Abstract
This study tested the hypothesis that glucagon-like peptide 1 (GLP-1) therapies improve cardiac contractile function at rest and in response to adrenergic stimulation in obese swine after myocardial infarction. Obese Ossabaw swine were subjected to gradually developing regional coronary occlusion using an ameroid occluder placed around the left anterior descending coronary artery. Animals received subcutaneous injections of saline or liraglutide (0.005–0.015 mg/kg/day) for 30 days after ameroid placement. Cardiac performance was assessed at rest and in response to sympathomimetic challenge (dobutamine 0.3–10 μg/kg/min) using a left ventricular pressure/volume catheter. Liraglutide increased diastolic relaxation (dP/dt; Tau 1/2; Tau 1/e) during dobutamine stimulation (P < 0.01) despite having no influence on the magnitude of myocardial infarction. The slope of the end-systolic pressure volume relationship (i.e., contractility) increased with dobutamine after liraglutide (P < 0.001) but not saline administration (P = 0.63). Liraglutide enhanced the slope of the relationship between cardiac power and pressure volume area (i.e., cardiac efficiency) with dobutamine (P = 0.017). Hearts from animals treated with liraglutide demonstrated decreased β1-adrenoreceptor expression. These data support that GLP-1 agonism augments cardiac efficiency via attenuation of maladaptive sympathetic signaling in the setting of obesity and myocardial infarction.
Introduction
Use of glucagon like peptide 1 (GLP-1)–based therapies for the treatment of type 2 diabetes (T2DM) has increased significantly since their discovery in the 1980s (1). Although these agents demonstrate unequivocal efficacy in the control of blood glucose concentration, an emerging body of evidence indicates direct cardiovascular benefit, including improvements in cardiac contractile function (2), reductions in myocardial infarct size (3) in animal studies, and improved cardiovascular event rates in some but not all clinical trials (4–6). Thus, there is strong interest in these apparent cardioprotective effects of GLP-1–based therapies in clinical applications of obesity and T2DM (7,8).
Prior studies of the cardiovascular effects of GLP-1 have largely been performed in animal models lacking obesity/metabolic disease phenotypes, in contrast to the fact that most patient populations treated with agents from this therapeutic class are overweight or obese (9). Studies from our laboratory and others have demonstrated obesity-related impairment in cardiovascular effects of GLP-1 agonists, including attenuation of GLP-1–mediated increases in myocardial glucose uptake in obese swine (10) and humans with T2DM (10,11). Further evidence of different responses in obesity comes from our recent report that the GLP-1R agonist exendin-4 augmented end-diastolic volume (EDV) and systolic pressure generation during coronary reperfusion in lean swine while maintaining systolic pressure despite marked reduction in diastolic filling in obese swine (12).
The mechanisms responsible for these obesity-related differences are unknown. However, the capacity for GLP-1 to induce changes in cardiac inotropy (13) and lusitropy (12) implicate underlying differences in adrenergic responsiveness that are known to exist in obesity (14). Such metabolic state–dependent effects of GLP-1 combined with the inconsistent cardiovascular benefits of GLP-1–based therapeutics in clinical trials of patients with diabetes (4,5) support the need for a better understanding of the cardiac effects of GLP-1 in the setting of obesity and metabolic dysregulation, especially in the setting of complex ischemic heart disease.
This study investigated the potential for liraglutide to influence cardiac function at rest and in response to β-adrenergic receptor (βADR) stimulation in an obese swine model of subacute, progressive coronary artery occlusion. We hypothesized that chronic (∼3–4 weeks) liraglutide administration (a GLP-1 analog) would demonstrate cardioprotective capacity in ischemic hearts of obese animals through infarct mitigation and/or alterations in cardiac contractile function.
Research Design and Methods
Surgical Preparation and Experimental Protocol
All experiments involving animals were approved by an Institutional Animal Care and Use Committee and performed in accordance with the Guide for the Care and Use of Laboratory Animals (National Institutes of Health Publication. No. 85-23, Revised 2011). Ossabaw swine were fed an obesogenic diet (10,15) for 6 months, after which an ameroid constrictor (Research Instruments Southwest) was placed around the left anterior descending coronary artery (LAD). Next, animals were randomly assigned to saline or liraglutide treatment groups. During the subsequent 4 weeks, liraglutide-treated animals received a step-up protocol of liraglutide (week 1: 0.005, week 2: 0.010, weeks 3 and 4: 0.015 mg/kg/day, delivered subcutaneously once daily), and saline-treated animals received volume-matched saline injections.
After this 4-week treatment period, during which time the ameroid constrictor induced a subacute, unrelieved LAD occlusion, a terminal in vivo study was performed to measure systemic hemodynamic parameters, blood gasses, and cardiac function. Measurements were obtained at rest and during a progressive sympathomimetic challenge (dobutamine 0.3–10 μg/kg/min).
Infarct Quantification
Immediately subsequent to the physiologic measurements, hearts were fibrillated, excised, and flushed with 4°C, Ca2+-free Krebs buffer via aortic cannulation. Hearts were frozen at −20°C, sliced into 1-cm-thick sections, stained with 1% weight/volume tetrazolium solution, and transferred to a 10% buffered formalin solution for at least 24 h. Formalin-fixed tissues were imaged, and the infarct area (unstained) versus viable tissue (stained) was quantified on each heart slice from each animal by two separate investigators blinded to condition using ImageJ software (National Institutes of Health).
Immunohistochemistry
Endocardial biopsy specimens from the 1-cm-thick heart slices were taken from both the ischemic and normally perfused regions of left ventricular myocardium for histologic analysis. Tissues were processed into 4- to 5-μm-thick slices stained for βADR (PA5-28808; Thermo Fisher, Rockford, IL) and imaged on the Aperio Scan Scope CS whole-slide digital imaging system (Aperio Technologies, Vista, CA) at original magnification ×20. Positive staining was quantified using a positive pixel algorithm (Aperio Technologies), image quantitation software approved by the U.S. Food and Drug Administration for providing molecular imaging analyses in support of new drug applications.
Statistical Analyses
Data are presented as mean ± SEM and were analyzed using SigmaPlot 12 software (Systat Software Inc., San Jose, CA) and SPSS 21 software (IBM). Comparisons were considered statistically significant when P < 0.05. Treatment groups and ischemic/nonischemic zone results were compared using unpaired t tests or linear mixed modeling evaluating the dobutamine dose response as a repeated measure, as appropriate. For significant ANOVAs, Student-Newman-Keuls post hoc testing was performed to identify pairwise differences between groups. Multiple linear regression and ANCOVA were used to compare the slopes and intercepts of the relationships between cardiac output (CO) versus EDV and cardiac power versus pressure volume (PV) area (PVA).
Results
Phenotypic Characteristics of Obese Swine
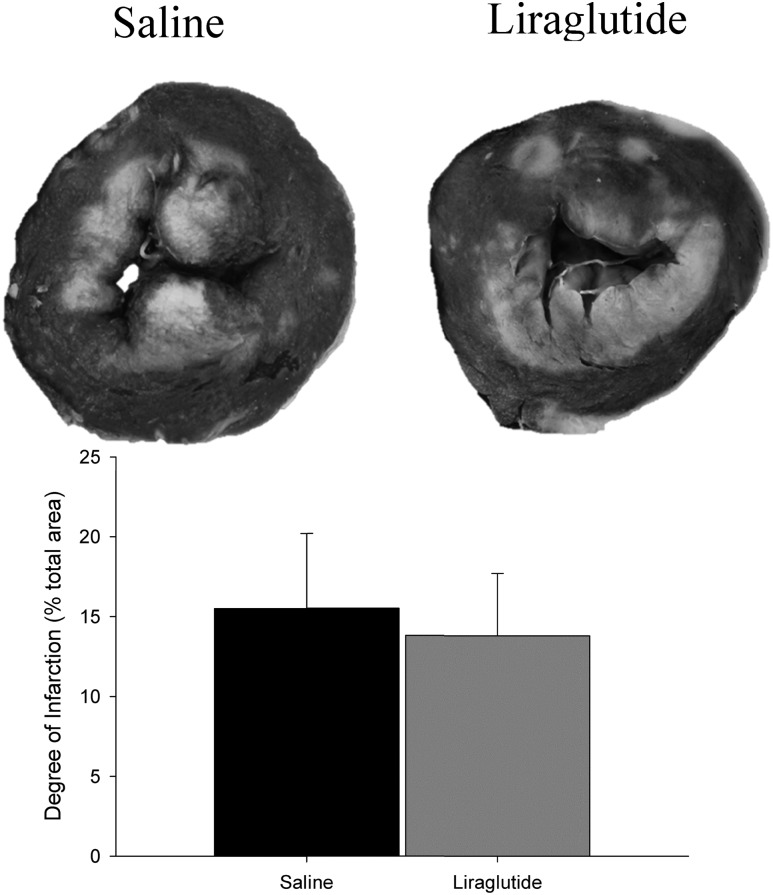
Body weight on the day of ameroid placement was not different in animals subsequently assigned to receive saline versus liraglutide (P = 0.31) (Table 1). On randomized treatment, the liraglutide-treated animals failed to gain weight, resulting in significantly lower weight at the time of physiologic studies relative to saline controls (P = 0.02) (Table 1). Liraglutide therapy did not significantly alter total cardiac mass (P = 0.85) (Table 1), heart weight-to-body ratio (P = 0.09) (Table 1), or the overall magnitude of infarction (P = 0.81) (Fig. 1). Also, left ventricular free wall thickness, measured 2 cm distal to the ameroid location, was not different between treatment groups (saline, 2.3 ± 0.1 vs. liraglutide, 2.3 ± 0.1 cm; P = 0.97).
Table 1.
Phenotype characteristics of obese swine
| Saline | Liraglutide | P value | |
|---|---|---|---|
| Body mass (kg) | |||
| At ameroid placement | 63 ± 11 | 52 ± 4 | 0.31 |
| At terminal study | 70 ± 6 | 54 ± 3 | 0.02 |
| ΔBody weight (kg) | 9 ± 4 | 1 ± 2 | 0.09 |
| Heart weight (g) | 223.3 ± 17.5 | 218.4 ± 13.9 | 0.85 |
| Heart weight–to–body weight ratio | 3.3 ± 0.04 | 4.1 ± 0.02 | 0.09 |
Values are mean ± SE for saline (n = 5) and liraglutide (n = 7).
Figure 1.
Quantification of myocardial infarction. Images (top) present representative transmural sections of a left ventricle. Unstained (white) tissue within the myocardium indicates infarcted tissue. Infarct was quantified (bottom) as the percentage of total left ventricular area of all slices. Liraglutide did not reduce infarct size (saline: 15.5 ± 1.9% of myocardium infarcted [n = 4] vs. liraglutide: 13.9 ± 5.4% [n = 6]; P = 0.81).
Effects of Liraglutide on Baseline Hemodynamic and Cardiac Parameters
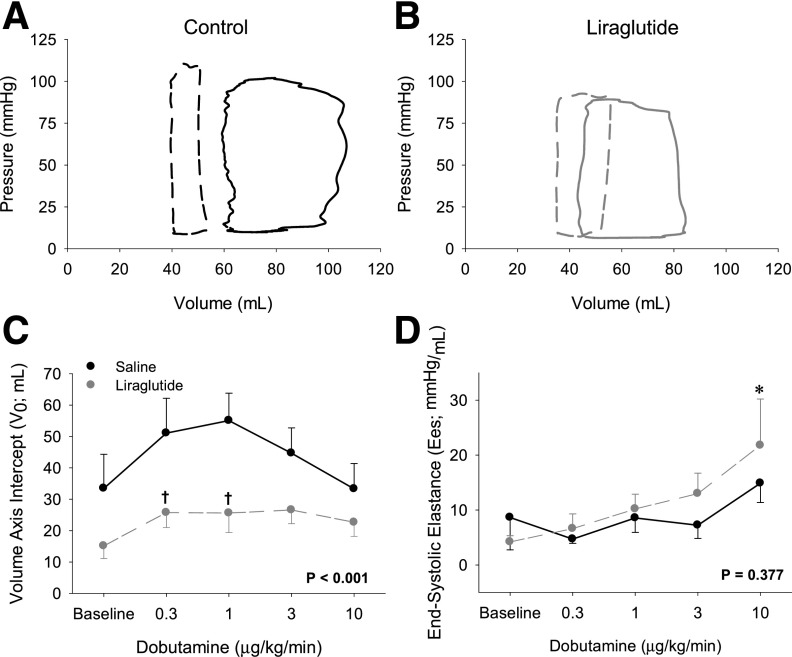
All physiologic data were obtained during an anesthetized procedure at the end of the treatment protocol (Table 2) for cross-sectional comparisons of saline versus liraglutide treatment in the setting of subacute unrelieved infarction. Mean arterial pressure was similar under resting conditions (P = 0.87), but heart rate was ∼40% higher in liraglutide- versus saline-treated animals (Table 2). Heart rate changes (described below) occurred independent of changes to peripheral vascular resistance, which is calculated as mean arterial pressure/CO (saline, 0.03 ± 0.004 vs. liraglutide, 0.03 ± 0.005 mmHg/mL; P = 0.82). Key indices of cardiac function, including ejection fraction, Tau 1/2, end-diastolic PV relationship (Table 2), end-systolic elastance (Ees) (Fig. 2D), and CO (Fig. 3B) were unaffected by liraglutide administration under resting conditions.
Table 2.
Effects of liraglutide therapies on hemodynamic and cardiac parameters
| Liraglutide | Dobutamine | Lir*Dob | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Dobutamine (μg/kg/min) |
effect | effect | interaction | ||||||
| Baseline | 0.3 | 1 | 3 | 10 | P value | P value | P value | ||
| Systolic pressure (mmHg) | Saline | 93 ± 7 | 96 ± 9 | 99 ± 8 | 104 ± 9 | 107 ± 8 | 0.244 | 0.524 | 0.951 |
| Liraglutide | 94 ± 3 | 93 ± 2 | 94 ± 1 | 97 ± 3 | 99 ± 6 | ||||
| Diastolic pressure (mmHg) | Saline | 64 ± 5 | 65 ± 6 | 67 ± 7 | 67 ± 5 | 68 ± 6 | 0.392 | 0.995 | 0.960 |
| Liraglutide | 65 ± 3 | 64 ± 3 | 64 ± 3 | 64 ± 3 | 62 ± 4 | ||||
| Mean pressure (mmHg) | Saline | 77 ± 6 | 77 ± 7 | 80 ± 7 | 81 ± 6 | 82 ± 7 | 0.509 | 0.932 | 0.974 |
| Liraglutide | 78 ± 3 | 77 ± 2 | 78 ± 2 | 79 ± 3 | 77 ± 4 | ||||
| Heart rate (bpm) | Saline | 77 ± 13 | 80 ± 14 | 89 ± 17 | 113 ± 18 | 145 ± 17* | 0.001 | 0.001 | 0.956 |
| Liraglutide | 107 ± 9 | 120 ± 12 | 125 ± 13 | 146 ± 14 | 162 ± 14* | ||||
| Ejection fraction (%) | Saline | 48 ± 9 | 39 ± 10 | 38 ± 9 | 36 ± 8 | 28 ± 6 | 0.965 | 0.384 | 0.772 |
| Liraglutide | 40 ± 5 | 38 ± 6 | 39 ± 4 | 37 ± 4 | 36 ± 4 | ||||
| Contraction time (ms) | Saline | 53 ± 2 | 57 ± 4 | 49 ± 5 | 43 ± 4 | 43 ± 4 | 0.573 | 0.001 | 0.424 |
| Liraglutide | 63 ± 7 | 60 ± 7 | 53 ± 7 | 43 ± 3* | 36 ± 2* | ||||
| Relaxation time (ms) | Saline | 142 ± 16 | 104 ± 18* | 131 ± 14 | 113 ± 13 | 96 ± 9* | 0.027 | <0.001 | 0.412 |
| Liraglutide | 120 ± 5 | 117 ± 4 | 110 ± 4 | 95 ± 4 | 82 ± 5* | ||||
| dPmax (mmHg/s) | Saline | 1,204 ± 157 | 1,230 ± 170 | 1,548 ± 250 | 2,350 ± 403* | 3,071 ± 574* | 0.618 | <0.001 | 0.798 |
| Liraglutide | 1,536 ± 108 | 1,460 ± 101 | 1,584 ± 140 | 2,249 ± 208 | 3,010 ± 392* | ||||
| dPmin (mmHg/s) | Saline | −858 ± 66 | −832 ± 138 | −955 ± 193 | −1,126 ± 235 | −1,379 ± 178 | 0.001 | 0.014 | 0.988 |
| Liraglutide | −1,159 ± 108 | −1,182 ± 102 | −1,281 ± 131 | −1,541 ± 121* | −1,839 ± 229* | ||||
| Tau ½ (ms) | Saline | 32 ± 2 | 29 ± 3 | 33 ± 4 | 30 ± 4 | 23 ± 2 | 0.006 | 0.002 | 0.479 |
| Liraglutide | 29 ± 2 | 28 ± 1 | 17 ± 1 | 22 ± 1† | 17 ± 2* | ||||
| Tau 1/e (ms) | Saline | 22 ± 2 | 20 ± 2 | 23 ± 3 | 22 ± 3 | 16 ± 2 | 0.005 | 0.004 | 0.428 |
| Liraglutide | 21 ± 2 | 20 ± 1 | 19 ± 1 | 15 ± 1† | 11 ± 2 | ||||
| End-diastolic PV relationship | Saline | 0.24 ± 0.10 | 0.22 ± 0.12 | 0.28 ± 0.21 | 0.22 ± 0.08 | 0.28 ± 0.09 | 0.164 | 0.283 | 0.726 |
| Liraglutide | 0.17 ± 0.05 | 0.21 ± 0.10 | 0.25 ± 0.12 | 0.36 ± 0.10 | 0.36 ± 0.12 | ||||
Values are mean ± SE for saline (n = 5) and liraglutide (n = 7). Treatment column reports P values for differences in mean response across dobutamine administration.
*P < 0.05 vs. baseline value (same treatment).
†P < 0.05 vs. dobutamine infusion rate-matched, saline controls.
Figure 2.
Cardiac effects of liraglutide. Representative PV relationships of saline-treated (A) and liraglutide-treated (B) animals before dobutamine administration (solid lines) and at 10 μg/kg/min after dobutamine (dashed lines). Dobutamine administration resulted in a profound leftward shift in saline-treated animals that was attenuated in liraglutide-treated animals. C: The volume axis intercept (V0) was significantly lower across the range of dobutamine infusions. D: Ees did not increase across a range of dobutamine administration in saline-treated animals but was significantly increased at the highest dobutamine dose in liraglutide-treated animals relative to saline-treated animals. Values for panels C and D are mean ± SE for saline (n = 5) and liraglutide (n = 7). *P < 0.05 vs. baseline value (same treatment). †P < 0.05 vs. dobutamine infusion rate-matched, saline controls.
Figure 3.
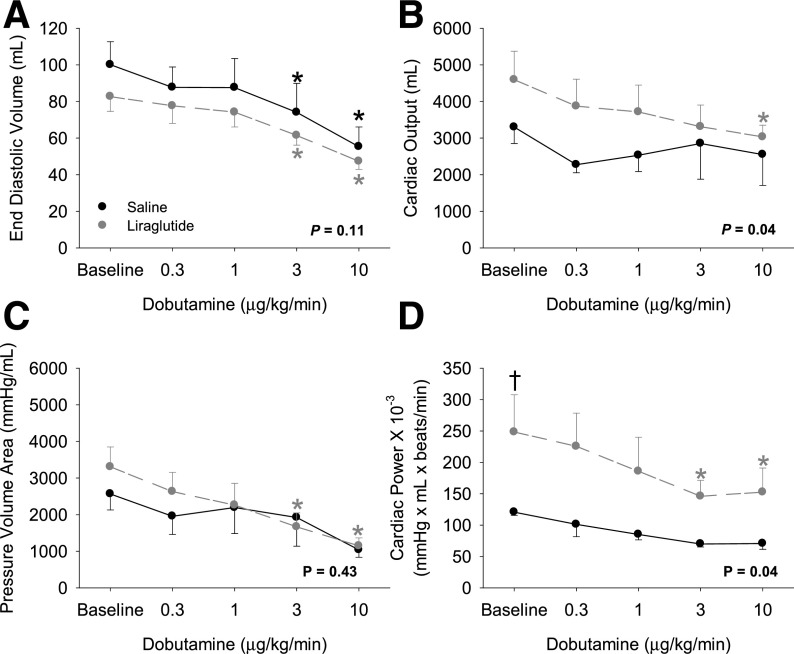
Effects of liraglutide treatment on cardiac volumes, oxygen consumption, and power. A: Dobutamine administration resulted in similar and significant decreases in EDV in both saline- and liraglutide-treated animals. B: CO exhibited a similar decrease with dobutamine administration in liraglutide- but not saline-treated animals. C: PVA similarly decreased in liraglutide-treated animals only. D: Cardiac power, however, was significantly greater on average in liraglutide-treated animals relative to saline controls. Values are mean ± SE for saline (n = 5) and liraglutide (n = 7). Displayed P values denote the overall treatment group comparison for differences in response to dobutamine. *P < 0.05 comparing individual doses against baseline within the treatment group (significant in panel C only for the liraglutide-treated animals). †P < 0.05 comparing the treatment groups under resting conditions.
Effects of Liraglutide Treatment on Responses to Adrenergic Stimulation
Systemic arterial pressures were not significantly increased by dobutamine (0.3–10 μg/kg/min) and were unaffected by liraglutide treatment (Table 2). Dobutamine increased heart rate in both groups, with an enhanced effect in liraglutide-treated animals (P = 0.001) (Table 2) and reduced CO (∼35%; P = 0.02) in liraglutide-treated animals at the highest levels of dobutamine (Fig. 3B). Liraglutide treatment was also associated with enhanced diastolic function, as indicated by increases in –dP/dtmin and Tau (Table 2), consistent with the enhanced CO of liraglutide-treated animals (P = 0.04) (Fig. 3B). End-diastolic PV relationships were unaffected by liraglutide treatment (Table 2).
Representative PV loops shown in Fig. 2A and B illustrate dobutamine-mediated reductions in EDV (right side of the PV loop), and end-systolic volume (ESV; left side of the PV loop), which decreased to a similar magnitude in both groups (EDV, P = 0.19; ESV, P = 0.47). Stroke volume decreased similarly in both groups (P = 0.48), reaching significance at the 10 µg/kg/min dose (saline, P = 0.005; liraglutide, P = 0.02). Overall, the volume axis intercept (V0; greatest left ventricular volume at which pressure is zero) was lower in liraglutide-treated swine (P < 0.001) (Fig. 2C). Load-dependent measures of cardiac contraction were enhanced by dobutamine in both groups, with dose-dependent increases in dP/dtmax (P = 0.001) as well as significant reductions of contraction time in the liraglutide groups (Table 2). Accordingly, the mean relaxation was different between groups across the range of the dobutamine challenge (dP/dtmin, P < 0.001; Tau 1/2, P = 0.06; Tau 1/e, P = 0.005). The slope of end-systolic PV relationship, a load-independent measure of cardiac contractility (Ees), was not different on average between groups (P = 0.38) (Fig. 2D); however, dobutamine infusion significantly increased contractility at the 10 μg/kg/min dose in liraglutide- but not saline-treated animals (P < 0.001) (Fig. 2D).
Effect of Liraglutide and Adrenergic Stimulation on Cardiac Function and Efficiency
EDV was significantly decreased relative to baseline in both saline- and liraglutide-treated animals at the highest concentrations of dobutamine (P < 0.001 for each group) (Fig. 3A). Dobutamine-dependent reductions in EDV were also similar between treatment groups (P = 0.11) (Fig. 3A). Dobutamine-driven changes in CO were dose-dependently decreased in liraglutide-treated animals, achieving significance at the highest dose (P = 0.02) (Fig. 3B). In saline-treated animals, which demonstrated modestly lower baseline CO values, CO was not significantly changed by dobutamine administration (Fig. 3B) despite significant increases in heart rate (Table 2).
PVA is linearly related to left ventricular myocardial oxygen consumption (MvO2) (16) and was not different between treatment groups under resting conditions (P = 0.29) or across the range of dobutamine exposures (P = 0.43) (Fig. 3C). However, PVA was decreased compared with resting baseline in liraglutide-treated animals at 3.0 (P = 0.005) and 10 μg/kg/min (P < 0.001) dobutamine doses; there were no significant changes in PVA from baseline within the saline-treated animals (Fig. 3C).
Cardiac power (product of stroke volume, mean aortic pressure, and heart rate) was significantly increased under resting conditions by liraglutide treatment (P = 0.03) and was greater in those animals across the range of dobutamine administration (P = 0.04) (Fig. 3D). Dobutamine administration resulted in significant reductions in cardiac power at the 3 μg/kg/min (P = 0.03) and 10 μg/kg/min (P = 0.01) doses in liraglutide-treated animals (Fig. 3D). Saline-treated animals, which showed lower cardiac power overall, demonstrated no change in cardiac power in response to dobutamine administration at any dose.
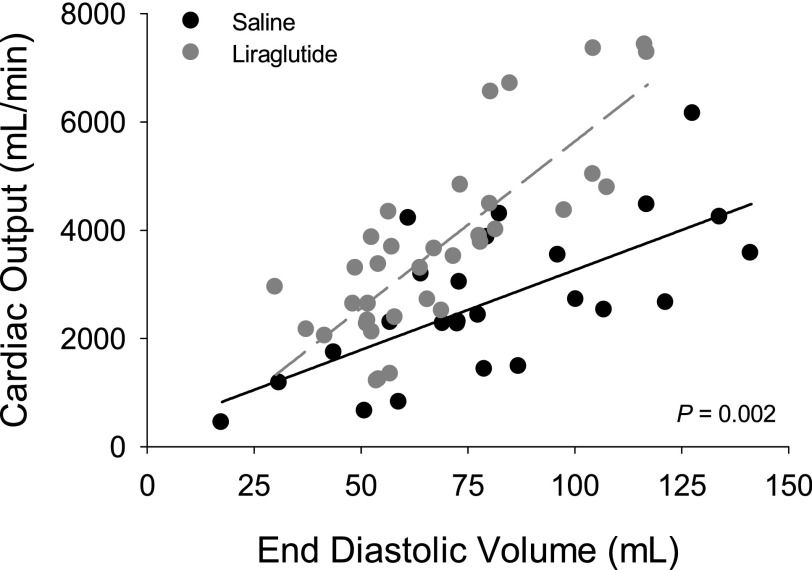
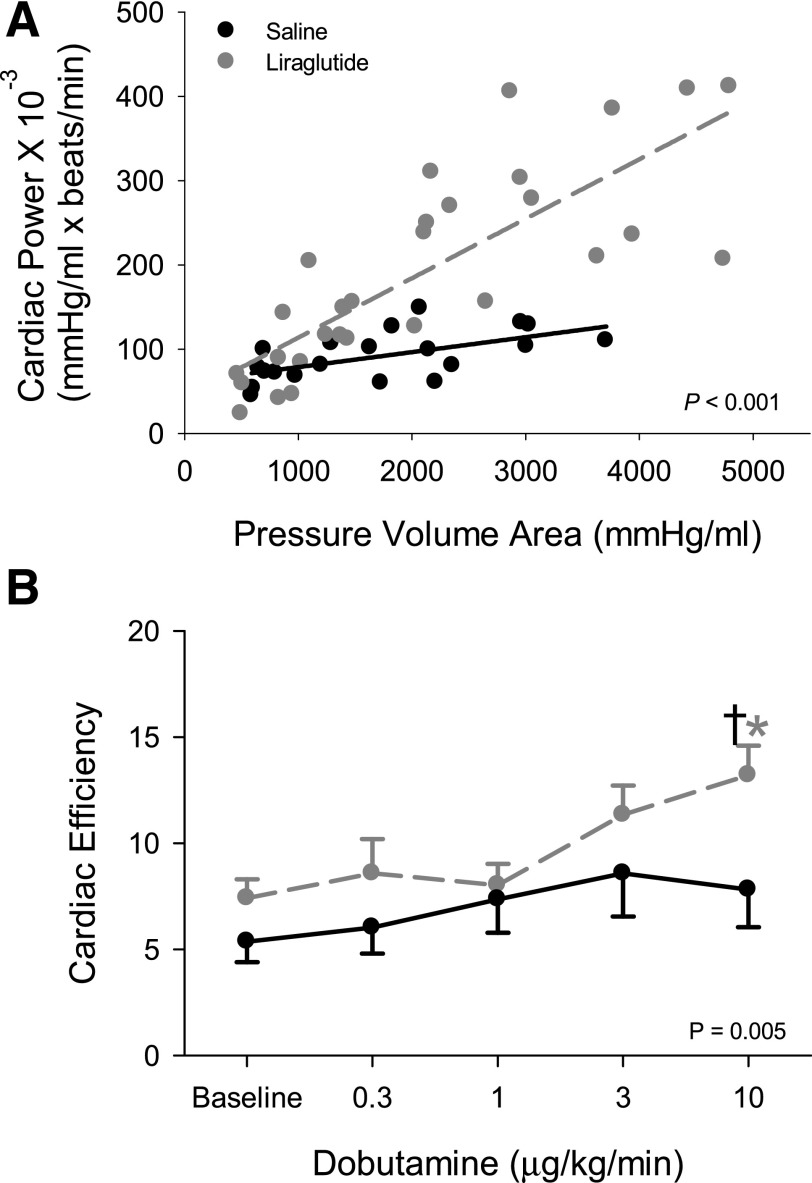
Figure 4 presents the relationship between CO and EDV for the saline- and liraglutide-treated animals before and during dobutamine administration. Liraglutide increased the slope of the relationship between CO and EDV with dobutamine challenge (P = 0.002), resulting in greater CO at higher values of EDV. When cardiac power is expressed relative to PVA, it produces an index of cardiac work efficiency – power per unit of oxygen consumed (16,17). Therefore, to assess whether liraglutide altered cardiac work efficiency, we plotted cardiac power relative to PVA (Fig. 5A). This relationship demonstrates that liraglutide treatment increased power generation at higher MvO2 (P = 0.001 for slope of relationship saline vs. liraglutide by multiple linear regression); that is, cardiac efficiency was greater in liraglutide-treated animals. Figure 5B demonstrates that cardiac efficiency (ratio of cardiac power to PVA) was enhanced by liraglutide and that dobutamine challenge resulted in significant enhancement of efficiency in liraglutide- but not in saline-treated animals.
Figure 4.
Liraglutide increases CO via a load-independent mechanism. Liraglutide treatment resulted in an increase in the slope of the relationship between CO and EDV (P = 0.002 by ANCOVA). As defined by the Frank-Starling law of the heart, a load-dependent increase in CO would result in a shift of values that would still fit the control line. A change in slope is indicative of a load-independent increase in CO. This analysis includes data points from all animals at all measurement points. Saline (n = 5) and liraglutide (n = 7).
Figure 5.
Liraglutide increases cardiac efficiency. A: The slope of the relationship between cardiac power and PVA was greater in liraglutide-treated swine hearts. The increased ratio of PVA (an index of cardiac oxygen consumption) to cardiac power evident in liraglutide-treated animals establishes that liraglutide increased the ratio of cardiac work to cardiac energetics. P value is by ANCOVA; P = 0.02 for homogeneity of regressions. B: To better establish efficiency at each dose of dobutamine, the ratio of cardiac power to the PVA was calculated for each animal at each dose. Liraglutide therapy increased the efficiency of this relationship overall (P = 0.005) and at the highest dose of dobutamine relative to both baseline and the dobutamine dose-matched saline control. *P < 0.05 comparing individual doses against baseline within the treatment group. †P < 0.05 comparing the treatment groups under resting conditions. Saline (n = 5) and liraglutide (n = 7).
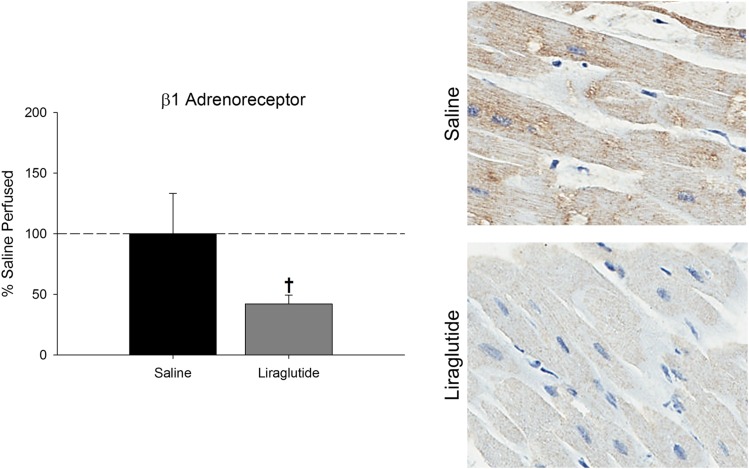
Immunohistochemistry of Formalin-Fixed Tissues
Immunohistochemistry was performed on formalin-fixed endocardial samples from the normally perfused myocardium. Abundance of β1ADR protein was decreased ∼52% (P = 0.045) in liraglutide-treated animals relative to their saline counterparts (Fig. 6).
Figure 6.
Liraglutide decreases expression of βADR. Liraglutide-treated animals exhibited significantly decreased left ventricular βADR abundance relative to saline-treated animals. Images show representative left ventricular myocardial staining for βADR in saline-treated (top) and liraglutide-treated (bottom) animals. Values are mean ± SE for saline (n = 4) and liraglutide (n = 4). †P < 0.05 vs. treatment same condition.
Discussion
GLP-1 receptor activation produces potentially cardioprotective phenomena in healthy animal models receiving recombinant GLP-1–based therapies (1–3,10,13,18). Inconsistent data exist regarding the cardioprotective potential of these therapies in the setting of ischemic heart disease with underlying obesity and metabolism dysfunction (4–6). Because GLP-1–based therapies are classically used for the purpose of glucose regulation in T2DM, a population with significant lifetime cardiovascular risk, understanding the cardiovascular effects of GLP-1–based treatments in the setting of obesity is crucial.
Here we examined the effects of GLP-1 receptor activation via liraglutide on cardiac function at rest and in response to sympathetic stimulation in an obese swine model of slowly developing myocardial ischemia. We hypothesized that chronic (∼3–4 weeks) administration of the GLP-1 analog liraglutide would demonstrate cardioprotective capacity in ischemic hearts of obese animals through infarct mitigation and/or alterations in cardiac contractile function. This study identifies the capacity of liraglutide to improve cardiac performance of significantly infarcted hearts in an energetically favorable fashion and is the first to identify a relationship between myocardial β1ADR abundance and GLP-1–based therapies.
Infarct Size
This study examined GLP-1–based cardioprotection in the context of a slowly developing, unrelieved, regional myocardial infarction using an ameroid constrictor around the LAD. Ameroid constrictors are a well-established tool in the study of coronary artery disease in swine models (19,20). Postmortem analyses verified a 100% closure rate of the ameroid constrictors in all study animals; that is, each animal experienced total loss of flow to the LAD perfusion territory distal to the ameroid constrictor. The consistency of closure between animals and treatment groups is evident in the tetrazolium staining, which demonstrated a consistent ∼15% infarction of the left ventricle (Fig. 1). This point is critical because these data demonstrate that differences in cardiac function with liraglutide administration are not related to underlying differences in the magnitude of infarction.
Data regarding the capacity of GLP-1 therapeutics to mitigate myocardial infarction remain equivocal because similar studies in swine from Kristensen et al. (21) and Ekström et al. (22) failed to show infarct mitigation, whereas Timmers et al. (3) and others have demonstrated infarct reductions with GLP-1–based therapies. Similarly equivocal findings exist in rodent models as well, which show varied capacity for infarct mitigation (23,24). Some discrepancy in the findings of the animal studies from different laboratories could arise as a result of differences in the duration of ischemic insult and the presence or absence of a reperfusion window. We posit that liraglutide failed to mitigate infarct size in the current study because of the absence of reperfusion (i.e., chronic total coronary artery occlusion) and because of the limited endogenous collateral network in swine (25). These factors would limit or prevent exposure of ischemic tissues to receive the therapeutic agent and have important implications for the cardioprotective efficacy in the clinical circumstance of chronically developing coronary occlusion because clinical studies also report varied efficacy of GLP-1 therapies to mitigate infarct (26–29).
Hemodynamics
Pressor effects of GLP-1 are particularly pronounced in rodent models, which routinely show significant increases in mean pressure as high as 20 mmHg (13), inconsistent with human studies that report elevations of 2–3 mmHg or reductions of <3 mmHg in response to GLP-1 receptor agonism (8,13,14). The hemodynamic profile of liraglutide-treated animals in this study is consistent with work by Lovshin et al. (30), who found that 3 weeks of liraglutide treatment failed to modulate blood pressure in patients with T2DM. The absence of a significant pressor response in this study (Table 2) is therefore consistent with the body of literature in human subjects that demonstrates variable or modest effects of GLP-1 drugs on blood pressure (13).
Central effects of GLP-1 therapies to modulate hemodynamics are well established in rodents but remain equivocal in large-animal models and humans (13). Previous work by our group identified no effect of hexamethonium treatment on changes to cardiac performance resulting from acute administration of GLP-1 (7-36) in the setting of myocardial ischemia (2). These data further support an absence of sympathomimetic modulation by GLP-1–based therapies with regard to pressor responses because systolic, diastolic, and mean pressures are all consistent between treatment groups across the range of dobutamine concentrations. Similarly, GLP-1– mediated chronotropy (positive or negative) is highly variable and differs by species (13). Tachycardia appears to be most pronounced in species that demonstrate the greatest pressor responses to GLP-1 therapies (13), whereas meta-analyses of human studies report only modest GLP-1–related tachycardia (1).
In response to the sympathomimetic challenge, GLP-1 therapy resulted in a significantly higher heart rate across the dose response range (P = 0.001) (Table 1), although the magnitude of change relative to baseline was consistent between groups (P = 0.44). These data support a potential to modulate heart rate, but whether this is the result of nodal activity remains to be determined. To assess the potential of liraglutide to produce peripheral dilation, peripheral vascular resistance was calculated and not different between groups (P = 0.82), removing the potential of peripheral dilation to bias the result.
Cardiac Function
Liraglutide significantly lowered V0, an index of end-diastolic relaxation, both at baseline and at lower dobutamine concentrations. This decrease runs counter to previously documented effects of GLP-1 (7-36) administration in the setting of acute myocardial ischemia (2), where preload-dependent increases in CO were accomplished in a GLP-1–dependent fashion, reflected by a constant Ees and increased V0. However, prior observations were made in lean swine, whereas the current observations included only obese swine. The current findings are consistent with recent observations that demonstrated GLP-1 analog–dependent increases in inotropy of obese hearts in the setting of ischemia-reperfusion (12). These changes in V0 could reflect low levels of positive inotropy before overt increases in Ees or could be the result of significant and differential cardiac remodeling between the two treatment groups (31). Regardless, the contrast of the current data against those obtained in lean animals support the paradigm that metabolic status significantly affects the cardiac effects of GLP-1 therapies.
Contractility, as determined by Ees, was not enhanced with dobutamine challenge in saline-treated animals when examined as an absolute change or as a change relative to baseline. By contrast, liraglutide therapies preserved the ability of infarcted hearts to respond to adrenoreceptor activation in that there was a continuous increase in Ees across the range of dobutamine concentrations both absolute and relative to baseline. Examination of the relationship between EDV and CO (Frank-Starling curve) (Fig. 4) reveals that liraglutide treatment results in a shift of the relationship of EDV to CO such that CO increases as EDV increases in liraglutide-treated animals relative to their saline counterparts. Classically, this relationship has been used to establish whether a system is demonstrating an inotropic response. We therefore interpret this set of observations as further evidence for a modest positive inotropic effect of liraglutide in obesity, even in the setting of significant myocardial infarction.
Cardiac Efficiency
Pioneering work by Suga (32,33) demonstrated a linear relationship between PVA and MvO2. Therefore, the data obtained with transient inferior vena cava occlusion in this study enabled us to use PVA as an index of MvO2. This index of oxygen consumption was similar between groups at baseline (P = 0.29). Despite similar PVAs, cardiac power (work per unit time; estimated here as the triple product of stroke volume, mean aortic pressure, and heart rate) was significantly greater at baseline in liraglutide-treated animals (Fig. 3D) at rest (P = 0.03) and over the range of dobutamine administration (P = 0.04). The relationship between cardiac power (work) and PVA (MvO2) is an index of cardiac efficiency (Fig. 5). Owing to enhanced power without attendant increases in MvO2, liraglutide treatment resulted in a significant enhancement of cardiac efficiency under conditions of enhanced metabolic demand imposed by dobutamine.
Obesity and ischemia-related heart failure are associated with reduced cardiac function and with impaired work efficiency (34,35), making therapies that simultaneously improve function and efficiency an attractive prospect. Our observations suggest that liraglutide may provide this advantageous combination of effects. The mechanism(s) underlying the improved work efficiency is of some interest. It is well recognized that utilization of fatty acids as a fuel source in the heart is accompanied by some ATP consumption unrelated to contractility through effects including an unfavorable phosphate-to-oxygen ratio, mitochondrial uncoupling, and futile cycling of metabolic intermediates (36). By corollary, switching away from fatty acid utilization can allow improved efficiency. Previous studies of GLP-1 agonists in animal models and in humans have described shifts in myocardial fuel selection toward glucose (11,37), with the important caveat that obesity and T2DM appear to induce resistance to these fuel-selection effects of GLP-1 agonists including in the swine model used in the current studies (10). The effects we observed were specific to the circumstance of acutely increased work under β-adrenergic stimulation. However, the response to acute increases in myocardial work under β-adrenergic stimulation is to preferentially utilize fatty acids, including mobilizing fatty acid stores from adipose tissue (36). The effect we observed prevailed despite these effects. Effects of GLP-1 on handling of metabolic intermediates, such as pyruvate (38) or effects to modulate mitochondrial handling of fuels or mitochondrial ATP production could help explain the observed effects but such phenomena have not been directly evaluated to date. Further study of GLP-1 effects on myocardial substrate selection and ATP generation, evaluating the effects of treatment type, duration, and metabolic status as modulators of these effects is needed.
βADR Expression
In light of the different β-adrenergic responsiveness induced by liraglutide treatment, we evaluated βADR expression in the myocardium (Fig. 6). Unexpectedly, and in contrast to the observed enhancements of adrenergic responsiveness relative to saline-treated animals, the normally perfused myocardium of liraglutide-treated animals exhibited ∼50% lower levels of β1ADR. This raises the possibility that liraglutide is affecting function and efficiency via effects on adrenergic responsiveness. It is well recognized that βADR antagonism can improve function in chronic heart failure (39) and that via effects to reduce fatty acid oxidation, βADR activation can improve work efficiency as well (40). Specific evaluations of effects on β-adrenergic responsiveness, and the role of adrenergic signaling as a modulator of GLP-1 agonist effects on contractility and work efficiency will help clarify the effect of the observed changes in receptor density.
Although the increased cardiac function in liraglutide-treated swine despite lower expression of β1ADR may seem paradoxical, this phenotypic combination has been previously observed as conferring benefit in other clinically relevant scenarios (41–43). Reduction in β1ADR signaling, via β-blockade, is frequently used to improve cardiac function, including in the setting of heart failure (44). Reducing β1ADR signaling disrupts the positive feedback loop (maladaptive adrenergic signaling) that pushes the heart toward hypertrophy and eventually failure (45) while also enhancing efficiency via decreased myocardial fat oxidation (40). Other ways that GLP-1 agonism might be influencing cardiac mechanical work without additional demand for myocardial oxygen uptake include effects on calcium handling (as seen, for example, with digoxin or milrinone) or effects on the contractile machinery (46). Prior proteomic studies performed by our laboratory (12) found that exendin-4, another GLP-1 agonist, changed the expression of key calcium-handling proteins, components and regulators of sarcomeric proteins, and protein mediators of intermediary metabolism.
Some efforts to explore the signaling mechanism supporting effects of GLP-1 on myocardial function have been undertaken. Noyan-Ashraf et al. (47) recently demonstrated significant enhancement to cardiac function with liraglutide therapies in obese mice that could be abolished through the application of an AMPK inhibitor. We previously found enhanced P38–mitogen-activated protein kinase activity in response to direct application of GLP-1 (7-36) to porcine myocardial slices (10). These pathways represent targets of further investigations to better understand the cardioprotective and hemodynamic effects of GLP-1–related therapies. Among other considerations is the question whether effects are exerted via direct effects on the canonical receptor, effects on a noncanonical receptor, or secondary effects resulting from effects in peripheral tissue. Our finding that responsiveness to adrenergic stimulation is preserved with liraglutide and that efficiency is improved in the treatment arm provides new opportunity for potentially translational applications of GLP-1–based therapies.
Limitations
Molecular analysis after euthanasia was limited by the need for intact, uncompromised heart slices for accurate infarct measurement. Formalin fixation and staining with tetrazolium chloride prevented subsequent use of these tissues for gel-based analysis or ELISA. Biopsy samples from formalin-fixed tissues were used for immunohistochemistry. To minimize bias inherent to histologic analysis, we used digital pathology techniques to quantify stain. Liraglutide treatment was associated with decreased weight gain across the study, introducing modest differences in obesity at the time of the study. Although our power to demonstrate small effects was limited by the relatively small numbers of animals in the study, these samples were sufficient to identify large important effects on key outcome variables.
Conclusions and Implications
This study is the first to identify the potential for GLP-1–based therapies to modulate myocardial β1ADR abundance and, by extension, the potential for liraglutide therapies to improve cardiac performance of significantly infarcted hearts in an energetically favorable fashion via attenuation of maladaptive β1ADR signaling, similar to β-blockade therapies used to combat chronic heart failure. These findings could explain recent observations by Marso et al. (6), who found that the rate of fatal cardiovascular events, nonfatal myocardial infarction, and nonfatal stroke was lower in liraglutide-treated patients with T2DM than the placebo group. Taken together, these data support that liraglutide (and potentially other GLP-1 agonists) therapies can augment cardiac efficiency and function through alterations to βADR expression and sensitivity, independent of changes to infarct area.
Article Information
Funding. Support was provided by National Heart, Lung, and Blood Institute grant HL-117620 (J.D.T. and K.J.M., primary investigators) and by National Center for Advancing Translational Sciences grant TL1-TR-000162 (A. Shekhar, primary investigator).
Duality of Interest. No potential conflicts of interest relevant to this article were reported.
Author Contributions. D.J.S., J.N.N., M.A.E., A.M.C., and A.G.G. performed studies and reviewed and edited the manuscript. D.J.S. and A.G.G. wrote the manuscript. J.D.T. and K.J.M. contributed to discussion and reviewed and edited the manuscript. J.T.S. assisted with data analysis. A.G.G. is the guarantor of this work and, as such, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
References
- 1.Robinson LE, Holt TA, Rees K, Randeva HS, O’Hare JP. Effects of exenatide and liraglutide on heart rate, blood pressure and body weight: systematic review and meta-analysis. BMJ Open 2013;3:e001986 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Goodwill AG, Tune JD, Noblet JN, et al. . Glucagon-like peptide-1 (7-36) but not (9-36) augments cardiac output during myocardial ischemia via a Frank-Starling mechanism. Basic Res Cardiol 2014;109:426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Timmers L, Henriques JP, de Kleijn DP, et al. . Exenatide reduces infarct size and improves cardiac function in a porcine model of ischemia and reperfusion injury. J Am Coll Cardiol 2009;53:501–510 [DOI] [PubMed] [Google Scholar]
- 4.Mogensen UM, Andersson C, Fosbøl EL, et al. . Cardiovascular safety of combination therapies with incretin-based drugs and metformin compared with a combination of metformin and sulphonylurea in type 2 diabetes mellitus--a retrospective nationwide study. Diabetes Obes Metab 2014;16:1001–1008 [DOI] [PubMed] [Google Scholar]
- 5.Pfeffer MA, Claggett B, Diaz R, et al.; ELIXA Investigators . Lixisenatide in patients with type 2 diabetes and acute coronary syndrome. N Engl J Med 2015;373:2247–2257 [DOI] [PubMed] [Google Scholar]
- 6.Marso SP, Daniels GH, Brown-Frandsen K, et al.; LEADER Steering Committee; LEADER Trial Investigators . Liraglutide and cardiovascular outcomes in type 2 diabetes. N Engl J Med 2016;375:311–322 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bastien M, Poirier P, Lemieux I, Després JP. Overview of epidemiology and contribution of obesity to cardiovascular disease. Prog Cardiovasc Dis 2014;56:369–381 [DOI] [PubMed] [Google Scholar]
- 8.Mathew B, Francis L, Kayalar A, Cone J. Obesity: effects on cardiovascular disease and its diagnosis. J Am Board Fam Med 2008;21:562–568 [DOI] [PubMed] [Google Scholar]
- 9.Qiao Q, Grandy S, Hiller J, Kostev K. Clinical and patient-related variables associated with initiating GLP-1 receptor agonist therapy in type 2 diabetes patients in primary care in Germany. PLoS One 2016;11:e0152281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Moberly SP, Mather KJ, Berwick ZC, et al. . Impaired cardiometabolic responses to glucagon-like peptide 1 in obesity and type 2 diabetes mellitus. Basic Res Cardiol 2013;108:365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gejl M, Søndergaard HM, Stecher C, et al. . Exenatide alters myocardial glucose transport and uptake depending on insulin resistance and increases myocardial blood flow in patients with type 2 diabetes. J Clin Endocrinol Metab 2012;97:E1165–E1169 [DOI] [PubMed] [Google Scholar]
- 12.Sassoon DJ, Goodwill AG, Noblet JN, et al. . Obesity alters molecular and functional cardiac responses to ischemia/reperfusion and glucagon-like peptide-1 receptor agonism. Basic Res Cardiol 2016;111:43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Goodwill AG, Mather KJ, Conteh AM, Sassoon DJ, Noblet JN, Tune JD. Cardiovascular and hemodynamic effects of glucagon-like peptide-1. Rev Endocr Metab Disord 2014;15:209–217 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Haddock RE, Hill CE. Sympathetic overdrive in obesity involves purinergic hyperactivity in the resistance vasculature. J Physiol 2011;589:3289–3307 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Berwick ZC, Dick GM, O’Leary HA, et al. . Contribution of electromechanical coupling between Kv and Cav1.2 channels to coronary dysfunction in obesity. Basic Res Cardiol 2013;108:370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Suga H, Hayashi T, Shirahata M. Ventricular systolic pressure-volume area as predictor of cardiac oxygen consumption. Am J Physiol 1981;240:H39–H44 [DOI] [PubMed] [Google Scholar]
- 17.Westerhof N. Cardiac work and efficiency. Cardiovasc Res 2000;48:4–7 [DOI] [PubMed] [Google Scholar]
- 18.Poudyal H. Mechanisms for the cardiovascular effects of glucagon-like peptide-1. Acta Physiol (Oxf) 2016;216:277–313 [DOI] [PubMed] [Google Scholar]
- 19.Harada K, Grossman W, Friedman M, et al. . Basic fibroblast growth factor improves myocardial function in chronically ischemic porcine hearts. J Clin Invest 1994;94:623–630 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Potz BA, Sabe AA, Elmadhun NY, et al. . Glycogen synthase kinase 3β inhibition improves myocardial angiogenesis and perfusion in a swine model of metabolic syndrome. J Am Heart Assoc 2016;5:e003694 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kristensen J, Mortensen UM, Schmidt M, Nielsen PH, Nielsen TT, Maeng M. Lack of cardioprotection from subcutaneously and preischemic administered liraglutide in a closed chest porcine ischemia reperfusion model. BMC Cardiovasc Disord 2009;9:31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ekström K, Dalsgaard M, Iversen K, et al. . Effects of liraglutide and ischemic postconditioning on myocardial salvage after I/R injury in pigs. Scand Cardiovasc J 2017;51:8–14 [DOI] [PubMed] [Google Scholar]
- 23.Noyan-Ashraf MH, Momen MA, Ban K, et al. . GLP-1R agonist liraglutide activates cytoprotective pathways and improves outcomes after experimental myocardial infarction in mice. Diabetes 2009;58:975–983 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Connelly KA, Advani A, Zhang Y, et al. . Dipeptidyl peptidase-4 inhibition improves cardiac function in experimental myocardial infarction: role of stromal cell-derived factor-1α. J Diabetes 2016;8:63–75 [DOI] [PubMed] [Google Scholar]
- 25.van den Wijngaard JP, Schulten H, van Horssen P, et al. . Porcine coronary collateral formation in the absence of a pressure gradient remote of the ischemic border zone. Am J Physiol Heart Circ Physiol 2011;300:H1930–H1937 [DOI] [PubMed] [Google Scholar]
- 26.Margulies KB, Hernandez AF, Redfield MM, et al.; NHLBI Heart Failure Clinical Research Network . Effects of liraglutide on clinical stability among patients with advanced heart failure and reduced ejection fraction: a randomized clinical trial. JAMA 2016;316:500–508 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lønborg J, Kelbæk H, Vejlstrup N, et al. . Exenatide reduces final infarct size in patients with ST-segment-elevation myocardial infarction and short-duration of ischemia. Circ Cardiovasc Interv 2012;5:288–295 [DOI] [PubMed] [Google Scholar]
- 28.Woo JS, Kim W, Ha SJ, et al. . Cardioprotective effects of exenatide in patients with ST-segment-elevation myocardial infarction undergoing primary percutaneous coronary intervention: results of exenatide myocardial protection in revascularization study. Arterioscler Thromb Vasc Biol 2013;33:2252–2260 [DOI] [PubMed] [Google Scholar]
- 29.Lønborg J, Vejlstrup N, Kelbæk H, et al. . Exenatide reduces reperfusion injury in patients with ST-segment elevation myocardial infarction. Eur Heart J 2012;33:1491–1499 [DOI] [PubMed] [Google Scholar]
- 30.Lovshin JA, Barnie A, DeAlmeida A, Logan A, Zinman B, Drucker DJ. Liraglutide promotes natriuresis but does not increase circulating levels of atrial natriuretic peptide in hypertensive subjects with type 2 diabetes. Diabetes Care 2015;38:132–139 [DOI] [PubMed] [Google Scholar]
- 31.Burkhoff D, Mirsky I, Suga H. Assessment of systolic and diastolic ventricular properties via pressure-volume analysis: a guide for clinical, translational, and basic researchers. Am J Physiol Heart Circ Physiol 2005;289:H501–H512 [DOI] [PubMed] [Google Scholar]
- 32.Suga H. Total mechanical energy of a ventricle model and cardiac oxygen consumption. Am J Physiol 1979;236:H498–H505 [DOI] [PubMed] [Google Scholar]
- 33.Suga H. Ventricular energetics. Physiol Rev 1990;70:247–277 [DOI] [PubMed] [Google Scholar]
- 34.How OJ, Aasum E, Severson DL, Chan WY, Essop MF, Larsen TS. Increased myocardial oxygen consumption reduces cardiac efficiency in diabetic mice. Diabetes 2006;55:466–473 [DOI] [PubMed] [Google Scholar]
- 35.Knaapen P, Germans T, Knuuti J, et al. . Myocardial energetics and efficiency: current status of the noninvasive approach. Circulation 2007;115:918–927 [DOI] [PubMed] [Google Scholar]
- 36.Lopaschuk GD, Ussher JR, Folmes CD, Jaswal JS, Stanley WC. Myocardial fatty acid metabolism in health and disease. Physiol Rev 2010;90:207–258 [DOI] [PubMed] [Google Scholar]
- 37.Hansen J, Brock B, Bøtker HE, Gjedde A, Rungby J, Gejl M. Impact of glucagon-like peptide-1 on myocardial glucose metabolism revisited. Rev Endocr Metab Disord 2014;15:219–231 [DOI] [PubMed] [Google Scholar]
- 38.Hall JL, Stanley WC, Lopaschuk GD, et al. . Impaired pyruvate oxidation but normal glucose uptake in diabetic pig heart during dobutamine-induced work. Am J Physiol 1996;271:H2320–H2329 [DOI] [PubMed] [Google Scholar]
- 39.Bristow MR, Gilbert EM, Abraham WT, et al.; MOCHA Investigators . Carvedilol produces dose-related improvements in left ventricular function and survival in subjects with chronic heart failure. Circulation 1996;94:2807–2816 [DOI] [PubMed] [Google Scholar]
- 40.Sharma V, Dhillon P, Wambolt R, et al. . Metoprolol improves cardiac function and modulates cardiac metabolism in the streptozotocin-diabetic rat. Am J Physiol Heart Circ Physiol 2008;294:H1609–H1620 [DOI] [PubMed] [Google Scholar]
- 41.Eichhorn EJ, Bedotto JB, Malloy CR, et al. . Effect of beta-adrenergic blockade on myocardial function and energetics in congestive heart failure. Improvements in hemodynamic, contractile, and diastolic performance with bucindolol. Circulation 1990;82:473–483 [DOI] [PubMed] [Google Scholar]
- 42.Kernis SJ, Harjai KJ, Stone GW, et al. . Does beta-blocker therapy improve clinical outcomes of acute myocardial infarction after successful primary angioplasty? J Am Coll Cardiol 2004;43:1773–1779 [DOI] [PubMed] [Google Scholar]
- 43.Grover GJ, Kostis JB, Weiss HR, Li JK, Kovacs T, Kedem J. Effect of beta-adrenoceptor stimulation or blockade on regional myocardial function and regional O2 consumption during myocardial ischemia. Arch Int Pharmacodyn Ther 1988;291:68–87 [PubMed] [Google Scholar]
- 44.Bristow MR. Beta-adrenergic receptor blockade in chronic heart failure. Circulation 2000;101:558–569 [DOI] [PubMed] [Google Scholar]
- 45.Esler M, Kaye D, Lambert G, Esler D, Jennings G. Adrenergic nervous system in heart failure. Am J Cardiol 1997;80:7L–14L [DOI] [PubMed] [Google Scholar]
- 46.ter Keurs HE. The interaction of Ca2+ with sarcomeric proteins: role in function and dysfunction of the heart. Am J Physiol Heart Circ Physiol 2012;302:H38–H50 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Noyan-Ashraf MH, Shikatani EA, Schuiki I, et al. . A glucagon-like peptide-1 analog reverses the molecular pathology and cardiac dysfunction of a mouse model of obesity. Circulation 2013;127:74–85 [DOI] [PubMed] [Google Scholar]