Abstract
In cervical artificial disc replacement (C-ADR), sometimes we encountered with such cases that implants of adjacent height both fit the target disc space properly. No study was available discussing the choice of implant height and the clinical outcomes under such circumstance. The purpose of this study was to evaluate the impact of different implant heights on the clinical outcomes and radiographic results when the implants of adjacent height both fit the disc space properly. This retrospective study included 34 patients underwent single-level C-ADR at the C5–C6 level at our institution. In these 34 patients, implant with either 5 mm height or 6 mm height fit the surgical level properly without overstretching the disc space or the facet joint space. Clinical outcomes were evaluated using the Japanese Orthopedic Association score, visual analog scale (VAS), and Neck Disability Index. Radiographic assessments were conducted on static and dynamic radiographs for the determination of the disc space height, intersegmental range of motion (ROM), and the ROM of the functional spinal unit (FSU) at the surgical level. The baseline information of the patients, such as age, gender, weight, follow-up time, and diagnosis, was similar between the 2 groups (P > .05). Postoperative mean VAS in group B was significantly lower than that in group A (2.1 ± 0.7 vs. 2.7 ± 1.0, P < .05). The mean VAS decrease in group B was significantly larger than that in group A (5.3 ± 0.8 vs. 4.6 ± 1.1, P < .05). Significant difference was found in the postoperative disc height of the surgical segment between the 2 groups (6.4 ± 0.4 mm vs. 7.5 ± 0.5 mm, P < .05). No significant differences were noted in the intersegmental ROM and ROM of the FSU between the 2 groups both before the surgery and at the last follow-up (P > .05). No hypermobility or instability was observed in these patients. Our results suggested that when implants of adjacent height both fit the disc space properly, using the larger implant could result in better pain relief without the risk of segmental hypermobility in patients underwent single-level C-ADR at the C5–C6 level.
Keywords: artificial disc replacement, cervical spine, clinical outcomes, implant height, range of motion
1. Introduction
Cervical artificial disc replacement (C-ADR) is a safe and effective option for the treatment of patients with cervical radiculopathy or myelopathy due to single- or bi-level disc degeneration.[1–4] Additional to the effective symptom relief and neurological function recovery, the primary benefit of cervical arthroplasty is to restore the intervertebral space height and maintain the intersegmental range of motion (ROM). Besides, patients underwent C-ADR could return to work in a relatively short period of time.
The implant size selection is essential for the fulfillment of the function of the cervical artificial disc. In order to obtain the primary stability as well as the mobility of the cervical artificial disc, the implant should fit snugly in the intervertebral disc space without overstretching the disc space or the facet joint space. If the implant height is too small, the primary stability of the implant could not be achieved. On the other hand, if the implant height is too large, it could result in hypermobility at the surgical segment and increase the incidence of postoperative neck pain. In clinical practice, sometimes we encountered with such cases that 2 implants of adjacent heights both fit the target disc space properly, according to surgeon's experience or on the intraoperative C-arm radiograph (Fig. 1). Under such circumstance, would the surgical outcomes be different if the choice of implant height differed? To the best of our knowledge, no previous studies have discussed this problem.
Figure 1.
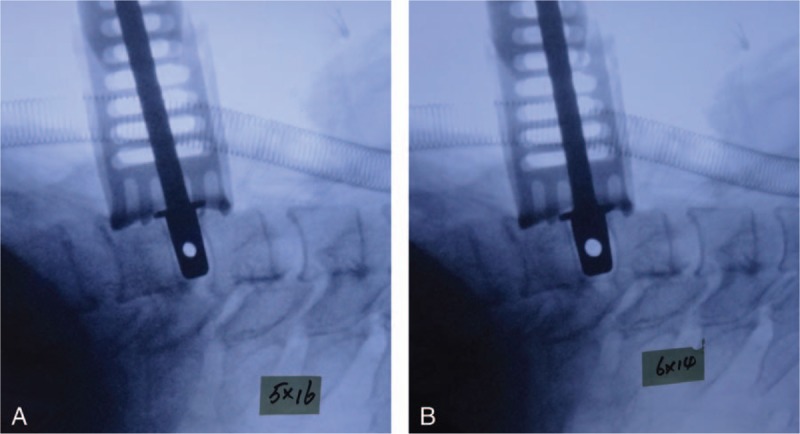
Implant size selection in cervical artificial disc replacement. Trial head of 5 mm height (A). Trial head of 6 mm height (B). Trial heads of both 5 mm height and 6 mm height fit the disc space properly without overstretching the disc space of the facet joint space.
The purpose of the present study was to evaluate the impact of different implant heights on the clinical outcomes and radiographic results when the implants of adjacent height both fit the disc space properly.
2. Materials and methods
2.1. Study design
This was a retrospective study from a cohort of patients underwent C-ADR at our institution from January 2008 to May 2014. All the patients signed the informed consent that their data would be used for research purposes. The inclusion criteria were as follow. Patients underwent single-level C-ADR at the C5–C6 level. Both of the 5 mm height trial and the 6 mm height trial provided snug fit without exceeding the adjacent normal disc height or overstretching the facet joint space (Fig. 1). The exclusion criteria were as follow. Patients underwent single-level C-ADR other than the C5–C6 level, multilevel C-ADR or hybrid surgery. Cases in which the 5 mm height trial can not fit the intervertebral disc space snuggly. Cases in which intervertebral disc space or facet joint space was confirmed overstretching by intraoperative C-arm image when using the 6 mm height trial. The included patients were then divided into 2 groups, where in group A the implant height was 5 mm and in group B the implant height was 6 mm.
2.2. Surgical procedure
All the operations were performed by 1 surgeon (HL). After general anesthesia, the patient was placed in the supine position. The neck was fixed in the neutral position with the neck supported by a rolled drape. A standard Smith–Robinson approach was adopted to expose the target level. After partial removal of the disc, the Casper cervical retractor (B. Braun Medical Inc., Bethlehem, PA) was applied to facilitate the complete discectomy and decompression. Then the retractor was removed. The endplate preparation was completed using a high-speed burr and the rasp, with great caution to preserve the cortical bone as much as possible. The implant trial was then used to determine the implant size with the help of the intraoperative C-arm fluoroscopy. The trial should provide snug fit without exceeding the adjacent normal disc height or overstretching the facet joint space. In this group patients, both the 5 mm height trial and the 6 mm trial suitable candidates. The final implant size was decided according to the surgeon's preference in these cases. After the proper placement of the Prestige-LP prosthesis (Medtronic Sofamor Danek, Memphis, TN), a drain was inserted and the incision was closed subsequently.
2.3. Clinical evaluation
The Japanese Orthopedic Association (JOA) score,[5] visual analog scale (VAS),[6] and Neck Disability Index (NDI)[7] were adopted for the clinical evaluation before the surgery and at each follow-up.
2.4. Radiographic assessment
The radiographic assessments were performed preoperatively and at the last follow-up. All the assessments were performed in the Canvas 11.0 software (ACD System Company, Fort Lauderdale, Florida) by 2 authors, independently. Each parameter was taken twice. The mean value was used for the analysis. The intervertebral disc space height (disc height) was determined on the lateral cervical radiographs (Fig. 2). The disc height was defined as the average of the anterior disc height and the posterior disc height. The intersegmental ROM and the ROM of functional spinal unit (FSU) were determined on the dynamic full flexion and extension radiographs (Fig. 3). Kyphotic angle was considered as a negative value. The angular difference between the values measured on the flexion and the extension radiographs was defined as the ROM.[8,9]
Figure 2.
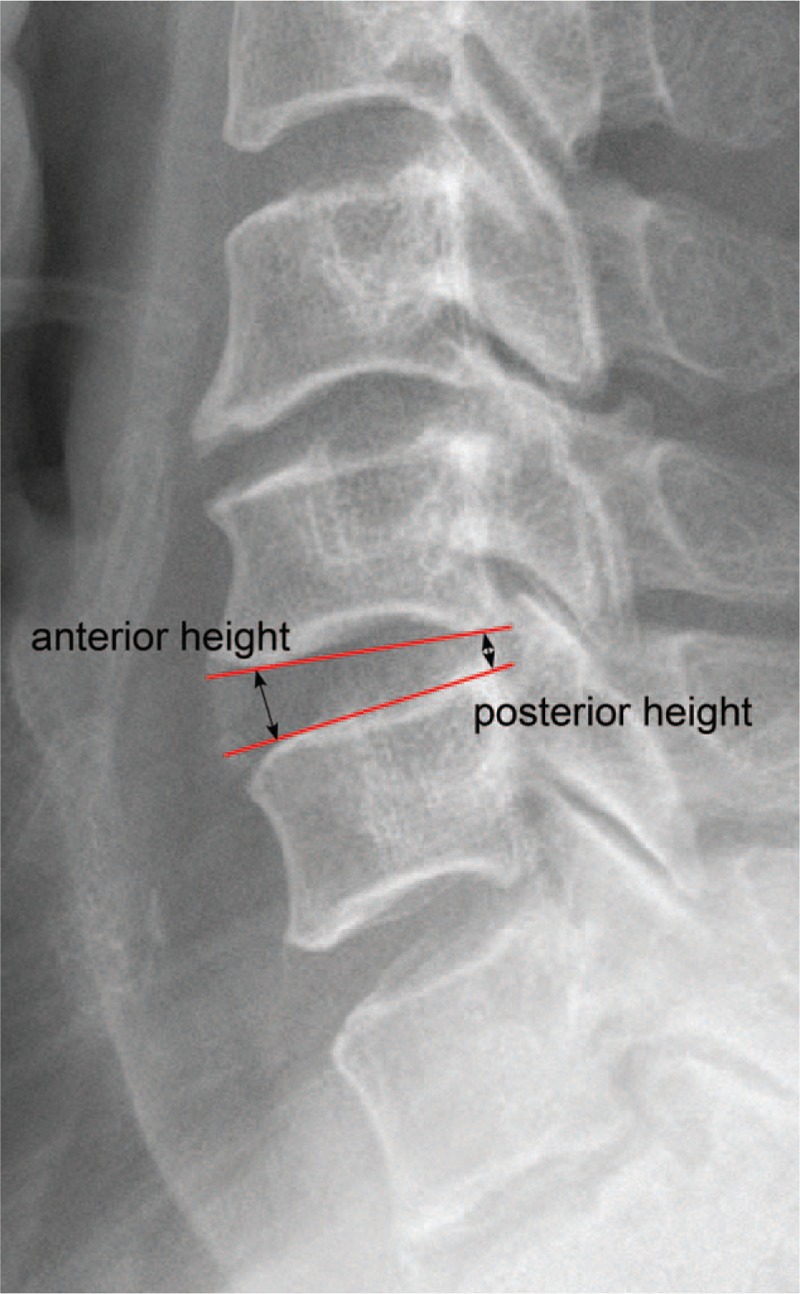
Disc height was defined as the average of the anterior height and the posterior height.
Figure 3.
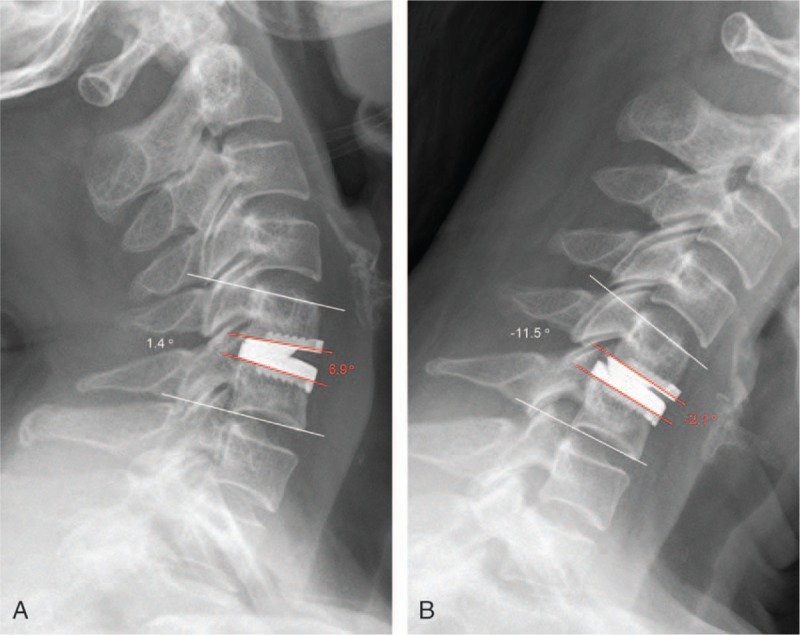
Intersegmental ROM and the ROM of FSU were determined on the dynamic full flexion (A) and extension (B) radiographs. The intersegmental ROM = 6.9° − (−2.1°) = 9°. The ROM of the FSU = 1.4° − (−11.5°) = 12.9°. FSU = functional spinal unit, ROM = range of motion.
2.5. Statistical analysis
Continuous variables were presented as mean ± standard deviation. Statistical analysis was performed by the SPSS version 19.0 software (SPSS Inc., Chicago, IL). The Student t and chi-squared tests were used to evaluate the differences of baseline parameters between the 2 groups. The paired t test was used to detect the difference of clinical outcomes and ROMs before the surgery and at the last follow-up in the 2 groups, respectively, if the data were normally distributed. If not, the Wilcoxon rank-sum test would be used. A P value of <.05 was considered statistically significant.
3. Results
3.1. Patient information
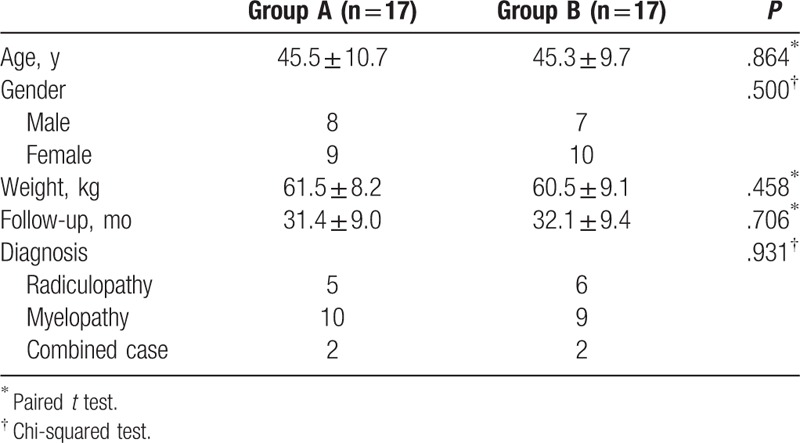
From January 2008 to May 2014, a total of 355 patients underwent C-ADR or hybrid surgery at our institution, among them 116 patients underwent single-level C-ADR at the C5–C6 level. Finally, a total of 34 patients (17 in group A and 17 in group B) were included in this study according to the inclusion and exclusion criteria. The patient baseline information, such as age, gender, weight, follow-up time, and diagnosis, was similar between the 2 groups (P > .05, Table 1). All patients in the 2 groups have completed at least 2-year follow-up. The average follow-up time was 31.8 months, ranging from 24 to 56 months.
Table 1.
Baseline information of the included patients.
3.2. Clinical outcomes
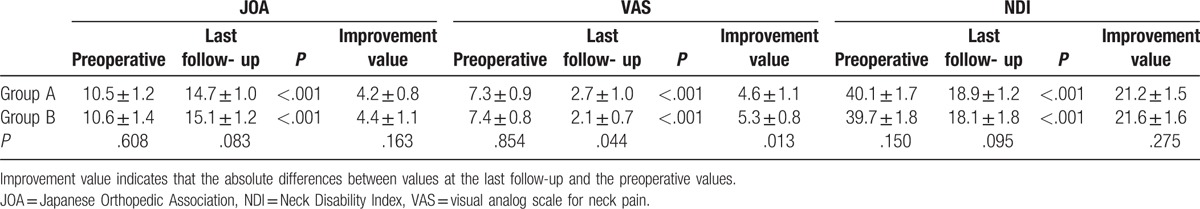
Preoperative JOA, VAS, and NDI were similar between the 2 groups (P > .05). The JOA scores at last follow-up increased significantly from the JOA scores before the surgery in both groups (P < .05). The VAS and NDI decreased significantly in both groups. Postoperative mean VAS in group B was significantly lower than that in group A (2.1 ± 0.7 vs. 2.7 ± 1.0, P < .05). The mean decrease of VAS in group B was significantly larger than that in group A (5.3 ± 0.8 vs. 4.6 ± 1.1, P < .05, Table 2).
Table 2.
JOA score, VAS, and NDI before and after cervical artificial disc replacement.
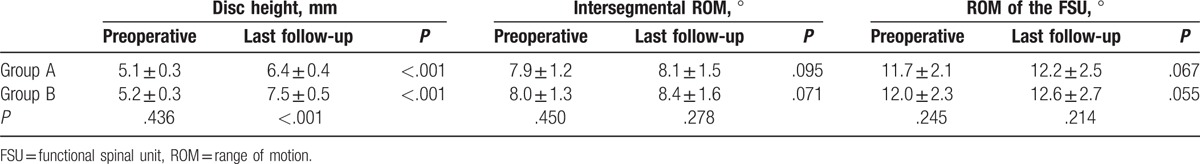
3.3. Radiographic results
The disc height of the surgical segment increased significantly postoperatively in both groups (P < .05). Significant difference was found in the postoperative disc height of the surgical segment between the 2 groups (6.4 ± 0.4 mm vs. 7.5 ± 0.5 mm, P < .05). Both the postoperative intersegmental ROM and ROM of the FSU were larger than those before the surgery, without significant difference (P > .05). No significant differences were noted in the intersegmental ROM and ROM of the FSU between the 2 groups (P > .05) (Table 3).
Table 3.
Radiographic assessments before and after cervical artificial disc replacement.
4. Discussion
The present study demonstrated that when implants of adjacent height both fit the disc space properly, using the implant of larger height could result in better pain relief without the risk of segmental hypermobility in patients underwent single-level C-ADR at the C5–C6 level.
In this study, patients in both groups obtained favorable clinical outcomes as the JOA scores increased and the VAS and NDI decreased significantly from those before the surgery. The VAS at the last follow-up was significantly smaller in group B than that in group A (2.1 ± 0.7 vs. 2.7 ± 1.0, P < .05) and the decrease of VAS in group B was significantly larger than that in group A (5.3 ± 0.8 vs. 4.6 ± 1.1, P < .05). Nerve root impingement due to herniated disc or narrowed intervertebral foramen was accounted for the development of the cervical radiculopathy. The pain relief could be achieved by decompression of the nerve root by the removal of the herniated disc and the increment of the intervertebral foramen size. An et al[10] concluded that, for discs with a preoperative baseline height between 3.5 and 6 mm, approximately 2 mm increment of the disc height above the baseline would result in maximal incremental change of the foramen size. In this study, the preoperative disc height in both groups was about 5 mm. The average disc height increment in group B was 2.3 mm, whereas in group A the increment was 1.3 mm. Therefore, 1 possible explanation of the better pain relief in group B might contribute to the larger increment of the foramen size.
Motion preservation is an important function of the artificial cervical disc. A few studies[11,12] suggested that the postoperative intersegmental ROM were affected by the disc height or disc height increment. Rohlmann et al[13] first reported the effect of implant height on intersegmental ROM in the lumbar spine, and concluded that an implant height 2 mm in excess of the normal disc space could increase the intersegmental ROM during standing and extension. In the study by Kang et al,[12] the preoperative ROM and the ROM at the last follow-up at the surgical level were 7.4° and 10.4°, respectively, with the mean disc height increment of 1.6 mm. They concluded that disc height increment was significantly correlated with postoperative intersegmental ROM. The increased disc height could result in the decreased overlap of the facet joint articulation, reducing the restriction of the flexion–extension motion, which would facilitate the cervical rotation in the sagittal plane.[14] On the one hand, disc height increment seemed to be beneficial to the motion preservation of the artificial cervical disc. However, on the other hand, excessive disc height increment might contribute to the facet joint subluxation, which could subsequently result in hypermobility or instability at the surgical level.[15] In this study, the disc height increment in group A and group B was 1.3 and 2.3 mm, respectively. No overstretching of the disc space or the facet joint space was recorded. Our results demonstrated that cervical motion was well preserved in the patients underwent single-level C-ADR. Besides, the postoperative intersegmental ROMs were similar between the 2 groups without hypermobility being noted.
There were several limitations in this study. First, this retrospective study only included patients underwent single-level C-ADR at the C5–C6 level. We chose to conduct the present study on C5–C6 level because the disc degeneration was most commonly seen at this level. We chose the single-level C-ADR patients for the analysis because the ROMs varied at different cervical levels. Although the current study could not be used directly to interpret the impact of different implant height on clinical outcomes and radiographic results at other cervical levels, it provided valuable reference information for implant height selection. Second, the sample size of this study was limited because this study was conducted at a single institutional set and because only part of C-ADR cases were encountered with 2 proper implant sizes. Prospective study of large sample sizes is needed to further verify our findings. Third, only one kind of artificial cervical disc was investigated. Many artificial cervical discs are currently available with different designs and structures. Thus, studies using different kinds of artificial cervical discs are needed to assess the effect of implant height on clinical outcomes and ROMs in C-ADR patients.
In conclusion, favorable clinical outcomes were achieved and cervical motion was well preserved in patients underwent single-level C-ADR at the C5–C6 level in the short-term follow-up. When implants of adjacent height both fit the disc space properly at the C5–C6 level, the implant with larger height might be a better choice.
Footnotes
Abbreviations: C-ADR = cervical artificial disc replacement, FSU = functional spinal unit, JOA = Japanese Orthopedic Association, NDI = Neck Disability Index, ROM = range of motion, VAS = visual analog score.
The authors have no funding and conflicts of interest to disclose.
References
- [1].Chen F, Yang J, Ni B, et al. Clinical and radiological follow-up of single-level Prestige LP cervical disc replacement. Arch Orthop Trauma Surg 2013;133:473–80. [DOI] [PubMed] [Google Scholar]
- [2].Garrido BJ, Taha TA, Sasso RC. Clinical outcomes of Bryan cervical disc arthroplasty a prospective, randomized, controlled, single site trial with 48-month follow-up. J Spinal Disord Tech 2010;23:367–71. [DOI] [PubMed] [Google Scholar]
- [3].Du J, Li M, Liu H, et al. Early follow-up outcomes after treatment of degenerative disc disease with the discover cervical disc prosthesis. Spine J 2011;11:281–9. [DOI] [PubMed] [Google Scholar]
- [4].Nabhan A, Ahlhelm F, Shariat K, et al. The ProDisc-C prosthesis: clinical and radiological experience 1 year after surgery. Spine 2007;32:1935–41. [DOI] [PubMed] [Google Scholar]
- [5].Fukui M, Chiba K, Kawakami M, et al. Japanese Orthopaedic Association Cervical Myelopathy Evaluation Questionnaire (JOACMEQ): part 2. Endorsement of the alternative item. J Orthop Sci 2007;12:241–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Price DD, McGrath PA, Rafii A, et al. The validation of visual analogue scales as ratio scale measures for chronic and experimental pain. Pain 1983;17:45–56. [DOI] [PubMed] [Google Scholar]
- [7].Vernon H, Mior S. The Neck Disability Index: a study of reliability and validity. J Manipulative Physiol Ther 1991;14:409–15. [PubMed] [Google Scholar]
- [8].Hayes MA, Howard TC, Gruel CR, et al. Roentgenographic evaluation of lumbar spine flexion-extension in asymptomatic individuals. Spine 1989;14:327–31. [DOI] [PubMed] [Google Scholar]
- [9].Lim MR, Girardi FP, Zhang K, et al. Measurement of total disc replacement radiographic range of motion: a comparison of two techniques. J Spinal Disord Tech 2005;18:252–6. [PubMed] [Google Scholar]
- [10].An HS, Evanich CJ, Nowicki BH, et al. Ideal thickness of Smith–Robinson graft for anterior cervical fusion. A cadaveric study with computed tomographic correlation. Spine 1993;18:2043–7. [DOI] [PubMed] [Google Scholar]
- [11].Peng CW, Quirno M, Bendo JA, et al. Effect of intervertebral disc height on postoperative motion and clinical outcomes after Prodisc-C cervical disc replacement. Spine J 2009;9:551–5. [DOI] [PubMed] [Google Scholar]
- [12].Kang KC, Lee CS, Han JH, et al. The factors that influence the postoperative segmental range of motion after cervical artificial disc replacement. Spine J 2010;10:689–96. [DOI] [PubMed] [Google Scholar]
- [13].Rohlmann A, Zander T, Bergmann G. Effect of total disc replacement with ProDisc on intersegmental rotation of the lumbar spine. Spine 2005;30:738–43. [DOI] [PubMed] [Google Scholar]
- [14].Liu J, Ebraheim NA, Haman SP, et al. How the increase of the cervical disc space height affects the facet joint: an anatomy study. Spine 2006;31:E350–4. [DOI] [PubMed] [Google Scholar]
- [15].Gautschi OP, Corniola MV, Stienen MN, et al. Postoperative segmental hypermobility after cervical arthroplasty: a possible pathomechanism for outcome failure. J Clin Neurosci 2015;22:1194–6. [DOI] [PubMed] [Google Scholar]


