Abstract
Objectives
The objective is to identify an evidence-based minimum physical activity threshold to predict improved or sustained high function for adults with lower limb joint symptoms.
Methods
Prospective multi-site data from 1629 adults aged 49 years or older with symptomatic lower limb joint pain/aching/stiffness participating in Osteoarthritis Initiative accelerometer monitoring substudy were clinically assessed two years apart. Improved/high function in 2-year gait speed and patient-reported outcomes (PRO) were based on improving or remaining in the best (i.e., maintaining high) function quintile compared to baseline status. Optimal thresholds predicting improved/high function were investigated using classification trees for the legacy federal guideline metric requiring 150 minutes/week of moderate-vigorous (MV) activity in bouts lasting 10 minutes or more (MV-bout) and other metrics (total MV, sedentary, light intensity activity, non-sedentary minutes/week).
Results
Optimal thresholds based on total MV minutes/week predicted improved/high function outcomes more strongly than the legacy or other investigated metrics. Meeting the 45 total MV minute/week threshold had increased relative risk (RR) for improved/high function (gait speed RR 1.8, 95% CI: 1.6 to 2.1; PRO physical function RR 1.4, 95% CI: 1.3 to 1.6) compared to less active adults. Thresholds were consistent across sex, BMI, knee OA status and age.
Conclusions
These results supported a physical activity minimum threshold of 45 total MV minutes/week to promote improved or sustained high function for adults with lower limb joint symptoms. This evidence-based threshold is less rigorous than federal guidelines (≥150 MV-bout minutes/week) and provides an intermediate goal towards the federal guideline for adults with lower limb symptoms.
INTRODUCTION
Physical activity is endorsed as a healthy lifestyle strategy. Federal guidelines for adults stipulate a minimum threshold of 150 minutes/week of moderate intensity or 75 minutes of vigorous intensity physical activity or an equivalent combination.1 These guidelines utilize a legacy metric requiring activity bouts of moderate or vigorous activity lasting at least 10 minutes based on studies demonstrating cardiovascular benefits from aerobic activity.2–5 But the vast majority of adults fail to meet these guidelines.6,7 Even more concerning, as many as 2 in 5 adults with lower limb joint conditions not only fail to meet guidelines, they register zero on the legacy bout metric; over an entire week they do not have a single session of moderate physical activity lasting 10 minutes.8,9
Maintaining function is crucial to independent community living for adults with physical impairments. For many adults living with joint conditions, improving or maintaining high function may be as great a concern as cardiovascular health. Physical function has long been recognized as a proxy for overall health. Physical function assessed by gait speed reflects functional status and health.10 Gait speed has been repeatedly associated with survival in epidemiologic studies.11–13 Similarly, patient-reported functional status is related to quality of life and life expectancy.14 Lower limb joint conditions such as hip or knee osteoarthritis (OA) increase a person’s risk for subsequent loss of function.12,15 While being physically active is associated with functional gains16 among adults with joint disease,17 it is not known if there is a level of physical activity that may promote better function or maintain high functional ability.18
Investigating what physical activity levels might improve low function or maintain high (improved/high) function among adults with lower limb symptoms motivates two questions: 1) Are there alternative physical activity metrics which better predict improved/high function than the legacy bout-based metric, which registers zero for a large portion of these adults? 2) What minimum threshold of physical activity best predicts improved/high function? The objective of this study is to identify optimal physical activity metrics and dosage thresholds related to improving low or maintaining high function among adults with lower limb joint symptoms.
METHODS
Study Population
Participants were a subcohort of the Osteoarthritis Initiative (OAI) enrolled into an accelerometer ancillary study conducted at the OAI 2008–2010 clinic visit (OAI 4-year follow-up), which is baseline for this study. The OAI is a multi-center prospective study investigating risk factors and biomarkers for the progression and/or onset of knee OA (see http://www.oai.ucsf.edu/datarelease/About.asp). At enrollment, the OAI recruited 4796 men and women between 45 to 79 years of age from four clinical sites: Baltimore MD, Pittsburgh PA, Pawtucket RI, and Columbus OH. The OAI enrolled participants with or at high risk for developing symptomatic, radiographic knee OA. High risk was defined as frequent knee symptoms without radiographic OA, or two or more eligibility risk factors (e.g. age, high body mass index, prior knee injury, knee surgery, family history of total knee replacement for OA, Heberden’s nodes, and repetitive knee bending).19 OAI eligibility criteria have been described in detail elsewhere.20 Approval was obtained from the institutional review board at each OAI site and at Northwestern University. Each participant provided written informed consent.
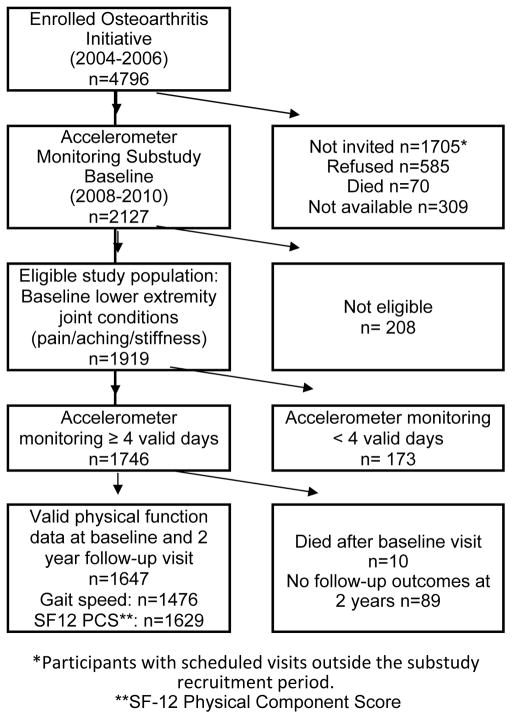
A subgroup of 2127 OAI participants participated in an accelerometer study at the 48 month clinic visit, which represents our study’s baseline. Eligibility for the substudy required a scheduled OAI follow-up visit between August 2008 and June 2010. The present study sample included1919 accelerometer study participants reporting ankle, foot, knee, and/or hip lower limb joint symptoms of pain, aching, or stiffness. Ankle, foot, and knee questions solicited symptoms over the past 30 days; hip questions solicited symptoms over the past 12 months. Of individuals reporting hip symptoms 90% were in the analysis sample based on symptoms reported in another joint. Loss to follow-up was minimal; over 96% (1845/1919) of this cohort participated in a follow-up visit two years later. For analysis purposes we restricted our sample to 1647 individuals with baseline and 2-year follow-up (2010–2012) physical function measured objectively by gait speed (n=1476) and/or by patient reported outcome (PRO) based on the SF-12 physical component score (n=1629) respectively (Figure 1). Excluded were 173 persons with inadequate accelerometer monitoring to support reliable physical activity estimates7 (i.e. less than 4 valid days of monitoring based on daily evidence of 10 hours or more accelerometer wear), and 89 did not have 2 year follow-up outcomes (64 with no contact, 23 with only phone contact, and 2 refused).
Figure 1.
Flow of analytical sample
*Participants with scheduled visits outside the substudy recruitment period.
**SF-12 Physical Component Score
Outcomes
The primary outcome was change in improved or high (improved/high) physical function status between baseline and 2-year follow-up, separately assessed by objective gait speed and by PRO physical function SF-12 physical component score. Improved/high function was based on transitions across functional quintiles over time. This method captures practical, meaningful changes in function over time in OA populations.21–23 Five quintile groups are defined from the full parent enrollment OAI knee OA cohort for objective gait speed physical function (Q1:<3.7, Q2: 3.7–4.0, Q3: 4.1–4.3, Q4: 4.4–4.7, Q5:≥4.8 feet per second) and PRO-physical function (Q1: <39.4, Q2: 39.4–46.9, Q3:47.0–52.1, Q4:52.2–56.0, Q5:≥56.1). Baseline and 2-year function scores from accelerometer substudy participants (n=1647) were categorized into each of these groups. Subsequent improved/high function was defined by maintaining function in the best group (i.e., Q5 at both evaluations) or moving into a better (i.e., moving from Q1–Q4 to a higher group) group at 24 months compared to baseline. We use function transitions to identify improved/high physical function outcomes rather than an improvement exceeding a minimal clinically important difference (MCID) due to 1) the value of retaining participants who maintain high function (e.g., participants whose high baseline function makes them unable to improve an MCID) and 2) validity concerns when applying MCIDs estimated from randomized clinical trial samples to community populations.24
Physical Activity Assessment
Physical activity was monitored using the ActiGraph GT1M uniaxial accelerometer.25 Trained research personnel gave uniform scripted in-person instructions to wear the accelerometer for seven consecutive days on a belt at the natural waistline in line with the right axilla upon arising in the morning until retiring, except during water activities. Participants maintained a daily log to record time spent in water and cycling activities, which may not be fully captured by accelerometers. Such activity was negligible (interquartile range: 0 to 0 minutes/week) and not utilized in the present study.
Accelerometer data were analytically filtered using validated methodology.26,27 Nonwear periods were defined as ≥ 90 minutes with zero activity counts (allowing for 2 consecutive interrupted minutes with counts <100)7. We identified participants with 4–7 valid monitoring days (i.e., 10 or more wear hours per day) needed for reliable physical activity estimates.7 Thresholds used by the National Cancer Institute (NCI) on a minute-by-minute basis were applied to identify sedentary (counts/minute<100), non-sedentary (counts/minute≥100), light (100–2019 counts/minute) and moderate-to-vigorous (counts/minute ≥ 2020) intensity activity (MV-total) 7 and MV activity accumulated in bouts lasting ≥ 10 minutes (MV-bout). Due to negligible vigorous (counts/minute ≥ 5999) activity (median=0, interquartile range: 0 to 0 minutes/week) in this cohort, vigorous time and vigorous bouts were not separately evaluated. Weekly activity minutes spent at each intensity level are summed from the daily totals over the monitoring hours and averaged across valid monitored days; for individuals with 4, 5, or 6 valid days of monitoring, weekly activity minutes were estimated as 7 average daily activity minutes spent at each intensity level.
Baseline covariates
Demographic factors included age and sex. Body mass index (BMI) was calculated from measured height and weight [weight (kg)/height (m)2] to classify individuals as normal weight (BMI 18.5–24.9), overweight (BMI 25.0–29.9), or obese (BMI ≥30). If baseline (i.e., OAI 4-year) BMI was missing (0.2%, n=4), the most recent annual assessment was used as a proxy. Knee osteoarthritis was identified by a Kellgren-Lawrence grade score of two or greater in one or both knees assessed from “fixed-flexion” knee radiography protocol28.
Statistical analysis
Candidate metrics (sedentary, non-sedentary, light, MV-total) were screened by comparing each to the legacy MV-bout metric, the basis for assessing current physical activity guidelines. For this purpose, we calculated the area under the receiver operating characteristic curve (AUC), to transform the predictive ability of each metric to a common 0 to 1 scale. For each legacy and candidate metric we first derived the receiver operating curve, which is graphically represented by the metric sensitivity plotted versus the fraction of false positives (i.e., 1-specificity) in relation to a physical function outcome. We then determined the AUC area.29 Candidate metrics which performed at least as well (i.e., greater AUC) as the legacy MV-bout reference metric AUC were retained for predictive modeling. Comparison of candidate metric AUC with the legacy MV-bout AUC used a test developed by Delong, Delong and Clarke-Pearson.30
Thresholds were identified using classification and regression tree (CART) methodology. We separately predicted improved/high gait speed and improved/high PRO physical function. For both outcomes, all candidate metrics with AUCs which exceeded the reference MV-bout metric AUC were used as classification tree predictors in addition to the reference MV-bout metric. A classification tree identifies the predictors and threshold of the selected predictor with the strongest relationship to the outcome based on the criterion of minimum classification error.31 To avoid overfitting, models were evaluated using cross-validation subsets and pruned to the most parsimonious model within one standard prediction error from the best-fit model.32 Classification tree analysis was selected over other traditional methods (e.g., stepwise logistic regression) given the goal to identify thresholds in an optimal prediction model (i.e., minimizes misclassification error).33,34 Analyses were performed using Salford Predictive Modeler software version 8.0.35 Classification tree algorithms retain all records having outcomes; missing predictors are handled by substituting “surrogate splitters,” which are back-up rules that closely mimic the primary splitting rules. Recognizing systematic differences between people with and without follow-up outcomes could influence our findings, we did weighted analyses recommended by Hogan36. For simplicity we report unweighted analyses because weighted analyses provided identical findings. To investigate the stability of thresholds across age, sex, BMI, and radiographic knee OA presence, we performed sensitivity analyses. Each factor was separately entered into a classification tree analysis in addition to physical activity metrics to predict improved/high function to explore separate thresholds within the factor investigated. Other analyses were performed using SAS software version 9.4. Statistical testing was conducted at a two-sided 5% significance level.
RESULTS
Participants in the Osteoarthritis Initiative accelerometer substudy with baseline lower limb joint symptoms and subsequent function outcomes (n=1647) were primarily female (56%), obese (37%), and ranged in age from 49 to 83 years. The most common lower limb symptoms reported were knee symptoms (93% of whom 61% with radiographic disease) followed by hip symptoms (60%), foot (12%), and ankle (11%). Both hip and knee symptoms were reported by 54% of this sample.
The baseline values of the legacy physical activity metric and candidate metrics are shown in Table 1 by subsequent improved/high function status. At the 2-year follow-up, 34% (500/1476) had improved/high gait speed and 38% (622/1629) had improved/high PRO physical function. The baseline legacy MV-bout metric and MV-total activity metric, showed the greatest separation across all metrics between people who did or did not belong to improved/high function groups (25% difference or greater). It is notable only sedentary time did not significantly differ between groups for either function measure.
Table 1.
Baseline physical activity metrics of adults by physical function status at two-year follow-up
| Baseline Physical Activity Metrics in minutes/week | Improved/high Objective Gait Speed Physical Function N=1476 |
Improved/high PRO Physical Function N=1629 |
||||
|---|---|---|---|---|---|---|
|
| ||||||
| Yes mean± SD n=500 |
No mean± SD n=976 |
Difference (95% Confidence Interval) | Yes mean± SD n=622 |
No mean± SD n=1007 |
Difference (95% Confidence Interval) | |
|
| ||||||
| Legacy Metric | 76±111 | 47±87 | 29 (19, 40) | 68±103 | 50±92 | 17 (8, 27) |
| MV-bout† | ||||||
|
| ||||||
| Candidate Metrics | ||||||
| Sedentary | 4123±647 | 4118±614 | 5 (-63, 72) | 4125±629 | 4122±620 | 3 (-59, 66) |
| Light activity | 2058±536 | 1964±554 | 94 (36, 154) | 2002±524 | 1964±558 | 38 (-17, 93) |
| MV-total‡ | 166±149 | 108±122 | 58 (43, 72) | 146±141 | 114±129 | 33 (19, 46) |
| Non-sedentary | 2224±576 | 2072±599 | 152 (89, 216) | 2149±568 | 2078±605 | 71 (12, 130) |
Minutes of moderate-to-vigorous physical activity acquired in bouts lasting ten or more minutes. Because
Total accumulated minutes of moderate-to-vigorous physical activity
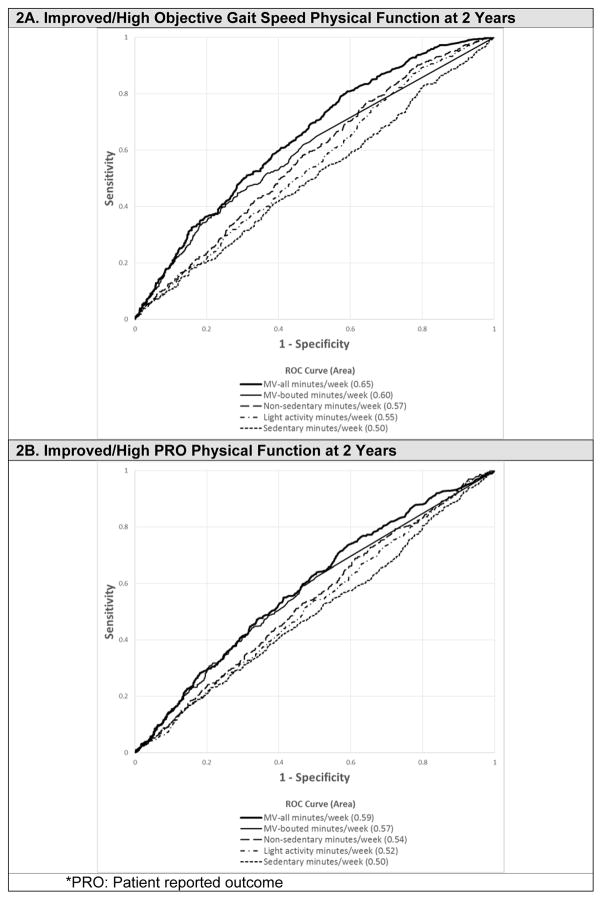
The relative predictive value of each metric to distinguish improved/high function status two years is visually represented by receiver operating characteristic curves shown in Figure 2A for improved/high gait speed function and Figure 2B for improved/high PRO physical function. The calculated area under each curve (AUC) indicates all metrics performed better than a random “coin flip” (AUC=0.5) to predict improved/high function measures. However, only the MV-total activity metric had greater AUC than the legacy MV-bout reference metric to predict both improved/high gait speed (AUC 0.65 versus 0.60; difference: 0.05; 95% CI: 0.03, 0.07) and PRO physical function (AUC 0.59 versus 0.57; difference: 0.02; 95% CI: 0.001, 0.03).
Figure 2.
Receiver Operating Characteristic (ROC) Curves for Improved/High Physical Function Outcomes at 2 Years by Physical Activity Metrics
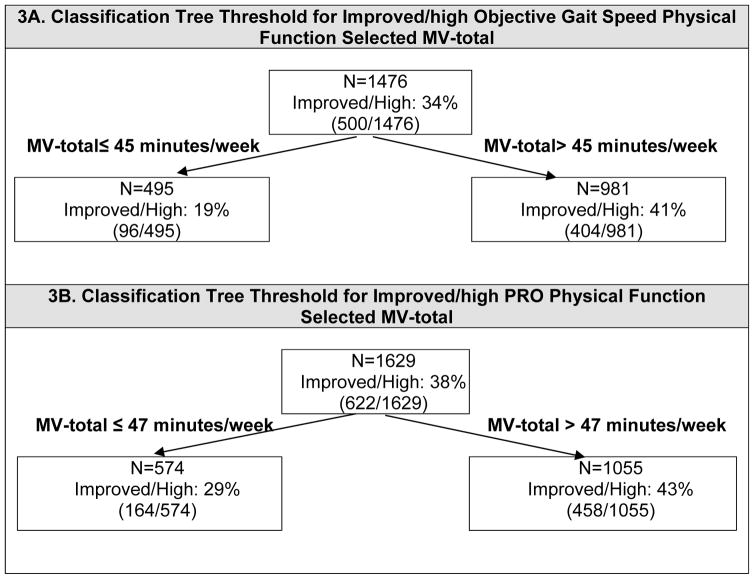
CART classification tree analysis was used to identify both the optimal metric and the physical activity threshold to best predict improved/high function. The MV-total candidate metric and the reference MV-bout metric were entered as classification tree predictors. Separate trees were grown to predict improved/high gait speed and improved/high PRO physical function outcomes. The optimal classification trees are shown in Figure 3. The MV-total metric was selected over MV-bout as the best predictor of both outcomes, consistent with the Figure 2 AUC analyses. The optimal threshold to predict improved/high objective gait speed physical function was 45 MV-total minutes per week. The optimal minimum threshold to predict improved/high PRO physical function was 47 MV-total minutes per week.
Figure 3.
Classification trees selecting physical activity dosage thresholds to predict improved/high* 2-year function in gait speed and SF-12 Physical Component Score.
Sensitivity analyses investigated if optimal physical activity thresholds were specific to age, sex, presence/absence of knee OA, or BMI. Each factor was separately entered in addition to MV-total and MV-bout into a classification tree analysis to predict improved/high function in gait speed and in PRO physical function. Seven of the eight sensitivity classification tree analyses (i.e., 4 exposure factors X 2 outcome trees) solely selected an MV-total threshold (MV-total thresholds of 45 minutes/week for gait speed and 47 minutes/week for PRO physical function). One of the eight sensitivity analyses to predict improved/high gait speed initially split on age (age ≤69 MV-total threshold: 46 minutes/week, age >69 threshold: none). Further investigation of the age>69 subgroup identified a candidate MV-total threshold (10 minutes/week) but the improvement in prediction accuracy was insufficient for retention (i.e., below the 1 SE rule criterion). These sensitivity analyses demonstrate good stability of the MV-total thresholds.
Table 2 summarizes the ability of the thresholds to predict subsequent improved/high function based on relative risks. The optimal gait speed MV-total threshold (>45 minutes per week) better discriminated subsequent improved/high function status than the current guideline (MV-bout≥150 minutes per week) demonstrated by the stronger relative risk (1.8 versus 1.4). Similarly the optimal PRO physical function MV-total threshold (>47 minutes per week) had a higher relative risk (1.4 vs 1.3) to predict improved/high function than the current guideline.
Table 2.
Improved/high 2-year function relative risk (RR) for physical activity metrics by dosage thresholds among adults with baseline lower limb symptoms
| Physical Activity in Minutes/week | Improved/high Objective Gait Speed Physical Function N=1476 RR (95% CI) |
Improved/high PRO* Physical Function N=1629 RR (95% CI) |
|---|---|---|
|
| ||
| Legacy threshold | ||
| MV-bout† ≥150 | 1.4 (1.3, 1.6) | 1.3 (1.2, 1.4) |
| Optimal threshold | ||
| MV-total‡ ≥45** | 1.8 (1.6, 2.1) | 1.4 (1.3, 1.6) |
| MV-total‡ ≥47*** | 1.8 (1.6, 2.0) | 1.4 (1.3, 1.6) |
Minutes of moderate-to-vigorous physical activity acquired in bouts lasting ten or more minutes
Total minutes of moderate-to-vigorous physical activity
Patient reported outcome
Optimal threshold for improved/high gait speed function
Optimal threshold for improved/high PRO physical function based on SF-12 physical component score
Recognizing a common threshold has communication advantages for public health applications, we further investigated the predictive ability of both MV-total thresholds for each functional outcome. Specifically, we evaluated if evidence supported a conceptually easier 45 minutes/week target for a common MV-total threshold. Table 3 illustrates the threshold predictive ability of MV-total >45 minutes/week compared to MV-total >47 minutes/week to distinguish improved/high gait speed identical (relative risk: 1.8 versus 1.8) or PRO physical function (relative risk: 1.4 versus 1.4). The similar performance across the functional outcomes tested supports a common MV-total >45 minute threshold to predict subsequent improved/high function.
DISCUSSION
The primary finding from this longitudinal study of adults with lower limb joint symptoms (n=1647) supports a minimum threshold of 45 minutes/week physical activity of MV-total activity to improve low function or sustain high function over two years. Attaining this evidence-based threshold better predicted improved/high function in gait speed and PRO physical function than current federal physical activity threshold and represents a less stringent standard than current guidelines (i.e., MV-bout ≥ 150 minutes/week). For adults with lower limb joint symptoms who often do little or no moderate activity, a less demanding physical activity target tied to function may be a valuable intermediate benchmark towards meeting the current physical activity guideline.
To our knowledge, this is the first study to investigate aerobic physical activity thresholds related to functional outcomes for adults living with lower limb joint symptoms. Evidence supporting the World Health Organization and US physical activity guidelines for adults was initially based on consensus of evidence for cardiovascular benefits related to the 150 MV-bout minute/week threshold.37 An extensive literature now supports broad morbidity and mortality benefits of meeting this guideline. A systematic literature review concluded engaging in recommended levels of physical activity could reduce the risk of developing cardiovascular disease, stroke, hypertension, colon and breast cancer, type 2 diabetes, and osteoporosis based on the most methodologically sound studies.38 Moreover, guideline adherence could result in 20% or greater reduced risk for premature all-cause mortality among adults with chronic disease.38–40 Despite strong evidence for meeting current physical activity guidelines to support cardiovascular health and a wide range of potential health benefits for the general adult population, many adults with mobility limiting conditions fail to achieve this goal. Fewer than 11% US adults with knee OA achieve current physical activity guidelines.41 This problem motivates investigating potential intermediate thresholds related to different health benefits, to encourage adults with lower joint symptoms to pursue physical activity.
Being physically active can improve function and reduce joint symptoms among adults with lower limb conditions. Randomized clinical trials demonstrate the benefit of physical activity programs to improve physical function in adults with lower limb conditions, including hip and knee osteoarthritis. 42–45 Non-structured moderate activity such as walking can improve function, and reduce symptomatic pain, fatigue, and stiffness among adults with rheumatic disease.46,47
Longitudinal studies support a dose response relationship between physical activity and function. A systematic review of the long-term effect of physical activity among older adults having knee pain found no evidence of worsened symptoms related to pain, loss of physical function or progression in structural disease.48 One case control study concluded that increasing levels of regular physical activity was associated with lower risk of disease progression to total knee replacement.49 Adults with mobility limiting conditions such as knee osteoarthritis who achieved current physical activity guidelines by engaging in low impact physical activity, experienced substantial improvement in physical function, pain, and quality of life. Although the benefits from physical activity to improve function are recognized, the minimum time commitment needed to experience health benefits is not known.50
Physical activity decreases with older age. Physical activity studies of adults based on objective accelerometer monitoring indicate only 10–15% of community dwelling adults meet national guidelines even after adjusting for age-related decline in physical activity capacity.6,51 This reality combined with a dose-response relationship between physical activity and health motivates clinical advice not to abandon guidelines, but to encourage older adults to pursue achievable incremental increases in physical activity.52 People who endure symptomatic joint disease often have a more difficult time being physically active than the general population and are at elevated risk for functional loss.53 Needed for this large population group is evidence to specify the amount and the intensity of physical activity associated with good functional outcomes.
Our study directly addressed the need for an evidence-based threshold for adults with lower limb symptoms by identifying physical activity metrics and thresholds which best predicted improved function or maintenance of high functional ability over a two year period. A big data approach using classification prediction trees identified a minimum threshold of 45 total minutes physical activity of at least moderate intensity acquired over one week predicted improved/high function in both objectively measured and PRO physical function. Sensitivity analyses indicated these MV-total thresholds were stable independent of sex, BMI, the presence of knee OA and age. This evidence-based threshold predicting good functional outcomes is different from the current guideline in two ways. First, the selected MV-total metric captured all weekly time spent in activities of at least moderate intensity as opposed to the legacy metric which included only MV activity time acquired in bouts lasting at least 10 minutes. For people with lower extremity symptoms, the removal of the 10-minute bouted constraint is a realistic step forward to increase activity levels in a symptomatic population, because those symptoms can inhibit deconditioned people (like those with joint issues) from being able to sustain 10 minutes of MV physical activity. Second, the evidence-based threshold requires a lower physical activity dose (i.e., fewer weekly minutes of MV activity) than current guidelines. The identified evidence-based MV-total>45 minutes/week threshold related to improved/high function is less stringent than the current aerobic guideline, but does not replace the current guideline which supports many other health benefits.
Strengths of the study included prospective data collection across multiple sites, the large sample size, the objective assessment of physical activity, and the age and sex diversity of this cohort. Study limitations need to be considered in interpreting results. The OAI sample does not represent the general population. The present sample was composed of adults with lower limb joint symptoms from a cohort having or at high risk for developing knee osteoarthritis. This sample may include a larger proportion of adults with symptomatic knees than the general population with lower limb symptoms, which may influence the generalizability of these results. However, the intentional stratified OAI recruitment produced a diverse cohort across age and sex. Although OAI ascertainment of hip symptoms used a longer time frame than foot, ankle, or knee symptom ascertainment, 90% of people reporting hip symptoms would be in the sample solely due to their additional report of other lower limb joints. It is notable physical activity thresholds held within subgroups with and without radiographic evidence of knee osteoarthritis, supporting the robustness of these findings to disease status. Although an important methodological strength is the objective measurement of physical activity using accelerometers, it is recognized the accelerometers used cannot capture water activities and may underestimate activities with minimal vertical acceleration/deceleration, such as cycling. However, time spent in these activities was negligible. It is acknowledged other outcome definitions may yield different thresholds and unreported treatments or factors may influence outcomes. Causation cannot be inferred from these observational data. Further research is warranted to confirm these findings
CONCLUSION
The current study supports an intermediate threshold to spend at least 45 minutes/week in accumulated physical activity of at least moderate intensity among adults having lower limb joint symptoms. This threshold to support improved/high function represents a less demanding goal than current federal physical activity guideline in two ways. First, all time spent in MV activities contributes to attaining this function-related minimum threshold in contrast to the current MV-bout threshold which is only met through activity acquired in bouts lasting at least 10 minutes. Second, a minimum of 45 minutes/week may represent a more feasible activity goal than the current physical activity guideline of 150 minutes/week. Success in meeting the MV-total threshold of 45 minutes/week increased the likelihood of functional preservation in high functioning persons and functional improvement in those with functional limitations, providing an intermediate goal towards achieving the current aerobic physical activity guideline.
Significance and Innovation.
These results support an intermediate threshold to spend at least 45 minutes/week in accumulated physical activity of at least moderate intensity among adults having lower limb joint symptoms.
This evidence-based threshold is less rigorous than federal guidelines (≥150 MV-bout minutes/week).
Acknowledgments
Grant Support: This study is supported in part by National Institute for Arthritis and Musculoskeletal Diseases (grant no. R01- AR054155, P60-AR064464, R21-AR068500, T32-AR007611-13).
The authors thank participants from the Osteoarthritis Initiative. This study is supported in part by National Institute for Arthritis and Musculoskeletal Diseases (grant no. 2 R01- AR054155, P60-AR064464, R21-AR068500, T32-AR007611-13), This report from original data utilized the Osteoarthritis Initiative public data which is available at http://oai.epi-ucsf.org/datarelease/DataClinical.asp. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health or the Osteoarthritis Initiative.
References
- 1.Department of Health and Human Services. 2008 Physical Activity Guidelines for Americans. Washington DC: Department of Health and Human Services USA; 2008. [Google Scholar]
- 2.World Health Organization. Global recommendations on physical activity for health. Geneva Switzerland: WHO Press; 2010. pp. 15–35. [PubMed] [Google Scholar]
- 3.Pate RR, Pratt M, Blair SN, et al. Physical activity and public health. A recommendation from the Centers for Disease Control and Prevention and the American College of Sports Medicine 5. JAMA: the journal of the American Medical Association. 1995;273:402–7. doi: 10.1001/jama.273.5.402. [DOI] [PubMed] [Google Scholar]
- 4.Church TS, Earnest CP, Skinner JS, Blair SN. Effects of different doses of physical activity on cardiorespiratory fitness among sedentary, overweight or obese postmenopausal women with elevated blood pressure: a randomized controlled trial. JAMA: the journal of the American Medical Association. 2007;297:2081–91. doi: 10.1001/jama.297.19.2081. [DOI] [PubMed] [Google Scholar]
- 5.Bates JH, Serdula MK, Khan LK, Jones DA, Macera CA, Ainsworth BE. Intensity of physical activity and risk of coronary heart disease 23. JAMA: the journal of the American Medical Association. 2001;285:2973. author reply 4. [PubMed] [Google Scholar]
- 6.Jefferis BJ, Sartini C, Lee IM, et al. Adherence to physical activity guidelines in older adults, using objectively measured physical activity in a population-based study. BMC Public Health. 2014;14:382. doi: 10.1186/1471-2458-14-382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Troiano RP, Berrigan D, Dodd KW, Masse LC, Tilert T, McDowell M. Physical activity in the United States measured by accelerometer. Medicine and science in sports and exercise. 2008;40:181–8. doi: 10.1249/mss.0b013e31815a51b3. [DOI] [PubMed] [Google Scholar]
- 8.Fontaine KR, Heo M, Bathon J. Are US adults with arthritis meeting public health recommendations for physical activity? Arthritis and rheumatism. 2004;50:624–8. doi: 10.1002/art.20057. [DOI] [PubMed] [Google Scholar]
- 9.Shih M, Hootman JM, Kruger J, Helmick CG. Physical activity in men and women with arthritis National Health Interview Survey, 2002. American journal of preventive medicine. 2006;30:385–93. doi: 10.1016/j.amepre.2005.12.005. [DOI] [PubMed] [Google Scholar]
- 10.Abellan van Kan G, Rolland Y, Andrieu S, et al. Gait speed at usual pace as a predictor of adverse outcomes in community-dwelling older people an International Academy on Nutrition and Aging (IANA) Task Force. J Nutr Health Aging. 2009;13:881–9. doi: 10.1007/s12603-009-0246-z. [DOI] [PubMed] [Google Scholar]
- 11.Cesari M, Kritchevsky SB, Newman AB, et al. Added value of physical performance measures in predicting adverse health-related events: results from the Health, Aging And Body Composition Study. Journal of the American Geriatrics Society. 2009;57:251–9. doi: 10.1111/j.1532-5415.2008.02126.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ostir GV, Kuo YF, Berges IM, Markides KS, Ottenbacher KJ. Measures of lower body function and risk of mortality over 7 years of follow-up. American journal of epidemiology. 2007;166:599–605. doi: 10.1093/aje/kwm121. [DOI] [PubMed] [Google Scholar]
- 13.Rosano C, Newman AB, Katz R, Hirsch CH, Kuller LH. Association between lower digit symbol substitution test score and slower gait and greater risk of mortality and of developing incident disability in well-functioning older adults. Journal of the American Geriatrics Society. 2008;56:1618–25. doi: 10.1111/j.1532-5415.2008.01856.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Keeler E, Guralnik JM, Tian H, Wallace RB, Reuben DB. The impact of functional status on life expectancy in older persons. The journals of gerontology Series A, Biological sciences and medical sciences. 2010;65:727–33. doi: 10.1093/gerona/glq029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jinks C, Jordan K, Croft P. Osteoarthritis as a public health problem: the impact of developing knee pain on physical function in adults living in the community: (KNEST 3) Rheumatology. 2007;46:877–81. doi: 10.1093/rheumatology/kem013. [DOI] [PubMed] [Google Scholar]
- 16.Stenholm S, Koster A, Valkeinen H, et al. Association of Physical Activity History With Physical Function and Mortality in Old Age. The journals of gerontology Series A, Biological sciences and medical sciences. 2015 doi: 10.1093/gerona/glv111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Feinglass J, Thompson JA, He XZ, Witt W, Chang RW, Baker DW. Effect of physical activity on functional status among older middle-age adults with arthritis. Arthritis and rheumatism. 2005;53:879–85. doi: 10.1002/art.21579. [DOI] [PubMed] [Google Scholar]
- 18.Ip EH, Church T, Marshall SA, et al. Physical activity increases gains in and prevents loss of physical function: results from the lifestyle interventions and independence for elders pilot study. The journals of gerontology Series A, Biological sciences and medical sciences. 2013;68:426–32. doi: 10.1093/gerona/gls186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Nevitt MC, Sharma L. OMERACT workshop radiography session 1 Osteoarthritis and cartilage/OARS. Osteoarthritis Research Society. 2006;14(Suppl A):A4–9. doi: 10.1016/j.joca.2006.02.020. [DOI] [PubMed] [Google Scholar]
- 20.Eckstein F, Wirth W, Nevitt MC. Recent advances in osteoarthritis imaging--the osteoarthritis initiative. Nat Rev Rheumatol. 2012;8:622–30. doi: 10.1038/nrrheum.2012.113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sharma L, Cahue S, Song J, Hayes K, Pai YC, Dunlop D. Physical functioning over three years in knee osteoarthritis: role of psychosocial, local mechanical, and neuromuscular factors. Arthritis and rheumatism. 2003;48:3359–70. doi: 10.1002/art.11420. [DOI] [PubMed] [Google Scholar]
- 22.Mallen CD, Peat G, Thomas E, Lacey R, Croft P. Predicting poor functional outcome in community-dwelling older adults with knee pain: prognostic value of generic indicators. Annals of the rheumatic diseases. 2007;66:1456–61. doi: 10.1136/ard.2006.067975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Thomas E, Peat G, Mallen C, et al. Predicting the course of functional limitation among older adults with knee pain: do local signs, symptoms and radiographs add anything to general indicators? Annals of the rheumatic diseases. 2008;67:1390–8. doi: 10.1136/ard.2007.080945. [DOI] [PubMed] [Google Scholar]
- 24.Wright A, Hannon J, Hegedus EJ, Kavchak AE. Clinimetrics corner: a closer look at the minimal clinically important difference (MCID) J Man Manip Ther. 2012;20:160–6. doi: 10.1179/2042618612Y.0000000001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Matthews CE, Ainsworth BE, Thompson RW, Bassett DR., Jr Sources of variance in daily physical activity levels as measured by an accelerometer. Medicine and science in sports and exercise. 2002;34:1376–81. doi: 10.1097/00005768-200208000-00021. [DOI] [PubMed] [Google Scholar]
- 26.Semanik P, Song J, Chang RW, Manheim L, Ainsworth B, Dunlop D. Assessing physical activity in persons with rheumatoid arthritis using accelerometry. Medicine and science in sports and exercise. 2010;42:1493–501. doi: 10.1249/MSS.0b013e3181cfc9da. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Song J, Semanik P, Sharma L, et al. Assessing physical activity in persons with knee osteoarthritis using accelerometers: Data from the Osteoarthritis Initiative. Arthritis care & research. 2010;62:1724–32. doi: 10.1002/acr.20305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Peterfy C, Li J, Zaim S, et al. Comparison of fixed-flexion positioning with fluoroscopic semi-flexed positioning for quantifying radiographic joint-space width in the knee: test-retest reproducibility. Skeletal Radiol. 2003;32:128–32. doi: 10.1007/s00256-002-0603-z. [DOI] [PubMed] [Google Scholar]
- 29.Pepe MS. The Statistical Evaluation of Medical Tests of Classification and Prediction. New York: Oxford University Press; 2004. The receiver operating curve for continuous tests; pp. 66–76. [Google Scholar]
- 30.DeLong ER, DeLong DM, Clarke-Pearson DL. Comparing the areas under two or more correlated receiver operating characteristic curves: a nonparametric approach. Biometrics. 1988;44:837–45. [PubMed] [Google Scholar]
- 31.Breiman L, Friedman JH, Oshen RA, Stone CJ. Classification and Regression Trees. Monterey, CA: Wadsworth & Brooks; 1984. [Google Scholar]
- 32.Esposito F, Malerva D, Semeraro G. Lecture Notes in Computer Science. London: Springer-Verlag; 1993. Decision tree prining as a search in the state space; pp. 165–84. [Google Scholar]
- 33.Pencina MJ, D’Agostino RB, Sr, D’Agostino RB, Jr, Vasan RS. Evaluating the added predictive ability of a new marker: from area under the ROC curve to reclassification and beyond. Statistics in medicine. 2008;27:157–72. doi: 10.1002/sim.2929. discussion 207–12. [DOI] [PubMed] [Google Scholar]
- 34.Cook NR. Use and misuse of the receiver operating characteristic curve in risk prediction. Circulation. 2007;115:928–35. doi: 10.1161/CIRCULATIONAHA.106.672402. [DOI] [PubMed] [Google Scholar]
- 35.Salford Systems. CART. 7.0 ed. San Diego CA: Salford Systems; 2008. [Google Scholar]
- 36.Hogan JW, Roy J, Korkontzelou C. Handling drop-out in longitudinal studies. Statistics in medicine. 2004;23:1455–97. doi: 10.1002/sim.1728. [DOI] [PubMed] [Google Scholar]
- 37.Haskell WL, Lee IM, Pate RR, et al. Physical activity and public health: updated recommendation for adults from the American College of Sports Medicine and the American Heart Association. Medicine and science in sports and exercise. 2007;39:1423–34. doi: 10.1249/mss.0b013e3180616b27. [DOI] [PubMed] [Google Scholar]
- 38.Warburton DE, Charlesworth S, Ivey A, Nettlefold L, Bredin SS. A systematic review of the evidence for Canada’s Physical Activity Guidelines for Adults. The international journal of behavioral nutrition and physical activity. 2010;7:39. doi: 10.1186/1479-5868-7-39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Wessel TR, Arant CB, Olson MB, et al. Relationship of physical fitness vs body mass index with coronary artery disease and cardiovascular events in women. JAMA: the journal of the American Medical Association. 2004;292:1179–87. doi: 10.1001/jama.292.10.1179. [DOI] [PubMed] [Google Scholar]
- 40.Katzmarzyk PT, Church TS, Blair SN. Cardiorespiratory fitness attenuates the effects of the metabolic syndrome on all-cause and cardiovascular disease mortality in men. Archives of internal medicine. 2004;164:1092–7. doi: 10.1001/archinte.164.10.1092. [DOI] [PubMed] [Google Scholar]
- 41.Dunlop DD, Song J, Semanik PA, et al. Objective physical activity measurement in the osteoarthritis initiative: Are guidelines being met? Arthritis and rheumatism. 2011;63:3372–82. doi: 10.1002/art.30562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Fransen M, McConnell S, Harmer AR, Van der Esch M, Simic M, Bennell KL. Exercise for osteoarthritis of the knee: a Cochrane systematic review. British journal of sports medicine. 2015;49:1554–7. doi: 10.1136/bjsports-2015-095424. [DOI] [PubMed] [Google Scholar]
- 43.Juhl C, Christensen R, Roos EM, Zhang W, Lund H. Impact of exercise type and dose on pain and disability in knee osteoarthritis: a systematic review and meta-regression analysis of randomized controlled trials. Arthritis Rheumatol. 2014;66:622–36. doi: 10.1002/art.38290. [DOI] [PubMed] [Google Scholar]
- 44.Uthman OA, van der Windt DA, Jordan JL, et al. Exercise for lower limb osteoarthritis: systematic review incorporating trial sequential analysis and network meta-analysis. Bmj. 2013;347:f5555. doi: 10.1136/bmj.f5555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Messier SP, Mihalko SL, Legault C, et al. Effects of intensive diet and exercise on knee joint loads, inflammation, and clinical outcomes among overweight and obese adults with knee osteoarthritis: the IDEA randomized clinical trial. JAMA: the journal of the American Medical Association. 2013;310:1263–73. doi: 10.1001/jama.2013.277669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Escalante Y, Garcia-Hermoso A, Saavedra JM. Effects of exercise on functional aerobic capacity in lower limb osteoarthritis: a systematic review. Journal of science and medicine in sport/Sports Medicine Australia. 2011;14:190–8. doi: 10.1016/j.jsams.2010.10.004. [DOI] [PubMed] [Google Scholar]
- 47.Callahan LF, Shreffler JH, Altpeter M, et al. Evaluation of group and self-directed formats of the Arthritis Foundation’s Walk With Ease Program. Arthritis care & research. 2011;63:1098–107. doi: 10.1002/acr.20490. [DOI] [PubMed] [Google Scholar]
- 48.Quicke JG, Foster NE, Thomas MJ, Holden MA. Is long-term physical activity safe for older adults with knee pain?: a systematic review Osteoarthritis and cartilage/OARS. Osteoarthritis Research Society. 2015;23:1445–56. doi: 10.1016/j.joca.2015.05.002. [DOI] [PubMed] [Google Scholar]
- 49.Manninen P, Riihimaki H, Heliovaara M, Suomalainen O. Physical exercise and risk of severe knee osteoarthritis requiring arthroplasty. Rheumatology. 2001;40:432–7. doi: 10.1093/rheumatology/40.4.432. [DOI] [PubMed] [Google Scholar]
- 50.Paterson DH, Warburton DE. Physical activity and functional limitations in older adults: a systematic review related to Canada’s Physical Activity Guidelines. The international journal of behavioral nutrition and physical activity. 2010;7:38. doi: 10.1186/1479-5868-7-38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Tucker JM, Welk GJ, Beyler NK. Physical activity in U.S: adults compliance with the Physical Activity Guidelines for Americans. American journal of preventive medicine. 2011;40:454–61. doi: 10.1016/j.amepre.2010.12.016. [DOI] [PubMed] [Google Scholar]
- 52.Sparling PB, Howard BJ, Dunstan DW, Owen N. Recommendations for physical activity in older adults. Bmj. 2015;350:h100. doi: 10.1136/bmj.h100. [DOI] [PubMed] [Google Scholar]
- 53.Voelker R. Few adults with knee osteoarthritis meet national guidelines for physical activity. JAMA: the journal of the American Medical Association. 2011;306:1428–30. doi: 10.1001/jama.2011.1388. [DOI] [PubMed] [Google Scholar]