Highlights
-
•
Primary small cell neuroendocrine carcinoma of the breast is a very rare diagnosis.
-
•
It has similar features to small cell neuroendocrine carcinoma of the lung.
-
•
Diagnostic workup must exclude metastasis from another primary site.
-
•
Treatment combines approaches for more common types of lung and breast cancer.
-
•
Further studies are needed to standardized the treatment for primary SCNCB.
Abbreviations: SCNCB, small cell neuroendocrine carcinoma of the breast; SCNCL, small cell neuroendocrine carcinoma of the lung; DCIS, ductal carcinoma in situ
Keywords: Breast, Breast cancer, Small cell neuroendocrine carcinoma, Case report, Chemotherapy
Abstract
Introduction
Primary small cell neuroendocrine carcinoma of the breast (SCNCB) is a very uncommon type of breast cancer. Histology and morphology are virtually indistinguishable from small cell neuroendocrine carcinomas of the lung (SCNCL), mandating a search for a primary site elsewhere in the body. There is no standard approach to treatment as there are only a limited number of cases reported in the literature. This report summarizes a case of primary SCNCB and presents a review of the literature.
Presentation of case
A 65-year-old female presented to her gynecologist with a right breast mass. After biopsy, she was diagnosed with a primary SCNCB with regional lymph node involvement. She was treated with chemotherapy and radiation therapy with a good clinical response.
Discussion
Due to the rare nature of this tumor, no standard treatment exits. Case reports have described breast conserving therapy combined with neoadjuvant or adjuvant chemotherapy as well as chemoradiation therapy alone for metastatic disease. Both chemotherapy regimens, those used to treat SCNCL and invasive breast cancer, have been described in these reports.
Conclusion
Primary SCNCB is a very rare type of breast cancer with no standard treatment. Further research is needed to better understand the behavior of this rare tumor in order to develop a standard approach to treatment.
1. Introduction
Primary small cell neuroendocrine carcinoma of the breast (SCNCB) is a very rare type of breast cancer. It is typically diagnosed in women over 60 who present with a palpable breast mass and morphologic features seen in other neuroendocrine tumors. It is very difficult to distinguish histologically from small cell neuroendocrine carcinoma of the lung (SCNCL), so a thorough search must be performed to rule out metastatic disease from another primary site [1]. Other useful diagnostic tools to determine the site of origin include the expression of neuroendocrine markers on immunohistochemical staining. These however are inconsistently expressed and only support the diagnosis rather than exclude it [2].
Due to its rarity, there is no standard treatment of SCNCB within the literature. Several treatment strategies have been described based on current guidelines for breast cancer treatment and small cell lung cancer treatment [3]. We describe a case of a 65-year-old female who presented to our community-based, university affiliated teaching hospital with primary SCNCB with regional lymph node involvement. She underwent treatment with chemotherapy and radiation therapy and achieved a good clinical response based on follow up PET-CT scan. This work has been reported in line with the SCARE criteria and PROCESS criteria [4], [5].
2. Presentation of case
A 65-year-old G0P0 Caucasian female presented to her gynecologist with complaints of a right breast mass noticed during her monthly self breast exam. She was referred to our Breast Health Center for consultation with a surgical breast oncologist. She had a remote smoking history (5.5 pack years, 35 years prior to presentation) with a heavy exposure to second-hand smoke. Her mother was diagnosed with breast cancer at age 65. She had a 15-year history of oral contraception use. Based on a modified Gail Model, her lifetime risk of developing breast cancer was 12.0%. The patient had a history of bilateral breast implants 30 years prior. Of note, she had a normal screening mammogram two-and-a-half months prior to presentation.
Clinical examination revealed a 5 cm palpable mass in the right breast, upper outer quadrant, approximately 17 cm from the nipple and associated with a subtle bulge. Her lungs were clear to auscultation, abdominal exam was without masses, and no inguinal, cervical, or contralateral axillary adenopathy was palpated. She proceeded to have a diagnostic mammogram (Fig. 1) and ultrasound (Fig. 2) which demonstrated an irregular mass in the right axilla with increased vascularity, highly suggestive of malignancy. This mass appeared to engulf the surrounding lymph nodes, which were enlarged up to 7 mm. Biopsies revealed small cell carcinoma with neuroendocrine features in both areas (Fig. 3), ER/PR negative, HER2 negative. Immunohistochemical staining was positive for TTF-1, synaptophysin and chromogranin, suggesting a primary small cell carcinoma of the breast (Fig. 4). Subsequent MRI (Fig. 5) revealed a 4.6 × 6.6 × 6.3 cm irregular mass in the right axilla with multiple oval masses in the right axillary tail just medial to the larger mass.
Fig. 1.
Diagnostic mammogram: Right mediolateral oblique view showing an irregular high density mass in the right breast, posterior depth, upper region.
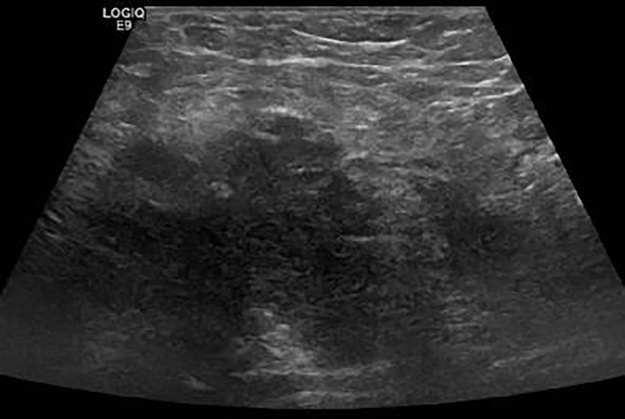
Fig. 2.
Ultrasonography of right breast and axilla: Irregular hypoechoic mass in the right axillary tail, resembling carcinoma and highly suggestive of malignancy.
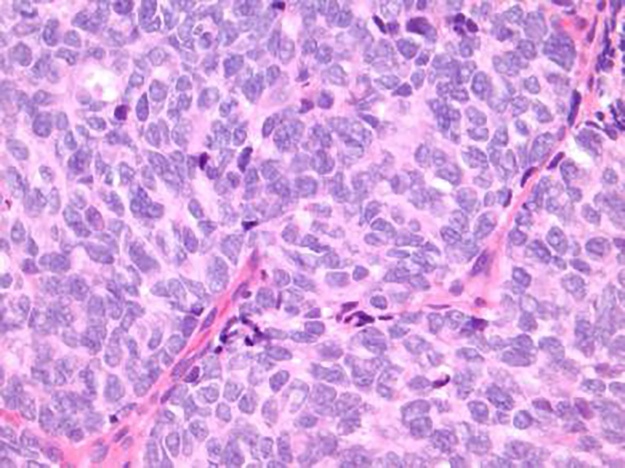
Fig. 3.
H&E staining on high power field (40×) showing neoplastic cells with nuclear pleomorphism, nuclear molding, mitotic figures, hyperchromatic nuclei, minimal cytoplasm, and indistinct nuclei consistent with the diagnosis of small cell neuroendocrine carcinoma.
Fig. 4.
Immunohistochemical staining for synaptophysin is positive with objective of 40x.
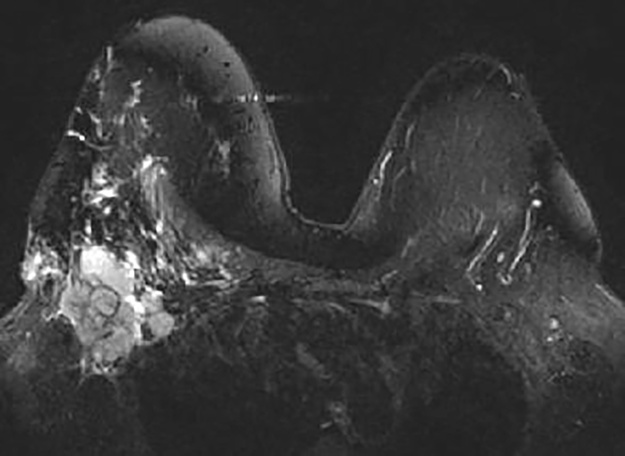
Fig. 5.
Breast MRI: 4.6 × 6.6 × 6.3 cm irregular mass in the right axilla with multiple oval masses in the right axillary tail consistent with pathological lymph nodes.
Radiologic workup included a CT of the chest, abdomen and pelvis as well as an MRI of the brain to exclude a primary tumor outside of the breast and complete a staging workup of the breast lesion. Additionally, a PET-CT scan of the torso was performed for radiation planning. There were no lung, pancreatic, adrenal, or pelvic masses identified. Based on the small cell neuroendocrine features and regional lymph node involvement, the patient was started on a chemotherapy regimen of carboplatin and etoposide followed by radiation therapy to decrease the risk of local recurrence and prolong survival based on treatment strategies for SCNCL. She tolerated this treatment well and follow up PET-CT scan showed a good clinical response three months after treatment.
3. Discussion
Small cell neuroendocrine carcinoma is an aggressive tumor most commonly found in the lung, but can arise in other sites, such as the breast, larynx, trachea, GI tract, bladder, prostate, cervix, and ovary [1], [2], [6]. Primary SCNCB is a very rare type of breast cancer, with a reported incidence of <0.1% to 1–5% of all breast cancers [3], [7]. There are only limited reports in the literature; they consist primarily of case reports with a few case series described more recently. Primary SCNCB typically presents as a palpable breast or axillary mass in women over 60 years old and 50–67% have lymph node involvement at the time of presentation [1].
Primary SCNCB is difficult to diagnose as it has similar histologic and morphologic features to that of SCNCL and other types of breast cancer. For this reason, a thorough investigation with CT and PET scans to rule out metastatic disease from another primary site is warranted. Another important diagnostic tool is the use of immunohistochemical staining for neuroendocrine markers, specifically chromogranin and synaptophysin [3]. While these markers aid in the diagnosis of a neuroendocrine tumor, they are inconsistently expressed in primary SCNCB and thus are not necessary for the diagnosis [2]. Estrogen receptors are positive in 35–54% of primary SCNCB, while HER2 is almost always negative [1], [7]. This is lower than that reported for other types of invasive breast cancer [7]. The presence of ductal carcinoma in situ (DCIS) can confidently confirm the diagnosis of small cell neuroendocrine carcinoma as a primary breast tumor [3]. Other diagnostic features that support a primary breast lesion are the absence of tumors in other organs on radiologic imaging and the presence of regional lymph node metastases [1].
Due to the rare occurrence and limited reports of this tumor, there is no standard approach to the treatment of primary SCNCB. Treatment regimens discussed in the literature include various combinations of surgery, chemotherapy, radiation therapy, and endocrine therapy. Early reports described modified radical mastectomy with adjuvant chemotherapy and/or radiation therapy as the treatment of choice [1]. More recent reports have described treatment with breast conservation therapy combined with either neoadjuvant or adjuvant chemotherapy depending on the clinical scenario. Most chemotherapy regimens described have used platinum agents and etoposide, typical therapies used for SCNCL; however, some have reported using anthracycline and taxane based combinations typically used for invasive breast cancer [1], [2], [3], [6].
Our patient represents a case of primary SCNCB due to the presence of neuroendocrine markers on immunohistochemical staining in combination with a large breast mass, regional lymph node involvement and lack of evidence of any masses in other organs on radiologic imaging. Based on our review of the literature, the size and histology of the tumor, and regional lymph node involvement, we treated the patient with systemic chemotherapy using carboplatin and etoposide along with radiation therapy. PET-CT scan performed upon completion of treatment showed a good clinical response.
4. Conclusion
Primary SCNCB is a very rare and aggressive type of breast cancer. It has similar histological and immunohistochemical features when compared to SCNCL and diagnostic evaluation must include a workup to rule out metastasis from another primary site such as the lung. Due to its rarity, no standard treatment exists. Treatment strategies described in the literature are based on extrapolating SCNCL and standard breast cancer treatments to primary SCNCB cases. Further studies are needed to standardize the treatment for this rare tumor.
Conflict of interest
The authors have no conflict of interest to declare.
Funding
This paper received no financial support.
Ethical approval
Approval to publish this case report was waived by the institution.
Consent
Written informed consent was not obtained as no personal information or identifying images are included.
Authors contribution
Abigail Tremelling, MD: drafted and critically revised article.
Selyne Samuel, MD: critically revised article.
Mary Murray, MD: critically revised article, surgeon involved in diagnosis and management plan.
Guarantors
Abigail Tremelling and Mary Murray.
Acknowledgement
Not applicable.
References
- 1.Latif N., Rosa M., Samian L., Rana F. An unusual case of primary small cell neuroendocrine carcinoma of the breast. Breast J. 2010;16:647–651. doi: 10.1111/j.1524-4741.2010.00974.x. [DOI] [PubMed] [Google Scholar]
- 2.Adegbola T., Connolly C.E., Mortimer G.S. Small cell neuroendocrine carcinoma of the breast: a report of three cases and review of the literature. J. Clin. Pathol. 2005;58:775–778. doi: 10.1136/jcp.2004.020792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Inno A., Bogina G., Turazza Bortesi L., Duranti S., Massocco A. Neuroendocrine carcinoma of the breast: current evidence and future perspectives. Oncologist. 2016;21:28–32. doi: 10.1634/theoncologist.2015-0309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Agha R.A., Fowler A.J., Saetta A., Barai I., Rajmohan S., Orgill D.P., for the SCARE Group The SCARE statement: consensus-based surgical case report guidelines. Int. J. Surg. 2016;34:180–186. doi: 10.1016/j.ijsu.2016.08.014. [DOI] [PubMed] [Google Scholar]
- 5.Agha R.A., Fowler A.J., Rajmohan S., Barai I., Orgill D.P., for the PROCESS Group Preferred reporting of case series in surgery; the PROCESS guidelines. Int. J. Surg. 2016;36:319–323. doi: 10.1016/j.ijsu.2016.10.025. [DOI] [PubMed] [Google Scholar]
- 6.Hojo T., Kinoshita T., Shien T., Terada K., Hirose S., Isobe Y. Primary small cell carcinoma of the breast. Breast Cancer. 2009;16:68–71. doi: 10.1007/s12282-008-0057-9. [DOI] [PubMed] [Google Scholar]
- 7.Wang J., Wei B., Albarracin C.T. Invasive neuroendocrine carcinoma of the breast: a population-based study from the surveillance, epidemiology and end results (SEER) database. BMC Cancer. 2014;14:147–156. doi: 10.1186/1471-2407-14-147. [DOI] [PMC free article] [PubMed] [Google Scholar]