Abstract
Rationale:
Pleomorphic carcinoma (PC) is a rare malignancy of the lung. It has a dual-cell component of spindle and/or giant cells, and of epithelial cells.
Patient Concerns and Diagnoses:
We presented a case of PC. A 69-year-old healthy asymptomatic woman who was occasionally found an abnormal shadow on her chest X-rays. A computerized tomography scan showed a mass located in the left lingular lobe and the percutaneous lung biopsy pathology confirmed sarcomatoid cancer.
Interventions and Outcomes:
The patient underwent pneumonectomy. A diagnosis of PC was confirmed after surgery through immunohistochemistry. The pathological stage was T2aN0M0 (Ib). Due to the patient's refusal, adjuvant chemotherapy was not taken and she has been living disease free for 12 months after the surgery.
Lessons:
PC of the lung represents a rare pathological entity. Surgical resection remains the cornerstone of the treatment and may offer the possibility of long-time survival in early-stage patients. More cases of PC should be reported to establish an optimal management.
Keywords: case report, primary lung pleomorphic carcinoma, surgical resection
1. Introduction
Pulmonary pleomorphic carcinoma (PC) is a rare malignant tumor of the lung and its incidence has been reported to range from 0.1% to 0.4% of all lung cancer.[1] According to the revised 2004 World Health Organization (WHO) classification, PC was grouped as a specific type of lung cancer with pleomorphic, sarcomatoid, or sarcomatous elements. As 1 of the 5 subtypes of sarcomatoid carcinomas, PC was defined as poorly differentiated adenocarcinoma, squamous cell carcinoma, or large cell carcinoma containing sarcomatoid components of spindle or giant cells in at least 10% of the cells or a carcinoma comprised entirely of giant and spindle cells.[2,3] PC has a more aggressive clinical course and a worse outcome than other nonsmall cell lung cancer (NSCLC).[4,5] In this study, we report a PC case with a patient who occasionally found a tumor located in the lingular lobe of left lung, received surgery treatment, and was finally diagnosed with PC by pathological examination.
2. Case report
A 69-year-old asymptomatic female was found an abnormal shadow on a chest X-ray during a regular health check-up. Then she was referred to Shandong Provincial Hospital Affiliated to Shandong University for further investigation.
She described her history of hypertension, diabetes, and depression and taken oral drugs to control the blood pressure, blood sugar, and the depression symptoms. The patient denied history of smoking and lung disease and had no respiratory complaints or other physical symptoms. She received the enhanced chest computerized tomography (CT) scan that showed a tumor located in the left lingular lobe (Figs. 1 and 2). Given that trans-bronchial lung biopsy or bronchial alveolar lavage might lead to a false-negative result, the percutaneous lung biopsy was undertaken to diagnosis precisely, and the biopsy pathology showed sarcomatoid cancer. Some other preoperative evaluations were also conducted including physical examinations, cardiac, and pulmonary function test. In addition, CT scans of the brain and abdomen and bone scintigraphy were performed to rule out distant metastasis. According to all the preoperative examinations, the clinical stage was classified as Ib stage and there was no obvious contraindication. The basic bronchoscopies were performed preoperatively to confirm the extent of tumor invasion. Based on all the examinations, the video-assisted thoracic surgery left lingular lobe with mediastinal lymph node dissection was carried out. The resected specimen showed a peripheral tumor measuring 4.0 cm in maximum diameter. Microscopic images showed that it was comprised 50% spindle cells, 30% giant cells, and 20% adenocarcinoma cells (Fig. 3). The final diagnosis was PC. Dissected hilar and mediastinal lymph nodes were free of metastatic disease. Postoperative adjuvant chemotherapy was not performed due to the patient's refusal and has been living cancer-free during the 12 months’ clinic visits after the surgery without any chief complaint. This study was approved by the Ethics Committee of Shandong Provincial Hospital Affiliated to Shandong University (Jinan, China).
Figure 1.
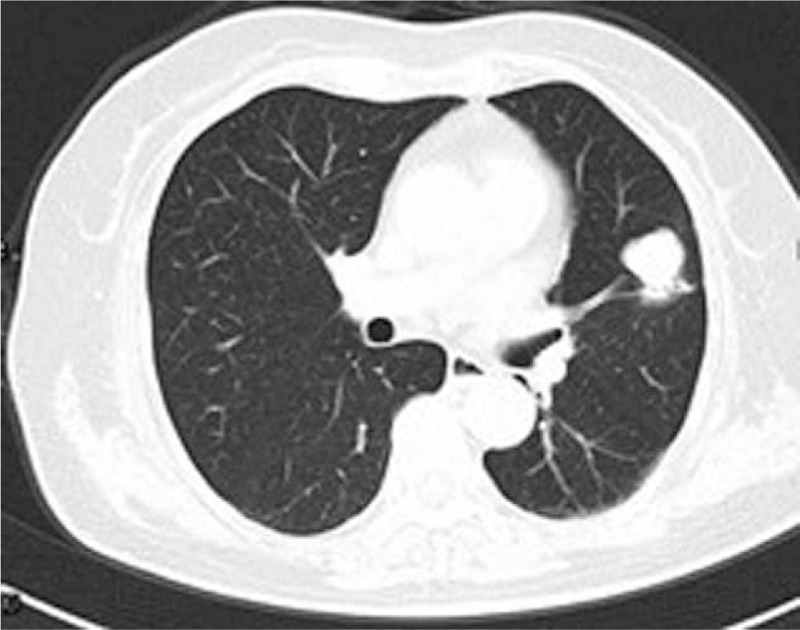
Computerized tomography (CT) scan showed a tumor located in the left lingular lobe.
Figure 2.
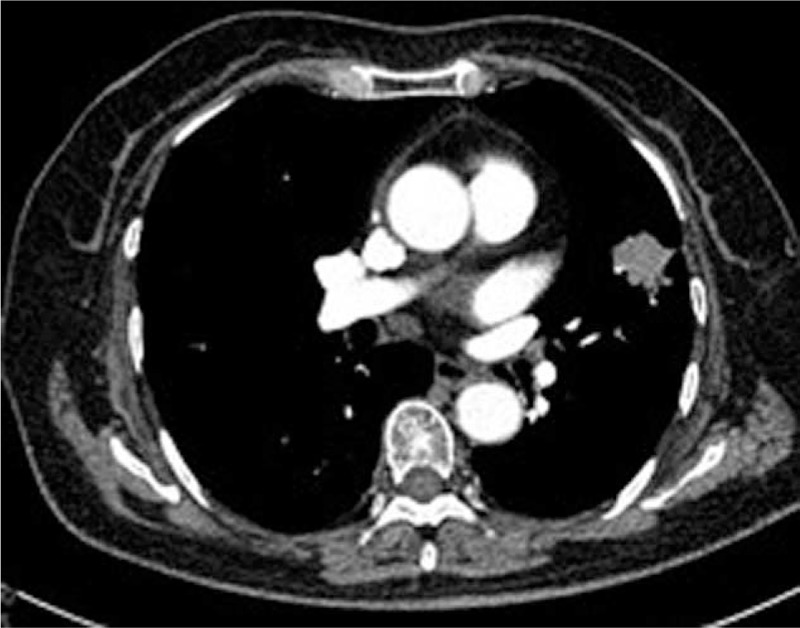
Contrasted CT scans showed the tumor with substantial enhancements. CT = computerized tomography.
Figure 3.
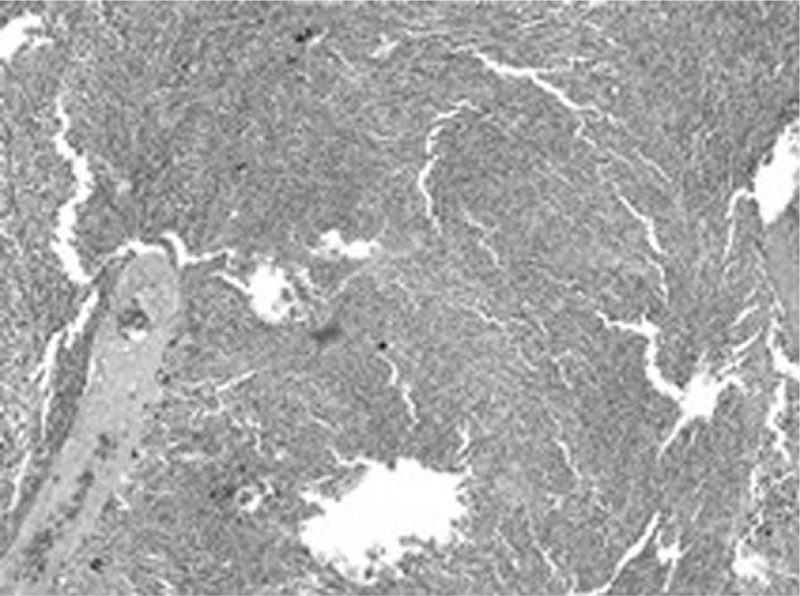
The postoperation pathology showed lung pleomorphic carcinoma with spindle cells, giant cells, and adenocarcinoma cells (hematoxylin and eosin ×100).
3. Discussion
PC is defined as a tumor that combines spindle or giant cell carcinoma with any of the more usual patterns of NSCLC.[6] Ever before, PC was considered a variant of other well-known lung cancers because of its biphasic appearance and its frequent association with other histological types. In PC, the most common carcinomatous element consists of conventional adenocarcinoma and squamous cell carcinoma and less commonly undifferentiated large cell carcinoma.[3] PC is 1 of the 5 subtypes of sarcomatoid carcinoma. Because of the limitation of biopsy tissues, pleomorphic carcinoma sometimes cannot be diagnosed precisely before the operation. It is easily mixed with the other 4 subtypes of sarcomatoid cancer: spindle cell carcinoma, giant cell carcinoma, carcinosarcoma, and pulmonary blastoma.
The incidence of PC has been reported to range from 0.1% to 0.4% of all lung cancers and only a few case reports have been published. Common clinical symptoms include irritate cough, hemosputum, chest pain, and fever. Mean age at diagnosis was 60 to 65 years, and more male patients were found with the gender ratio was about 2.1:1. 60% to 90% of the patients were exsmokers, which suggested a strong correlation with smoking.[1,4–6] PC patients were ever reported in different ethnic groups. The exact incidence was not reported in different ethnic groups because of the rare number. The patient in the study described no discomfort. Her regular health checkup revealed tumor occasionally. Radiologically, most lesions were peripheral large masses with substantial enhancements on contrasted CT scans. Lesions with the diameter longer than 5 cm often showed central low attenuation areas and myxoid degeneration, corresponded to regions of hemorrhage or necrosis. Cavity lesions were also often seen resulting from central necrosis.[7] The diagnosis of PC depended mainly on the postoperation pathological examination. Several monoclonal antibodies are available to evaluate the pulmonary epithelial tumor, particularly thyroid transcription factor-1, surfactant apoprotein-A, and cytokeratins. As for the sarcomatous elements, vimentin is always positive.
PC has a more aggressive clinical course and a worse outcome than other NSCLC. However, there has yet no consensus on the treatment of pleomorphic carcinoma. Usually, surgery is the first choice for the early stage of pleomorphic carcinoma. Palliative chemotherapy is always used in advanced pulmonary pleomorphic carcinoma. The targeted therapy may be an option for the epidermal growth factor receptor (EGFR) mutation patients. Given the tendency to early metastasis and the high relapse rate, more aggressive treatment strategy may be needed. PCs have a tendency to grow rapidly and to invade adjacent structures in the early stage. Several favorable prognostic factors have been reported, including complete surgical resection, no lymph nodes metastasis, lower pathologic stages, and tumor necrosis. On the other hand, pleural involvement was reported as an adverse prognostic factor.[8] Overall, the prognosis for PC is poor. Fishback et al and Rossi et al reported the median survival time is 8 to 19 months.[4,5] Chang et al[1] reported that 7 patients who received surgical resections were found distal metastases within a few months. They occurred in bone and organs, including brain, adrenal gland, esophagus, jejunum, rectum, and kidney.[1] The advanced pulmonary pleomorphic carcinoma was found to respond poorly to the platinum- and nonplatinum-based chemotherapy regimens. All of these are active in NSCLC and conventional radiation therapy has had little effect on PC.[9] Chang et al[1] also reported the median survival time was only 3 months for 9 inoperable cases that were treated by chemoradiotherapy. In our case, the patient received complete resection and the pathological stage was T2aN0M0 (Ib). Due to the patient's refusal, adjuvant chemotherapy was not taken and she has been living disease free for 12 months after the surgery without any complaint.
4. Conclusion
Pleomorphic carcinoma is a rare lung tumor with low incidence and an aggressive biological behavior. The prognosis of PC is still poorer than other nonsmall cell lung cancers. With 1 case, our study shows that surgical intervention and resection of the possible involved lymph node is appropriate for its treatment. It offers the possibility of long-time survival in an early stage patient. To establish the best effective treatment strategy for this type of cancer, we need more reports like this to compare with different treatment methods and effectiveness.
Acknowledgment
The authors thank Jing Helmersson from Department of Public Health and Clinical Medicine, Umea University, Sweden for revising the language.
Footnotes
Abbreviations: CT = computerized tomography, EGFR = epidermal growth factor receptor, NSCLC = nonsmall cell lung cancer, PC = pleomorphic carcinoma, WHO = World Health Organization.
XZ and YW contributed equally to this work.
The authors have no conflicts of interest to disclose.
References
- [1].Chang YL, Lee YC, Shih JY, et al. Pulmonary pleomorphic (spindle) cell carcinoma: peculiar clinicopathologic manifestations different from ordinary non-small cell carcinoma. Lung Cancer 2001;34:91–7. [DOI] [PubMed] [Google Scholar]
- [2].Brambilla E, Travis WD, Colby TV, et al. The new World Health Organization classification of lung tumours. Eur Respir J 2001;18:1059–68. [DOI] [PubMed] [Google Scholar]
- [3].Travis WD, Brambilla E, Muller-Hermelink HK, et al. (eds). World Health Organization Classification of Tumors: Pathology and Genetics of Tumours of the Lung, Pleura, Thymus and Heart. Lyon: IARC Press; 2004:53–58. [Google Scholar]
- [4].Fishback NF, Travis WD, Moran CA, et al. Pleomorphic (spindle/giant cell) carcinoma of the lung. A clinicopathologic correlation of 78 cases. Cancer 1994;73:2936–45. [DOI] [PubMed] [Google Scholar]
- [5].Rossi GCA, Sturn N, Migaldi M, et al. Pulmonary carcinomas with pleomorphic, sarcomatoid, or sarcomatous elements: a clinicopathlogic and immunohistochemical study of 75 cases. Am J Surg Pathol 2003;27:11–24. [DOI] [PubMed] [Google Scholar]
- [6].Yamamoto S, Hamatake D, Ueno T, et al. Clinicopathological investigation of pulmonary pleomorphic carcinoma. Eur J Cardiothorac Surg 2007;32:873–6. [DOI] [PubMed] [Google Scholar]
- [7].Kim TH, Kim SJ, Ryu YH, et al. Pleomorphic carcinoma of lung: comparison of CT features and pathologic findings. Radiology 2004;232:554–9. [DOI] [PubMed] [Google Scholar]
- [8].Raveglia F, Mezzetti M, Panigalli T, et al. Personal experience in surgical management of pulmonary pleomorphic carcinoma. Ann Thorac Surg 2004;78:1742–7. [DOI] [PubMed] [Google Scholar]
- [9].Bae HM, Min HS, Lee SH, et al. Palliative chemotherapy for pulmonary pleomorphic carcinoma. Lung Cancer 2007;58:112–5. [DOI] [PubMed] [Google Scholar]


