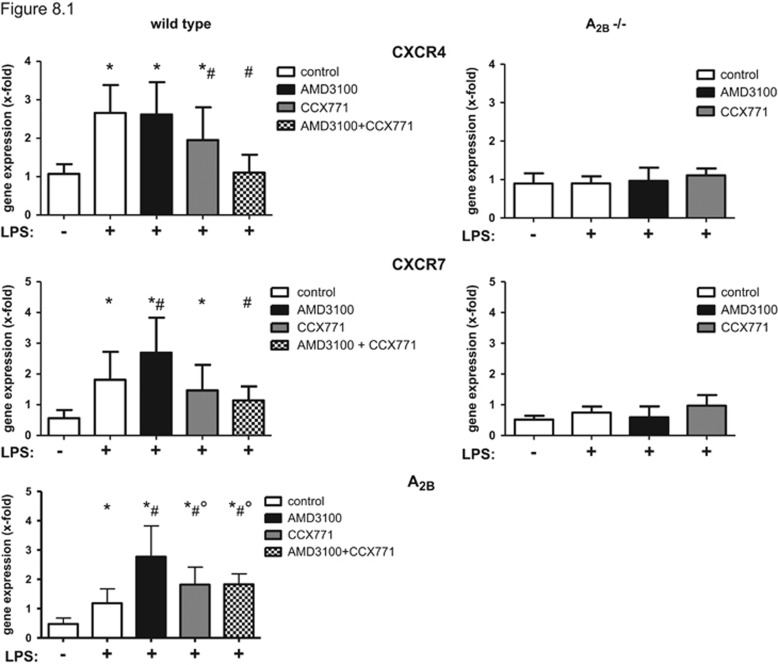
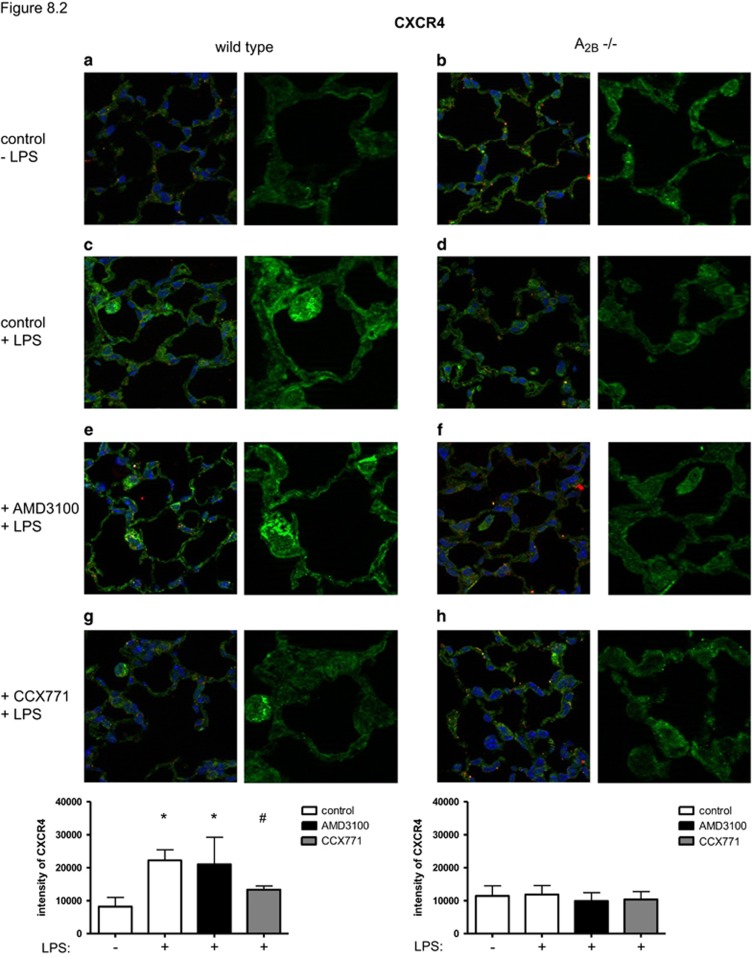
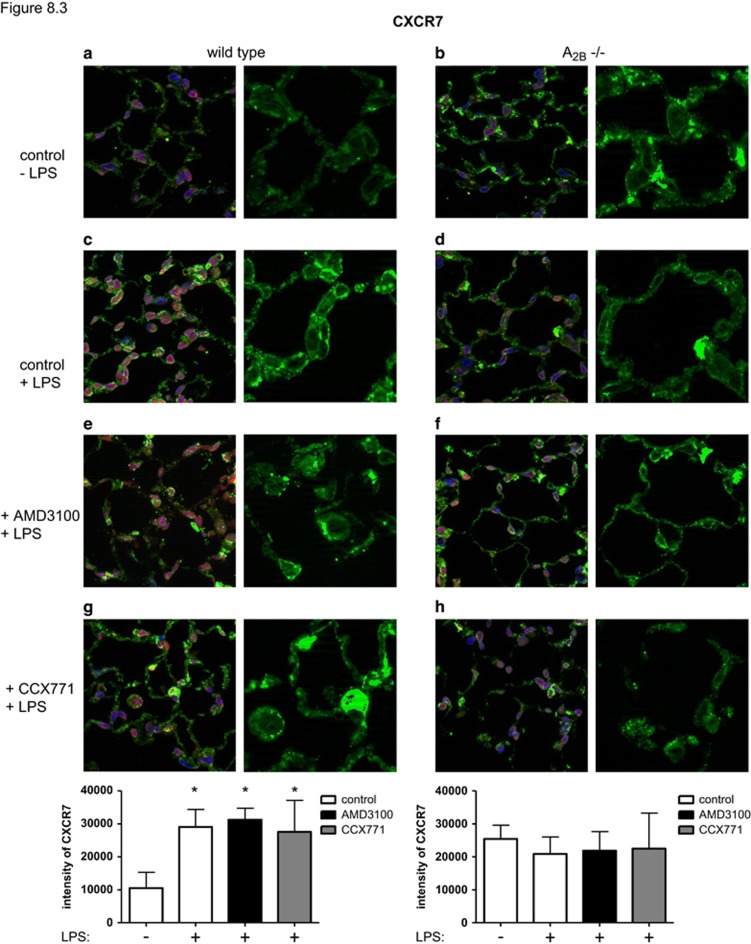
CXCR4/CXCR7- and A2B-gene expression and protein level in the lung
LPS-inhalation increased the expression of CXCR4 significantly (Figure 8.1). The inhibition of CXCR4 did not result in reduced expression of the receptor, whereas CXCR7-antagonism reduced CXCR4 levels as well as the synergistic administration of both inhibitors. These findings were confirmed on protein levels (Figure 8.2).
Figure 8.
The impact of inflammation, CXCR4- and CXCR7-antagonism on the expression of both receptors and the A2B-receptor. LPS induced CXCR4 (n≥7), CXCR7- (n≥7) and A2B-gene expression (n≥6) in lungs of mice (8.1). Images are representatives of four experiments with similar results (original magnification, × 63). CXCR4 (8.2) (respectively CXCR7 (8.3)) were stained with specific antibodies and appear green, nuclei were stained with DAPI and emerge blue. Data are presented as mean±S.D.; n≥6; *P<0.05 versus control; #P<0.05 versus LPS-treated; °P<0.05 versus single treatment of AMD3100
The expression of CXCR7 was also augmented during inflammation (Figure 8.1). AMD3100 increased CXCR7-expression even further, while CCX771 showed no effect. On protein level, both inhibitors did not lead to any change (Figure 8.3). The synergistic administration of both inhibitors reduced CXCR7-expression. The expression of both receptors was not influenced in A2B−/− mice—neither by inflammation nor by the administration of the specific inhibitors.
The expression of A2B was increased after LPS-inhalation and by the administration of both inhibitors even further, highlighting again the link of CXCR4/CXCR7 and the A2B-receptor.
Discussion
In humans, it has been shown that SDF-1 is expressed in the lung during acute lung injury.13 For the first time, we determined the pivotal role of the receptors of SDF-1—CXCR4 and CXCR7—in acute pulmonary inflammation and linked their anti-inflammatory potential to A2B-receptor signalling.
In the present study, we investigated a previously unknown anti-inflammatory effect of CXCR7 in acute pulmonary inflammation, predominantly in reducing transepithelial PMN migration into the alveolar space. Additionally, we are the first to determine the impact of CXCR4-inhibition on PMN migration into the different compartments of the lung. According to the findings of Petty et al,13 CXCR4-antagonism increased circulating PMNs, but decreased migrated PMNs into the interstitium of the lung and also the BAL, highlighting its anti-inflammatory potential. Thereby, inhibition of CXCR4 was also effective in decreasing interstitial PMN migration when given even 6 h after the inflammatory stimulus, verifying the role of SDF-1 in the later phase of PMN recruitment13 and also highlighting its clinical potential.
In the present study, the inhibition of CXCR4 and CXCR7 also showed a pivotal role in stabilization of the endothelial barrier. Both antagonists decreased the size of alveolar septae and minimized capillary leakage—the second hallmark of acute pulmonary inflammation.
Hypoxia induced the SDF-1/CXCR4 axis in multipotent stromal cells and increased their migration.21, 22 Additionally, hypoxia increased protein expression of CXCR4 and CXCR7 in the lung.23, 24 In our study on acute pulmonary inflammation, the expression of CXCR4 and CXCR7 also augmented as a reaction on hyper-inflammation. This is in accordance with the hypoxia-induced rise since inflammation is associated with tissue hypoxia, causing the so-called inflammatory hypoxia.25
In the present study, the results emphasized a previously unknown detrimental role of the A2B-receptor on SDF-1 signalling in acute pulmonary inflammation. Our findings indicate that the anti-inflammatory effects of CXCR4- and CXCR7-antagonism in terms of PMN migration, chemokine release and microvascular permeability are linked to adenosine A2B-receptor signalling. Inflammation increased the expression of CXCR4 and CXCR7 in wild type animals. A2B−/− mice express both receptors in the lung, but their expression was not influenced by inflammation or the inhibition of one of the receptors. Pointing to the same direction, the anti-inflammatory increase of the A2B-receptor as a reaction on inflammation10 was significantly augmented by inhibiting CXCR4 or CXCR7. Previous studies implicated a connection between adenosine and the chemokine SDF-1. It has been shown that extracellular adenosine triphosphate potentiated the chemotactic response to bone marrow-derived human mesenchymal stem cells and increased their migration.26 Dibutyryl cAMP increased expression of SDF-1 in wound tissue and enhanced endothelial progenitor cell migration.27 A link between CXCR4 and the A2B-receptor has been shown by a study about human colorectal carcinoma cells.5 Adenosine, which is present in the extracellular fluid of tumours because of their hypoxia, acted through A2A- and A2B-receptors to upregulate CXCR4-expression on tumour cells. A higher CXCR4-expression enables tumour cells to migrate towards SDF-1 and enhances proliferation and tumour dissemination.
The A2B-receptor plays a detrimental role in acute lung injury. Several studies showed that deletion of the receptor deteriorates the inflammation, whereas the administration of a specific A2B-receptor-agonist ameliorates tissue inflammation.10, 28, 29, 30, 31 In a previous study of our group, we identified the A2B-receptor on bone marrow cells as crucial for the anti-inflammatory effects of this receptor in our model of acute pulmonary inflammation.10 This is in accordance with the findings of the present study, where the anti-inflammatory effects of CXCR4- and CXCR7-antagonism depend on the expression of A2B on blood cells. The findings of Yang et al also point to this direction, where chimeric mice with the expression of A2B on blood cells showed less vascular lesion formation most probably due to reduced CXCR4 signalling.11
Sepsis changes adenosine affinity to its receptors and can further influence the receptor expression.10, 32 According to our results, patients with acute pulmonary inflammation, who would potentially benefit from inhibiting CXCR4 or CXCR7, should first be examined on their adenosine levels and receptor distribution. Considering our findings from the in vivo migration assay with chimeric mice, the expression of the A2B-receptor on hematopoietic cells is crucial. With the link of the anti-inflammatory effects of CXCR4/7-antagonism and A2B, we follow the recommendations from Dushiantan et al, who suggests to identify subgroups of patients where a specific treatment of pulmonary inflammation would be successful.33
Conclusion
The presented data show a pivotal anti-inflammatory effect of inhibiting CXCR4 and CXCR7 in terms of PMN migration, chemokine release and microvascular permeability in acute pulmonary inflammation. We linked these anti-inflammatory effects to hematopoietic A2B-receptor signalling.
Materials and methods
Animals
C57BL/6 male mice were obtained from Charles River Laboratories (Germany) as corresponding wild type animals for A2B gene-deficient mice (A2B−/−), which we received from Dr Katya Ravid (Boston University, School of Medicine, Department of Biochemistry, Boston, MA, USA). Mice were between 8 and 12 weeks old. All animal protocols were approved by the Animal Care and Use Committee of the University of Tübingen.
CXCR4- and CXCR7-inhibitors
Ideal concentration of the specific CXCR4-inhibitor AMD3100 (Sigma-Aldrich, Germany) and CCX771, the specific CXCR7-inhibitor, (ChemoCentryx, CA, USA) were tested intraperitoneally respectively subcutaneoulsy based on the literature and company recommendations, respectively12, 24 (data not shown). The effect of the time-dependency of the inhibition of both receptors was evaluated (n≥4). Control mice received the solvent and close analogue of the antibody (ChemoCentryx).
Murine model of acute lung injury
As described in detail before, 4–8 animals inhaled nebulized LPS from Salmonella enteritidis (Sigma-Aldrich) (a total of 7 ml, 500 μg/ml), which led to a reproducible acute pulmonary inflammation.34, 35
Immunohistochemistry
Lungs were prepared as described previously (n=4).10 Since there were no differences between the solvent of AMD3100 and the vehicle control of CCX771 (data not shown), only one control is displayed in Figure 2.
In vivo migration assay
Twenty-four hours after LPS-inhalation, we determined PMN migration into the different compartments of the lung via a flowcytometry-based method as described in detail before, including the gating process (n≥7).36 Briefly, fluorescent GR-1 (clone RB6-8C5) was injected into the tail vein of mice to mark all intravascular PMNs. To remove non-adherent leukocytes from the pulmonary vasculature, lungs were flushed free of blood by injecting saline into the beating right ventricle. PMNs from the alveolar space were obtained by BAL, which was performed with 5 ml NaCl. Lungs were homogenized and incubated with enzymes (hyaluronidase, collagenase and DNAse) for 30 min at 37 °C. Absolute cell counts were determined in the BAL and lungs. Fluorescent antibodies to CD45 (clone 30-F11) and 7/4 (clone 7/4) were added to the received cell suspension. All leukocytes were gated by their typical appearance in the forward/sideward scatter and further specified by their CD45 positive appearance. In the lung, we identified out of this CD45+-population intravascular PMNs, which were 7/4 positive and GR-1 positive. Interstitial PMNs were assigned as CD45 positive, 7/4 positive and GR-1 negative cells. In the BAL, CD45+ cells were further classified as 7/4 positive and GR-1 positive and identified as PMNs.
Generation of chimeric mice
To identify whether the expression of the A2B-receptor on hematopoietic or non-hematopoietic cells is necessary for the anti-inflammatory effects of CXCR4- and CXCR7-inhibition, we generated chimeric mice (n≥5) as described previously.10 RT-PCRs of tissue and bone marrow were performed as control for successful transplantation (data not shown).
Differential blood counts
Blood counts were performed from peripheral blood of the tail vein at indicated time points (modified Giemsa staining: Diff Quik; Dade Behring, Newark, DE, USA) (n≥3). Differential counts were conducted by two experienced independent observers by counting 100 leukocytes in randomly selected fields of view.
Chemokine release
SDF-1 levels were determined in the supernatant of lung homogenates (n=8) and in the BAL (n=4) 6 and 24 h after LPS-inhalation according to the protocol of the manufacturer (Quantikine ELISA, R&D, Abingdon, UK).
Three hours after LPS-inhalation, the release of CXCL 1, CXCL 2/3, tumour necrosis factor-α (TNFα) and interleukin-6 (IL-6) were measured in the BAL of mice (n≥6).37
Microvascular leakage
Evans blue extravasation was determined as a marker of capillary leakage.37 Evans blue (20 mg/kg, Sigma Aldrich, Steinheim, Germany) was injected into the tail vein 6 h after LPS exposure (n≥6).10 Thirty minutes later, intravascular Evans blue in the lungs was removed by flushing the beating right ventricle. Lungs were homogenized and Evans blue was extracted with formamide and the final concentration determined colorimetrically.
CXCR4- and CXCR7 expression and protein level
We determined the expression of CXCR4, CXCR7 and A2B in lungs of mice by RT-PCR (n≥7). The method was performed with the following primers CXCR4 (5′-CCC CGA TAG CCT GTG GAT-3′ and 5′-AGG ATG ACT GTC GTC TTG AGG G-3′), CXCR7 (5′-GGA GCC TGC AGC GCT CAC CG-3′ and 5′-CTT AGCCTG GAT ATT CAC CC-3′), and A2B (5′-GCA TTA CAG ACC CCC ACC AA-3′ and 5′-TTT ATA CCT GAG CGG GAC GC-3′) as described.37
To further verify results from gene expression on protein level, we measured light intensity of fluorescent slides of lungs of mice. Rabbit polyclonal anti-CXCR4 and goat polyclonal anti-CXCR7 were used as primary antibody (Santa Cruz Biotechnology, Dallas, TX, USA). Images were visualized by using a confocal microscope (LSM 510, Meta, Carl Zeiss, Jena, Germany) and analysed by ZEN 5.0. Images are representatives of four experiments and were analysed using imageJ, a public programme being developed at the National Institutes of Health to officially analyse scientific images.
In vitro PMN migration
We performed the in vitro transmigration assay of human PMNs through a monolayer of pulmonary epithelial (NCI-H441, ATCC, USA) (n≥3) or primary pulmonary endothelial cells (HMVEC-L, Lonza Walkersville, Walkersville, MD, USA). Endothelial (respectively epithelial) cells, PMNs, or both were incubated with the specific CXCR4 or CXCR7 antagonist at indicated concentrations. Human endothelial/epithelial cells were cultivated on inserts of a transwell system (3.0-μm pore size, 6.5-mm diameter; Costar, Cambridge, MA, USA) until reaching confluence. Isolated human PMNs (Percoll gradient; GE Healthcare Bio-Sciences AB, Uppsala, Sweden) migrated through the monolayer of endothelial/epithelial cells along a chemotactic gradient (CXCL2/3; 200 ng/ml; Pepro Tech, Hamburg, Germany). Migrated PMNs were quantified by determination of myeloperoxidase (absorption length: 405 nm) in the bottom wells. Additionally, migrated PMNs were evaluated by modified Giemsa staining (Diff Quik) by two experienced independent observers.
Influence of CXCR4/CXCR7 inhibition on cAMP levels in human PMNs
Isolated human PMNs (Percoll gradient; GE Healthcare Bio-Sciences) were treated with the specific CXCR4/CXCR7 antagonist (1 μmol) and LPS (1 μg/μl). Anti-cAMP antibody (Abcam, Cambridge, UK) was used as primary antibody. Images were visualized by using a confocal microscope (LSM 510, Meta, Carl Zeiss) and analysed by ZEN 5.0. Images are representatives of four experiments and were analysed using imageJ, a public programme being developed at the National Institutes of Health to officially analyse scientific images.
Statistical analysis
Data are presented as mean±S.D. unless indicated otherwise. Statistical analysis was performed using GraphPad Prism version 5.3 for Windows (GraphPad Software, San Diego, CA, USA). Differences between the groups were evaluated by one-way ANOVA followed by Bonferroni post hoc test. P<0.05 was considered statistically significant.
Acknowledgments
A2B gene-deficient mice were provided by Professor Katya Ravid (Boston University, School of Medicine, Department of Biochemistry, Boston, MA, USA)
CCX771, the specific CXCR7-inhibitor, was supplied by ChemoCentryx, USA.
Footnotes
Edited by Y Shi
The authors declare no conflict of interest.
References
- Matthay MA, Ware LB, Zimmerman GA. The acute respiratory distress syndrome. J Clin Invest 2012; 122: 2731–2740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herridge MS, Cheung AM, Tansey CM, Matte-Martyn A, Diaz-Granados N, Al-Saidi F et al. One-year outcomes in survivors of the acute respiratory distress syndrome. N Engl J Med 2003; 348: 683–693. [DOI] [PubMed] [Google Scholar]
- Grommes J, Soehnlein O. Contribution of neutrophils to acute lung injury. Mol Med 2011; 17: 293–307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aiuti A, Webb IJ, Bleul C, Springer T, Gutierrez-Ramos JC. The chemokine SDF-1 is a chemoattractant for human CD34+ hematopoietic progenitor cells and provides a new mechanism to explain the mobilization of CD34+ progenitors to peripheral blood. J Exp Med 1997; 185: 111–120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Richard CL, Tan EY, Blay J. Adenosine upregulates CXCR4 and enhances the proliferative and migratory responses of human carcinoma cells to CXCL12/SDF-1alpha. Int J Cancer 2006; 119: 2044–2053. [DOI] [PubMed] [Google Scholar]
- Konrad FM, Braun S, Ngamsri KC, Vollmer I, Reutershan J. Heme oxygenase-1 attenuates acute pulmonary inflammation by decreasing the release of segmented neutrophils from the bone marrow. Am J Physiol Lung Cell Mol Physiol 2014; 307: L707–L717. [DOI] [PubMed] [Google Scholar]
- Rath D, Chatterjee M, Borst O, Muller K, Stellos K, Mack AF et al. Expression of stromal cell-derived factor-1 receptors CXCR4 and CXCR7 on circulating platelets of patients with acute coronary syndrome and association with left ventricular functional recovery. Eur Heart J 2014; 35: 386–394. [DOI] [PubMed] [Google Scholar]
- Chen WC, Tzeng YS, Li H, Tien WS, Tsai YC. Lung defects in neonatal and adult stromal-derived factor-1 conditional knockout mice. Cell Tissue Res 2010; 342: 75–85. [DOI] [PubMed] [Google Scholar]
- Eckle T, Koeppen M, Eltzschig HK. Role of extracellular adenosine in acute lung injury. Physiology 2009; 24: 298–306. [DOI] [PubMed] [Google Scholar]
- Konrad FM, Witte E, Vollmer I, Stark S, Reutershan J. Adenosine receptor A2b on hematopoietic cells mediates LPS-induced migration of PMNs into the lung interstitium. Am J Physiol Lung Cell Mol Physiol 2012; 303: L425–L438. [DOI] [PubMed] [Google Scholar]
- Yang D, Koupenova M, McCrann DJ, Kopeikina KJ, Kagan HM, Schreiber BM et al. The A2b adenosine receptor protects against vascular injury. Proc Natl Acad Sci USA 2008; 105: 792–796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martin C, Burdon PC, Bridger G, Gutierrez-Ramos JC, Williams TJ, Rankin SM. Chemokines acting via CXCR2 and CXCR4 control the release of neutrophils from the bone marrow and their return following senescence. Immunity 2003; 19: 583–593. [DOI] [PubMed] [Google Scholar]
- Petty JM, Sueblinvong V, Lenox CC, Jones CC, Cosgrove GP, Cool CD et al. Pulmonary stromal-derived factor-1 expression and effect on neutrophil recruitment during acute lung injury. J Immunol 2007; 178: 8148–8157. [DOI] [PubMed] [Google Scholar]
- Gambaryan N, Perros F, Montani D, Cohen-Kaminsky S, Mazmanian M, Renaud JF et al. Targeting of c-kit+ haematopoietic progenitor cells prevents hypoxic pulmonary hypertension. Eur Respir J 2011; 37: 1392–1399. [DOI] [PubMed] [Google Scholar]
- Tchernychev B, Ren Y, Sachdev P, Janz JM, Haggis L, O'Shea A et al. Discovery of a CXCR4 agonist pepducin that mobilizes bone marrow hematopoietic cells. Proc Natl Acad Sci USA 2010; 107: 22255–22259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kubo H, Graham L, Doyle NA, Quinlan WM, Hogg JC, Doerschuk CM. Complement fragment-induced release of neutrophils from bone marrow and sequestration within pulmonary capillaries in rabbits. Blood 1998; 92: 283–290. [PubMed] [Google Scholar]
- van Eeden SF, Kitagawa Y, Klut ME, Lawrence E, Hogg JC. Polymorphonuclear leukocytes released from the bone marrow preferentially sequester in lung microvessels. Microcirculation 1997; 4: 369–380. [DOI] [PubMed] [Google Scholar]
- van Eeden SF, Lawrence E, Sato Y, Kitagawa Y, Hogg JC. Neutrophils released from the bone marrow by granulocyte colony-stimulating factor sequester in lung microvessels but are slow to migrate. Eur Respir J 2000; 15: 1079–1086. [DOI] [PubMed] [Google Scholar]
- Schmal H, Shanley TP, Jones ML, Friedl HP, Ward PA. Role for macrophage inflammatory protein-2 in lipopolysaccharide-induced lung injury in rats. J Immunol 1996; 156: 1963–1972. [PubMed] [Google Scholar]
- Schumacher C, Clark-Lewis I, Baggiolini M, Moser B. High- and low-affinity binding of GRO alpha and neutrophil-activating peptide 2 to interleukin 8 receptors on human neutrophils. Proc Natl Acad Sci USA 1992; 89: 10542–10546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hung SC, Pochampally RR, Hsu SC, Sanchez C, Chen SC, Spees J et al. Short-term exposure of multipotent stromal cells to low oxygen increases their expression of CX3CR1 and CXCR4 and their engraftment in vivo. PLoS One 2007; 2: e416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsai CC, Yew TL, Yang DC, Huang WH, Hung SC. Benefits of hypoxic culture on bone marrow multipotent stromal cells. Am J Blood Res 2012; 2: 148–159. [PMC free article] [PubMed] [Google Scholar]
- Ceradini DJ, Kulkarni AR, Callaghan MJ, Tepper OM, Bastidas N, Kleinman ME et al. Progenitor cell trafficking is regulated by hypoxic gradients through HIF-1 induction of SDF-1. Nat Med 2004; 10: 858–864. [DOI] [PubMed] [Google Scholar]
- Costello CM, McCullagh B, Howell K, Sands M, Belperio JA, Keane MP et al. A role for the CXCL12 receptor, CXCR7, in the pathogenesis of human pulmonary vascular disease. Eur Respir J 2012; 39: 1415–1424. [DOI] [PubMed] [Google Scholar]
- Eltzschig HK, Bratton DL, Colgan SP. Targeting hypoxia signalling for the treatment of ischaemic and inflammatory diseases. Nat Rev Drug Discov 2014; 13: 852–869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferrari D, Gulinelli S, Salvestrini V, Lucchetti G, Zini R, Manfredini R et al. Purinergic stimulation of human mesenchymal stem cells potentiates their chemotactic response to CXCL12 and increases the homing capacity and production of proinflammatory cytokines. Exp Hematol 2011; 393: 360–374. [DOI] [PubMed] [Google Scholar]
- Asai J, Takenaka H, Katoh N, Kishimoto S. Dibutyryl cAMP influences endothelial progenitor cell recruitment during wound neovascularization. J Invest Dermatol 2006; 126: 1159–1167. [DOI] [PubMed] [Google Scholar]
- Eckle T, Grenz A, Laucher S, Eltzschig HK. A2B adenosine receptor signaling attenuates acute lung injury by enhancing alveolar fluid clearance in mice. J Clin Invest 2008; 118: 3301–3315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoegl S, Brodsky KS, Blackburn MR, Karmouty-Quintana H, Zwissler B, Eltzschig HK. Alveolar epithelial A2B adenosine receptors in pulmonary protection during acute lung injury. J Immunol 2015; 195: 1815–1824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koscso B, Trepakov A, Csoka B, Nemeth ZH, Pacher P, Eltzschig HK et al. Stimulation of A2B adenosine receptors protects against trauma-hemorrhagic shock-induced lung injury. Purinergic Signal 2013; 9: 427–432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schingnitz U, Hartmann K, Macmanus CF, Eckle T, Zug S, Colgan SP et al. Signaling through the A2B adenosine receptor dampens endotoxin-induced acute lung injury. J Immunol 2010; 184: 5271–5279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kreth S, Kaufmann I, Ledderose C, Luchting B, Thiel M. Reduced ligand affinity leads to an impaired function of the adenosine A2A receptor of human granulocytes in sepsis. J Cell Mol Med 2009; 13: 985–994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dushianthan A, Grocott MP, Postle AD, Cusack R. Acute respiratory distress syndrome and acute lung injury. Postgrad Med J 2011; 87: 612–622. [DOI] [PubMed] [Google Scholar]
- Konrad FM, Knausberg U, Hone R, Ngamsri KC, Reutershan J. Tissue heme oxygenase-1 exerts anti-inflammatory effects on LPS-induced pulmonary inflammation. Mucosal Immunol 2015; 9: 98–111. [DOI] [PubMed] [Google Scholar]
- Reutershan J, Stockton R, Zarbock A, Sullivan GW, Chang D, Scott D et al. Blocking p21-activated kinase reduces lipopolysaccharide-induced acute lung injury by preventing polymorphonuclear leukocyte infiltration. Am J Respir Crit Care Med 2007; 175: 1027–1035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reutershan J, Basit A, Galkina EV, Ley K. Sequential recruitment of neutrophils into lung and bronchoalveolar lavage fluid in LPS-induced acute lung injury. Am J Physiol Lung Cell Mol Physiol 2005; 289: L807–L815. [DOI] [PubMed] [Google Scholar]
- Konrad FM, Neudeck G, Vollmer I, Ngamsri KC, Thiel M, Reutershan J. Protective effects of pentoxifylline in pulmonary inflammation are adenosine receptor A2A dependent. FASEB J 2013; 27: 3524–3535. [DOI] [PubMed] [Google Scholar]