Abstract
Background:
Although the method has been used widely, one of the greatest challenges for intramedullary nailing is to position the distal locking screw. A new technology, the electromagnetic navigation system, is a radiation-free way to locate the position of the drill bit and provide 3-dimensional real-time feedback of location and orientation of the drill bit relative to the locking holes. The purpose of our study was to evaluate the reliability and efficiency of the free-hand technique compared to the new electromagnetic navigation system.
Methods:
Fifty-four patients with femoral fracture who needed treatment with intramedullary nails were divided into 2 groups. One group including 26 patients underwent distal locking using the standard free-hand method, whereas the electromagnetic navigation system was used with the other 29 patients. Intraoperative fluoroscopy exposure times, screw insertion times, and healing times were recorded; these parameters were used for comparison between the 2 groups.
Results:
There were 17 males and 9 females who had femoral intramedullary nails using the free-hand technique, whereas 21 males and 8 females received intramedullary nails using the electromagnetic navigation system. The mean time of distal locking was 19.5 ± 6.0 minutes in the free-hand (FH) group, whereas the time was 6.1 ± 1.4 minutes in the electromagnetic (ET) group. The exposure time for the FH group was 26.8 ± 13.3 seconds and 2.2 ± 1.1 seconds for the ET group. Healing time proved to be comparable in the FH and ET groups (16.4 ± 3.7 weeks vs 15.1 ± 2.8 weeks).
Conclusion:
Under the premise of achieving the same effect, the electromagnetic navigation system has the advantage of less distal locking time and less radiation dose.
Keywords: distal femoral fracture, electromagnetic navigation system, free-hand technique, intramedullary nailing, radiation exposure
1. Introduction
Intramedullary nailing is the gold standard for the treatment of diaphyseal fractures of long bones and has the advantages of minimal soft tissue injury and stable fracture fixation.[1–4] More studies have recognized that intramedullary nailing can provide high union and low complication rates in the treatment of long bone fractures. The first commercially available interlocking nail was introduced in 1972.[1] For surgeons, one of the greatest challenges for intramedullary nails is to position the distal locking screw, although several methods have been widely applied in clinical therapy because of the advantages of intramedullary nails.
Numerous systems and techniques have been introduced to solve the problem. These approaches include a free-hand fluoroscopic method to localize distal locking holes,[5] a laser guiding system,[6] the flag and grid technique,[7] self-locking nailing systems[8] and proximally mounted targeting devices.[9] However, each device has some limitations, radiation exposure to the surgeon and patients during orthopedic procedures using the free-hand fluoroscopic method and the laser guiding system is a universal concern. The self-locking nailing systems do not exhibit the same torsional qualities as distally locked screws and the technique are not always acceptable. Proximally mounted targeting devices seem to fail due to lacking compensation for insertion related deformation of the implant. The flag and grid technique, a method that many think is too unwieldy to be practical. Therefore, the free-hand fluoroscopic technique remains the most popular method for distal locking. The free-hand technique, which is based on fluoroscopy, is widely used to accurately position the distal locking screw. Therefore, the patient, surgeons and all staff in the operating room are exposed to lots of radiation. Furthermore, the free-hand technique is related to surgeon proficiency and has a steep learning curve. The radiation dose and the accuracy of screw placement should be considered. A new, advanced technique should be developed to solve the problem.
The electromagnetic navigation system is a radiation-free way to confirm the position of the drill bit and to show 3-dimensional real-time feedback of the location and orientation of the drill bit relative to the locking holes.[10] The reliability, operation time, and radiation exposure were discussed in our research to compare the efficacy of the standard free-hand technique with the new electromagnetic navigation system for distal locking of femoral nails.
2. Materials and method
Fifty-four patients with femoral fracture were enrolled in our study and, after signing informed consent, were treated with intramedullary nails (Smith & Nephew, Inc., Memphis, TN) at the Second Hospital of Anhui Medical University from February 2010 to December 2015. According to the Declaration of Helsinki 2013, every research study involving human subjects should be registered in a publicly accessible database. The Research Registration Unique Identifying Number (UIN) is researchregistry1734. The study was approved by the ethics committee of our hospital. Injury mechanisms of the patients included traffic accidents, traumatic injury, falling from a height, and any other accidents; patients with pathological or periprosthetic fractures were excluded. Participants were numbered and randomly divided into 2 groups. One group including 26 patients underwent distal locking with the standard free-hand method, whereas the electromagnetic navigation system (SURESHOT, Smith & Nephew, Inc., Memphis, TN) was used with the other 29 patients. Two distal screws were inserted by the same surgeon in both groups.
For the group undergoing the free-hand fluoroscopic technique, it was crucial to confirm that the 2 distal nail holes appeared as a perfect circle when inserting distal screws based on the fluoroscopic imaging. Then, a skin incision was made through the soft tissue, down to the bone cortex. The drill bit and the distal locking hole stayed on the same axis. The screw insertion was performed when the hole was contacted with the tip of the screw.
The electromagnetic navigation system is widely used to localize the drill position for screws during distal interlocking. The targeting system mainly consists of 3 parts, a computerized control unit located within the system's display unit, a hand-held “donut-shaped” targeter that produces a focused electromagnetic field and a sensor probe inserted in the nail and mediating information to the control unit (Fig. 1). The whole process utilizes computerized electromagnetic field tracking technology via a probe that is placed in the center of the nail, along with a computer-based calibrated software to allow a real-time system for distal locking without fluoroscopy. A nail length-adjusted probe was inserted into the proximal end of the nail according to the real-time information provided by electromagnetic tracking data. For the distal locking procedure, the surgeon drilled through a central slot in the electromagnetic field generator. The location of the drill and locking holes were visualized on a computer monitor providing real-time information for the surgeon during the locking procedure. The distal screws were inserted when the green and red targeting circles overlapped on the computer monitor (Fig. 2). The correct positioning of the distal screw was finally confirmed based on fluoroscopy.
Figure 1.
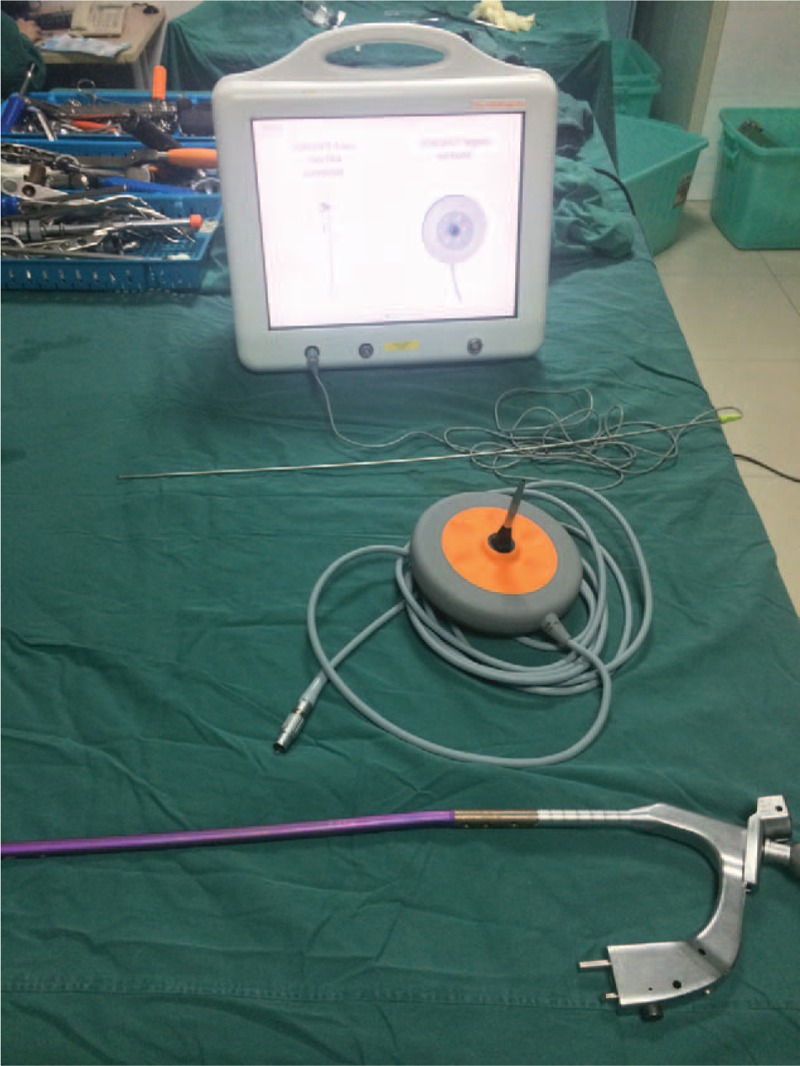
The electromagnetic navigation system. From top to bottom: (1) a computerized control unit. (2) The electromagnetic probe. (3) The electromagnetic field generator. (4) The nail mounted onto the jig with an insertion device.
Figure 2.
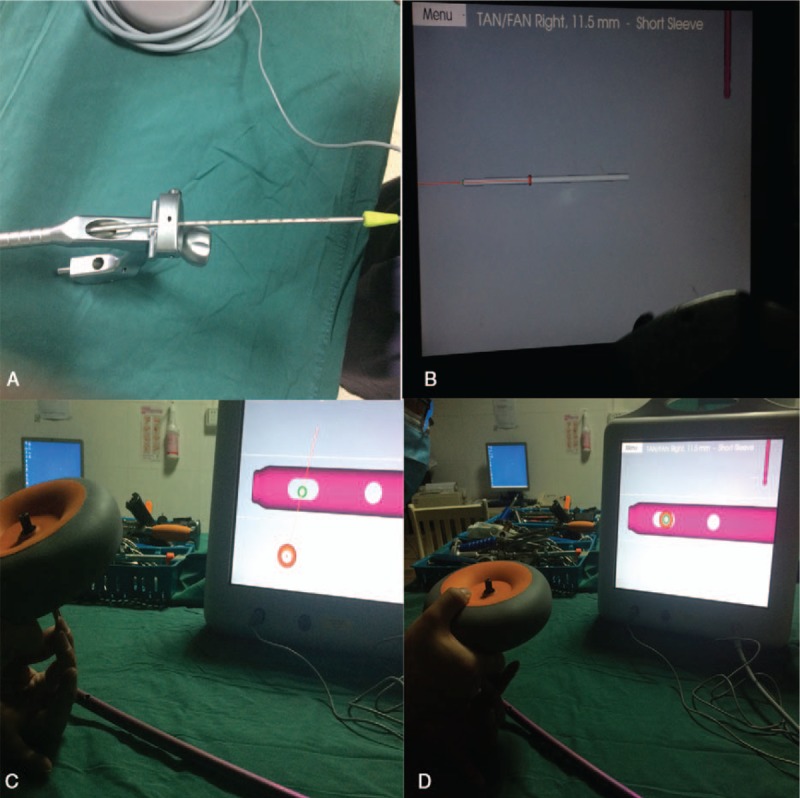
Distal locking using the electromagnetic navigation system. (A) A nail length adjusted probe was inserted into the proximal end of the nail. (B) The real-time information provided by electromagnetic tracking data. (C) The location of drill and locking holes was visualized on a computer monitor. (D) The distal screws were inserted when the green and the red targeting circles were overlaps.
The standardized time of both groups was recorded with a stopwatch. Intraoperative fluoroscopy exposure times, screw insertion times, and healing times were documented in both groups. The total number of unsuccessful and intraoperative complications was recorded for both techniques. All patients were followed up at 1, 3, 6, and 12 months with radiographs to evaluate the recovery of fractures (Fig. 3).
Figure 3.

(A) Distal locking screws inserted using free-hand fluoroscopic guidance. (B) Distal locking screws inserted using electromagnetic navigation. Both groups achieved bony union after 6 months follow-up.
Statistical Package for the Social Sciences (SPSS) was used for statistical analysis. Data for continuous variables, including intraoperative fluoroscopy exposure times, distal locking times and healing times, were presented as the mean ± standard deviation. Normality was analyzed using the Kolmogorov–Smirnov test. Relationships between nominal variables were calculated using the chi-squared test and median levels between the groups were compared using the Mann–Whitney U test. P < .05 was considered significant for all statistical data.
3. Result
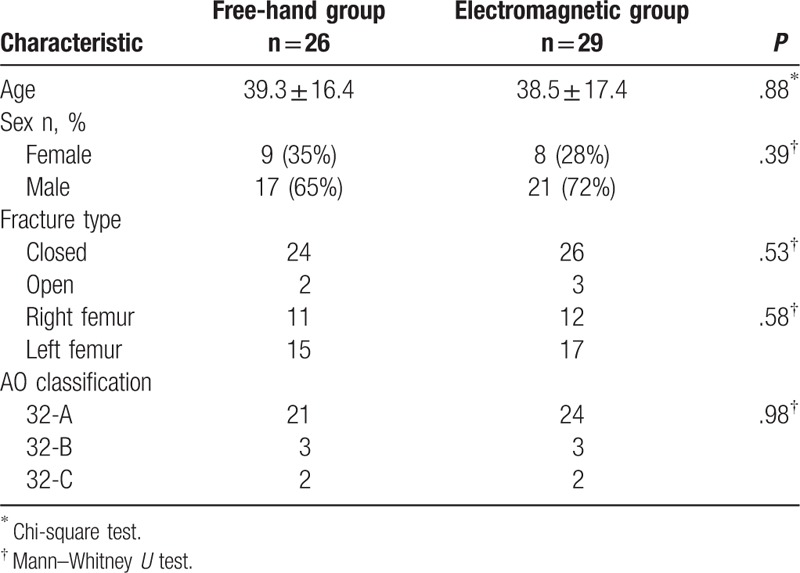
There were 17 males and 9 females who had femoral intramedullary nailing with the free-hand technique, whereas 21 males and 8 females underwent intramedullary nailing with the electromagnetic navigation system. The mean age of the free-hand group was 39.27 years (SD,16.37), where the mean age of the ET group was 38.55 years (SD,17.37). The mechanisms of injury included traffic accidents (40,73%), traumatic injury (3,5%), falling from a height (6,11%), and any other accidents (6,11%). According to the AO classification, patients with femoral fractures included in our study were classified as type 32-A (45), type 32-B (6), and type 32-C (4). There were 5 open fractures and all were categorized into grade I according to the Gustilo classification. No patients complicated with multiple other injuries underwent the operation after corresponding treatment. There were no significant differences regarding age, gender, injury mechanism, AO classification, or open fractures (Table 1).
Table 1.
Patient characteristics of 2 groups.
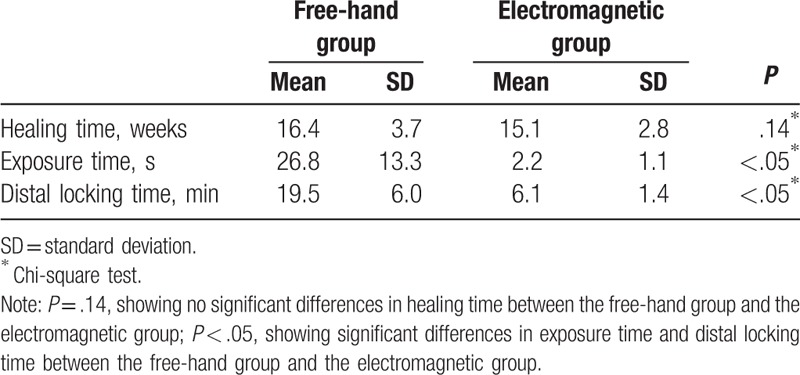
The mean time of distal locking was 19.5 ± 6.0 minutes with the FH technique, whereas the time was 6.1 ± 1.4 minutes in the ET group. The exposure time for the FH group was 26.8 ± 13.3 s and 2.2 ± 1.1 s for the ET group. The healing time proved to be comparable in the FH and ET groups (16.4 ± 3.7 weeks vs 15.1 ± 2.8 weeks). The mean time of distal locking for placing the distal screws was statistically significantly shorter in the ET group compared to the FH group (P < .05), and the exposure time was significantly reduced in the ET group compared to the FH group. There was no significant difference in healing time between the 2 groups (P = .14) (Table 2).
Table 2.
Results of 2 groups.
4. Discussion
In our study, we found that the operative time for distal screw insertion and radiation exposure time was significantly reduced using the electromagnetic navigation system compared with the free-hand technique. Another comparison showed that radiation exposure was not eliminated in the ET group, although the time of radiation exposure was significantly reduced. Fluoroscopy was used to identify the location of the distal screw and to make sure the drill and the nail holes were aligned during intramedullary nailing.
Intramedullary nails continue to be the gold standard for the treatment of diaphyseal fractures of long bones.[1–4] However, how to insert the distal locking screw correctly is a confusing problem for the surgeon. With the traditional method, radiation-independent aiming systems, surgeon cannot correctly determine the location of distal screws due to deformation of the nail during the procedure.[11,12] Although numerous innovative systems and techniques have been introduced to settle this problem, the free-hand technique is still the most effective method for the placement of distal locking screws.
Although the free-hand technique plays an important role in distal locking screw insertion, there are still many serious effects on the surgeon. The most important is radiation exposure, the occupational exposure recommended by the International Commission on Radiological Protection (ICRP) for all orthopedic surgeons and patients who have been exposed to radiation over 5 years is no more than 50 mSv in any 1 year.[13] Kirousis et al[14] reported that the primary operator should not exceed the dose constraint of 10 mSv per year. During intramedullary nailing of the tibia, the surface dose to the gonads of the patients was less than 8.8 mGy and the maximum dose recorded being to the operator of the fluoroscopic equipment was 0.11 mSv. Muzaffar et al[15] proved that the hand and eye receive 0.27 mSv and 0.09 mSv per procedure, respectively, for the surgeon when using a thermoluminescent dosimeter to quantify the dose. Madan and Blakeway[16] designed a study to estimate the radiation hazard to patients and surgeons during intramedullary nailing for lower limb fractures. The results suggest that radiation dose is related to the distance from the x-ray beam, and the mean radiation dose was 1.36 mSv for the gonads of patients with femoral nailing. The radiation dose to the surgeon's hand for at 15, 30, and 60 cm for femoral nailing was 1.272, 0.314, and 0.080 mSv, respectively. In addition, the significant differences of radiation exposure exist in experienced versus inexperienced surgeons performing the free-hand technique. The radiation dose for consultant surgeon and middle-grade surgeon were 0.049, 0.077 mSv during identifying proximal nail insertion and distal locking. This conclusion has been proven by Blattert et al.[17] The electromagnetic navigation system is used to decrease the dose of radiation. In our study, we found that the electromagnetic navigation system achieved a positive result with less time and less radiation dose compared with the free-hand technique. The radiation dose to the surgeon is well under the maximum permissible dose recommended by the ICRP. However, extended periods of operation should be considered for misplacement of the distal locking screws.[18]
The electromagnetic navigation system, which decreases the time for distal locking of the intramedullary nail, was introduced to the clinic. Ciftdemir et al[19] reported that the mean time of image intensifier shots was 26.1 seconds, ranging from 16 to 41 seconds in the whole intramedullary nailing procedure used electromagnetic-manual guidance. Hoffmann et al[20] reported that the time for drilling the anteroposterior distal locking hole plus insertion of the screw was 84.04 s in the electromagnetic group and 186.22 s in the free-hand group. Uruc et al[5] reported that total fluoroscopy time and distal locking time were 48 seconds, 21 minutes for femoral fractures with an intramedullary nail in the free-hand group, whereas the time was 24 seconds, 8 minutes in the electromagnetic group. In this study, we found that the fluoroscopy time required to insert the distal interlocking screws and the insertion time of both screws were reduced significantly using the electromagnetic navigation technique compared with the free-hand method; the times were reduced to 2.2 seconds, 6.1 minutes, and 26.8 seconds, 19.5 minutes, respectively. The electromagnetic technique can achieve perfect circles and correctly find drill placement based on a real-time feedback system without radiation.
Distal locking failure is another major problem in the process of distal locking. The deformation of nails inserted into the medullary canal could be responsible for failure in distal locking. Anastopoulos et al[21] reported 5 unsuccessful cases in 127 patients being treated with the use of a proximally mounted aiming device. From our data, there were no failures in either group. It is possible that both target devices can compensate for the deformation of nails. In addition, all locking procedures were performed by an experienced surgeon and completed quickly. The mean time of the locking process was 19.5 minutes and 6.1 minutes in the free-hand group and the electromagnetic group, respectively. Compared with the free-hand technique, the electromagnetic technique has a short learning curve for the inexperienced surgeon. Langfitt et al[18] found that junior residents spent more time on inserting the distal screw with the free-hand technique. It is inevitable for the surgeon to receive an excessive dose of radiation, especially for surgeons who do not often perform intramedullary nailing. For these surgeons, the electromagnetic technique is an effective and accessible method because it is radiation-independent and has a short learning curve. This viewpoint was confirmed by Leroux et al.[22] The ET technique is one of the most common and effective methods, although many other methods have been developed to settle the problems of free-hand distal locking.
We did not design a control for comparison with the time of distal insertion between experienced and inexperienced surgeons. In both groups, we used the time of exposure to evaluate the radiation without quantifying the exposure dose. Our study presents a persuasive outcome based on the facts, although the study has several limitations. The insertion of distal screws was performed by the same surgeon in both groups, thus eliminating the variability caused by a different surgeon.
5. Conclusion
From our study, no patients incurred complications related to the intramedullary nails. Bone union was achieved in both groups with an assessment of radiographs after the procedure. The free-hand technique and electromagnetic navigation system are feasible and effective methods for distal locking. Under the premise of achieving the same effect, the electromagnetic navigation system has the advantage of less distal locking time and less radiation dose. Further studies are required to strengthen the validity of our study outcomes, and we hope we can develop a method without any radiation in the future.
Footnotes
Abbreviations: ET = electromagnetic, FH = free-hand.
BH and ZS contributed equally to this study.
Funding: This work was supported by the National Natural Science Foundation of China (81671204), the Natural Science Foundation of Anhui province (1708085QH221), the Hefei Independent Innovative Foundation (YW201608080006), Traditional Chinese Medicine Research Foundation of Anhui Province (2016zy92), and Anhui Medical University Science Foundation (2013xkj032)
The authors have no conflicts of interest to disclose.
References
- [1].Kempf I, Grosse A, Beck G. Closed locked intramedullary nailing. Its application to comminuted fractures of the femur. J Bone Joint Surg Am 1985;67:709–20. [PubMed] [Google Scholar]
- [2].Rapp M, Gros N, Zachert G, et al. Improving stability of elastic stable intramedullary nailing in a transverse midshaft femur fracture model: biomechanical analysis of using end caps or a third nail. J Orthop Surg Res 2015;10:96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Ricci WM, Gallagher B, Haidukewych GJ. Intramedullary nailing of femoral shaft fractures: current concepts. J Am Acad Orthop Surg 2009;17:296–305. [DOI] [PubMed] [Google Scholar]
- [4].Winquist RA, Hansen ST, Jr, Clawson DK. Closed intramedullary nailing of femoral fractures. A report of five hundred and twenty cases. J Bone Joint Surg Am 1984;66:529–39. [PubMed] [Google Scholar]
- [5].Uruc V, Ozden R, Dogramaci Y, et al. The comparison of freehand fluoroscopic guidance and electromagnetic navigation for distal locking of intramedullary implants. Injury 2013;44:863–6. [DOI] [PubMed] [Google Scholar]
- [6].Goulet JA, Londy F, Saltzman CL, et al. Interlocking intramedullary nails. An improved method of screw placement combining image intensification and laser light. Clin Orthop Relat Res 1992;281:199–203. [PubMed] [Google Scholar]
- [7].Yiannakopoulos CK, Kanellopoulos AD, Apostolou C, et al. Distal intramedullary nail interlocking: the flag and grid technique. J Orthop Trauma 2005;19:410–4. [DOI] [PubMed] [Google Scholar]
- [8].Lepore L, Lepore S, Maffulli N. Intramedullary nailing of the femur with an inflatable self-locking nail: comparison with locked nailing. J Orthop Sci 2003;8:796–801. [DOI] [PubMed] [Google Scholar]
- [9].Anastopoulos G, Ntagiopoulos PG, Chissas D, et al. Distal locking of tibial nails: a new device to reduce radiation exposure. Clin Orthop Relat Res 2008;466:216–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Moreschini O, Petrucci V, Cannata R. Insertion of distal locking screws of tibial intramedullary nails: a comparison between the free-hand technique and the SURESHOT Distal Targeting System. Injury 2014;45:405–7.24140179 [Google Scholar]
- [11].Krettek C, Mannss J, Miclau T, et al. Deformation of femoral nails with intramedullary insertion. J Orthop Res 1998;16:572–5. [DOI] [PubMed] [Google Scholar]
- [12].Moor BK, Ehlinger M, Arlettaz Y. Distal locking of femoral nails. Mathematical analysis of the appropriate targeting range. Orthop Traumatol Surg Res 2012;98:85–9. [DOI] [PubMed] [Google Scholar]
- [13].Wrixon AD. New ICRP recommendations. J Radiol Prot 2008;28:161–8. [DOI] [PubMed] [Google Scholar]
- [14].Kirousis G, Delis H, Megas P, et al. Dosimetry during intramedullary nailing of the tibia. Acta Orthop 2009;80:568–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Muzaffar TS, Imran Y, Iskandar MA, et al. Radiation exposure to the surgeon during femoral interlocking nailing under fluoroscopic imaging. Med J Malaysia 2005;60(suppl C):26–9. [PubMed] [Google Scholar]
- [16].Madan S, Blakeway C. Radiation exposure to surgeon and patient in intramedullary nailing of the lower limb. Injury 2002;33:723–7. [DOI] [PubMed] [Google Scholar]
- [17].Blattert TR, Fill UA, Kunz E, et al. Skill dependence of radiation exposure for the orthopaedic surgeon during interlocking nailing of long-bone shaft fractures: a clinical study. Arch Orthop Trauma Surg 2004;124:659–64. [DOI] [PubMed] [Google Scholar]
- [18].Langfitt MK, Halvorson JJ, Scott AT, et al. Distal locking using an electromagnetic field-guided computer-based real-time system for orthopaedic trauma patients. J Orthop Trauma 2013;27:367–72. [DOI] [PubMed] [Google Scholar]
- [19].Ciftdemir M, Tuncel SA, Ozcan M, et al. Does electromagnetic-manual guided distal locking influence rotational alignment in antegrade femoral nailing? Int Orthop 2015;39:507–12. [DOI] [PubMed] [Google Scholar]
- [20].Hoffmann M, Schroder M, Lehmann W, et al. Next generation distal locking for intramedullary nails using an electromagnetic X-ray-radiation-free real-time navigation system. J Trauma Acute Care Surg 2012;73:243–8. [DOI] [PubMed] [Google Scholar]
- [21].Anastopoulos G, Ntagiopoulos PG, Chissas D, et al. Evaluation of the Stryker S2 IM Nail Distal Targeting Device for reduction of radiation exposure: a case series study. Injury 2008;39:1210–5. [DOI] [PubMed] [Google Scholar]
- [22].Leroux T, Khoshbin A, Nousiainen MT. Training distal locking screw insertion skills to novice trainees: a comparison between fluoroscopic- and electromagnetic-guided techniques. J Orthop Trauma 2015;29:441–6. [DOI] [PubMed] [Google Scholar]


