Abstract
Telemedicine has deeply innovated the field of emergency cardiology, particularly the treatment of acute myocardial infarction. The ability to record an ECG in the early prehospital phase, thus avoiding any delay in diagnosing myocardial infarction with direct transfer to the cath-lab for primary angioplasty, has proven to significantly reduce treatment times and mortality. This consensus document aims to analyse the available evidence and organizational models based on a support by telemedicine, focusing on technical requirements, education, and legal aspects.
Keywords: Telemedicine, Telecardiology, Acute myocardial infarction, Unstable angina, STEMI, Acute coronary syndrome, Hub & spoke networks
Revised by: Antonio Francesco Amico, Roberto Antonicelli, Francesco Sisto
Consensus Document Approval Faculty in appendix
Introduction
Definition of telemedicine
Telemedicine is defined as a mode of delivering health care services, through the use of innovative technologies, in particular the Information and Communication Technologies, in situations where the health professional and the patient or two professionals are not in the same place. Telemedicine involves the secure transmission of information and medical data in the form of text, sound, images or other modalities for the prevention, diagnosis, treatment and subsequent patient follow-up.1 The telemedicine services should be therefore considered as a true diagnostic/therapeutic health service.
Utility of telemedicine
Telemedicine can be used in different contexts and by different operators: general practitioners, hospital specialists, any health care worker, including non-physicians, and patients may benefit from the use of telemedicine in several aspects (better management, simplification of procedures, reduction in transfer). Telemedicine transmission may include texts (medical records, personal data), images (electrocardiograms, ambulatory electrocardiograms, telemetric monitoring, radiological exams, ultrasound), audio recordings, videos.
Telemedicine and cardiovascular disease
The most important areas of application of telemedicine in the field of cardiology are:
early (pre-hospital) diagnosis of acute myocardial infarction (AMI) with electrocardiogram transmission
remote control of device (pacemakers, defibrillators)
monitoring of patients with chronic heart failure
monitoring of patients arrhythmias
transmission of echo images to a III level centre for a ‘second opinion’
ST-elevation acute myocardial infarction (STEMI) network activation for primary percutaneous coronary intervention (PCI) is recommended by guidelines and should be as fast as possible; most regions in Italy have therefore implemented efficient STEMI networks over the past 15 years. Pre-hospital electrocardiogram and diagnosis is one of the most efficient solutions to reduce time of treatment. Current technologies allow now for electrocardiogram transmission in a very short time and with a very high quality to dispatch centres, arranging the best reperfusion strategy.2 Similarly, remote control and monitoring of ICDs has progressively improved over the last years, and this has allowed a significant reduction in clinical visits and hospital access, and faster recognition of device failure or arrhythmic complications.
Home monitoring of heart failure patients seems to have positive effects by reducing hospital admissions; remote monitoring of simple parameters (blood pressure, heart rate, body weight) can anticipate an occurring destabilization of the patient with heart failure, and, when followed by changes in drug therapy, reducing re-hospitalizations.3,4
Remote monitoring of heart failure patients with ICDs/CRT-Ds significantly reduce long-term mortality in a real-world clinical condition, 2.1% vs. 11.5% 1-year mortality (P < 0.0001), also maintained during a 3-year follow-up (4.9% vs. 22.3%, P < 0.0001).5 In other studies, the use of healthcare resources was significantly reduced by remote telemedicine monitoring as a result of a marked reduction of in-office visits without compromising patient safety.6
Transmission of data and images between different centres has become routine in radiology, but also very common in cardiology, in particular for ‘second opinion’ consultation.
Tele-echocardiography may guide treatment, reduce long and potentially risky transports, and triage transports to destination centres with the most appropriate cardiac capabilities.7 In case of neonantes with suspected congenital heart disease, transfer to the regional unit was avoided in 72% of patients thanks to remote second opinion consultation with tele-echocardiography.8 More and more fields in cardiology are interested by progress in telemedicine.
Telemedicine in cardiovascular emergencies: acute myocardial infarction and acute coronary syndrome
ST-elevation acute myocardial infarction
The guidelines of the European Society of Cardiology (ESC) on the treatment of STEMI recommend primary angioplasty (pPCI) as the preferred treatment strategy when performed in due time. The maximum benefit is obtained when the reperfusion is achieved in the first 3 h of symptom onset. The delay due to the health care system can be reduced if there is a network between spoke hospitals by which the patient is promptly transferred to a hub centre for pPCI, an efficient transfer service by ambulances, if the cathlab can be activated by ‘en route’ ambulance. Therefore, early diagnosis of STEMI, which is possible with pre-hospital 12-lead electrocardiogram, can greatly reduce the time of treatment, by-passing any delay through the emergency department. The time indicated by the guidelines as optimal for pPCI from first medical contact is 90 min (acceptable a 120-min delay).
ST-elevation acute myocardial infarction networks
A network for the efficient treatment of STEMI should be characterized by:
a clear definition of the geographic areas covered by the service;
protocols for the transport, by ambulance or helicopter, equipped with 12-lead electrocardiogram, remote transmission of the electrocardiogram, defibrillator and at least one health care (doctor or nurse) expert in advanced life support;
possibility to transfer the patient for pPCI with a transfer time <60 min
cathlab activation while the patient is en route
availability of the cathlab staff within 20 min of calling
patient’s direct transport directly to cathlab by-passing the emergency department
in case of access in a hospital without pPCI capability, electrocardiogram within 10’and, in case of confirmed diagnosis of STEMI, transfer to hub for pPCI within 30’, if the travel time is less than 60’, otherwise fibrinolysis.
The hub-spoke organizational model for the management of STEMI reduces the delay to treatment and increases the rates of patients who receive reperfusion treatment within benchmark time. In any STEMI network, each time interval should be monitored to enable actions aimed at performance improvement and delay reductions.
The public decision-maker involvement is essential for the optimization of resources and to resolve conflicts in management (automated, paramedic, emergency physician, or interventional cardiologist interpretation of the electrocardiograms Hub cathlabs position through the country).
Non-ST-evaluation acute myocardial infarction and unstable angina
The ESC 2015 guidelines for the management of patients with NSTE–acute coronary syndrome (ACS)9 recommend in patients with chest pain:
The execution of 12-lead electrocardiogram within 10 min of first medical contact and its interpretation. Therefore, even if the network for NSTEMI management is not, with some exceptions, time-dependent, pre-hospital electrocardiogram is however required: the STEMI network can be used also for patients with NSTE–ACS.
Only cases with very high-risk criteria (haemodynamic instability or shock, refractory angina to medical therapy, cardiac arrest or life-threatening arrhythmias, acute heart failure, mechanical complications of infarction, transient ST changes, especially if ST-elevation) should be referred to the hub centre where angioplasty should be performed within 120 min.
In other cases, which are the majority, there is time to decide which is the best treatment, as it must also take account the ischaemic risk of bleeding and comorbidities. In any case, the patient should be admitted to a cardiology ward, as close as possible (not necessarily the hub centre), to where electrocardiogram monitoring is possible (in the cardiology care unit (CCU) or just telemetry depending on the clinical severity).
If, by evaluating the risk/benefit ratio, it is considered appropriate to perform a revascularization, this should be done within 24 h, even transferring the patient to the hub centre for the PCI, and returning at the centre spoke after the procedure, if not complicated.
Telemedicine in arrhythmic emergencies
The applications of telemedicine have been classified into three categories in relation to the place where the service is carried out: pre-hospital, in-hospital, and post-hospital. In all these areas it is possible to identify potential uses of telemedicine in the management of arrhythmias.
Pre-hospital
Pre-hospital electrocardiogram directly interpreted or transmitted for telediagnosis may be extremely useful for the management of severe arrhythmias, allowing for immediate intervention or patient’s admission in the most appropriate structure. Several studies have demonstrated the feasibility of using a 12-lead electrocardiogram in pre-hospital setting.10–13 Good quality diagnostic electrocardiograms are transmitted with a success rate of 85%.14
In-hospital
In-hospital telecardiology is often used for electrocardiogram sharing between different departments or between peripheral hospitals to central hospitals.15–17 The diagnostic quality of the images sent and received through the use of telemedicine has proved to be very high.
Post-hospital
The post-hospital management of patients with arrhythmias can be articulated in two points: the teleconsultation between general practitioners and specialists, the use of telemedicine in chronic cardiovascular disease. General practitioners can access via telemedicine specialist tele-diagnosis of a 12-lead electrocardiogram, concurring in real time the best treatment for the patient.
Remote monitoring of implantable cardiac devices has proven to be extremely important in the diagnosis of atrial fibrillation, particularly silent. In patients with defibrillators capable of remote monitoring (TRUST trial), the recognition of atrial fibrillation occurred with 34.5 days in advance18; in another population of pacemakers with daily monitoring (COMPAS trial), the incidence of hospitalizations for atrial arrhythmias and stroke proved by 7.3% in the control group and 2.4% in the remote monitoring group with an incidence of stroke of 3.3% and 0.8%, respectively.19
On the other hand, in case of episodes of tachycardia and ventricular fibrillation with or without shock delivery, remote monitoring of ICD allows a ready assessment of appropriateness and effectiveness of the therapy delivered. It is therefore possible, with an individualized management of the event, avoiding unplanned and unnecessary emergency room or clinic access.
Telemedicine for the reduction of time to treatment: supporting evidence
First studies on the pre-hospital electrocardiogram transmission from ambulances, aimed at the activation of cathlab for primary angioplasty in AMI, now back in the late 90’s.20–21(Table 1) Data from non-randomized studies show that patients with AMI and pre-hospital telemedicine diagnosis are treated in a shorter time than patients whose diagnosis is performed in the hospital, either in case of direct access to a hub centre or to a spoke centre22 (median 41 mins less, in the 81st s). The transmission of a pre-hospital 12-lead electrocardiogram directly to the cardiologist by mobile phone is able to reduce the door-to-balloon time of about an hour [34 vs. 97 min (median)].23 This diagnostic approach is associated with a time between first medical contact and angioplasty of 74 min (median) in contrast to 127 with traditional approach without telemedicine.
Table 1.
Reduction of time to treatment of acute myocardial infarction thanks to pre-hospital electrocardiogram by telemedicine
| Study (authors) | N (telemedicine vs. controls) | Time interval | Differences | Relative reduction |
|---|---|---|---|---|
| Terkelsen & al. | 21 vs. 85 vs. 55a | Call-to-balloon | 87 vs. 168 min | −48% |
| Sejersten & al. | 146 vs. 89 | Door-to-balloon | 34 vs. 97 min | −65% |
| Call-to-balloon | 74 vs. 127 min | −42% | ||
| Sorensen & al. | 460 vs. 83 vs. 216a | Call-to-balloon | 92 vs. 153 min | −40% |
| Brunetti & al. | 123 vs. 174 | ECG to balloon | 41 vs. 94 min | −56% |
| Optimal time perfusion rate | 85% vs. 35% | +143% | ||
| 69% vs. 29% in rural areas | +138 | |||
| Pedersen & al. | 616 vs. 821 | Door-to-balloon | 83 vs. 103 min | −19% |
| 61% vs. 36% | +69% | |||
| Chan & al. | 167 vs. 427 | Optimal time perfusion rate | 80% vs. 9% | +789% |
| Zanini & al. | 136 vs. 263 | Total time to balloon | 148 vs. 262 min | −43% |
| Sanchez-Ross & al. | 92 vs. 50 | Door-to-balloon | 63 vs. 119 min | −47% |
PCI, percutaneous coronary intervention.
Triage by telemedicine and direct transfer for PCI vs. triage with telemedicine without direct transfer vs. traditional triage without telemedicine.
The diagnosis by pre-hospital electrocardiogram and direct transfer to cathlab enable patients with STEMI who live far from a hub centre performing primary PCI and or in rural areas to be treated with an angioplasty within times comparable to that of patients who live in close proximity to a centre with primary angioplasty. In 750 patients with STEMI enrolled in a Danish registry, subjects with pre-hospital diagnosis by telemedicine in rural areas and direct access in cathlab had a treatment time of 92 min (median) compared with 153 subjects without pre-hospital diagnosis: those from rural areas, despite traveling longer distances [further 30 km (median)], had treatment times only 9 min longer than those from urban areas.24
In an Italian registry on over 27 000 patients screened with pre-hospital electrocardiogram by telemedicine, almost 50% of patients with STEMI received a diagnosis within 30 min of symptom onset.25 More recent data from the Apulia emergency medical service (EMS) (1-1-8) registry on pPCI for STEMI show times from pre-hospital electrocardiogram to primary angioplasty of 41 min (mean) vs. 1 h and 34 min in subjects not triaged by telemedicine, with a relative time to treatment reduction of 56%: the relative reduction is 49% even in areas distant from cathlabs.26 Thanks to the pre-hospital diagnosis by telemedicine the rates of subjects with time from diagnosis to treatment <1 h rose from 29% to 69% in ‘remote’ areas (+138%) and from 35% to 85% in the whole population observed (+143%). In another Danish registry on almost 1500 patients with STEMI, patients with pre-hospital triage by telemedicine were characterized by door-to-balloon times of 83 min (median) compared with 103 of the ‘controls’: the times <90’ were achieved in 61% of subjects in the telemedicine group vs. 36% of others.27 With transfer distances likely to be greater, in British Columbia, pre-hospital triage by telemedicine has been able to increase the percentage of patients with door-to-balloon <90 min from 9% to 80%.28 Data from the US National Register on STEMI (more than 50 000 patients) show door-to-balloon times of 94 min in case of pre-hospital triage against 110 of ‘control’.29
Immediate screening with pre-hospital electrocardiogram can reduce the false negative rate in cases of STEMI with atypical presentation.30 From a clinical point of view, moreover, the early assessment and pre-hospital triage of patients with STEMI using telemedicine reduce the time door-to-balloon, the infarct size, impaired ejection fraction and subsequent duration of hospitalization.31 The pre-hospital triage by telemedicine is in fact able to impact significantly also on the endpoint mortality. A dramatic 60% reduction of early and late mortality associated with the use of pre-hospital electrocardiogram by telemedicine was observed in registries on AMI28; pre-hospital triage is thus an independent predictor of survival at 1 year (hazard ratio: 0.37). Even a modest increase in the rate of subjects with call-to-balloon <90 min (28% vs. 21%) was associated in a large population of almost 290 000 patients with a significant reduction in 30-day mortality (7.4% vs. 8.2%) of patients with acute coronary syndrome (STEMI and NSTEMI).32
Even data from meta-analyses show a 0.65 relative risk of intra hospital mortality for AMI in the case of pre-hospital diagnosis by telemedicine compared with standard treatment.33 Data from a recent meta-analysis of 14 randomized trials of approximately 4400 patients with STEMI show that pre-hospital triage and direct transfer are associated with a reduction in 30-day mortality of 42%.34
The use of pre-hospital electrocardiogram by telemedicine in a network for the treatment of STEMI has been already implemented in different areas of Italy35–37 and in the world,38,39 with optimal results. In an Italian provincial network for the treatment of STEMI, treatment times were significantly reduced in the group using telemedicine diagnosis compared with controls 148 ± 81 min vs. 262 ± 112.37 Reducing the time of treatment seems to significantly affect the prognosis, especially in patients with increased risk of complications and more unstable medical conditions, cardiogenic shock,40 more comorbidities,41 more severe Killip class.36
Telemedicine and cardiovascular emergency networks in Italy
Several networks for cardiovascular emergencies with telemedicine support, mainly based on 12-lead pre-hospital electrocardiogram, have been implemented so far in Italy. The Italian Ministry of Health and the Superior Council of Health set in 2010 a working group for telemedicine in order to have a shared governance model and harmonized models of implementation.42 The working group followed prior experiences43 and aimed to build a map of the networks to facilitate the exchange of best practices and organizational models. Each model in the system is described in its general characteristics, the type of service, the scope, and the state of the project, the technology used and the geographical area. The telemedicine projects for cardiovascular emergency, reported on the www.onecare.cup2000.it site are reported in Table 2. The projects, mainly based on four types of organizational models, are shown in Figure 1. All telemedicine emergency models are characterized by a spoke, sending an electrocardiogram, the EMS (in Italy 1-1-8) and a hub receiving the electrocardiograms (a cardiology ward/CCU or 118 dispatch centre). In one case, the hub is represented by a dedicated telemedicine centre with cardiologists experienced in interpreting pre-hospital electrocardiograms other than a cardiology ward/CCU.
Table 2.
Telemedicine experience on cardiovascular emergency reported on the national Ministry of Health website www.onecare.cup2000.it (1 November 2015)
| Region | Project | Area | Descrizione | Connectivity | Tools |
|---|---|---|---|---|---|
| Basilicata | TELESAL | Region | Satellite communication technologies to improve or enable telemedicine applications and services | Satellite | |
| Rete cardiologica SCA | Region | Avoid unnecessary hospitalization, enable early pharmacologic treatment of acute myocardial infarction, primary angioplasty, thrombolysis, prevention of heart failure | GSM | Lifepak 12 Medtronic | |
| Campania | Sistema di Telecardiologia in emergenza | City of Benevento | Activation of telediagnosis for patients with suspected AMI, triaged at emergency department and mobile stations; the goal is to record a pre-hospital standard electrocardiogram (12-lead) immediately, transmitted to a telemedicine hub, with the aims of an early diagnosis, a timely treatment, and a fast transfer | Telephone line | Monitor ECG/defibrillator |
| UMTS/GPRS | |||||
| Progetto per la diagnosi, trattamento precoce e trasporto assistito presso strutture specializzate del paziente con patologie cardiovascolari acute ai fini della riduzione della mortalità preospedaliera | City of Avellino | EMS electrocardiogram sent to Ariano Irpino CCU. | Telephone line | ||
| Emilia Romagna | Trasmissione telematica di ECG verso l'Unità Terapia Intensiva Coronarica dell'Azienda Ospedaliera di Reggio Emilia | City of Reggio Emilia | The telemedicine hub located in the Azienda Ospedaliera Arcispedale Santa Maria Nuova enable the on-duty 24/7 cardiologist to confirm the diagnosis of STEMI eligible for primary PCI. | UMTS/GPRS | Lifepak 12 |
| Gestione Emergenza Extra-Intraospedaliera | City of Forli’-Cesena | Condirmation of STEMI diagnosis | UMTS/GPRS | ||
| Piemonte | S.C. Servizio emergenza sanitaria territoriale 118 Provincia di Alessandria | Region | Since 2011 transmission of 12-lead ECG and clinical data from EMS ambulance to dispatch centre and from this to cathlab for primary PCI | UMTS/GPRS | Mobimed Ortivus |
| Puglia | La Telecardiologia per il 118 nella Regione Puglia | Region | Pre-hospital 12-lead electrocardiogram to a single telemedicine hub with dedicated cardiologists active 24/7 for pre-hospital diagnosis of cardiovascular emergency, STEMI and cathlab alert for primary PCI | Telephone line | CardioVox P12 |
| UMTS/GPRS | |||||
| Sicilia | Telecardio SEA Project | City of Trapani, Egadi Island, Pantelleria | Pre-hospital diagnosis of STEMI and arrhythmias | Electrocardiograph, blood pressure, and saturation data transmission | |
| Toscana | Telelettura ECG in emergenza territoriale da parte della centrale 118 | District of Florence | Pre-hospital ECG (nurses) transmitted and diagnosed by cardiologist in CCU | Broadband | |
| Percorso diagnostico terapeutico dell’Infarto Miocardico Acuto | City of Massa Carrara | UMTS/GPRS | |||
| STEMI: trattamento dolore toracico acuto non traumatico | City of Lucca | ECG transmission to EMS dispatch centre and CCU of Versilia Hospital | Telephone line | ||
| UMTS/GPRS | |||||
| 118 Cuore | City of Empoli | Telephone transmission to CCU of ECG | UMTS/GPRS | ||
| Progetto pilota di teleconsulto su mezzo mobile | City of Prato | TelediagnosisTeleconsultation | Satellite | Electrocadiograph and Videocamera | |
| Gestione telematica delle emergenze coronariche per l'attuazione preospedaliera della Trombolisi Sistemica | PIstoia | Pre-hospital ECG transmission to CCU and pre-hospital fibrinolysis. | UMTS/GPRS | ||
| Collegamento Auto Medica 118-Centrale Operativa | Siena | Teleconsultation between EMS dispatch centre and ambulances | UMTS/GPRS broadband | Defibrillator/monitor, multichannel router, PC. | |
| Bluetooth | |||||
| Rilevazione e refertazione di ECG nel Carcere di Sollicciano | Prison of Sollicciano | Remote electrocardiogram transmission and interpretation | GSM | electrocardiograph, blue tooth and laptop. | |
| Data are transmitted to Torregalli Hospital as PDF and after to a hub in Florence | |||||
| Umbria | Trattamento Ottimale della Sindrome Coronarica Acuta (TOSCA) | Part of Umbria | Teleconsultation between EMS ambulances and CCU of Perugia | UMTS/GPRS | |
| Valle d’Aosta | Partout Sanita’ - E-refuge | Region | Video conference and data-transmission from Alpine shelters for teleconsultation (EMS, CCU) | UMTS/GPRSBluetooth | |
| Partout sanita’—video/telepresenza | Region | Video conference for EMS | UTMS/GPRS | ||
| STEMI | Region | Network for online read of ECGs | Defibrillator/monitor, electrocardiograph, blood oxygen |
PCI, percutaneous coronary intervention; STEMI, ST-elevation myocardial infarction; EMS, emergency medical service; CCU, cardiology care unit.
Figure 1.
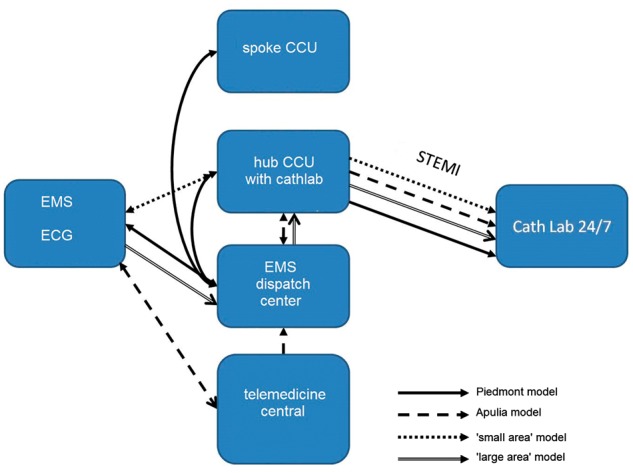
Model of telemedicine network for cardiovascular emergency report on website www.onecare.2000cup.it (1 November 2015).
The Piedmont regional model is the most complex: the electrocardiogram of a suspected STEMI is transmitted by the 118 ambulance crew to a dispatch centre, where, in case of suspected STEMI, it is forwarded to the closest CCU, which decides for cathlab activation.44
The Apulian regional telemedicine model instead provides 12-lead electrocardiogram transmitted by EMS ambulances to a telemedicine dispatch centre operated by experienced cardiologists in electrocardiography, which return the correct diagnosis, leaving the EMS responsible for direct transfer for pPCI.
In local networks of territories covered by a single cathlab 24/7, as for example in the nearby of Massa Carrara, the model is much simpler and consists of the direct transmission of 12-lead electrocardiogram to the only CCU/cathlab hub covering the area that, after diagnosis, receives the patient with STEMI (Figure 1).
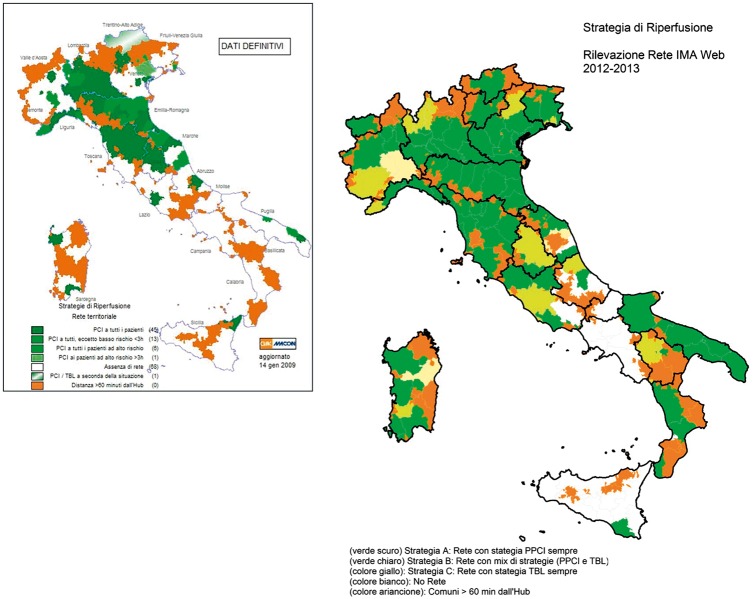
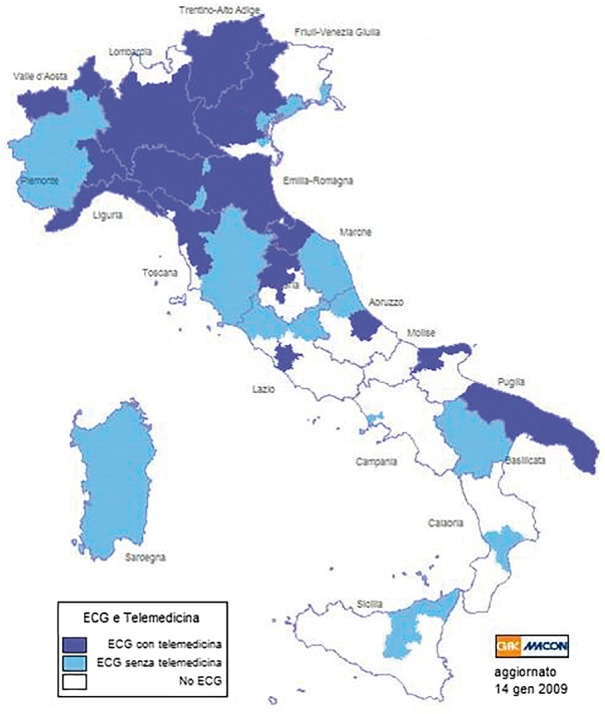
Two surveys conducted respectively in 2006–2008 and 2012–2013, with the support of the Italian Interventional Cardiology Society GISE and Stent-for-Life initiative, took a snapshot of current management of STEMI in Italy45–47 (Figures 2 and 3).
Figure 2.
Pre-hospital 12-lead electrocardiogram 12 (IMAWeb 1 survey 2006–2009).
Figure 3.
Reperfusion strategies in Italy according to IMAWeb 1 2006–2009 (left) and 2012–2013 (right) survey.
Professional profiles and organizational models
Devices for electrocardiogram transmission
In recent years, the concept of network as groups of professionals who work in a coordinated manner, to ensure equitable provision of effective, ‘high-quality’ services48 has been progressively implemented in health systems, becoming an organizational model able to provide effective solutions for the optimal management of the complex patient and to enhance the action of interdisciplinary professionals.49,50
For these reasons, the network model, which integrates emergency EMS with hospitals with different levels of care, represents the standard of care even more for the treatment of acute time-dependent disease, by ensuring equal access to procedures and using diagnostic and therapeutic strategies shared and modulated on both the patient’s risk profile and on the structural and logistical resources available.
This document therefore aims to describe a telemedicine-system-model that pursues and achieves the objectives of the network model, with the most advanced and innovative organizational models. In spite of a large implementation of networks for STEMI, there are still a number of problems that require improvement actions in terms of ‘maintenance’ of the network, standardization, and facilitation of clinical pathways. Despite the implementation of information systems with fast connectivity, there are still existing problems that mainly consist of:
still suboptimal implementation of the fast track paths (EMS-cathlab);
improvable timing between first medical contact and cathlab admission;
delays in the time to balloon of patients with STEMI accessing the network through spoke centres.
It should be considered that the network could and should be extended also to other time-dependent diseases such as NSTE–ACS, acute aortic syndromes, cardiac arrest and severe acute heart failure.
New frontier of telemedicine applied to networks for cardiovascular emergencies also intends to pursue the following objectives:
to identify and implement clinical and organizational requirements essential to guarantee the quality of care provided by the network, also with regards to accreditation;
to define the parameters for the monitoring and the improvement of the network performance;
to optimize the diagnostic and therapeutic pathways for the cardiovascular patient, encouraging the early diagnosis with the use of digital systems for remote transmission of electrocardiogram and tele-consultation with hub centres;
to rationalize the use of resources by avoiding duplication of services and ensuring respect for the principles of inclusiveness and distinctive vocations of the hub centres;
to encourage the development and maintenance of ‘clinical competence’ based on minimal activity requirements in terms of volume per operator and per hospital as defined by international benchmarks;
to promote a network system of governance, which integrates each hospital involved in the network;
to extend the network activities to other urgent cardiovascular diseases such as NSTE–ACS, acute aortic syndromes, cardiac arrest and acute heart failure.
Organizational models
State of the art and advanced application in telemedicine
Acute myocardial infarction with ST-segment elevation
Clinical, instrumental, and organizational recommendations
direct transfer to the hub by direct EMS activation
correct treatment even before hospital admission by remote transmission of pre-hospital 12-lead electrocardiogram, preferably with digital devices, to a dispatch centre where the electrocardiogram diagnosis can be confirmed by skilled operators (Tables 3 and 4).
direct access to the cathlab possibly with fast-tracks by-passing emergency room or CCU;
pre-hospital treatment, pharmacological and non-pharmacological, for EMS crews operating in remote areas far from the cathlab;
correct and timely diagnosis of STEMI in emergency room by seriate 12-lead electrocardiogram monitoring and automatic electronic sharing of diagnosis and treatment with the CCU cardiologist;
immediate transfer to cathlab for STEMI patients directly accessing the network through spoke emergency rooms;
preferentially hospitalization in cardiology wards;
inter-hospital transfers in the most homogeneous ways throughout any region network;
appropriate drug prescription at discharge;
follow-up after discharge.
Table 3.
Management, administration, and system service modules
 |
Log and security | |
| Module including all the application security functions such as authentication and user profiling, and the users' tracing and access logs function | ||
| Requirements | Authorization system through user profiling and definition of distinct privileges for profile | |
 |
Configuration and encodings | |
| Module collecting all the management functions of the encoding tables and registers necessary for the application system | ||
 |
Reporting | |
| Drawing, execution, and publication of the reports (both standard and custom) component used by the process modules of the application system | ||
Table 4.
Process’ modules
 |
Process manager (process workflow) | |||
| It is the module of coordination and cooperation of the other modules, which implements the process workflow by addressing the reporting and patient transport requests according to dispatch centres’ resources. It also includes the applicative cooperation layer with external systems. | ||||
| Availability of an appropriate application designed to determine the most suitable dispatch centre | ||||
| Re-addressing function of reporting requests, with activation of the alert system, in the case of transmission of the application to the competent dispatch centre error | ||||
| Ability to interface with external systems via standard HL7 protocol | ||||
 |
Intervention management in emergency cardiology | |||
| The module containing the functions dedicated to the health emergency personnel. It allows the collection of all data required for the subsequent assessment, including the instrumental data through two components of managing and interfacing electrocardiograph and defibrillator; it links data to the EMS ID code | ||||
| Requirements | Ability to acquire ECG and EMS ID Code wirelessly transmitted by electrocardiographs/ defibrillators monitor | |||
 |
Repository of data and reports | |||
| Data and documents collected or produced during the process management module. It allows the storage, classification, research, and publication of data and documents, using competence and profiling criteria, previously configured, to regulate the access by users | ||||
| Requirements | Storage capacity, and online management of at least 1 000 000 ECG in high definition on at least 12 leads | |||
| ECG and report display and print function on the client systems of the dispatch centres | ||||
| Digital archiving of the report and ECG | ||||
| Ability to store more ECG (with related reports) relating to the same emergency event (the same EMS ID code) | ||||
| Ability to search in archives the ECG and the related reports according to the EMS ID code | ||||
 |
Reporting and analysis dashboard | |||
| Framework in which functions and components dedicated to the analysis of clinical data and the production of the report digitally signed document are accessible. It manages the work lists of the dispatch centre and transmits the alarm signal. It uses of components dedicated to ECG analysis, the signature, reporting | ||||
| Requirements | Possibility of reporting from multiple stations simultaneously | |||
| Ability to process adult ECG | ||||
| Ability to process paediatric ECG | ||||
| Availability of an alarm system alerting the dispatch centre responsible for the ECG | ||||
| deactivation of the alert system after request processing by the competent dispatch central; ability to generate the report with date and time of request receipt tracking | ||||
| Capacity of digital or electronic report signature | ||||
| Management of reports’ state: ‘Waiting for processing’; ‘in process’ or ‘processing completed’ | ||||
| Output data format DICOM, XML, PDF | ||||
| All modules must comply with the following requirements | ||||
| Requirements | Web-based architecture: application access via the web, through the major market browsers | |||
| Online download for accessory applications for the remote computer's configuration | ||||
 |
Clinical decision support system | |||
| After acquisition and of medical history, patient’s vital and instrumental data, DSS suggests activities, therapeutic pathways and information in accordance with approved protocols and literature validated at international level, both for the operator of the emergency network and for the reporting cardiologist, early diagnosing cases of STEMI/NSTEMI. | ||||
STEMI, ST-elevation myocardial infarction; NSTEMI, non-STEMI; DSS, decision support system; EMS, emergency medical service.
Electrocardiogram and pre-hospital diagnosis of acute myocardial infarction
The EMS should be staffed with personnel able to perform a 12-lead electrocardiogram. The telematic destination of en-route electrocardiogram should be always known in advance, according to the different clinical and electrocardiogram settings (STEMI, NSTEMI, cardiac arrest, tachy-arrhythmias, brady-arrhythmias) and capabilities of network facilities (Cardiology wards, CCU, cathlab). The electrocardiogram tele-transmission and the availability of clinical data and medical history collected on site allow the cardiologist in the dispatch centre to confirm the diagnosis, in agreement with EMS ambulance staff.23,36,51–54 In case of uncertain diagnosis but with reasonable suspicion of STEMI or equivalent syndrome (typical pain without persistent ST-segment elevation or atypical pain and ST borderline anomalies), direct transfer for coronary angiography should be organized.
Referral centres and direct referral paths
Any network protocols must clearly identify the referral cathlab where EMS ambulance should transfer subjects with suspected ACS. The same protocol should be followed for patients with STEMI accessing the network through emergency rooms or spoke hospitals.
Agreement protocols between EMS, spoke and hub hospitals must include times, means and staff required for each step in the management of the patient. A telemedicine system is capable of tracking each phase of the process.
Emergency room
Direct presentation to the nearest emergency department is another modality to access the STEMI network. In a telemedicine model-system EMS automatically provides for a rapid transfer to cathlab (Figure 4 and Table 5).
Figure 4.
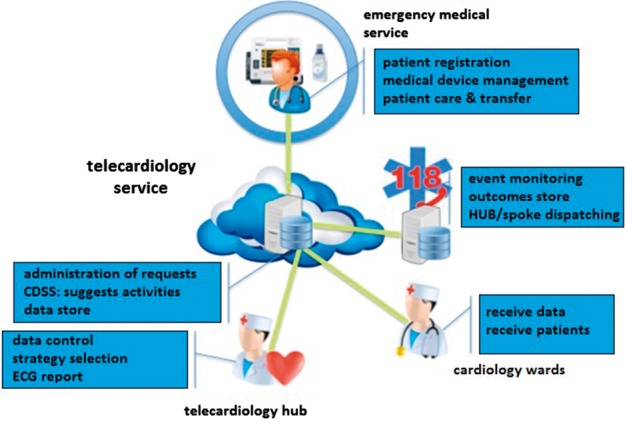
Organizational telemedicine model for cardiovascular emergency.
Table 5.
Telecardiology and urgent care centres of the hub-and-spoke
|
STEMI, ST-elevation myocardial infarction; EMS, emergency medical service.
Cathlab
The cathlab (Table 6) represents a crucial point in the diagnostic evaluation and treatment because it is there that primary angioplasty is performed (Table 4). The hub cathlab must provide a 24/7 availability, have adequate instruments and staffing in accordance with the regional accreditation criteria and the recommendations of the national consensus documents,55 and access to telemedicine systems by accredited profile credentials. The cathlab team should be automatically alerted by the telemedicine system soon as the diagnosis of STEMI is made.
Table 6.
The telemedicine and the haemodynamic laboratories of hub centres
|
The parameters specified as a standard of activity are monitored through indicators derived from administrative or clinical databases. The analysis of such parameters could be further useful for regional health care planning as representative of the quality of care.
Cardiology care units
The CCU of the hub centres have to manage patients with STEMI after treatment with primary angioplasty, awaiting the activation of the cathlab, as well as those for which PCI reperfusion is not feasible (late arrival, patient refusal, contraindications to anticoagulant and antiplatelet therapy, lack of arterial access, etc.).
Acute myocardial infarction without ST segment elevation, and unstable angina
Clinical and organizational recommendations
The telemedicine system-model should monitor and ensure preferentially, but by automatic protocol, hospitalization in a cardiology ward;
provide the patient with ACS and moderate risk of ischaemic events performing a coronary angiogram within 72 h of presentation at the hospital;
ensure the patient with ACS and high risk of ischaemic events performing a coronary angiogram within 24 h of presentation at the hospital;
facilitate and promote transfers between hospitals;
Indicators and measurable standard with an advanced telemedicine system
The following list represents the set of indicators and reference standards that will serve as a reference for performance evaluations of health facilities and the planning of any audits and corrective actions. The telemedicine system model records and automatically analyses the indicators.
STEMI
Reperfused/STEMI patients
Primary angioplasty/thrombolysis
Primary angioplasty <120’
Primary angioplasty/patients in patients with cardiogenic shock
Timing of diagnosis and treatment (early pain/ECG/reperfusion)
Access by EMS/patients presenting to the emergency room
False positives sent from EMS to cathlab
False negatives sent from EMS in emergency department
Inpatients (CCU/ICU/other)
Length of stay
In-hospital mortality
Mortality at 30 days
NSTEMI–ACS
Number and standardized rate of hospitalization per 100 000 inhabitants
Patients treated with angioplasty within 3 days out of the total of NSTE–ACS patients (>70%)
Patients admitted to the spoke and never sent to hub (<25%)
Patients admitted to spoke, re-sent to a spoke (post-acute) after passing through a hub (>95%)
Patients admitted to the cardiology department (>90%)
Length of stay in the CCU and full hospitalization (2 days and 7 days)
-
Proper drafting of the discharge letter (>90%)
Clinical and prognostic assessment with indications for life-style changes
Planned outpatient controls
Drug therapy
Drug prescription at discharge
In-hospital mortality/cardiology ward (<8% and <4%, respectively)
Mortality at 30 days
Security management
The security module typically contains a diffuse pattern identified by the triple A, which is the size AAA—authentication, authorization, and accounting.
Signal transmission requirements
All electrocardiograms should follow the guidelines for the electrocardiogram standardization56 and comply with bandwidth of at least 0.05 up to 150 Hz.
Training
The telemedicine for cardiovascular emergency requires skills that are often not part of the know-how of the clinical cardiologist. Different training required for tele-diagnosis of electrocardiogram depends crucially on to who this task should pertain. 2010 ILCOR guidelines stated the possibility for lay people adequately trained to access electrocardiogram tele-recording systems.57 In this specific situation, in the presence of lay or non-medical individuals, the training must be focused on the execution of a maximally standardized recording, with positions of the peripheral and precordial electrodes on anatomical landmarks and simple devices. Many of the devices available also allow an automatic interpretation in line with the existing conventions with good specificity.58 It appears however inadvisable to encourage the use of the only automatic interpretation of the electrocardiogram, unless in the absolute impossibility of obtaining an expert-opinion, even at a distance.
Lay personnel training should comply to teaching methods issued by scientific societies (ILCOR, ANMCO, ESC, ERC, AHA), should include theoretical sessions, showing opportunities and criticalities (privacy and consent to the procedure), and at least a practical training session, supervised by expert trainers. Local protocols should be developed on specific territorial needs.
The nursing staff should be trained, not indeed in electrocardiogram recording, which is part of the usual nurse skills, but in the management of patients in the absence of direct medical care. The nursing staff can be given simple and interpretive information, as widely standardized in ACLS training methodologies of the American Heart Association ALS or ERC.
Effective models for distance education via e-learning allowing the goals required with a minimum occupation of time have been therefore developed, also to reduce cost of education.49
Regulatory issues
The regulatory assessment regarding telemedicine and emergency network needs to be addressed separately since the two aspects have a completely different regulatory framework. In fact, while for telemedicine there is a National legislation which regulates principal aspects, emergency networks are normed by national guidelines and several regional deliberations. The State-Regions agreement of 20 February 2014 regulates the matter and aims to harmonize purposes and applications of telemedicine models, as a prerequisite to interoperability of services. The memorandum of understanding enounces principles and requirements for accreditation and operability of telemedicine centres.42 The document refers to classical aspects of the patient’s informed consent and the processing of personal data. However, the use of telemedicine in cardiology is mainly focused on patients in imminent risk of death and, therefore, the obtaining of consent is a marginal issue. Much more important aspects, instead, from a regulatory perspective, are represented by the responsibility for diagnosis or therapeutic approach, the problems related to the malfunctioning of the computer system, the confidentiality of information.
Professional liability in telemedicine
Telemedicine revolutionized the classic relationship between doctor and patient and introduced more actors and more places: from this point of view, then the professional responsibility does not fall only on the physician interpreting the remote electrocardiogram, but also on the operator recording the electrocardiogram. From this point of view, then the profiles of professional liability cover not only the inadequate professional training in the use of the devices but also the inadequate supervisory action on the presence of device and system malfunctions that are not reported. There are therefore two further types of negligent attitude: ‘Culpa in Vigilando’ that is the fault of those who omit a necessary control action, and ‘Culpa in Eligendo’, that is the fault of those who do not properly follow the operating procedures. Then there are the responsibilities attributed to the manufacturer of the health equipment used and the responsibilities attributed to those who are using the equipment with lack of maintenance or incorrect use thereof. In general, the physician who interprets the electrocardiogram or the images is responsible for the error related to the interpretation of the data, while the sender is responsible for an erroneous or misleading transmission. It’s important to note, however, that if the physician who interprets is aware of impaired quality of the data, he is also responsible for any mistake, regardless of the quality of the transmission. If the delay in the transmission of data, or alteration of the data transferred confer an injury to the patient, in the context of a network management, levels of responsibility should be determined. In this respect, it is necessary to identify a Director of telemedicine service, who is responsible both for the selection of medical staff and the control of its employees. Obviously, the Director can’t be informed of any act that is done by the team and therefore, as established by the Supreme Court, the Clerk’s responsibility is not unlimited. (Cassaz. Civ., 16 May 2000, n. 6318). Moreover, as telemedicine implies a relationship not only between patient and physician but also with another provider (doctor or nurse) who, from a distance, records an electrocardiogram, it is mandatory to refer to the principle of ‘reliance on’, whereby each operator is required to monitor the work of colleagues being remedied for errors, regardless of role. In the present case, therefore, during the transmission of an electrocardiogram, all actors involved are required to assess the possibility of error on the part of colleagues, regardless of the role they play.
Procedures and guidelines
Internal procedures are required to adapt international guidelines to local networks and technological resources. It’s important that internal procedures clearly identify proper individual roles (who should do it), the skills of each team member (who does what) and the correct mode of execution (how it should be done), in order to avoid gaps in protocol indications or conflicting activities. Internal protocols complying to international guidelines improve patient safety and also prevent unpleasant legal consequences.
Privacy in telemedicine
The obligation to respect the privacy pertains to telemedicine in the same way as any other field in medicine, with some variants. The legislation refers to the 31 December 1996, n. 675 act (Protection of persons and other subjects regarding the processing of personal data) and subsequent amendments and additions and the Legislative Decree 30 June 2003, n. 196 (Code on the protection of personal data) articles 75–94 referring to ‘Privacy in healthcare’. In telemedicine, protection of data electronically managed and of databases containing personal health data should be carefully pursued (Table 7)
Table 7.
Regulatory aspects telemedicine
|
National law for emergency networks and regional statements
In the field of networks for emergency, the latest regulations issued by the Ministry of Health is represented by the 2 April 2015 Decree No. 70 entitled ‘Regulation defining the quality, structural technological and quantitative standards for hospital care’ published in the Official Gazette of 24 September 2015. The regulation in Section 8 defines the characteristics of the ‘Network for Emergency Cardiovascular Care’ indicating the network and the current standard of care for STEMI. The document also provides explicitly the possibility of support by telemedicine for STEMI networks.
Besides national statements, regions, with diverse levels of complexity and state of progress, have produced regional resolutions that regulate in detail the formation, characteristics and areas of responsibility of networks for emergency in cardiology.
Model frequently used in emergency telecardiology service with the required functionality in a modern information system for the management of a telecardiology service (Figure 4).
The staff of the Network acquires the personal and clinical data of the patient and manages medical devices (portable electrocardiograph/defibrillator) in order to allow cardiologists in the telemedicine central interpretation of electrocardiogram and diagnose. EMS dispatch centre directs the staff. A single regional central for EMS and telecardiology service providing the application of services to all actors and mediate communications between them. The identification of cases handled is generally based on the unique code assigned by the EMS.
Inside the telecardiology service, appears important in perspective the innovative function of a clinical decision support system (CDSS) both in phase of emergency intervention and in the evaluation phase. The CDSS, through instruments of guidance and management of the workflow, might help the Territorial Network staff to reduce errors and to codify the outcome of an event as quickly as possible.
Consensus Document Approval Faculty
Abrignani Maurizio Giuseppe, Alunni Gianfranco, Amodeo Vincenzo, Angeli Fabio, Aspromonte Nadia, Battistoni Ilaria, Bianca Innocenzo, Bisceglia Irma, Bongarzoni Amedeo, Cacciavillani Luisa, Calculli Giacinto, Capecchi Alessandro, Caporale Roberto, Caretta Giorgio, Carmina Maria Gabriella, Casazza Franco, Casolo Giancarlo, Cassin Matteo, Casu Gavino, Cemin Roberto, Chiarandà Giacomo, Chiarella Francesco, Chiatto Mario, Cibinel Gian Alfonso, Clerico Aldo, Colivicchi Furio, De Luca Giovanni, De Maria Renata, Del Sindaco Donatella, Di Fusco Stefania Angela, Di Lenarda Andrea, Di Tano Giuseppe, Egman Sabrina, Enea Iolanda, Fattirolli Francesco, Ferraiuolo Giuseppe, Francese Giuseppina Maura, Geraci Giovanna, Giardina Achille, Gregorio Giovanni, Iacoviello Massimo, Khoury Georgette, Ledda Antonietta, Lucà Fabiana, Lukic Vjerica, Macera Francesca, Marini Marco, Maseri Attilio, Masson Serge, Maurea Nicola, Mennuni Mauro, Menozzi Alberto, Mininni Nicola, Moreo Antonella, Moretti Luciano, Mortara Andrea, Mureddu Gian Francesco, Murrone Adriano, Musumeci Giuseppe, Nardi Federico, Navazio Alessandro, Nicolosi Gian Luigi, Oliva Fabrizio, Parato Vito Maurizio, Parrini Iris, Patanè Leonardo, Pini Daniela, Pino Paolo Giuseppe, Pirelli Salvatore, Pulignano Giovanni, Radini Donatella, Rao Carmelo Massimiliano, Rasetti Gerardo, Riccio Carmine, Roncon Loris, Rossini Roberta, Ruggieri Maria Pia, Rugolotto Matteo, Sanna Fabiola, Sauro Rosario, Scherillo Marino, Tarantini Luigi, Uguccioni Massimo, Urbinati Stefano, Valente Serafina, Vatrano Marco, Vianello Gabriele, Vinci Eugenio, Zuin Guerrino.
Conflict of interest: none declared.
References
- 1. www.salute.gov.it/imgs/c_17_pubblicazioni_2129_allegato.pdf (1 November 2015).
- 2. Rasmussen MB, Frost L, Stengaard C, Brorholt-Petersen JU, Dodt KK, Søndergaard HM, Terkelsen CJ.. Diagnostic performance and system delay using telemedicine for prehospital diagnosis in triaging and treatment of STEMI. Heart 2014;100:711–715. [DOI] [PubMed] [Google Scholar]
- 3. Mortara A, Oliva F,, Di Lenarda A.. Prospettive della telemedicina e del monitoraggio mediante dispositivi nel paziente con scompenso cardiaco cronico: luci e ombre. G Ital Cardiol 2010;11(5 Suppl 2):33S–37S. [PubMed] [Google Scholar]
- 4. Slotwiner D, Varma N, Akar JG, Annas G, Beardsall M, Fogel RI, Galizio NO, Glotzer TV, Leahy RA, Love CJ, McLean RC, Mittal S, Morichelli L, Patton KK, Raitt MH, Ricci RP, Rickard J, Schoenfeld MH, Serwer GA, Shea J, Varosy P, Verma A, Yu CM.. HRS Expert Consensus Statement on remote interrogation and monitoring for cardiovascular implantable electronic devices. Heart Rhythm 2015;12:e69–e100. [DOI] [PubMed] [Google Scholar]
- 5. Kurek A, Tajstra M, Gadula-Gacek E, Buchta P, Skrzypek M, Pyka L, Wasiak M, Swietlinska M, Hawranek M, Polonski L, Gasior M, Kosiuk J.. Impact of remote monitoring on long-term prognosis in heart failure patients in a real-world cohort: results from all-comers COMMIT-HF Trial. J Cardiovasc Electrophysiol 2017; doi: 10.1111/jce.13174. [DOI] [PubMed] [Google Scholar]
- 6. Boriani G, Da Costa A, Quesada A, Ricci RP, Favale S, Boscolo G, Clementy N, Amori V, Mangoni di S Stefano L, Burri H; MORE-CARE Study Investigators. Effects of remote monitoring on clinical outcomes and use of healthcare resources in heart failure patients with biventricular defibrillators: results of the MORE-CARE multicentre randomized controlled trial. Eur J Heart Fail 2017;19:416–425. [DOI] [PubMed] [Google Scholar]
- 7. Rouse CA, Woods BT, Mahnke CB.. A retrospective analysis of a pediatric tele-echocardiography service to treat, triage, and reduce trans-Pacific transport. J Telemed Telecare 2017; doi: 10.1177/1357633X16689500. [DOI] [PubMed] [Google Scholar]
- 8. McCrossan BA, Grant B, Morgan GJ, Sands AJ, Craig B, Casey FA.. Diagnosis of congenital heart disease in neonates by videoconferencing: an eight-year experience. J Telemed Telecare 2008;14:137–140. [DOI] [PubMed] [Google Scholar]
- 9. The task Force for the Management of Acute Coronary Syndromes in Patients presenting without Persistent ST-Segment Elevation of the European Society of Cardiology (ESC). 2015 ESC guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation. Eur Heart J 2016;37:267–315. [DOI] [PubMed] [Google Scholar]
- 10.Pozen MW, D'Agostino RB, Mitchell JB, Rosenfeld DM, Guglielmino JT, Schwartz ML, Teebagy N, Valentine JM, Hood WB Jr. The usefulness of a predictive instrument to reduce inappropriate admissions to the coronary care unit. Ann Intern Med 1980;92(2 Pt 1):238–242. [DOI] [PubMed] [Google Scholar]
- 11.Selker HP, Zalenski RJ, Antman EM, Aufderheide TP, Bernard SA, Bonow RO, Gibler WB, Hagen MD, Johnson P, Lau J, McNutt RA, Ornato J, Schwartz JS, Scott JD, Tunick PA, Weaver WD. An evaluation of technologies for identifying acute cardiac ischemia in the emergency department: a report from a National Heart Attack Alert Program Working Group. Ann Emerg Med 1997;29:13–87. [DOI] [PubMed] [Google Scholar]
- 12. Fedele F, Scalvini S.. Modelli di telecardiologia attualmente in uso. G Ital Cardiol 2009;10(Suppl 1-1):31S–33S. [Google Scholar]
- 13. Brunetti ND, De Gennaro L, Dellegrottaglie G, Antonelli G, Amoruso D, Di Biase M.. Prevalence of cardiac arrhythmias in pre-hospital tele-cardiology electrocardiograms of emergency medical service patients referred for syncope. J Electrocardiol 2012;45:727–732. [DOI] [PubMed] [Google Scholar]
- 14. Aufderheide TP, Hendley GE, Woo J, Lawrence S, Valley V, Teichman SL.. A prospective evaluation of prehospital 12-lead ECG application in chest pain patients. J Electrocardiol 1992;24(Suppl):8–13. [DOI] [PubMed] [Google Scholar]
- 15.Aufderheide TP, Hendley GE, Thakur RK, Mateer JR, Stueven HA, Olson DW, Hargarten KM, Laitinen F, Robinson N, Preuss KC, Hoffman RG. The diagnostic impact of prehospital 12-lead electrocardiography. Ann Emerg Med 1990;19:1280–1287. [DOI] [PubMed] [Google Scholar]
- 16. Sable C. Telecardiology: potential impact on acute care. Crit Care Med 2001;29 (Suppl):N159–N165. [DOI] [PubMed] [Google Scholar]
- 17. Scalvini S, Glisenti F.. Centenary of tele-electrocardiography and telephonocardiography—where are we today? J Telemed Telecare 2005;11:325–330. [DOI] [PubMed] [Google Scholar]
- 18. Varma N, Epstein AE, Irimpen A, Schweikert R, Love C; TRUST Investigators. Efficacy and safety of automatic remote monitoring for implantable cardioverter-defibrillator follow-up: the Lumos-T Safely Reduces Routine Office Device Follow-up (TRUST) trial. Circulation 2010;122:325–332. [DOI] [PubMed] [Google Scholar]
- 19. Mabo P, Victor F, Bazin P, Ahres S, Babuty D, Da Costa A, Binet D, Daubert JC; COMPAS Trial Investigators. A randomized trial of long-term remote monitoring of pacemaker recipients (the COMPAS trial). Eur Heart J 2012;33:1105–1111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Giovas P, Papadoyannis D, Thomakos D, Papazachos G, Rallidis M, Soulis D, Stamatopoulos C, Mavrogeni S, Katsilambros N.. Transmission of electrocardiograms from a moving ambulance. J Telemed Telecare 1998;4:5–7. [DOI] [PubMed] [Google Scholar]
- 21. Terkelsen CJ, Nørgaard BL, Lassen JF, Gerdes JC, Ankersen JP, Rømer F, Nielsen TT, Andersen HR.. Telemedicine used for remote prehospital diagnosing in patients suspected of acute myocardial infarction. J Intern Med 2002;252:412–420. [DOI] [PubMed] [Google Scholar]
- 22. Terkelsen CJ, Lassen JF, Nørgaard BL, Gerdes JC, Poulsen SH, Bendix K, Ankersen JP, Gøtzsche LB, Rømer FK, Nielsen TT, Andersen HR.. Reduction of treatment delay in patients with ST-elevation myocardial infarction: impact of prehospital diagnosis and direct referral to primary percutaneous coronary intervention. Eur Heart J 2005;26:770–777. [DOI] [PubMed] [Google Scholar]
- 23. Sejersten M, Sillesen M, Hansen PR, Nielsen SL, Nielsen H, Trautner S, Hampton D, Wagner GS, Clemmensen P.. Effect on treatment delay of prehospital teletransmission of 12-lead electrocardiogram to a cardiologist for immediate triage and direct referral of patients with ST-segment elevation acute myocardial infarction to primary percutaneous coronary intervention. Am J Cardiol 2008;101:941–946. [DOI] [PubMed] [Google Scholar]
- 24. Sørensen JT, Terkelsen CJ, Nørgaard BL, Trautner S, Hansen TM, Bøtker HE, Lassen JF, Andersen HR.. Urban and rural implementation of pre-hospital diagnosis and direct referral for primary percutaneous coronary intervention in patients with acute ST-elevation myocardial infarction. Eur Heart J 2011;32:430–436. [DOI] [PubMed] [Google Scholar]
- 25. Brunetti ND, Amodio G, De Gennaro L, Dellegrottaglie G, Pellegrino PL, Di Biase M, Antonelli G.. Telecardiology applied to a region-wide public emergency health-care service. J Thromb Thrombolysis 2009;28:23–30. [DOI] [PubMed] [Google Scholar]
- 26. Brunetti ND, Di Pietro G, Aquilino A, Bruno AI, Dellegrottaglie G, Di Giuseppe G, Lopriore C, De Gennaro L, Lanzone S, Caldarola P, Antonelli G, Di Biase M.. Prehospital electrocardiogram triage with telecardiology support is associated with shorter time to balloon and higher rates of timely reperfusion even in rural areas: data from the Bari-BAT public Emergency Medical Service 118 registry on primary angioplasty in STEMI. Eur Heart J Acute Cardiovasc Care 2014;3:204–213. [DOI] [PubMed] [Google Scholar]
- 27. Pedersen SH, Galatius S, Hansen PR, Mogelvang R, Abildstrom SZ, Sørensen R, Davidsen U, Galloe A, Abildgaard U, Iversen A, Bech J, Madsen JK, Jensen JS.. Field triage reduces treatment delay and improves long-term clinical outcome in patients with acute ST-segment elevation myocardial infarction treated with primary percutaneous coronary intervention. J Am Coll Cardiol 2009;54:2296–2302. [DOI] [PubMed] [Google Scholar]
- 28. Chan AW, Kornder J, Elliott H, Brown RI, Dorval JF, Charania J, Zhang R, Ding L, Lalani A, Kuritzky RA, Simkus GJ.. Improved survival associated with pre-hospital triage strategy in a large regional ST-segment elevation myocardial infarction program. JACC Cardiovasc Interv 2012;5:1239–1246. [DOI] [PubMed] [Google Scholar]
- 29. Curtis JP, Portnay EL, Wang Y, McNamara RL, Herrin J, Bradley EH, Magid DJ, Blaney ME, Canto JG, Krumholz HM; National Registry of Myocardial Infarction-4. The pre-hospital electrocardiogram and time to reperfusion in patients with acute myocardial infarction, 2000–2002: findings from the National Registry of Myocardial Infarction-4. J Am Coll Cardiol 2006;47:1544–1552. [DOI] [PubMed] [Google Scholar]
- 30. Brunetti ND, De Gennaro L, Amodio G, Dellegrottaglie G, Pellegrino PL, Di Biase M, Antonelli G.. Telecardiology improves quality of diagnosis and reduces delay to treatment in elderly patients with acute myocardial infarction and atypical presentation. Eur J Cardiovasc Prev Rehabil 2010;17:615–620. [DOI] [PubMed] [Google Scholar]
- 31. Sanchez-Ross M, Oghlakian G, Maher J, Patel B, Mazza V, Hom D, Dhruva V, Langley D, Palmaro J, Ahmed S, Kaluski E, Klapholz M.. The STAT-MI (ST-Segment Analysis Using Wireless Technology in Acute Myocardial Infarction) trial improves outcomes. JACC Cardiovasc Interv 2011;4:222–227. [DOI] [PubMed] [Google Scholar]
- 32. Quinn T, Johnsen S, Gale CP, Snooks H, McLean S, Woollard M, Weston C; Myocardial Ischaemia National Audit Project (MINAP) Steering Group. Effects of prehospital 12-lead ECG on processes of care and mortality in acute coronary syndrome: a linked cohort study from the Myocardial Ischaemia National Audit Project. Heart 2014;100:944–950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. de Waure C, Cadeddu C, Gualano M, Ricciardi RW.. Telemedicine for the reduction of myocardial infarction mortality: a systematic review and a meta-analysis of published studies. Telemed J E. Health 2012;18:323–328. [DOI] [PubMed] [Google Scholar]
- 34. Postma S, Kolkman E, Rubinstein SM, Jansma EP, De Luca G, Suryapranata H, van 'T Hof AW. Field triage in the ambulance versus referral via non-percutaneous coronary intervention centre in ST-elevation myocardial infarction patients undergoing primary percutaneous coronary intervention: A systematic review. Eur Heart J Acute Cardiovasc Care 2015; pii: 2048872615600098. [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 35. Brunetti ND, De Gennaro L, Dellegrottaglie G, Amoruso D, Antonelli G, Di Biase M.. A regional prehospital electrocardiogram network with a single telecardiology "hub" for public emergency medical service: technical requirements, logistics, manpower, and preliminary results. Telemed J E Health 2011;17:727–733. [DOI] [PubMed] [Google Scholar]
- 36. Martinoni S, De Servi E, Boschetti R, Zanini T, Palmerini A, Politi G, Musumeci G, Belli M, De Paolis F, Ettori E, Piccaluga D, Sangiorgi A, Repetto M, D'urbano B, Castiglioni F, Fabbiocchi M, Onofri N, De Cesare G, Sangiorgi C, Lettieri F, Poletti S, Pirelli S; Klugmann Lombardima Study Group. Importance and limits of prehospital electrocardiogram in patients with ST elevation myocardial infarction undergoing percutaneous coronary angioplasty. Eur J Cardiovasc Prev Rehabil 2011;18:526–532. [DOI] [PubMed] [Google Scholar]
- 37. Zanini R, Aroldi M, Bonatti S, Buffoli F, Izzo A, Lettieri C, Romano M, Tomasi L, Ferrari MR.. Impact of prehospital diagnosis in the management of ST elevation myocardial infarction in the era of primary percutaneous coronary intervention: reduction of treatment delay and mortality. J Cardiovasc Med 2008;9:570–575. [DOI] [PubMed] [Google Scholar]
- 38. Kalla K, Christ G, Karnik R, Malzer R, Norman G, Prachar H, Schreiber W, Unger G, Glogar HD, Kaff A, Laggner AN, Maurer G, Mlczoch J, Slany J, Weber HS, Huber K; VIENNA STEMI Registry Group. Implementation of guidelines improves standard of care: the Viennese registry on reperfusion strategies in ST-elevation myocardial infarction (VIENNA-STEMI Registry). Circulation 2006;113:2398–2405. [DOI] [PubMed] [Google Scholar]
- 39. Jollis JG, Roettig ML, Aluko AO, Anstrom KJ, Applegate RJ, Babb JD, Berger PB, Bohle DJ, Fletcher SM, Garvey JL, Hathaway WR, Hoekstra JW, Kelly RV, Maddox WT Jr, Shiber JR, Valeri FS, Watling BA, Wilson BH, Granger CB; Reperfusion of Acute Myocardial Infarction in North Carolina Emergency Departments (RACE) Investigators. Implementation of a statewide system for coronary reperfusion for ST-segment elevation myocardial infarction. JAMA 2007;298:2371–2380. [DOI] [PubMed] [Google Scholar]
- 40. Ortolani P, Marzocchi A, Marrozzini C, Palmerini T, Saia F, Serantoni C, Aquilina M, Silenzi S, Baldazzi F, Grosseto D, Taglieri N, Cooke RM, Bacchi-Reggiani ML, Branzi A.. Clinical impact of direct referral to primary percutaneous coronary intervention following pre-hospital diagnosis of ST-elevation myocardial infarction. Eur Heart J 2006;27:1550–1557. [DOI] [PubMed] [Google Scholar]
- 41. Brunetti ND, Bisceglia L, Dellegrottaglie G, Bruno AI, Di Pietro G, De Gennaro L, Di Biase M.. Lower mortality with pre-hospital electrocardiogram triage by telemedicine support in high risk acute myocardial infarction treated with primary angioplasty: Preliminary data from the Bari-BAT public Emergency Medical Service 118 registry. Int J Cardiol 2015;185:224–228. [DOI] [PubMed] [Google Scholar]
- 42. Repubblica Italiana, Ministero della Salute. Telemedicina: Linee di indirizzo nazionali. www.salute.gov.it/imgs/C_17_pubblicazioni_2129_allegato.pdf (1 November 2015).
- 43. www.onecare.2000cup.it (1 November 2015).
- 44. www.regione.piemonte.it/governo/bollettino/…/dddb200000010_830.pdf (1 November 2015).
- 45. Marzocchi A, Saia F, Bolognese L, Tamburino C, Giordano A, Ramondo A, Sangiorgi GM, Tomai F, Cavallini C, Sardella G, Cortesi P, Di Pasquale G, De Servi S. La rete per il trattamento dell’infarto miocardico acuto con sopraslivellamento del tratto ST in Italia. Risultati della rilevazione RETE IMA WEB. G Ital Cardiol 2011;12:354–364. [DOI] [PubMed] [Google Scholar]
- 46. http://www.gise.it/index.php?section=sezioni&idSection=1&idNotizia=1303 (1 November 2015).
- 47. McCabe JM, Armstrong EJ, Kulkarni A, Hoffmayer KS, Bhave PD, Garg S, Patel A, MacGregor JS, Hsue P, Stein JC, Kinlay S, Ganz P.. Prevalence and factors associated with false-positive ST-segment elevation myocardial infarction diagnoses at primary percutaneous coronary intervention–capable centers: a report from the Activate-SF registry. Arch Intern Med 2012;172:864–871. [DOI] [PubMed] [Google Scholar]
- 48.ECG dello STEMI: dalla diagnosi al Decision Making. FAD edito da OIC Firenze www.oicold.tecnofad.it/fadami/intro.aspx (1 November 2015).
- 49. http://www.regione.piemonte.it/sanita/cms2/notizie-87209/notizie-dallassessorato/archivio/2112-un-corso-a-distanza-per-riconoscere-linfarto-miocardico-acuto-il-piemonte-pioniere-di-uniniziativa-pilota-rivolta-a-medici-e-infermieri-dellemergenza (1 November 2015).
- 50. Baker CD, Lorimer AR.. Cardiology: the development of a managed clinical network. BMJ 2000;321:1152–1153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Provan K, Kenis P.. Modes of network governance: structure, management, and effectiveness. J Public Adm Res Theory 2008;18:229–252. [Google Scholar]
- 52. Cadilhac DA, Pearce DC, Levi CR, Donnan GA.. Improvements in the quality of care and health outcomes with new stroke care units following implementation of a clinician-led, health system redesign programme in New South Wales, Australia. Qual Saf Health Care 2008;17:329–333. [DOI] [PubMed] [Google Scholar]
- 53. Diercks DB, Kontos MC, Chen AY, Pollack CV Jr, Wiviott SD, Rumsfeld JS, Magid DJ, Gibler WB, Cannon CP, Peterson ED, Roe MT.. Utilization and impact of pre-hospital electrocardiograms for patients with acute ST-segment elevation myocardial infarction: data from the NCDR (National Cardiovascular Data Registry) ACTION (Acute Coronary Treatment and Intervention Outcomes Network) Registry. J Am Coll Cardiol 2009;53:161–166. [DOI] [PubMed] [Google Scholar]
- 54. Jacobs AK, Antman EM, Faxon DP, Gregory T, Solis P.. Development of systems of care for ST-elevation myocardial infarction patients: executive summary. Circulation 2007;116:217–230. [DOI] [PubMed] [Google Scholar]
- 55. Documento di consenso. La rete interospedaliera per l’emergenza coronarica. Ital Heart J 2005;6:5S–26S. [Google Scholar]
- 56. Kligfield P, Gettes LS, Bailey JJ, Childers R, Deal BJ, Hancock EW, van Herpen G, Kors JA, Macfarlane P, Mirvis DM, Pahlm O, Rautaharju P, Wagner GS, Josephson M, Mason JW, Okin P, Surawicz B, Wellens H; American Heart Association Electrocardiography and Arrhythmias Committee, Council on Clinical Cardiology; American College of Cardiology Foundation; Heart Rhythm Society . Recommendations for the standardization and interpretation of the electrocardiogram: part I: the electrocardiogram and its technology a scientific statement from the American Heart Association Electrocardiography and Arrhythmias Committee, Council on Clinical Cardiology; the American College of Cardiology Foundation; and the Heart Rhythm Society endorsed by the International Society for Computerized Electrocardiology. J Am Coll Cardiol 2007;49:1109–1127. [DOI] [PubMed] [Google Scholar]
- 57. Nolan JP, Soar J, Zideman DA, Biarent D, Bossaert LL, Deakin C, Koster RW, Wyllie J, Böttiger B; ERC Guidelines Writing Group. European Resuscitation Council Guidelines for Resuscitation 2010 Section 1. Executive summary. Resuscitation 2010;81:1219–1276. [DOI] [PubMed] [Google Scholar]
- 58. Gregoratos G, Abrams J, Epstein AE, Freedman RA, Hayes DL, Hlatky MA, Kerber RE, Naccarelli GV, Schoenfeld MH, Silka MJ, Winters SL.. ACC/AHA/NASPE 2002 Guideline Update for Implantation of Cardiac Pacemakers and Antiarrhythmia Devices–summary article: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (ACC/AHA/NASPE Committee to Update the 1998 Pacemaker Guidelines). J Am Coll Cardiol 2002;40:1703–1719. [DOI] [PubMed] [Google Scholar]
- 59. Thorne CJ, Lockey AS, Bullock I, Hampshire S, Begum-Ali S, Perkins GD.. E-learning in advanced life support – an evaluation by Resuscitation Council (UK). Resuscitation 2015;90:79–84. [DOI] [PubMed] [Google Scholar]