Abstract
The first sacral nerve root block (S1 nerve root block) is a practical procedure for patients with radiating lower back pain. In general, S1 nerve root block is performed under x-ray fluoroscopy. It is necessary to adjust the position of the patient and angle of fluoroscopy to properly visualize the first dorsal sacral foramen (dorsal S1 foramen). The purpose of this study was to analyze the location of dorsal S1 foramen and lumbar facet joint in S1 nerve root block.
A total of 388 patients undergoing x-ray fluoroscopy–guided S1 nerve root block in the prone position were examined. X-ray fluoroscopy was fixed at the corresponding location of facet joint of L4–5 and L5-S1. The relationship of the connecting line vertical to L5-S1 facet joint and upper margin sacrum was evaluated. The surface anatomical relationships between dorsal S1 foramen and lumbar facet joint were assessed.
Based on the localization of dorsal S1 foramen, the line drawn from point to upper margin sacrum passed through the dorsal S1 foramen in all cases. The horizontal distance from the spinous process to the dorsal S1 foramen was 25.9 ± 3.0 mm for men and 26.2 ± 1.4 mm for women. The horizontal distance from the between posterior superioriliac spine to the dorsal S1 foramen was 26.2 ± 2.7 mm for men and 26.8 ± 1.7 mm for women. The vertical distance from the upper margin of sacrum to dorsal S1 foramen to the dorsal S1 foramen was 45.6 ± 6.5 mm for men and 43.8 ± 6.0 mm for women.
The connecting line vertical to L5-S1 facet joint and upper margin sacrum is located on the same line from the dorsal S1 foramen. For difficult cases of locating dorsal S1 foramen, the lumbar facet joint can assist in predicting the vertical location of the dorsal S1 foramen.
Keywords: facet joint, first dorsal sacral foramen, first sacral nerve root block, posterior superioriliac spine, upper margin of sacrum
1. Introduction
The selective nerve root block, introduced by Macnab[1] in 1971, is a diagnostic test performed to detect whether a specific spinal nerve is the source of pain.[2] The first sacral nerve root block (S1 nerve root block) is a useful nerve block that is frequently applied to diagnose and treat pain associated to the S1 nerve root. Recent selective nerve block procedures have relied on ultrasound due to the disadvantage of radiation exposure and the need for fluoroscopy equipment.[3,4] However, limitations for ultrasound for selective nerve block procedures include high muscle density, deep nerve root, and transverse process impedance of the accurately position the needle and locating the site of intravascular injection.[4] Therefore, selective nerve root block is generally performed under x-ray fluoroscopy. It is necessary to adjust the position of the patient and angle of C-arm to properly visualize the first dorsal sacral foramen (dorsal S1 foramen). In addition, variations in sacrum and its components, especially the features on its dorsal surface, have been reported.[5] Because there is a limited explanation about anatomical path of S1 nerve, the present research was done with the aim of predicting the location of dorsal S1 foramen based on fluoroscopic findings from the S1 nerve root block procedure under x-ray fluoroscopy.
2. Methods
2.1. Patients
After informed consent was obtained, this single-center, retrospective study was conducted from January 2010 to December 2015. The study involved 388 patients with cases of S1 nerve, complaints of lower extremity pain radiating from the lumbar herniated intervertebral disc or spinal stenosis of S1 nerve root diagnosed by clinical and radiological procedures (magnetic resonance imaging or computed tomography), and S1 nerve root block under x-ray fluoroscopy. Exclusion criteria were cauda equina syndrome, history of lumbar spine surgery, severe compression fracture of lumbar spine, lumbarization, and sacralization.
2.2. Interventions
All the procedures were performed by 1 physician with experience of more than 1000 fluoroscopy-guided selective nerve root blocks. With the patient in the prone position, the skin was prepped and draped in a sterile fashion. Then, the S1 nerve root block was performed under C-arm (GEMSS) fluoroscopy using a 22-gauge, 60-mm disposable nerve block needle (K-3 Lancet point, Unisis Corp, Tokyo, Japan) and contrast medium (IOHEXOL). Before the S1 nerve root block, the patient was in the anteroposterior (AP) position, face down with a pillow parallel to the body. The S1 foramen was confirmed through contrast enhancement. In our experience, it is easier to confirm the location of the dorsal S1 foramen by placing the end-plate to upper margin of L5 rather than lower margin of L5 or upper margin of S1 for the S1 nerve root block. The patient was placed in the prone position with a pillow (8 cm in height) under the lower abdomen to reduce lumbar lordosis. The angle of x-ray fluoroscopy was adjusted to be between 10 and 30 degrees for the end plate of upper margin of L5 and the oblique position, to perform the S1 nerve root block. The site of entry was visualized by adjusting the fluoroscopic beam to align the dorsal S1 foramen with the ventral S1 foramen by rotating the C-arm cephalad and slightly laterally. The success of the blocking procedure was confirmed through contrast media.
2.3. Interpretation
From the AP view in a well exposed case of dorsal S1 foramen by separation of ventral and dorsal sacral foramen, (A) was the location of the dorsal S1 foramen, and (B) was the facet joint of L5-S1 lumbar area. X-ray fluoroscopy was fixed at the position in which L4–5 and L5-S1 facet joints met. A vertical line drawn from (B) to (A) was evaluated (Fig. 1). The horizontal distance from the vertical line of L5 spinous process to first dorsal sacral foramen was measured (a, Fig. 1). Horizontally, the correlation of the distance (b) between posterior superioriliac spine (PSIS) (C) and the vertical line connecting L5-S1 facet joint and dorsal S1 foramen was evaluated (Fig. 1). The vertical distance (c) from the upper margin of sacrum (D) to dorsal S1 foramen was measured (Fig. 1). Also, the difference of a, b, and c between genders was evaluated. Also, the location relationship between dorsal S1 foramen (A) and L5-S1 lumbar facet joint (B) from oblique view was evaluated (Fig. 2).
Figure 1.
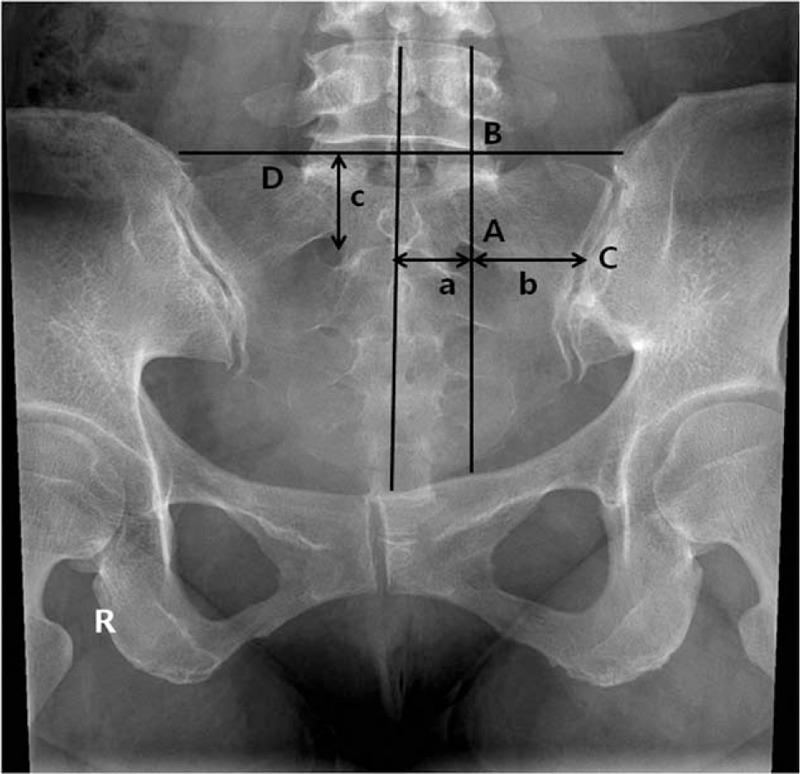
Anteroposterior view of lumbar spine and sacrum, (A) dorsal S1 foramen; (B) the facet joint of L5-S1 lumbar area; (C) posterior superioriliac spine; (D) upper margin of sacrum; (a) the horizontal distance from the vertical line of L5 spinous process to first dorsal sacral foramen; (b) the horizontal distance between posterior superioriliac and the vertical line connecting L5-S1 facet joint and dorsal S1 foramen; (c) the vertical distance from the upper margin of sacrum to dorsal S1 foramen.
Figure 2.
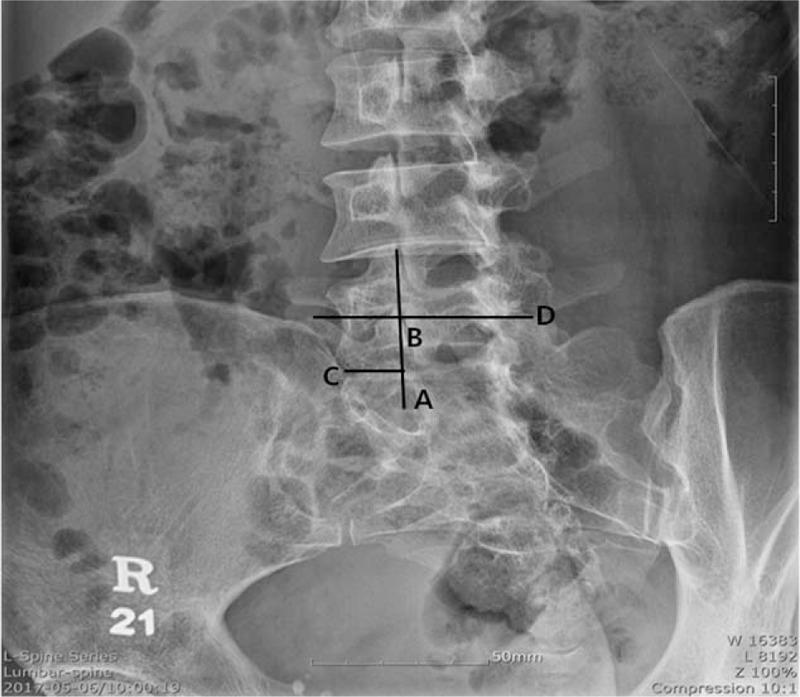
Oblique view of lumbar spine and sacrum, (A) dorsal S1 foramen; (B) the facet joint of L5-S1 lumbar area; (C) posterior superioriliac spine; (D) upper margin of sacrum.
2.4. Statistical analyses
The SPSS for Windows software package (ver. 19.0; SPSS Inc, Chicago, IL) was used for statistical analysis, and the sum and subtraction of the mean and standard deviation were described. To compare demographic data from the 2 groups, the χ2 test was used to assess categorical data, as appropriate. Student t test was used to analyze numerical data, as appropriate. Comparisons between men and women were done by independent sample t test. A P value of <.05 was considered statistically significant, except for Bonferroni correction. To exclude or reduce type I errors in the association analysis of each variables, Bonferroni corrections were used to adjust the P value for multiple testing.
3. Results
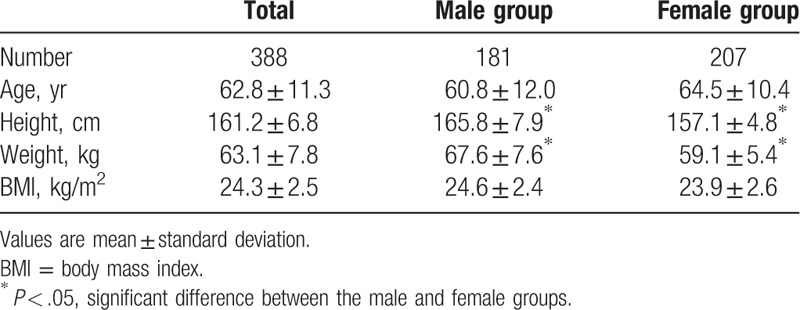
There were no complications after the block. There were 388 cases with the dorsal S1 foramen and ventral S1 foramen that were separated to expose the dorsal S1 foramen and no prior history of lumbar spine surgery, severe compression fracture of lumbar spine, lumbarization, and sacralization. Age, height, and weight of patients are shown in Table 1. Age and body mass index between male and female patients did not differ significantly, but height and weight differed significantly between the 2 groups (P < .05). All of the subjects studied were native South Koreans.
Table 1.
Demographic data.
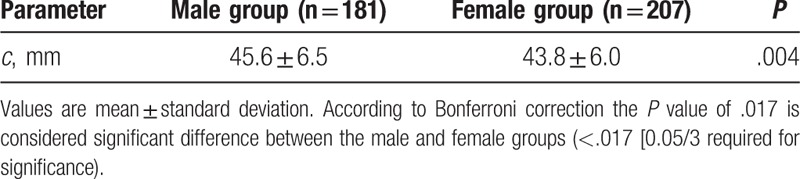
Based on the localization of dorsal S1 foramen, the line drawn from point (B) to the upper margin sacrum passed through the dorsal S1 foramen (A) in all cases. After Bonferroni correction, the significance level became P = .016 instead of P = .05. The horizontal distance (a) between the dorsal S1 foramen and the line vertically drawn between spinous process and coccyx of L4 and L5 in the male and female group is shown in Table 2. The horizontal distance from the spinous process to the dorsal S1 foramen did not significantly differ between male and female groups (P = .167). After Bonferroni correction, the horizontal distance (b) between the dorsal S1 foramen and PSIS (C) is significantly differ between sex (P = .010) (Table 3). In contrast, the vertical distance (b) of the upper margin of sacrum (D) running parallel to dorsal S1 foramen is significantly differ between sex (P = .004) (Table 4).
Table 2.
The horizontal distance from the spinous process to the dorsal S1 foramen.
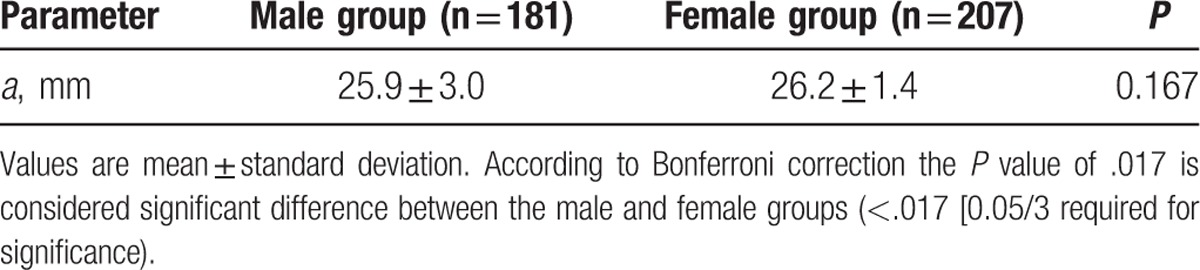
Table 3.
The horizontal distance from the posterior superioriliac spine to the dorsal S1 foramen.
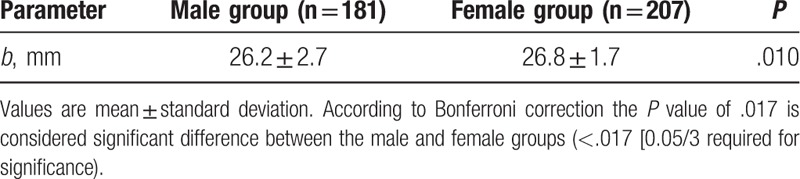
Table 4.
The vertical distance from the upper margin of sacrum to dorsal S1 foramen.
4. Discussion
The dorsal sacral foramen is smaller than the ventral sacral foramen under x-ray fluoroscopy. Thus, it is more difficult to find the dorsal sacral foramen than the ventral sacral foramen. In addition, it can be difficult to confirm the location of the dorsal sacral foramen, such as intestinal gas retention, obesity, or osteoporosis. Therefore, an estimated location of the dorsal sacral foramen is beneficial for S1 nerve root block procedure. There was a rare report of the detailed location of the dorsal sacral foramen. However, the anatomy of sacrum in which the dorsal sacral foramen is located differs between sex, ethnicities, and heights.[6] The dorsal S1 foramen is about the same height of PSIS in upper and lower parts, from 40 to 60% of the predicted area of the midline, and in between the PSIS in medial and lateral parts, and closer to the center in caudal parts.[7] The dorsal S1 foramen is located 1 cm centrally and 1 cm caudally.[7] The present study evaluating the location relationship between the needle entry point of S1 nerve root block and the location of PSIS from physical examination found that the entry point was located 28.7 ± 8.8 mm centrally and 3.5 ± 14.0 mm caudally. These measurements differ between men and women, and are inconsistent between different individuals.[8] Another study reported that the S1 foramen exists in the position 2.5 ± 0.2 cm laterally and 3.5 ± 0.4 cm cranially for men and 3.1 ± 0.5 cm for women from the midpoint of the line connecting both PSISs.[9]
Several studies have provided several methods to find the exact location of the dorsal S1 foramen. However, those studies did not directly locate it using x-ray fluoroscopy. S1 nerve block procedure using x-ray fluoroscopy is inconvenient to measure the distance or the angles of the anatomical structures. This study provides a clear and innovative demonstration of an alternative procedure that involves exposing x-ray fluoroscopy in the line in which L4–5 and L5-S1 facet joints meet, as well as finding the location of dorsal sacral foramen by drawing an imaginary line from the facet joint of L5-S1. The facet joint is a synovial joint formed in which the superior articular process and inferior articular process of vertebral bodies meet; it is also called the zygapophyseal or apophyseal joint.[10] Intervertebral foramen of the spine is an anatomical boundary of upper and lower vertebral body, and the pedicle and articular facet joint of the annulus fibrosus, in which spinal nerves, arteries, and veins traverse.[10] When structures form the intervertebral foramen of the spine, the articular facet joint is connected by the inferior articular process of the upper spine and superior articular process of the lower spine, and the 2 articular processes are connected by the articular capsule. Furthermore, the sacrum is a large triangular bone at the base of the spine, and it is attached by the wedge of 2 hip bones located at the upper dorsal area of the pelvic cavity.[11] The upper part is connected to the lower back bone and the lower part to the coccyx. Children usually have 5 unfused vertebrae, which will fuse between 16 and 18 years of age, and solidify as 1 single bone around the 26 years of age.[12] The sacrum of humans is not positioned posteriorly at birth and it is during the first few years that the sacrum moves dorsally in relation with the progressive attainment of erect posture and the ontogeny of bipedal propulsion.[13] The sacrum, unlike other vertebra, does not show a facet joint after fusion. However, as the intervertebral foramen of the vertebra is a boundary around the articular facet joint, it could be deduced that dorsal S1 foramen is vertically located at the facet joint of the upper lumbar. This was demonstrated in this study.
This study showed that the average vertical distance between the midline of dorsal S1 foramen and vertical line to the upper margin of the sacrum differs between men and women (45.6 ± 6.5 and 43.8 ± 6.0 mm, respectively) with a longer distance in men than in women. This could be the result of a longer sacrum due to the greater height in men. This study results prove that the location of PSIS is not horizontally in the same location of the midpoint in the dorsal S1 foramen, but is in a more caudal and lateral position, with a length of 26.2 ± 2.7 mm for men and 26.8 ± 1.7 mm for women, with the length being greater in women. This reflects the different shape of the pelvis and wider and shorter sacrum of women than men.[5] However, the horizontal distance from the spinous process to the dorsal S1 foramen did not significantly differ between men and women (P = .167). This result implies that the although the difference between the horizontal distance between the dorsal S1 foramen and PSIS, and vertical distance between the midline of the dorsal S1 foramen and vertical line to upper margin sacrum differs between sex, the horizontal distance spinous process to the dorsal S1 foramen value does not vary significantly depending on sex. The study helps to predict the location of dorsal S1 foramen regardless of sex.
This study had some limitations. First, it was conducted retrospectively in a single center, which weakens the generalizability of the results. Further larger prospective studies are required to confirm these results. Second, it is not easy to locate the dorsal S1 foramen in patients with difficult visualization of facet joint, such as elderly patients, patients with surgery history, severe compression fracture of spine, and facet joint hypertrophy. Third, there is the issue of anatomical differences in the S1 foramen according to many demographic, clinical, and genetic factors. All of these variables could have affected our results.
5. Conclusions
The location of dorsal S1 foramen was measured in 388 healthy native South Koreans using fluoroscopic findings from the nerve block procedure performed under x-ray fluoroscopy. For difficult cases of locating dorsal S1 foramen under x-ray fluoroscopy, prediction of the location of the dorsal S1 foramen for S1 nerve block should be aided by the present findings. For imaging the location and nerve path of dorsal S1 foramen, sex and height should be considered. With difficult cases of locating dorsal S1 foramen, the lumbar facet joint can assist in predicting the vertical location of the dorsal S1 foramen, and PSIS would lead to predict the horizontal location of the dorsal S1 foramen.
Acknowledgments
The authors would like to thank all the study participants for their participation in this study.
Footnotes
Abbreviations: AP = anteroposterior, PSIS = posterior superioriliac spine, S1 foramen = the first dorsal sacral foramen, S1 nerve root block = the first sacral nerve root block.
Written informed consent was obtained from the patient for publication of this study and any accompanying images. A copy of the written consent is available for review by the Editor of this journal.
All relevant data will be made available upon publication of the study results.
Y.D.C. and J.K.C. contributed equally to this work.
This work was supported by Inha University Hospital Research Grant.
The authors have no conflicts of interest to disclose.
References
- [1].Macnab I. Negative disc exploration: an analysis of the causes of nerve-root involvement in sixty-eight patients. J Bone Joint Surg Am 1971;53:891–903. [PubMed] [Google Scholar]
- [2].Pfirrmann CW, Oberholzer PA, Zanetti M, et al. Selective nerve root blocks for the treatment of sciatica: evaluation of injection site and effectiveness—a study with patients and cadavers. Radiology 2001;221:704–11. [DOI] [PubMed] [Google Scholar]
- [3].Sato M, Mikawa Y, Matuda A. Ultrasound and electrical nerve stimulation-guided S1 nerve root block. J Anesth 2013;27:775–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Sato M, Simizu S, Kadota R, et al. Ultrasound and nerve stimulation-guided L5 nerve root block. Spine 2009;34:2669–73. [DOI] [PubMed] [Google Scholar]
- [5].Weisz G, Houang M. Classification of the normal variation in the sagittal alignment of the human lumbar spine and pelvis in the standing position. Spine (Phila Pa 1976) 2005;30:1558–9. author reply 1559. [DOI] [PubMed] [Google Scholar]
- [6].Yuan SG, Wen YL, Zhang P, et al. Ligament, nerve, and blood vessel anatomy of the lateral zone of the lumbar intervertebral foramina. Int Orthop 2015;39:2135–41. [DOI] [PubMed] [Google Scholar]
- [7].Philip Ob, Denise Jw. Michael JC, Philip OB, Denise JE. The lower extremity: somatic blockade. Neural Blockade in Clinical Anesthesia and Management of Pain 3rd edPhiladelphia: Lippincott-Raven; 1998. 378. [Google Scholar]
- [8].Kim SH, Yoon KB, Yoon DM, et al. An analysis of location of needle entry point and palpated PSIS in S1 nerve root block. Korean J Pain 2010;23:242–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Hasan ST, Shanahan DA, Pridie AK, et al. Surface localization of sacral foramina for neuromodulation of bladder function. An anatomical study. Eur Urol 1996;29:90–8. [DOI] [PubMed] [Google Scholar]
- [10].Jaumard NV, Welch WC, Winkelstein BA, et al. Spinal facet joint biomechanics and mechanotransduction in normal, injury and degenerative conditions. J Biomech Eng 2011;133:071010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Falco FJ, Manchikanti L, Datta S, et al. An update of the effectiveness of therapeutic lumbar facet joint interventions. Pain Physician 2012;15:E909–53. [PubMed] [Google Scholar]
- [12].Cheng JS, Song JK. Anatomy of the sacrum. Neurosurg Focus 2003;15:E3. [DOI] [PubMed] [Google Scholar]
- [13].Ghasemi A, Haddadi K, Khoshakhlagh M, et al. The relation between sacral angle and vertical angle of sacral curvature and lumbar disc degeneration: a case-control study. Medicine (Baltimore) 2016;95:e2746. [DOI] [PMC free article] [PubMed] [Google Scholar]


