Abstract
Objectives
To calculate the prevalence of all falls, non-accidental falls and syncope in an older population and characterize cardiovascular risk profiles.
Design
Prospective, longitudinal cohort study.
Setting
The first two waves of data from the Irish Longitudinal Study on Ageing (TILDA).
Participants
8172 community-dwelling adults aged 50 years and older resident in the Republic of Ireland
Measurements
Self-reported history of all falls, non-accidental falls and syncope in the year preceding the first two waves of data collection. Demographic factors and self-reported cardiovascular conditions were used to characterize cardiovascular risk profiles.
Results
The prevalence of all falls in the past year was 19.2% or 192 per thousand persons and increased with age (50–64 years 17.5%; 65–74 years 19.4%; 75+ years 24.4%). Non-accidental falls had an estimated prevalence of 5.1% or 51 falls per thousand persons and accounted for 26.5% of all falls reported and also increased with age (50–64 years 4.0%; 65–74 years 5.5%; 75+ years 8.0%). The prevalence for syncope was estimated to be 4.4% or 44per thousand persons but did not show a similar age gradient. Participants with at least 5 cardiovascular conditions were more likely to report all falls (OR = 2.07, 95% CI 1.18–3.64, p<0.05) and NAF (OR = 2.89, 95%CI 1.28–6.52, p<0.05).
Conclusions
The prevalence of all falls and non-accidental falls increases with age but the same pattern was not consistently observed for syncope. There is an increased odds of reporting all three outcomes with increasing number of self-reported cardiovascular conditions. Further work is needed to uncover the interplay between cardiovascular disease and subsequent falls.
Introduction
Falls and syncope are common in older adults. Currently, falls account for 4% of the healthcare budget while syncope accounts for 1–2% of all emergency department (ED) presentations per year in the United States [1, 2]. Given projected changes in global demographics and advancing age, the management of falls and syncope and their consequences will become even more pertinent in the near future[3].
Falls frequently occur due to the environment or accidental events such as trips or slips [4]. These accidental falls become more common with advancing age and are often due to age and disease associated reductions in physical, sensory and cognitive function which make an individual more susceptible to environmental hazards[4].
However, some falls are not accidental but rather are due to drops in blood pressure which may lead to either balance instability or, in some cases, loss of consciousness i.e. syncope[5]. Similar to syncope, non-accidental falls (NAF) have been linked to cardiovascular disorders with a possible common causal pathway and overlap[6]. Dynamic changes in blood pressure with higher rates of orthostatic hypotension have been associated with an increased risk of NAF and injurious falls in community-dwelling adults [7]. Disorders which are known to cause syncope in the elderly including vaso-vagal syncope and carotid sinus syndrome occur in up to 25% of NAF [8, 9] [10–12]. In addition to shared cardiovascular associations there is a higher reported prevalence of depression in patients with both NAF and syncope[13, 14]. Despite the overlap, falls, NAF and syncope are generally reported separately, therefore studies which distinguish between them and examine them in more depth are required [15].
We hypothesise that the prevalence of all falls, NAF and syncope increase with age and share common demographic and cardiovascular risk factors. In order to show this, we calculated the prevalence of all reported falls, NAF and syncope in a population study of community-dwelling adults aged 50 years and over and examined the demographic and cardiovascular health variables associated with all falls, NAF and syncope.
Methods
Sample
This study utilised the first two waves of data from The Irish Longitudinal Study on Ageing (TILDA). TILDA is a prospective cohort study of the social, economic and health circumstances of community-dwelling adults aged 50 years and older resident in the Republic of Ireland. The sampling procedure and the study design have been described in detail previously [16, 17]. Briefly, the sampling frame was the Irish Geodirectory, a listing of all residential addresses in the Republic of Ireland. The RANSAM sampling system was used to randomly target households and all household residents aged 50 years or older and their spouse/partner (of any age) were invited to participate in the study. All participants provided written informed consent and ethical approval for the study was granted by the Research Ethics Committee of Trinity College Dublin. All experimental procedures adhered to the Declaration of Helsinki.
The household response rate was 62%, leading to a final wave one sample of 8,172 adults aged 50 and older who completed an in-home interview between October 2009 and February 2011. Follow-up data for wave two were collected between March 2012 and March 2013 (2 year gap between waves). Attrition accounted for a 12% sample reduction and death a further 2.5%.
Data collection involved an in-home computer-aided personal interview conducted by trained social interviewers, a self-completion questionnaire completed and returned by participants in their own time; and a comprehensive health assessment carried out by research nurses in a dedicated health centre or if required, a modified assessment carried out in the participant’s own home. The response rates for the self-completion questionnaire and the health assessment were 85% and 72%, therefore to maximise the sample size, this analysis uses data obtained during the in-home interview only.
Measures
Syncope—Participants were asked if they had experienced a faint or blackout in the past twelve months (yes/no). Syncope was defined as at least one syncopal event in the past year.
All falls—Participants were asked if they had fallen in the past year (yes/no). A fall was defined as at least one reported fall in the last year.
Non-Accidental Falls (NAF)—Participants were asked if any of the falls they had experienced in the last year were non-accidental, i.e. with no apparent or obvious reason (yes/no). A NAF was defined as at least one reported NAF in the last year.
Demographic and Health Status variables—In addition to demographic variables (age and sex), participants were asked to self-report any doctor diagnosed cardiovascular conditions including: hypertension, angina, a heart attack, congestive heart failure, diabetes or high blood sugar, a stroke (cerebral vascular disease), mini-stroke or transient ischaemic attack, high cholesterol, a heart murmur, an abnormal heart rhythm (arrhythmia). Due to small numbers within individual variables, and the potential for overlap, a composite cardiovascular disease exposure variable was generated. This indicator variable for cardiovascular conditions was created by summing the number of conditions.
All medications taken regularly were coded using the World Health Organisation Anatomical Therapeutic Chemical (ATC) Classification system[18]. Anti-hypertensives were identified by ATC codes beginning with C02, C03, C07, C08 or C09. Depressive symptoms were assessed using the 20-item Centre for Epidemiological Studies Depression scale (CES-D)[19] where scores of < 16 indicated insignificant symptoms for depression; >16 and < 26 indicated moderate to severe depressive symptoms and > 26 indicated severe depressive symptoms. All demographic and health variables were obtained at wave one. Unsteadiness during walking was divided into a binary variable based on self-reported steadiness while walking [20].
Statistical analysis
Prevalence estimates were weighted with respect to age, sex and education to the Quarterly National Household Survey (2010) to ensure that data were nationally representative. Incidence at wave 2 was calculated using the sub-sample who did not report a syncopal event or fall in wave 1. An attrition weight was used to adjust for loss to follow-up through participant refusal, loss of contact or death between waves. Cross tabulation was used to estimate prevalence and 95% confidence intervals. Inferential statistics (design-based F statistic, p <0.01) were computed for age and sex estimates using analysis of variance.
To better understand the relationships between basic demographic variables and general health with respect to all falls, NAF and syncope, logistic regression was used, without survey weights with univariate odds ratios calculated. Multivariate logistic regression models were built using causal modelling including age, sex, depressive symptoms, anti-hypertensive drugs, self-reported cardiovascular conditions, and self- reported unsteadiness while walking. A second model was built analysing CVD as a composite number of conditions. Odds ratios, p-values and 95% confidence intervals were used to assess the association with potential risk factors. A p-value <0.05 represented statistical significance. All analyses were conducted using Stata 12.1 Statacorp LP.
Results
The total number of participants aged 50 years and over included in the study was 8,172 (50-65years (n = 4664; 57%), 65–74 years (n = 2159; 26.4%), 75+ years (n = 1352; 16.5%)); mean age 63.7 years (SD 9.7); 55.6% (n = 4,724) female.
Prevalence of all falls, NAF and syncope in the Irish population
Baseline descriptives for groups reporting all falls, NAF and syncope are provided in Table 1.
Table 1. Baseline variables for all participants reporting all falls (n = 1,579), non-accidental falls (NAF)(n = 406) and syncope (n = 363) in wave one of TILDA.
| Variable | Falls N (%) | NAF N (%) | Syncope N(%) |
|---|---|---|---|
| Age (years) | |||
| 50–65 | 882 (56) | 234 (58) | 186 (51) |
| 65–75 | 433 (27) | 105 (26) | 107 (29) |
| 75+ | 264 (17) | 67 (17) | 70 (19) |
| Gender (female) | 919 (58) | 238 (59) | 177 (49) |
| Anti-hypertensive medications1 | 634 (40) | 198 (49) | 169 (47) |
| Unsteadiness2 | 311 (23) | 132 (46) | 72 (24) |
| Number of cardiovascular conditions3 | |||
| 0 | 346 (22) | 70 (17) | 54 (15) |
| 1 | 901 (57) | 236 (58) | 213 (59) |
| 2 | 209 (13) | 63 (16) | 51 (14) |
| 3 | 74 (5) | 15 (4) | 25(7) |
| >3 | 49 (3) | 22 (5) | 20 (6) |
| Depression4 | |||
| None/insignificant | 1006 (64) | 212 (52) | 197 (54) |
| Moderate | 323 (20) | 106 (26) | 82 (23) |
| Severe | 219 (14) | 78 (19) | 75 (21) |
1As coded by the WHO Anatomic Therapeutic Chemical (ATC) Classification System; anti-hypertensive medication with ATC unsteadiness during walking code C02, C03, C07, C08, C09
2Self reported unsteadiness during walking
3Self- reported doctor diagnosed cardiovascular conditions including angina, hypertension, congestive cardiac failure, diabetes, stroke, transient ischemic attack, high cholesterol, cardiac murmurs and cardiac arrhythmia
4 As measured by Centre for Epidemiological Studies scale (CES-D) scale; scores of < 16 indicated insignificant symptoms for depression; >16 and < 26 indicated moderate to severe depressive symptoms and > 26 indicated severe depressive symptoms.
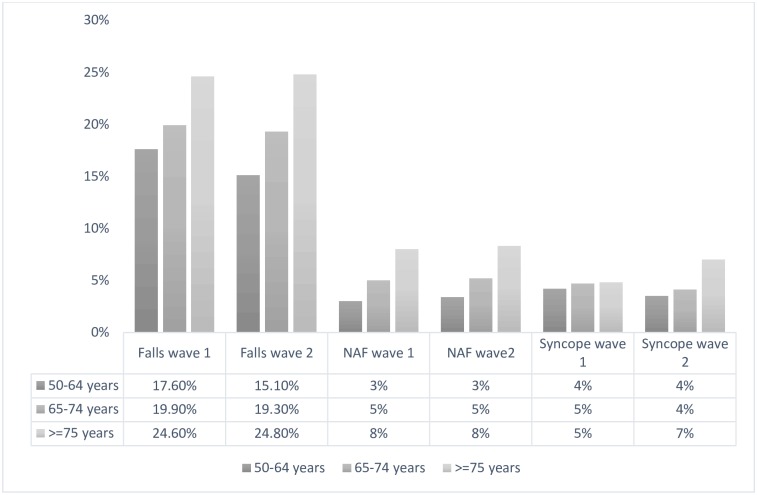
The prevalence (wave 1) and incidence (wave 2) of all falls, NAF and syncope stratified by age is presented in Fig 1. The overall prevalence of all falls in the past year was 19.2% or 192 per thousand persons and increased with age (50–64 years 17.5%; 65–74 years 19.4%; 75+ years 24.4%) (F(2,1240.7) = 15.92, p<0.001). Falls were more prevalent in females (20.1%) compared to males (18.2%).
Fig 1. Prevalence and incidence of all falls, non-accidental falls (NAF) and syncope.
Prevalence (wave one) and incidence (wave two) based on self-reported data from TILDA participants (n = 8172).
NAF had an estimated prevalence of 5.1% or 51 falls per thousand persons and accounted for 26.5% of all falls reported. Again, the prevalence increased with age (50–64 years 4.0%; 65–74 years 5.5%; 75+ years 8.0%) (F(2,1247.3) = 15.15, p<0.001).
The prevalence for syncope was estimated to be 4.4% or 44 per thousand persons (Fig 1). Prevalence was similar for males (4.4%) and females (4.5%) and did not differ when stratified by age in wave one (F(2,1235.8) = 0.87, p< 0.10) (Fig 1).
Incidence
The estimated overall incidence of all falls was 17.5% while NAF was 5%. In both cases, incidence was highest for those aged 75 years and older (all falls 24.8%; NAF 8%) (Fig 1). Overall, the estimated incidence of syncope was 4.2%. There was an age-related increase in incidence, with those over 75 years demonstrating a higher incidence of syncope (50–64 years 3.5%; 65–74 years 4.1%; 75+ years 7%) (F(2,1228.8) = 12.56, p <0.05). The estimated incidence for males aged 75 and older was 5.2% compared to 8.3% in females of the same age.
Clinical characteristics
Tables 2 and 3 illustrate the univariate and multivariate associations between cardiovascular conditions with all falls, NAF and syncope. In univariate analysis, cardiovascular conditions including angina, heart failure, stroke, TIA, diabetes and arrhythmia displayed an association with all three outcomes. When adjusted for potential confounders none of the cardiovascular conditions showed an individual association with all three outcomes. Heart murmur showed an association with all falls 1.35(95% CI 1.07–1.71, p<0.05) and syncope 1.71 (96% CI 1.17–2.52, p<0.05); self reported arrhythmia was associated with all falls 1.30 (95% CI 1.06–1.60, p<0.05) and syncope 1.58 (95% CI 1.13–2.22, p<0.05).
Table 2. Univariate odds ratios (OR) all falls (AF), non- accidental falls (NAF) and syncope in the 12 months prior to wave 1 based on self-reported health variables for TILDA participants (n = 8172).
| Conditions | All Falls OR (95% CI) | Non- accidental Falls OR (95%CI) | Syncope OR (95% CI) |
|---|---|---|---|
| Gender (Female) | 1.02 (0.92–1.14) | 1.05 (0.87–1.29) | 0.70 (0.57–0.86) |
| 50–64 years old | 1.02(0.77–1.37) | 1.28 (0.73–2.27) | 0.93 (0.53–1.62) |
| 65–75 years old | 1.10 (0.82–1.48) | 1.24 (0.69–2.24) | 1.17 (0.66–2.07) |
| Over 75 years old | 1.07 (0.78–1.45) | 1.27 (0.69–2.32) | 1.23 (02.68–2.21) |
| Anti- hypertensive medications1 | 1.10 (0.99–1.24) | 1.57 *(1.30–1.92) | 1.42* (1.16–1.75) |
| Depressive symptoms2 | |||
| Mild | REF | REF | REF |
| Moderate | 1.45* (1.27–1.67) | 2.09* (1.65–2.66) | 1.78 (1.37–2.30) |
| severe | 1.88 *(1.59–2.22) | 3.01* (2.31–3.93) | 2.96 (2.25–3.90) |
| Composite CVD3 | |||
| 0–2 | 1.54* (1.14–2.07) | 1.33* (1.02–1.73) | 0.99 (.87–1.14) |
| 3 to 4 | 3.59* (2.36–5.46) | 1.83* (1.17–2.87) | 1.35* (1.05–1.73) |
| 4 to 5 | 1.69 (0.51–5.58) | 3.78* (1.73–8.25) | 2.24* (1.30–3.85) |
| Unsteadiness4 | 2.74* (2.36–3.19) | 4.73* (3.79–5.89) | 2.22* (1.70–2.91) |
| Self- reported cardiac conditions | |||
| Hypertension | 1.08 (0.96–1.29) | 1.50*(1.23–1.83) | 1.48*(1.20–1.82) |
| Angina | 1.41*(1.13–1.75) | 1.97*(1.40–2.77) | 2.22*(1.58–3.13) |
| Heart attack | 0.98 (0.75–1.27 | 1.2 (0.77–1.87) | 1.78*(1.19–2.65) |
| Heart failure | 1.64* (1.03–2.62) | 2.47* (1.27–4.81) | 2.15*(1.03–4.49) |
| Stroke | 1.87*(1.29–2.71) | 3.50*(2.15–5.69) | 3.94*(2.42–6.41) |
| Diabetes | 1.36*(1.12–1.64) | 1.40*(1.01–1.94) | 1.48*(1.06–2.08) |
| TIA | 1.82* (1.31–2.52) | 2.68*(1.68–4.28) | 2.35*(1.41–3.92) |
| High Cholesterol | 1.11*(1.00–1.24) | 1.21 (0.99–1.48) | 1.20 (0.98–1.49) |
| Heart murmur | 1.56*(1.25–1.96) | 1.45 (0.98–2.16) | 1.98*(1.37–2.88) |
| Arrhythmia | 1.49*(1.23–1.81) | 1.42*(1.01–1.99) | 2.05*(1.51–2.81) |
1Antihypertensive medications (coded by the Anatomic Therapeutic Chemical (ATC) anti-hypertensive medication with ATC code C02, C03, C07, C08, C09)
2Depressive symptoms (as measured by Centre for Epidemiological Studies scale (CES-D) scale with scores of < 16 indicating insignificant symptoms for depression; >16 and < 26 indicating moderate to severe depressive symptoms and > 26 indicating severe depressive symptoms.)
3composite number of self- reported doctor diagnosed cardiac conditions including angina, hypertension, diabetes, stroke, TIA(transient ischemic attack), heart murmur, high cholesterol and cardiac arrhythmia.
4 Self-reported unsteadiness during walking
*Denotes statistical significance at p<0.05
Table 3. Adjusted odds ratios † (OR) with confidence intervals (CI) for all falls (AF), non-accidental falls (NAF) and syncope in the 12 months prior to wave 1 (n = 8172).
| Conditions | All falls OR (95% CI) | Non-accidental Falls OR (95%CI) | Syncope OR (95% CI) |
|---|---|---|---|
| Hypertension | 0.96 (0.81–1.12) | 1.10 (0.83–1.45) | 1.29 (0.97–1.72) |
| Angina | 1.11 (0.87–1.42) | 1.15 (0.79–1.68) | 1.58* (1.08–2.31) |
| Heart attack | 0.84(0.64–1.11) | 0.81 (0.51–1.29) | 1.35 (0.88–2.07) |
| Heart failure | 1.26 (0.78–2.06) | 1.38 (0.68–2.81) | 1.44 (0.67–3.08) |
| Stroke | 1.22 (0.81–1.82) | 1.65 (0.96–2.85) | 2.88*(1.69–4.89) |
| Diabetes | 1.21 (0.99–1.48) | 0.98 (0.69–1.40) | 1.25 (0.88–1.79) |
| TIA (transient ischemic attack) | 1.36 (0.96–1.92) | 1.55(0.94–2.55) | 1.80* (1.05–3.07) |
| High Cholesterol | 1.08 (0.96–1.21) | 1.10 (0.89–1.36) | 1.10 (0.89–1.38) |
| Heart murmur | 1.35*(1.07–1.71) | 1.09 (0.72–1.65) | 1.71*(1.17–2.52) |
| Arrhythmia | 1.30*(1.06–1.60) | 0.94 (0.65–1.34) | 1.58* (1.13–2.22) |
†Based on logistic regression controlling for age, sex, antihypertensives (coded by the Anatomic Therapeutic Chemical (ATC) anti-hypertensive medication with ATC code C02, C03, C07, C08, C09), depressive symptoms (as measured by Centre for Epidemiological Studies scale with scores of < 16 indicating insignificant symptoms for depression; >16 and < 26 indicating moderate to severe depressive symptoms and > 26 indicating severe depressive symptoms.) and Self-reported unsteadiness during walking
*denotes statistical significance at p<0.05
Table 4 presents the results of multivariate analysis using a composite number of CV conditions. Participants with at least 5 cardiovascular conditions were more likely to report all falls (OR = 2.07, 95% CI 1.18–3.64, p<0.05) and NAF (OR = 2.89, 95%CI 1.28–6.52, p<0.05). Having three to four cardiovascular conditions was associated with increased odds of reporting syncope (OR = 2.62, 95% CI 1.65–4.17, p<0.05). Moderate and severe depressive symptoms were associated with a greater likelihood of reporting any falls, NAF and syncope in the past year (Table 4). Self-reported gait instability showed a statistically significant association with all three conditions as well (all falls OR = 2.49, 95% CI 2.13–2.94, NAF OR = 3.78 95% CI 2.97–4.80, syncope OR 1.50 95% CI 1.12–2.01).
Table 4. Multi-variate analysis with odds ratios (OR) of participants reporting all falls (n = 1,579), non-accidental falls (NAF) (n = 406) and syncope (n = 363) in wave one of TILDA (n = 8,172).
| Conditions | All Falls OR (95% CI)† | Non-Accidental Falls OR (95% CI)† | Syncope OR (95% CI)† |
|---|---|---|---|
| Gender (female) | 1.03 (0.93–1.16) | 1.05 (0.85–1.29) | 0.67 (0.54–0.83) |
| AGE | |||
| 50–64 years old | 0.98 (0.73–1.34) | 1.38 (0.76–2.50) | 0.76 (0.43–1.36) |
| 65–75 years old | 1.09 (0.80–1.49) | 1.30 (0.71–2.38) | 0.98 (0.55–1.75) |
| Over 75 years old | 1.08 (0.78–1.49) | 1.29 (0.69–2.40) | 1.04 (0.57–1.89) |
| Anti-hypertensive medication1 | 0.97 (0.85–1.10) | 1.22 (0.97–1.52) | 1.12 (0.89–1.42) |
| Depression2 | |||
| Mild | Ref | Ref | Ref |
| Moderate | 1.35*(1.18–1.56) | 1.86*(1.46–2.36) | 1.70* (1.31–2.20) |
| Severe | 1.54*(1.29–1.83) | 2.17*(1.63–2.87) | 2.54* (1.91–3.39) |
| Composite CVD3 | |||
| 0–2 | 0.92 (0.78–1.07) | 1.18 (0.87–1.59) | 1.22 (0.88–1.71) |
| 3 to 4 | 1.09 (0.82–1.44) | 0.99 (0.60–1.62) | 2.62*(1.65–4.17) |
| 4 to 5 | 1.91*(1.07–3.39) | 2.51*(1.08–5.79) | 1.43 (0.42–4.83) |
| Unsteadiness4 | 2.49*(2.13–2.94) | 3.78*(2.97–4.80) | 1.50*(1.12–2.01) |
† Adjusted for each parameter listed in the model (gender, age group category, depression severity, composite cardiovascular disease (CVD) score and unsteadiness during walking).
1As coded by the World Health Organisation Anatomic Therapeutic Chemical (ATC) antihypertensive medication with ATC code C02, C03, C07, C08, C09.
2As measured by Centre for Epidemiological Studies Depression Scale (CES-D); scores of < 16 indicated insignificant symptoms for depression; >16 and < 26 indicated moderate to severe depressive symptoms and > 26 indicated severe depressive symptoms.
3 composite number of self- reported doctor diagnosed cardiac conditions including angina, hypertension, diabetes, stroke, TIA(transient ischemic attack), heart murmur, high cholesterol and cardiac arrhythmia.
4 Self-reported unsteadiness during walking
CI = confidence interval
*denotes statistical significance with p-value <0.05
Discussion
This paper describes the prevalence of all falls (19.2%), NAF (5.1%) and syncope (4.4%) in the past year in a community-dwelling population aged 50 years and older. The prevalence and incidence of all falls and NAF increases with age but the same pattern was not observed for syncope. There are increased odds of reporting all three conditions with increasing number of self-reported cardiovascular conditions.
We have reported a consistent prevalence and incidence rate of all falls of 19.2%. Other community-based studies have reported higher accidental falls rates of 25–30% when measured retrospectively and 35–40% when measured prospectively [21–26]. The younger average age profile in the first wave of TILDA may account for the lower reported yearly prevalence. Consistent with previous studies, the over 75-year age group represents over 20% of falls reported.
Non-accidental falls (NAF), defined as a fall without any obvious slip or trip accounted for about one quarter of all falls, with those over the age of 75 years twice as likely to report NAF as adults aged 50–64 years (8% versus 4%). This study remains the largest community-based cohort to report on the prevalence of NAF and is consistent with a previously reported prevalence of 5% in community-dwelling older adults in New Zealand. [26–28]. In contrast, between 20–50% of all falls presenting to emergency departments are non-accidental[27], perhaps indicating a high morbidity associated with NAF.
We have been able to show unique prevalence and incidence estimates for syncope in the same population. Our cohort has a lower prevalence of syncope to that reported by the Olmstead community cohort (which also focused on older adults), who reported 16.9% overall [29]. TILDA has demonstrated a consistent rate of syncope occurrence at 4 per 1000 person years in our cohort. The Framingham cohort studies had reported higher cumulative incidence rate of 5.7 per 1000 person years in men aged 60–69 years and had a sharp rise to 11.1% per 1000 person years in men aged 70 years and older[30]. They used a definition of syncope that included transient ischaemic attack, stroke and seizures making it difficult to make direct comparison to our cohort. Although at wave two, we reported an increase in syncope incidence in the over 75 age group, it does not demonstrate the same degree of change as reported in the Framingham cohort. This lack of age variation is also in contrast to all falls and NAF and may represent an under-reporting of syncope in older age groups; or the presentation of syncope as a fall.
Low blood pressure, intermittent arrhythmia and heart failure have all shown associations with falls risk in epidemiological studies[31]. Observational studies also support the link between cardiovascular disease and NAF with higher rates of cardiac arrhythmia and carotid sinus syndrome in participants who report NAF[32, 33]. We have demonstrated that increasing cardiovascular co-morbidity were associated with an increase in reporting NAF adding to the evidence linking cardiovascular disease to NAF. Cardiovascular assessment has been enshrined in the original American Geriatrics Society/British Geriatrics Society guidelines for falls prevention and our data would suggest a continued emphasis on the use of a structured cardiovascular assessment as part of a falls prevention work-up[34]. Given the similarities between NAF and syncope, it is recommended that NAF are managed in the same way as syncope in order to realise beneficial responses to intervention [35, 36].
Strengths and limitations
TILDA provides an opportunity to distinguish between and characterise all falls, NAF and syncope in a large, community-dwelling cohort. Few studies present these together despite the strong overlap between all three. However, there are also some limitations, including the use of self-reported falls and syncope over the past year which relies on a participant’s ability to recall past events leading to recall bias. This may lead to inaccurate reporting of these events when compared to cohorts in which falls are recorded prospectively, for example with falls diaries. Currently, Ireland does not have a unique health identifier which would allow this data to be linked to medical records and therefore, we are unable to clinically verify the final diagnosis and as a result they may suffer from mis-classification bias. Despite this limitation, the cohort is well characterised and will continue to be followed at regular intervals providing a rich source of information as to the exact incidence and associations between falls and syncope in older adults. This cohort was a community dwelling, cognitively intact cohort so results may not pertain to more frail, institutional dwelling older adults.
Conclusions
We have shown that the prevalence of all falls and NAF is 19.2% and 5.1% respectively in the community-dwelling middle-aged and older population in Ireland. Prevalence of all falls and non-accidental falls in particular are higher in the older age groups. Syncope has yearly occurrence rates of 4.4% and a less consistent age gradient. We have demonstrated that all falls, NAF and syncope have common associations; particularly with increasing cardio-vascular co-morbidity, depressive symptoms and unsteadiness during walking. TILDA represents the largest community-dwelling cohort to present data on all falls, NAF and syncope and allows researchers to focus efforts on untangling the associations between these conditions in order to focus appropriate clinical management strategies and future prevention.
Data Availability
The anonymised TILDA dataset is publicly available to researchers who meet the criteria for access, at no monetary cost, from the Irish Social Science Data Archive (ISSDA) at University College Dublin (http://www.ucd.ie/issda/data/tilda/) and the Interuniversity Consortium for Political and Social Research (ICPSR) at the University of Michigan (http://www.icpsr.umich.edu/icpsrweb/ICPSR/studies/34315). TILDA also considers applications for privileged access to the dataset through an onsite “hot desk” facility based in TILDA (visit www.tilda.ie for further information).
Funding Statement
Funding for TILDA was gratefully received from the Atlantic Philanthropies (www.atlanticphilanthropies.org), the Irish Government, and the Health Research Board (www.hrb.ie). TILDA was funded by the Department of Health and Atlantic Philanthropies, along with support from Irish Life in the form of a charitable gift. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.CDC—Older Adult Falls—Falls Among Older Adults: An Overview—Home and Recreational Safety—Injury Center 2014. http://www.cdc.gov/homeandrecreationalsafety/falls/adultfalls.html.
- 2.Probst MA, Kanzaria HK, Gbedemah M, Richardson LD, Sun BC. National trends in resource utilization associated with ED visits for syncope. Am J Emerg Med. 2015;33(8):998–1001. Epub 2015/05/07. doi: 10.1016/j.ajem.2015.04.030 ; [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.WHO | Falls. WHO. 2014. /entity/mediacentre/factsheets/fs344/en/index.html.
- 4.Rubenstein LZ. Falls in older people: epidemiology, risk factors and strategies for prevention. Age Ageing. 2006;35 Suppl 2:ii37–ii41. doi: 10.1093/ageing/afl084 . [DOI] [PubMed] [Google Scholar]
- 5.Cronin H, Kenny RA. Cardiac causes for falls and their treatment. Clin Geriatr Med. 2010;26(4):539–67. Epub 2010/10/12. doi: 10.1016/j.cger.2010.07.006 . [DOI] [PubMed] [Google Scholar]
- 6.Shaw FE, Kenny RA. The overlap between syncope and falls in the elderly. Postgrad Med J. 1997;73(864):635–9. ; [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Finucane C, O'Connell MD, Donoghue O, Richardson K, Savva GM, Kenny RA. Impaired Orthostatic Blood Pressure Recovery Is Associated with Unexplained and Injurious Falls. J Am Geriatr Soc. 2017;65(3):474–82. Epub 2017/03/16. doi: 10.1111/jgs.14563 . [DOI] [PubMed] [Google Scholar]
- 8.Anpalahan M, Gibson S. The prevalence of Neurally Mediated Syncope in older patients presenting with unexplained falls. Eur J Intern Med. 2012;23(2):e48–52. Epub 2012/01/31. doi: 10.1016/j.ejim.2011.10.010 . [DOI] [PubMed] [Google Scholar]
- 9.Richardson DA, Bexton RS, Shaw FE, Kenny RA. Prevalence of cardioinhibitory carotid sinus hypersensitivity in patients 50 years or over presenting to the accident and emergency department with "unexplained" or "recurrent" falls. Pacing & Clinical Electrophysiology. 1997;20(3 Pt 2):820–3. . [DOI] [PubMed] [Google Scholar]
- 10.Parry SW, Frearson R, Steen N, Newton JL, Tryambake P, Kenny RA. Evidence-based algorithms and the management of falls and syncope presenting to acute medical services. Clin Med. 2008;8(2):157–62. Epub 2008/05/16. . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Jansen S, Frewen J, Finucane C, de Rooij SE, van der Velde N, Kenny RA. AF is associated with self-reported syncope and falls in a general population cohort. Age Ageing. 2015. Epub 2015/02/26. doi: 10.1093/ageing/afv017 . [DOI] [PubMed] [Google Scholar]
- 12.Jansen S, Kenny RA, de Rooij SE, van der Velde N. Self-reported cardiovascular conditions are associated with falls and syncope in community-dwelling older adults. Age Ageing. 2014. Epub 2014/10/22. doi: 10.1093/ageing/afu164 . [DOI] [PubMed] [Google Scholar]
- 13.Menant JC, Wong AK, Trollor JN, Close JC, Lord SR. Depressive Symptoms and Orthostatic Hypotension Are Risk Factors for Unexplained Falls in Community-Living Older People. J Am Geriatr Soc. 2016;64(5):1073–8. Epub 2016/05/27. doi: 10.1111/jgs.14104 . [DOI] [PubMed] [Google Scholar]
- 14.Bhangu JS, King-Kallimanis B, Cunningham C, Kenny RA. The relationship between syncope, depression and anti-depressant use in older adults. Age Ageing. 2014. Epub 2014/02/06. doi: 10.1093/ageing/afu003 . [DOI] [PubMed] [Google Scholar]
- 15.Alboni P, Coppola P, Stucci N, Tsakiridu V. Differential diagnosis between 'unexplained' fall and syncopal fall: a difficult or impossible task. J Cardiovasc Med (Hagerstown). 2015;16(2):82–9. Epub 2014/05/20. doi: 10.2459/jcm.0000000000000076 . [DOI] [PubMed] [Google Scholar]
- 16.Kearney PM, Cronin H, O'Regan C, Kamiya Y, Savva GM, Whelan B, et al. Cohort profile: the Irish Longitudinal Study on Ageing. Int J Epidemiol. 2011;40(4):877–84. Epub 2011/08/04. doi: 10.1093/ije/dyr116 . [DOI] [PubMed] [Google Scholar]
- 17.Whelan BJ, Savva GM. Design and methodology of the Irish Longitudinal Study on Ageing. J Am Geriatr Soc. 2013;61 Suppl 2:S265–8. Epub 2013/05/17. doi: 10.1111/jgs.12199 . [DOI] [PubMed] [Google Scholar]
- 18.Health NIoP. ATC/DDD Index 2016. In: Methodology WCCfDS, editor. Oslo2016.
- 19.Weissman MM, Sholomskas D, Pottenger M, Prusoff BA, Locke BZ. Assessing depressive symptoms in five psychiatric populations: a validation study. Am J Epidemiol. 1977;106(3):203–14. Epub 1977/09/01. . [DOI] [PubMed] [Google Scholar]
- 20.Clark DO, Callahan CM, Counsell SR. Reliability and validity of a steadiness score. J Am Geriatr Soc. 2005;53(9):1582–6. Epub 2005/09/03. doi: 10.1111/j.1532-5415.2005.53485.x . [DOI] [PubMed] [Google Scholar]
- 21.Prudham D, Evans JG. Factors associated with falls in the elderly: a community study. Age & Ageing. 1981;10(3):141–6. . [DOI] [PubMed] [Google Scholar]
- 22.Campbell AJ, Reinken J, Allan BC, Martinez GS. Falls in old age: a study of frequency and related clinical factors. Age & Ageing. 1981;10(4):264–70. . [DOI] [PubMed] [Google Scholar]
- 23.Downton JH, Andrews K. Prevalence, characteristics and factors associated with falls among the elderly living at home. Aging-Clinical & Experimental Research. 1991;3(3):219–28. . [DOI] [PubMed] [Google Scholar]
- 24.Rapp K, Freiberger E, Todd C, Klenk J, Becker C, Denkinger M, et al. Fall incidence in Germany: results of two population-based studies, and comparison of retrospective and prospective falls data collection methods. BMC Geriatr. 2014;14:105 doi: 10.1186/1471-2318-14-105 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Tinetti ME, Speechley M, Ginter SF. Risk factors for falls among elderly persons living in the community. N Engl J Med. 1988;319(26):1701–7. Epub 1988/12/29. doi: 10.1056/NEJM198812293192604 . [DOI] [PubMed] [Google Scholar]
- 26.Campbell AJ, Borrie MJ, Spears GF, Jackson SL, Brown JS, Fitzgerald JL. Circumstances and consequences of falls experienced by a community population 70 years and over during a prospective study. Age Ageing. 1990;19(2):136–41. Epub 1990/03/01. . [DOI] [PubMed] [Google Scholar]
- 27.Davies AJ, Kenny RA. Falls presenting to the accident and emergency department: types of presentation and risk factor profile. Age Ageing. 1996;25(5):362–6. Epub 1996/09/01. . [DOI] [PubMed] [Google Scholar]
- 28.Rafanelli M, Ruffolo E, Chisciotti VM, Brunetti MA, Ceccofiglio A, Tesi F, et al. Clinical aspects and diagnostic relevance of neuroautonomic evaluation in patients with unexplained falls. Aging-Clinical & Experimental Research. 2014;26(1):33–7. http://dx.doi.org/10.1007/s40520-013-0124-8. . [DOI] [PubMed] [Google Scholar]
- 29.Chen LY, Shen WK, Mahoney DW, Jacobsen SJ, Rodeheffer RJ. Prevalence of syncope in a population aged more than 45 years. Am J Med. 2006;119(12):1088 e1–7. doi: 10.1016/j.amjmed.2006.01.029 . [DOI] [PubMed] [Google Scholar]
- 30.Soteriades ES, Evans JC, Larson MG, Chen MH, Chen L, Benjamin EJ, et al. Incidence and prognosis of syncope. N Engl J Med. 2002;347(12):878–85. Epub 2002/09/20. doi: 10.1056/NEJMoa012407 . [DOI] [PubMed] [Google Scholar]
- 31.Jansen S, Bhangu J, de Rooij S, Daams J, Kenny RA, van der Velde N. The Association of Cardiovascular Disorders and Falls: A Systematic Review. J Am Med Dir Assoc. 2015. Epub 2015/10/13. doi: 10.1016/j.jamda.2015.08.022 . [DOI] [PubMed] [Google Scholar]
- 32.Bhangu J, McMahon CG, Hall P, Bennett K, Rice C, Crean P, et al. Long-term cardiac monitoring in older adults with unexplained falls and syncope. Heart. 2016. Epub 2016/01/30. doi: 10.1136/heartjnl-2015-308706 . [DOI] [PubMed] [Google Scholar]
- 33.Kenny RA, Richardson DA, Steen N, Bexton RS, Shaw FE, Bond J. Carotid sinus syndrome: a modifiable risk factor for nonaccidental falls in older adults (SAFE PACE). J Am Coll Cardiol. 2001;38(5):1491–6. Epub 2001/11/03. . [DOI] [PubMed] [Google Scholar]
- 34.Summary of the Updated American Geriatrics Society/British Geriatrics Society clinical practice guideline for prevention of falls in older persons. J Am Geriatr Soc. 2011;59(1):148–57. Epub 2011/01/14. doi: 10.1111/j.1532-5415.2010.03234.x . [DOI] [PubMed] [Google Scholar]
- 35.Moya A, Sutton R, Ammirati F, Blanc JJ, Brignole M, Dahm JB, et al. Guidelines for the diagnosis and management of syncope (version 2009). Eur Heart J. 2009;30(21):2631–71. Epub 2009/08/29. doi: 10.1093/eurheartj/ehp298 ; [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kenny RA, Brignole M, Dan GA, Deharo JC, van Dijk JG, Doherty C, et al. Syncope Unit: rationale and requirement—the European Heart Rhythm Association position statement endorsed by the Heart Rhythm Society. Europace. 2015;17(9):1325–40. Epub 2015/06/26. doi: 10.1093/europace/euv115 . [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The anonymised TILDA dataset is publicly available to researchers who meet the criteria for access, at no monetary cost, from the Irish Social Science Data Archive (ISSDA) at University College Dublin (http://www.ucd.ie/issda/data/tilda/) and the Interuniversity Consortium for Political and Social Research (ICPSR) at the University of Michigan (http://www.icpsr.umich.edu/icpsrweb/ICPSR/studies/34315). TILDA also considers applications for privileged access to the dataset through an onsite “hot desk” facility based in TILDA (visit www.tilda.ie for further information).