Abstract
Traditional fee-for-service (FFS) Medicare’s prospective payment systems for postacute care provide little incentive to coordinate care or control costs. In contrast, Medicare Advantage plans pay for postacute care out of monthly capitated payments and thus have stronger incentives to use it efficiently. We compared the use of postacute care in skilled nursing and inpatient rehabilitation facilities by enrollees in Medicare Advantage and FFS Medicare after hospital discharge for three high-volume conditions: lower extremity joint replacement, stroke, and heart failure. After accounting for differences in patient characteristics at discharge, we found lower intensity of postacute care for Medicare Advantage patients compared to FFS Medicare patients discharged from the same hospital, across all three conditions. Medicare Advantage patients also exhibited better outcomes than their FFS Medicare counterparts, including lower rates of hospital readmission and higher rates of return to the community. These findings suggest that payment reforms such as bundling in FFS Medicare may reduce the intensity of postacute care without adversely affecting patient health.
Medicare’s spending on postacute care for beneficiaries with traditional fee-for-service (FFS) coverage was $59.2 billion in 2014, representing approximately 10 percent of Medicare’s total expenditures.[1] Postacute care includes short-term rehabilitation, skilled nursing, and other services provided to patients after their discharge from a hospital and may be provided by an inpatient rehabilitation facility, a skilled nursing facility, a long-term care hospital, or a home health agency.
Numerous commentators have noted that Medicare’s separate prospective payment systems for FFS Medicare beneficiaries provide limited financial incentive to make judicious use of postacute care, with regard to both overall use and choice of setting.[2–4] This problem is exacerbated by the limited clinical evidence about when and how postacute care should be used. For example, patients can receive intensive rehabilitation in either a skilled nursing facility or an inpatient rehabilitation facility. Skilled nursing facilities receive per diem payments while inpatient rehabilitation facilities receive a single payment per discharge, and the overall level of payment for an episode of care is typically higher at an inpatient rehabilitation facility than in a skilled nursing facility.[5]
Patients admitted to the two types of facilities may differ on average, reflecting their clinical needs and the rehabilitation they are able to tolerate (inpatient rehabilitation facility patients must be able to tolerate three hours of therapy a day[6]). However, the optimal clinical setting for some patients is unknown, reflecting in part mixed evidence on the relative effects of inpatient rehabilitation facility versus skilled nursing facility care on outcomes.[5,7] In the absence of clear clinical guidelines for such patients, nonclinical considerations such as payment incentives may play a stronger role]—for example, when hospitals and postacute care providers are under common ownership, there may be an incentive to refer patients to the postacute care provider owned by the hospital. In other cases, there may be too little consideration of costs when deciding on postacute setting for these patients. Once admitted to a skilled nursing facility, per diem payments provide little incentive to limit the length-of-stay, while single episode payments for inpatient rehabilitation facilities produce incentives for shorter stays.
The percentage of Medicare beneficiaries enrolled in private Medicare Advantage health plans has nearly doubled in the past decade, from 16 percent in 2006 to 31 percent in 2015.[8] Medicare Advantage plans negotiate contracts with providers of postacute care and pay for their services out of the monthly capitated payments the plans receive for each covered enrollee. Medicare Advantage plans also have a greater ability to manage enrollees’ use of postacute care compared to FFS Medicare. Unlike FFS Medicare, Medicare Advantage plans can restrict enrollees’ choice of providers.[9] Previous research has shown that Medicare Advantage plans may require prior authorization for postacute care and require enrollees to use a preferred network of “high value” providers of the care.[10] Medicare Advantage enrollees also face higher cost sharing for skilled nursing facility care and hospitalizations, compared to FFS Medicare beneficiaries with supplemental coverage.[11]
These payment structures may lead to differences in the overall use and intensity of postacute care between Medicare Advantage and FFS Medicare enrollees. Historically under FFS Medicare, a hospital had limited financial incentives to influence the location of a patient’s postacute care or its length-of-stay, or to coordinate care to avoid a readmission to the hospital—though this is changing with the Hospital Readmissions Reduction Program and new payment models such as accountable care organizations (ACOs) and bundled payments. In contrast, Medicare Advantage plans benefit financially from avoiding unnecessary use of postacute care and hospital readmissions, and thus they have an interest in carefully selecting and coordinating postdischarge care. These incentives could result in too little use of postacute care, which could be detrimental to patient outcomes. However, there is little evidence on differences between Medicare Advantage and FFS Medicare in the overall use of postacute care and associated patient outcomes.
Understanding differences between Medicare Advantage and FFS Medicare enrollees in the use of postacute care is important, given current Medicare payment reforms. First, Medicare Advantage enrollment continues to grow, and some politicians have proposed changing Medicare to a system of “premium support,” which would further shift beneficiaries from traditional Medicare FFS payment to capitated plans with payment incentives similar to those in Medicare Advantage.[12] Second, with the adoption of new payment models such as bundled payments and ACOs, Medicare is increasingly shifting financial responsibility for postacute care and accountability on quality performance to hospitals and other entities. An unanswered question is whether these changes in financial incentives will lead to more efficient use of such care. Examining Medicare Advantage’s experience is informative, because although the specific payment structures differ for Medicare Advantage plans and the recipients of bundled payments, both entities pay for postdischarge care out of a fixed payment from Medicare.
We compared Medicare Advantage enrollees and FFS Medicare beneficiaries in terms of their use of inpatient rehabilitation and skilled nursing facilities and their outcomes. To determine a potential mechanism for differences in post-acute care use and intensity and patient outcomes, we investigated whether hospitals discharged Medicare Advantage patients to fewer postacute providers than was the case with FFS Medicare patients, potentially indicating use of limited networks of preferred providers (as described above).
We focused on hospital discharges between January 2011 and June 2013 for three high-volume conditions with varying use of postacute care: lower extremity joint replacement, stroke, and heart failure. We investigated lower extremity joint replacement because it is the focus of Medicare’s mandatory bundled payment program, it often requires physical therapy, and it is one of the thirteen conditions that must account for 60 percent of a facility’s case load for that facility to qualify as an inpatient rehabilitation facility and receive a higher Medicare payment rate for a stay than an acute care hospital does.[6,13,14] Stroke is another of the thirteen qualifying conditions for inpatient rehabilitation facilities, and stroke patients may require physical rehabilitation, speech therapy, and occupational therapy. Finally, heart failure contrasts with the other two conditions because it is treated medically and is not a qualifying condition for inpatient rehabilitation facilities.
Our analysis excluded two postacute care settings, long-term care hospitals and home health care. Long-term care hospitals are less commonly used than other postacute care settings: There were only thirty-seven long-term care hospital cases—compared to a hundred inpatient rehabilitation facility cases—per 10,000 FFS Medicare beneficiaries in 2013.[1] Home health care is used more widely than long-term care hospitals (9 percent of FFS Medicare beneficiaries received home health care in 2013). However, it is less intensive and costly than care at an inpatient rehabilitation or skilled nursing facility, with average episode payments of under $3,000 in 2014, compared to average case payments of $18,632 at inpatient rehabilitation facilities.[1]
Study Data And Methods
Study Population
We focused on hospitals that received disproportionate-share or medical education payments from Medicare and thus were required to submit information-only claims to Medicare for stays by Medicare Advantage enrollees starting in 2008.[15,16] This is important as Medicare Advantage claims are not generally available in standard Medicare claims data sources. Compared to hospitals that did not receive these payments, the hospitals that did were larger and more likely to be teaching centers, and they accounted for 92 percent of Medicare discharges in the period 2011–13 (online Appendix Exhibit 1).[17] For the hospitals in our sample, we identified “index” discharges that occurred between January 2011 and June 2013 for lower extremity joint replacement, stroke, or heart failure.[18] We defined episodes for our analysis as an index hospitalization and a ninety-day postdischarge period. We excluded episodes in which patients were admitted directly from nursing homes.
Data Sources
We identified hospital discharges in the Medicare Provider Analysis and Review File. We linked discharges with information on Medicare coverage and other beneficiary information from the Master Beneficiary Summary File. Since postacute care facilities are required to submit patient assessments to Medicare for both Medicare Advantage and FFS Medicare patients, we used assessments in the Minimum Data Set to identify skilled nursing facility stays and assessments in the Inpatient Rehabilitation Facility Patient Assessment Instrument to identify inpatient rehabilitation facility stays. We obtained hospital-level information from the Provider of Services File, Hospital Compare, and Hospital Cost Reports.
Study Measures
We determined whether beneficiaries were continuously enrolled in traditional FFS Medicare (that is, Parts A and B) or in Medicare Advantage from the month before the index discharge through the end of the postdischarge episode, and we excluded the small percentage of episodes in which coverage was not continuously Medicare Advantage or FFS Medicare. We used a series of clinical controls including the specific Medicare Severity-Diagnosis Related Group recorded on the index hospital discharge, comorbidity indicators from the list of diagnoses for the index hospitalization, and condition-specific severity measures.[19,20] We identified beneficiaries’ sex, age, race and ethnicity, whether or not they were also covered by Medicaid, and eligibility for the Part D low-income subsidy.
Measures of use of skilled nursing and inpatient rehabilitation facilities were whether a patient had an admission to one of the facilities and the number of days spent in each type of facility. Our construction of measures of use of skilled nursing facilities is described in more detail in the Appendix.[17] Hospitalization measures were length-of-stay for the index hospitalization and whether there were any readmissions to the hospitals in our sample within thirty or ninety days of the index discharge.
We established community residence in each day of the ninety-day postdischarge episode by determining whether an individual was in a hospital in our sample, a skilled nursing facility, an inpatient rehabilitation facility, or a long-term nursing home or had died. Using these daily locations, we constructed indicators for whether beneficiaries were in the community for the full ninety days following discharge, for the full period following an initial postacute care discharge (if we observed an admission to an inpatient rehabilitation or skilled nursing facility), and at the end of the episode (day 90).
We did not observe Medicare Advantage admissions to long-term care hospitals, critical access hospitals, or acute care hospitals that were not required to submit Medicare Advantage claims (explained above). Given that only a small percentage of Medicare patients were admitted to such facilities, this was unlikely to substantially affect our results.[21]
We constructed measures of hospital referral patterns to skilled nursing and inpatient rehabilitation facilities separately for enrollees in FFS Medicare and Medicare Advantage. First, we pooled episodes across the conditions in our sample. In this analysis we included only hospitals with five or more discharges to skilled nursing or inpatient rehabilitation facilities for both FFS Medicare and Medicare Advantage enrollees. For each hospital, we calculated the number of unique providers of postacute care to which it referred patients. We also constructed measures to capture whether hospitals referred patients to few or many providers of postacute care. We calculated the share of each hospital’s patients discharged to each inpatient rehabilitation facility or skilled nursing facility. We used these shares to construct two hospital-level measures: the maximum share of patients from each hospital referred to any single provider of postacute care, and a concentration index based on the sum of squared shares of each provider. This index ranged from zero to one, with values closer to one indicating that postacute care was more concentrated in fewer providers for the given hospital.
Additional details on our construction of episodes of care and study measures are presented in the Appendix.[17]
Empirical Approach
We performed cross-sectional analyses, comparing episodes of care following hospital discharges for patients with Medicare Advantage and FFS Medicare coverage. One potential concern was positive selection into Medicare Advantage instead of FFS Medicare, since historically Medicare Advantage enrollees were healthier than FFS Medicare beneficiaries.[22] To investigate the presence of positive selection, we compared both groups of patients in terms of demographic characteristics (sex, age, and race and ethnicity), socioeconomic status (Medicaid enrollment and eligibility for the Part D low-income subsidy), and clinical status (comorbidities listed for the index hospital stay and condition-specific severity measures).
We used linear regression to test whether differences between Medicare Advantage and FFS Medicare enrollees] were significant after adjusting for the discharging hospital (by including indicators for hospitals) and the specific Medicare Severity-Diagnosis Related Group.
In our main analysis, we compared Medicare Advantage and FFS Medicare patients in terms of use of inpatient rehabilitation and skilled nursing facilities, hospital readmission, measures of community residence, and mortality. To account for differences in patient characteristics between the two groups, we estimated linear regressions that adjusted for demographic characteristics, socioeconomic status, and clinical status (described above) and the Medicare Severity-Diagnosis Related Group from the initial hospital stay. To account for differences in the hospitals from which the two groups of patients were discharged, our main regression specifications also adjusted for the discharging hospital. Thus, our estimated differences reflected within-hospital differences in postacute care received by enrollees in Medicare Advantage and FFS Medicare. We also adjusted for the quarter year of the index hospital discharge, to account for secular trends in use of postacute care. Finally, we clustered standard errors at the level of the hospital referral region level, to account for the correlation of regression model errors within geographic markets.[23]
Next, we estimated what the change in Medicare spending would be for FFS Medicare episodes if use of postacute care and readmissions were set at Medicare Advantage levels. First, we calculated hospital-level average FFS Medicare payment rates for skilled nursing facility and inpatient rehabilitation facility episodes and readmissions (for more details about this calculation, see the Appendix).[17] We constructed measures of predicted FFS Medicare costs for FFS Medicare and Medicare Advantage patients by multiplying each episode’s utilization by the average hospital-level FFS Medicare payment rate for each setting. Then, we used the linear regression specification described above, including hospital indicator variables, to estimate adjusted differences in Medicare costs between Medicare Advantage and FFS Medicare patients. Thus, the adjusted differences represent the average of within-hospital differences in predicted Medicare costs between Medicare Advantage and FFS Medicare patients and illustrate the potential savings to Medicare if FFS Medicare patients used Medicare Advantage levels of postdischarge care.
Finally, we explored the concentration of referrals across providers of postacute care as a potential explanation for differences between Medicare Advantage and FFS Medicare patients in use of that care and outcomes. We investigated the presence of differing referral patterns for Medicare Advantage and FFS Medicare patients within each hospital, specifically comparing the number of unique skilled nursing facilities and inpatient rehabilitation facilities to which each hospital referred patients, the maximum skilled nursing facility and inpatient rehabilitation facility share, and the hospital-specific skilled nursing facility and inpatient rehabilitation facility concentration indices for Medicare Advantage and FFS Medicare patients. By comparing the two groups of patients at each hospital, we held constant the availability of postacute care.
If there were fewer Medicare Advantage than FFS Medicare patients at a hospital discharged to inpatient rehabilitation or skilled nursing facilities, the minimum possible concentration index for Medicare Advantage patients would be higher than the minimum possible concentration index for FFS Medicare patients. We accounted for this by estimating linear regressions that adjusted for the specific volume of Medicare Advantage and FFS Medicare patients discharged to inpatient rehabilitation or skilled nursing facilities using a quadratic function (that is, controlling for volume and squared volume).
Limitations
Our study had several limitations. First, we assumed that, after observable patient characteristics were controlled for, estimated differences in use of postacute care and outcomes between Medicare Advantage and FFS Medicare patients were driven by differences in how Medicare Advantage plans provide postacute care compared to FFS Medicare, independent of patient characteristics. However, enrollees in Medicare Advantage and FFS Medicare may differ in unobserved attributes that might also affect the provision of postacute care and other outcomes.
Second, we included only care at a hospital, inpatient rehabilitation facility, or skilled nursing facility in our analysis. Medicare Advantage patients may have received home health care, outpatient visits, and other services that offset some of the differences in institutional care between them and FFS Medicare patients.
Third, differences in intensity of postacute care could have affected measures of functional status that were less extreme than community residence, but that we did not observe for all patients discharged from acute care hospitals.
Study Results
Characteristics Of Patients
We identified 1,023,899 episodes for lower extremity joint replacement, 536,333 episodes for stroke, and 877,851 episodes for heart failure. After excluding episodes with index hospital admissions from nursing homes, discontinuous Medicare Advantage or FFS Medicare coverage, or any missing data, we retained 95 percent (968,936) of lower extremity joint replacement episodes, 90 percent (481,074) of stroke episodes, and 87 percent (762,228) of heart failure episodes (Exhibit 1). Across the conditions in our sample, Medicare Advantage patients accounted for 25–27 percent of episodes. Focusing on the adjusted differences comparing FFS Medicare and Medicare Advantage patients, Medicare Advantage patients were more likely to be male (except for joint replacement), slightly younger (0.6–1.2 years across conditions), less likely to be non-Hispanic whites, and more likely to be non-Hispanic blacks.
Exhibit 1.
Characteristics of Medicare Advantage (MA) and fee-for-service (FFS) Medicare enrollees discharged from the hospital by condition, January 2011–June 2013
| Lower extremity joint replacement | Stroke | Heart failure | |||||||
|---|---|---|---|---|---|---|---|---|---|
| MA mean | FFS mean | Adjusted difference | MA mean | FFS mean | Adjusted difference | MA mean | FFS mean | Adjusted difference | |
| Episodes | 259,111 | 709,825 | 130,395 | 350,679 | 192,518 | 569,710 | |||
| Demographic characteristics | |||||||||
| Male (%) | 34.4% | 34.7% | −0.0 | 44.1% | 42.5% | 1.8** | 46.5% | 44.8% | 2.0** |
| Age (years) | 74.9 | 75.3 | −0.6** | 78.7 | 79.6 | −1.1** | 79.8 | 80.7 | −1.2** |
| Non-Hispanic white | 84.3% | 89.2% | −3.6** | 72.9% | 80.2% | −5.5** | 71.8% | 79.1% | −5.4** |
| Non-Hispanic black | 6.9 | 5.1 | 2.5** | 14.7 | 11.3 | 4.4** | 16.2 | 12.5 | 4.6** |
| Socioeconomic status | |||||||||
| Covered by Medicaid | 9.7 | 9.2 | 0.8 | 17.2 | 18.4 | −0.8 | 20.5 | 22.1 | −1.1 |
| Eligible for Part D low-income subsidy | 13.1 | 11.4 | 2.3** | 23.7 | 22.8 | 1.7** | 27.9 | 27.3 | 1.7 |
| Clinical status | |||||||||
| Comorbidities | 1.6 | 1.6 | −0.04** | 2.0 | 2.0 | −0.01 | 2.8 | 2.8 | 0.0 |
| Diabetes (%) | 19.5% | 19.8% | 0.9** | 28.7% | 28.2% | 2.2** | 33.9% | 34.0% | 2.3** |
| Diabetes with complications | 3.1 | 1.8 | 0.3** | 7.0 | 4.8 | 0.8** | 12.0 | 8.6 | 1.0** |
| Obese | 16.2 | 13.8 | 1.0** | 7.5 | 6.5 | 0.9** | 15.4 | 13.7 | 1.8** |
| Depression | 10.7 | 11.3 | −0.3** | 9.0 | 9.9 | −0.5** | 8.8 | 9.7 | −0.7** |
| Hypertension | 74.4 | 74.1 | 0.0 | 86.7 | 85.8 | 0.9** | 74.9 | 73.0 | 0.7** |
| Chronic lung disease | 15.5 | 15.6 | −0.4** | 15.4 | 15.6 | 0.2 | 37.3 | 38.0 | 0.8** |
| Condition-specific severity | |||||||||
| Morbid obesity | 4.0% | 3.7% | 0.3** | ||||||
| Lower extremity fracture | 13.4 | 15.4 | −2.1** | ||||||
| Osteoarthritis | 83.8 | 81.9 | 2.1** | ||||||
| Hemorrhagic stroke | 12.3% | 12.3% | −0.7** | ||||||
| Chronic heart failure | 1.8% | 1.8% | −0.1** | ||||||
| Acute heart failure (diastolic) | 29.3 | 29.4 | −0.9** | ||||||
| Acute heart failure (systolic) | 28.0 | 27.3 | 0.5** | ||||||
| Acute heart failure (combined systolic and diastolic) | 8.1 | 8.5 | −0.2** | ||||||
SOURCE Authors’ analysis of data on hospital discharges in the period January 2011–June 2013 from the Medicare Master Beneficiary Summary File and Provider Analysis and Review File
NOTES Adjusted differences include Medicare Severity-Diagnosis Related Group and hospital fixed effects. Standard errors were clustered at the level of the hospital referral region. For lower extremity joint replacement, 26.7 percent of the episodes were for MA enrollees, and 73.2 percent were for FFS Medicare enrollees. For stroke, the shares were 27.1 percent and 72.9 percent, respectively. For heart failure, the shares were 25.3 percent and 74.7 percent, respectively.
p < 0.05
Among joint replacement and stroke patients, Medicare Advantage enrollees were more likely than FFS Medicare enrollees to be eligible for the Part D low-income subsidy. Across the three conditions, Medicare Advantage and FFS Medicare patients exhibited similar numbers of comorbidities on the index hospital claim, but Medicare Advantage patients were more likely than FFS Medicare patients to be diagnosed with diabetes and obesity and less likely to be diagnosed with depression. Differences were mixed for hypertension and chronic lung disease.
Among joint replacement patients, those with Medicare Advantage were slightly more likely than those with FFS Medicare to be morbidly obese (which complicates rehabilitation). Medicare Advantage patients were 2 percentage points more likely than FFS Medicare patients to receive a joint replacement for osteoarthritis (instead of for a fracture, in which case joint replacement is more urgent and complex). Compared to FFS Medicare patients, Medicare Advantage stroke patients were less likely to have a hemorrhagic stroke, and Medicare Advantage heart failure patients were less likely to present with combined systolic and diastolic heart failure.
Overall, we did not find large differences between FFS Medicare and Medicare Advantage patients, nor did we find that the condition of Medicare Advantage patients was systematically less severe than that of FFS Medicare patients. Thus, it is unlikely that differences in the composition of the Medicare Advantage and FFS Medicare patient populations explained the differences in use of postacute care and postdischarge outcomes that we document below.
Postacute Care By Source Of Coverage
Among lower extremity joint replacement patients, 42.4 percent of Medicare Advantage patients were admitted to skilled nursing facilities, compared to 40.4 percent of FFS Medicare patients (Exhibit 2). However, Medicare Advantage patients spent 19.7 days in these facilities conditional on admission (that is, just including patients with a skilled nursing facility stay), compared to 24.0 days for FFS Medicare patients. After we adjusted for patient characteristics and the discharging hospital (using hospital fixed effects), we found that—compared to FFS Medicare enrollees—Medicare Advantage enrollees were 2.0 percentage points more likely to be admitted to a skilled nursing facility but stayed 3.2 fewer days in the facility conditional on admission, leading to 0.8 fewer skilled nursing facility days overall (that is, unconditional on admission, including patients with no skilled nursing facility days).
Exhibit 2.
Hospital stays, use of postacute care, and outcomes for Medicare Advantage (MA) and fee-for-service (FFS) Medicare enrollees
| Lower extremity joint replacement | Stroke | Heart failure | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Mean | Mean | Mean | |||||||
| MA | FFS | Adjusted difference | MA | FFS | Adjusted difference | MA | FFS | Adjusted difference | |
| Episodes | 259,111 | 709,825 | —a | 130,395 | 350,679 | —a | 192,518 | 569,710 | —a |
| Length of initial hospitalization (days) | 3.52 | 3.60 | 0.04** | 4.50 | 4.54 | 0.11** | 4.43 | 4.60 | −0.02 |
| Skilled nursing facility | |||||||||
| Any use | 42.4% | 40.4% | 2.0** | 32.6% | 33.6% | 0.6 | 19.4% | 21.9% | −0.7** |
| Days (conditional on admission) | 19.7 | 24.0 | −3.2** | 36.1 | 40.7 | −3.5** | 27.6 | 30.1 | −1.7** |
| Days (unconditional) | 8.4 | 9.7 | −0.8** | 11.8 | 13.7 | −1.0** | 5.4 | 6.6 | −0.5** |
| Inpatient rehabilitation facility | |||||||||
| Any use | 3.7% | 11.0% | −6.4** | 17.4% | 24.8% | −7.2** | 0.8% | 2.8% | −1.8** |
| Days (conditional on admission) | 11.5 | 11.4 | −0.2 | 16.2 | 16.2 | 0.1 | 12.9 | 12.9 | −0.2 |
| Days (unconditional) | 0.4 | 1.3 | −0.7** | 2.8 | 4.0 | −1.2** | 0.1 | 0.4 | −0.2** |
| Skilled nursing or inpatient rehabilitation facility | |||||||||
| Any use | 45.5% | 49.5% | −3.3** | 44.7% | 49.8% | −3.7** | 20.0% | 23.9 | −2.1** |
| Hospital readmissions postdischarge | |||||||||
| Within 30 days | 5.5% | 6.2% | −0.4** | 11.9% | 12.8% | −0.9** | 19.3% | 21.0% | −1.7** |
| Within 90 days | 10.2 | 11.5 | −0.8** | 21.5 | 23.6 | −1.9** | 36.1 | 39.3 | −3.2** |
| In the community postdischarge | |||||||||
| For 90 days postdischarge | 50.7% | 46.2% | 3.7** | 40.6% | 34.6% | 3.9** | 50.0% | 45.5% | 3.1** |
| Continuously following postacute discharge | 77.4 | 74.7 | 1.2** | 44.4 | 40.3 | 2.9** | 23.9 | 23.2 | 0.7** |
| At end of 90-day episode | 95.8 | 94.2 | 0.8** | 76.9 | 71.5 | 2.9** | 79.2 | 76.1 | 1.7** |
| Mortality during episode | 1.6 | 1.9 | −0.0 | 13.6 | 15.0 | 0.3 | 13.6 | 14.4 | 0.1 |
SOURCE Authors’ analysis of data on hospital discharges for the period January 2011–June 2013 from the Medicare Master Beneficiary Summary File, Provider Analysis and Review File, Minimum Data Set, and the Inpatient Rehabilitation Facility Patient Assessment Instrument.
NOTES Adjusted differences include Medicare Severity-Diagnosis Related Group and patient demographic characteristics, socioeconomic status, and clinical status. Standard errors were clustered at the level of the hospital referral region. “Days (conditional on admission)” indicates average days in a facility among patients who were admitted. “Days (unconditional)” indicates average days in a facility across all patients.
[Please provide].
p < 0.05
Only 3.7 percent of Medicare Advantage joint replacement patients were admitted to inpatient rehabilitation facilities, compared to 11.0 percent of FFS Medicare patients. Adjusted differences show that Medicare Advantage patients were 6.4 percentage points less likely than FFS Medicare patients to be admitted to such a facility, but the two groups of patients had similar lengths-of-stay conditional on admission.
Medicare Advantage patients were 3.3 percentage points less likely than FFS Medicare patients to be admitted to any postacute care facility (either a skilled nursing or an inpatient rehabilitation facility). Differences in use of postacute care were not explained by the length of the index hospitalization, which was very similar across the two groups of patients.
Differences in use of postacute care between Medicare Advantage and FFS Medicare stroke patients were similar to those we found for joint replacement patients. Compared to FFS Medicare patients, Medicare Advantage patients had a similar probability of admission to a skilled nursing facility and shorter stays conditional on admission. The probability of admission to an inpatient rehabilitation facility was higher for both Medicare Advantage and FFS Medicare stroke patients (17.4 and 24.8 percent, respectively), compared to joint replacement patients, but the difference between Medicare Advantage and FFS Medicare patients was similar for both joint replacement and stroke.
Medicare Advantage heart failure patients were less likely to be admitted to a skilled nursing facility and stayed at those facilities for fewer days, compared to FFS Medicare patients. As expected, use of inpatient rehabilitation facilities was uniformly low among heart failure patients.
Readmissions And Return To The Community By Source Of Coverage
Among joint replacement patients, 5.5 percent of Medicare Advantage enrollees were readmitted to the hospital within thirty days, compared to 6.2 percent of FFS Medicare patients (Exhibit 2). After we adjusted for patient characteristics and the discharging hospital, we found that Medicare Advantage enrollees were 0.4 percentage points less likely than FFS Medicare enrollees to be readmitted within thirty days and 0.8 percentage points less likely to be to be readmitted within ninety days. Compared to FFS Medicare patients, Medicare Advantage patients were 3.7 percentage points more likely to remain in the community continuously following the initial hospital discharge, 1.2 percentage points more likely to remain in the community following discharge from a postacute provider, and 0.8 percentage point more likely to reside in the community at the end of the episode. Mortality during the episode did not differ between the two groups of patients.
When we compared stroke patients and joint replacement patients, we found that both thirty- and ninety-day readmission rates were higher for stroke patients and that there were larger differences between Medicare Advantage and FFS Medicare patients in the case of stroke. As in the case of joint replacement, Medicare Advantage patients were more likely than FFS Medicare patients to return to the community after a stroke but exhibited no significant difference in mortality. Heart failure patients exhibited similar patterns to those of stroke patients.
We performed sensitivity analyses for the adjusted differences in Exhibit 2 that did not include hospital fixed effects and that included beneficiaries who shifted between FFS Medicare and Medicare Advantage coverage during an episode. Overall, we found a similar pattern of results in each case. For a discussion of these findings, see the Appendix; for the results, see Appendix Exhibit 2.[17]
FFS Medicare Savings With Medicare Advantage Levels Of Use
If FFS Medicare patients had the same patterns of postacute care use and readmissions as Medicare Advantage patients did, Medicare would realize per episode savings of $1,455 for joint replacement, $2,397 for stroke, and $1,143 for heart failure (Exhibit 3). Full estimates are presented in Appendix Exhibit 3.[17] Relative to the total projected post-discharge spending for Medicare FFS patients using average hospital-level FFS payments, this represents a 16 percent reduction in post-discharge spending averaged across the three conditions.
Exhibit 3.
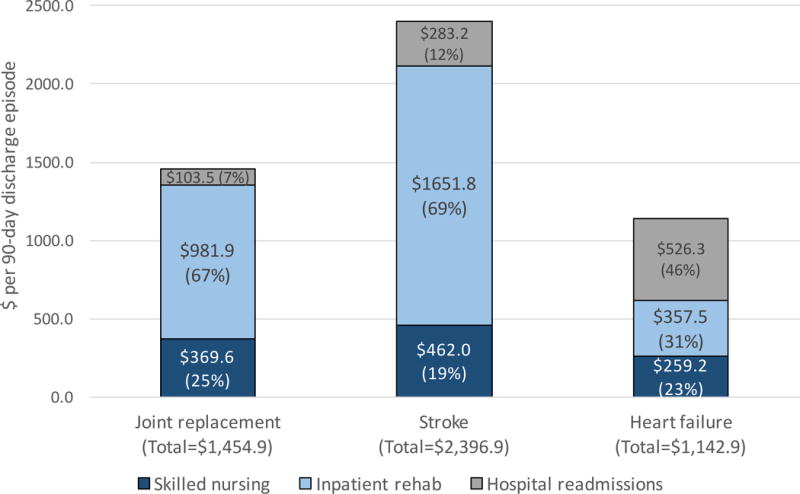
Estimated savings in spending per episode of postacute care if fee-for-service (FFS) Medicare patients used Medicare Advantage levels of postdischarge care
Source/Notes: SOURCE Authors’ analysis of hospital discharges for the period January 2011–June 2013 from the Medicare Master Beneficiary Summary File, Provider Analysis and Review File, Minimum Data Set, and the Inpatient Rehabilitation Facility Patient Assessment Instrument. NOTES The savings are for per ninety-day postdischarge episode, using hospital-specific FFS Medicare payment rates (per day for skilled nursing facility and per episode for inpatient rehabilitation and hospital readmission). “Joint replacement” is lower extremity joint replacement.
Inpatient rehabilitation was the most important component of spending for joint replacement and stroke. Readmission was the most important component for heart failure.
Referral Patterns
On average, the hospitals in our sample discharged Medicare Advantage patients to sixteen skilled nursing facilities and FFS Medicare patients to thirty facilities (Exhibit 4). Some, but not all, of this difference can be explained by the higher volume of FFS Medicare discharges, compared to Medicare Advantage discharges. The hospital-level maximum skilled nursing facility share and the concentration index were both slightly higher for Medicare Advantage patients than for FFS Medicare patients, even when the volume of the two groups of patients sent to skilled nursing facilities was adjusted for. Overall, this evidence suggests that Medicare Advantage patients were concentrated into fewer skilled nursing facilities than FFS Medicare patients. Within-hospital inpatient rehabilitation facility referral patterns were also slightly more concentrated for Medicare Advantage patients, compared to FFS Medicare patients.
Exhibit 4.
Hospital-level patterns of referral to skilled nursing and inpatient rehabilitation facilities for Medicare Advantage (MA) and fee-for-service (FFS) Medicare enrollees
| Referrals to: | MA patients | FFS patients | Adjusted difference |
|---|---|---|---|
| Skilled nursing facility | |||
| Average number of referred facilities, across hospitals | 16.1 | 29.6 | −4.3 |
| Average number of patients discharged to facilities, across hospitals | 84.6 | 226.7 | —a |
| Maximum share of patients from hospital referred to any single facility, average across hospitals | 37.4% | 35.7% | 2.1 |
| Concentration index | 0.24 | 0.22 | 0.03 |
| Inpatient rehabilitation facility | |||
| Average number of referred facilities, across hospitals | 2.8 | 5.6 | −1.2 |
| Average number of patients discharged to facilities, across hospitals | 26.8 | 125.8 | —a |
| Maximum share of patients from hospital referred to any single facility, average across hospitals | 82.3% | 80.6% | 3.1 |
| Concentration index | 0.75 | 0.72 | 0.05 |
SOURCE Authors’ analysis of data on postacute provider referrals after hospitalizations for lower extremity joint replacement, stroke, and heart failure, including hospital discharges from January 2011–June 2013 from the Medicare Master Beneficiary Summary File, Provider Analysis and Review File, Minimum Data Set, and the Inpatient Rehabilitation Facility Patient Assessment Instrument.
NOTES The adjusted difference is the average within-hospital difference between MA and FFS patients, adjusting for the volume of MA and FFS patients admitted to each facility type (as a quadratic function). All adjusted differences were significant (p < 0.05). Standard errors were clustered at the level of the hospital referral region. The sample included 2,212 hospitals that referred at least five Medicare Advantage and FFS Medicare patients to skilled nursing facilities, and 1,176 hospitals that referred at least five Medicare Advantage and FFS Medicare patients to inpatient rehabilitation facilities. The concentration index is explained in the text; values closer to 1.00 indicate that postacute care was more concentrated (that is, hospitals referred patients to fewer providers), while values closer to 0.00 indicate that the care was less concentrated.
Discussion
After adjusting for patient characteristics, we found that Medicare beneficiaries with Medicare Advantage coverage were less likely than those with FFS Medicare coverage to be admitted to inpatient rehabilitation facilities and had shorter lengths-of-stay in skilled nursing facilities, and this difference existed between Medicare Advantage and FFS Medicare beneficiaries discharged from the same hospital. Among the patients in our sample, there was little evidence that FFS Medicare patients were systematically sicker than Medicare Advantage patients based on observable characteristics. This suggests that lower use of postacute care by Medicare Advantage enrollees was not driven by favorable selection. In addition, we did not find that Medicare Advantage patients were adversely affected by lower use of postacute care, as they also exhibited lower probability of hospital readmission and higher rates of return to the community, compared to FFS patients. Overall, these differences imply that Medicare could reduce postdischarge costs by approximately 16 percent per episode across the conditions in our sample if FFS Medicare patients received the same treatment as Medicare Advantage patients did.
We also found some evidence that Medicare Advantage patients were concentrated in fewer skilled nursing facilities than FFS Medicare patients were. Recent research has shown that Medicare Advantage plans manage enrollees’ use of postacute care through requiring prior authorization and limiting coverage to preferred networks of “high value” providers of postacute care, while FFS Medicare entities such as ACOs are more restricted in managing referrals to postacute care.[10] In addition, previous research has shown that hospitals with closer linkages with skilled nursing facilities experience lower readmission rates.[24] Thus, Medicare Advantage plans’ ability to more actively manage the postacute care used by their enrollees, in part through more selective referral networks for that care, may be one explanation for our findings.
We were unable to examine intermediate measures of functional status that might be affected by differences in levels of postacute care between Medicare Advantage and FFS Medicare patients. More research is needed to understand whether reducing inpatient rehabilitation facility use and skilled nursing facility lengths-of-stay would affect specific aspects of patients’ functional status. Narrow networks of postacute care providers could adversely affect patients’ choice of providers. In addition, we cannot rule out the possibility that our results were driven in part by differences in unobserved severity of condition between Medicare Advantage and FFS Medicare patients.
Conclusion
Medicare is shifting away from FFS reimbursement of postacute care providers, with an increasing share of its beneficiaries electing Medicare Advantage coverage and its adoption of payment reforms such as bundled payment. Our results suggest that such payment changes may reduce the intensity of postacute care, both through changes in setting and reductions in lengths-of-stay. Our finding that, compared to FFS Medicare patients, Medicare Advantage patients exhibited lower readmissions and higher rates of return to the community suggests that such reductions in postacute care intensity may not adversely affect patient health.
Supplementary Material
Acknowledgments
An earlier version of this article was presented previously at the American Society of Health Economics Biennial Meeting, Philadelphia, Pennsylvania, June 13, 2016 and at the AcademyHealth Annual Research Meeting, Boston, Massachusetts, June 28, 2016.
This work was funded by the National Institute on Aging (Grant No. R01 AG-046838).
Biographies
Bio 1: Peter J. Huckfeldt (huckfeld@umn.edu) is an assistant professor in the Division of Health Policy and Management, School of Public Health, at the University of Minnesota, in Minneapolis.
Bio 2: José J. Escarce is a professor of medicine in the David Geffen School of Medicine at the University of California, Los Angeles.
Bio 3: Brendan Rabideau is a research programmer at the Leonard D. Schaeffer Center for Health Policy and Economics at the University of Southern California, in Los Angeles.
Bio 4: Pinar Karaca-Mandic is an associate professor in the Division of Health Policy and Management, School of Public Health, at the University of Minnesota.
Bio 5: Neeraj Sood is a professor and vice dean for research at the Sol Price School for Public Policy and director of research at the Schaeffer Center for Health Policy and Economics, both at the University of Southern California.
Notes
- 1.Medicare Payment Advisory Commission. A data book: health care spending and the Medicare program [Internet] Washington (DC): MedPAC; 2016. Jun, http://www.medpac.gov/docs/default-source/data-book/june-2016-data-book-health-care-spending-and-the-medicare-program.pdf. [cited 2016 Nov 17]. Available from: [Google Scholar]
- 2.Mechanic RE. Post-acute care—the next frontier for controlling Medicare spending. N Engl J Med. 2014;370(8):692–4. doi: 10.1056/NEJMp1315607. [DOI] [PubMed] [Google Scholar]
- 3.Chandra A, Dalton MA, Holmes J. Large increases in spending on postacute care in Medicare point to the potential for cost savings in these settings. Health Aff (Millwood) 2013;32(5):864–72. doi: 10.1377/hlthaff.2012.1262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Newhouse JP, Garber AM. Geographic variation in Medicare services. N Engl J Med. 2013;368(16):1465–8. doi: 10.1056/NEJMp1302981. [DOI] [PubMed] [Google Scholar]
- 5.Medicare Payment Advisory Commission. Report to the Congress: Medicare and the health care delivery system [Internet] Washington (DC): MedPAC; 2014. Jun, [cited 2016 Nov 17]. Chapter 6: site-neutral payments for select conditions treated in inpatient rehabilitation facilties and skilled nursing facilities. Available from: http://www.medpac.gov/docs/default-source/reports/chapter-6-site-neutral-payments-for-select-conditions-treated-in-inpatient-rehabilitation-facilities.pdf?sfvrsn=0. [Google Scholar]
- 6.Medicare Payment Advisory Commission. Inpatient rehabilitation facilities payment system [Internet] Washington (DC): MedPAC; [revised 2016 Oct cited 2016 Nov 17]. Available from: http://www.medpac.gov/docs/default-source/payment-basics/medpac_payment_basics_16_irf_final.pdf?sfvrsn=0. [Google Scholar]
- 7.Buntin MB, Colla CH, Deb P, Sood N, Escarce JJ. Medical spending and outcomes after postacute care for stroke and hip fracture. Med Care. 2010;48(9):776–84. doi: 10.1097/MLR.0b013e3181e359df. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jacobson G, Damico A, Neuman T, Gold M. Medicare Advantage 2015 spotlight: enrollment market update [Internet] Menlo Park (CA): Henry J. Kaiser Family Foundation; 2015. Jun 30, [cited 2016 Nov 17]. (Issue Brief). Available from: http://kff.org/medicare/issue-brief/medicare-advantage-2015-spotlight-enrollment-market-update/ [Google Scholar]
- 9.Medicare Payment Advisory Commission. Medicare Advantage program payment system [Internet] Washington (DC): MedPAC; [revised 2016 Oct cited 2016 Nov 27]. Available from: http://medpac.gov/docs/default-source/payment-basics/medpac_payment_basics_16_ma_final.pdf?sfvrsn=0. [Google Scholar]
- 10.Medicare Payment Advisory Commission. Report to the Congress: Medicare payment policy [Internet] Washington (DC): MedPAC; 2015. Mar, [cited 2016 Nov 17]. Chapter 7: Medicare’s post-acute care: trends and ways to rationalize payments. Available from: http://www.medpac.gov/docs/default-source/reports/chapter-7-medicare-s-post-acute-care-trends-and-ways-to-rationalize-payments-march-2015-report-.pdf?sfvrsn=0. [Google Scholar]
- 11.Keohane LM, Grebla RC, Mor V, Trivedi AN. Medicare Advantage members’ expected out-of-pocket spending for inpatient and skilled nursing facility services. Health Aff (Millwood) 2015;34(6):1019–27. doi: 10.1377/hlthaff.2014.1146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Jacobson G, Neuman T. Turning Medicare into a premium support system: frequently asked questions [Internet] Menlo Park (CA): Henry J. Kaiser Family Foundation; 2016. Jul 19, [cited 2016 Nov 17]. (Issue Brief). Available from: http://kff.org/medicare/issue-brief/turning-medicare-into-a-premium-support-system-frequently-asked-questions/ [Google Scholar]
- 13.Press MJ, Rajkumar R, Conway PH. Medicare’s new bundled payments: design, strategy, and evolution. JAMA. 2016;315(2):131–2. doi: 10.1001/jama.2015.18161. [DOI] [PubMed] [Google Scholar]
- 14.The lower extremity joint replacement cases in our sample are nonbilateral. For a nonbilateral joint replacement, a patient must be morbidly obese or age eighty-five or older to count toward the 60 percent criterion.
- 15.Medicare Learning Network. Capturing days on which Medicare beneficiaries are entitled to Medicare Advantage (MA) in the Medicare/Supplemental Security Income (SSI) fraction. MLN Matters [serial on the Internet] 2007 Jul 20; [cited 2016 Nov 17]. Available from: https://www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNMattersArticles/downloads/MM5647.pdf.
- 16.Research Data Assistance Center. Medicare managed care enrollees and the Medicare utilization files [Internet] Minneapolis (MN): ResDAC; 2011. Jun 1, [cited 2016 Nov 17]. Available from: https://www.resdac.org/resconnect/articles/114. [Google Scholar]
- 17.To access the Appendix, click on the Appendix link in the box to the right of the article online.
- 18.We identified these discharges by the use of Medicare Severity-Diagnosis Related Group numbers 469–70 for lower extremity joint replacement 61–66 for stroke, and 291–93 for heart failure.
- 19.Elixhauser A, Steiner C, Harris DR, Coffey RM. Comorbidity measures for use with administrative data. Med Care. 1998;36(1):8–27. doi: 10.1097/00005650-199801000-00004. [DOI] [PubMed] [Google Scholar]
- 20.The condition-specific severity measures were morbid obesity and a principal diagnosis of lower extremity fracture for joint replacement, whether a stroke was hemorrhagic, and whether a heart failure admission was due to chronic or acute heart failure (and if acute, whether the presentation was defined as diastolic, systolic, or combined diastolic and systolic).
- 21.According to the Medicare Payment Advisory Commission’s 2016 data book (see Note 1), 3.4 percent of Medicare hospital discharges were from critical access hospitals in 2014. The hospitals in our sample captured 92 percent of the discharges from short-term acute care hospitals (that is, those that were not critical access hospitals). Finally, only 121,532 FFS Medicare enrollees were admitted to long-term care hospitals in 2013
- 22.Newhouse JP, Price JA, Huang J, McWilliams JM, Hsu J. Steps to reduce favorable risk selection in Medicare Advantage largely succeeded, boding well for health insurance exchanges. Health Aff (Millwood) 2012;31(12):2618–28. doi: 10.1377/hlthaff.2012.0345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Dartmouth Institute for Health Policy and Clinical Practice. The Dartmouth atlas of health care: data by region [Internet] Lebanon (NH): The Institute; c2016. [cited 2016 Nov 18]. Available from: http://www.dartmouthatlas.org/data/region/ [Google Scholar]
- 24.Rahman M, Foster AD, Grabowski DC, Zinn JS, Mor V. Effect of hospital-SNF referral linkages on rehospitalization. Health Serv Res. 2013;48(6 Pt1):1898–919. doi: 10.1111/1475-6773.12112. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


