Abstract
Background:
Symptomatic or significant vascular lesions of Takayasu arteritis (TA) need interventions. Although percutaneous transluminal angioplasty with balloon is a less invasive and safe method, stent implantation in TA can be an alternative option. However, superiority between balloon angioplasty and stenting in TA is not conclusive.
Methods:
A meta-analysis comparing balloon angioplasty and stenting outcomes was performed using the MEDLINE and EMBASE databases.
Results:
A total of 7 studies on 266 patients and 316 lesions were included. Balloon angioplasty was performed in 186 lesions and stenting in 130 lesions. There were no significant differences in the incidence of both restenosis and other complications between balloon angioplasty and stenting [odds ratio (OR) = 2.39, 95% confidence interval (CI) = 0.66–8.66, P = .18; OR = 1.80, 95% CI = 0.49–6.65, P = .38, respectively]. In the renal arteries, the risk of restenosis in stenting was significantly higher than that in balloon angioplasty (OR = 4.40, 95% CI = 2.14–9.02, P < .001). The clinical efficacy of improving renal hypertension between balloon angioplasty and stenting at the renal artery lesions was similar (OR = 0.65, 95% CI = 0.28–1.51, P = .31); however, acute vascular complications were significantly fewer in stenting than in balloon angioplasty (OR = 0.07, 95% CI = 0.02–0.29, P < .001).
Conclusion:
This meta-analysis found that balloon angioplasty can yield better results in renal artery interventions than stenting. Nonetheless, it is desirable to avoid vessel dissections during balloon angioplasty, which can eventually require stent implantations.
Keywords: balloon angioplasty, complication, restenosis, stent implantation, Takayasu arteritis
1. Introduction
Takayasu arteritis (TA) is a granulomatous large-vessel vasculitis involving the aorta, subclavian arteries, carotid arteries, and renal arteries.[1] TA commonly begins from the aortic annuls, and the major branches of the aorta are involved. Although some patients show a monophasic and self-limited disease course, others have a progressive arteritis causing vascular obstructions.[2] TA occurs generally at age < 40 years, and a younger onset of TA suggests that the mechanisms of vascular obstruction are different from atherosclerosis. TA actually shows a patchy and transmural fibrous thickening, resulting in multiple vascular obstructions.[3] Although initial vascular interventions are usually successful, the long-term patency of the vessels is poor, and repeat vascular interventions are frequently needed.[4]
Treatment of TA using steroids, immunosuppressants, and biological agents improves the outcomes. Nonetheless, symptomatic or significant vascular lesions need interventions. One of the established methods is percutaneous transluminal angioplasty with balloon.[5] Balloon angioplasty is less invasive, safe, and most widely used. Another option can be a stent implantation. However, the superiority between balloon angioplasty alone and with stenting has been unresolved. There have been several studies reporting on the results of endovascular treatment of TA; however, the results are a matter of debate. Because neither meta-analyses nor large-scale studies are available for balloon angioplasty versus stenting in TA, we conducted a meta-analysis to examine the outcomes of these endovascular treatments. In this study, we described and compared the results of balloon angioplasty and stenting, focusing on the patency of the arteries, clinical effects, and complications.
2. Methods
2.1. Database and search strategy
We searched for studies using MEDLINE and EMBASE databases from January 1980 up to January 2017. The search terms were as follows: “Takayasu arteritis” AND “surgery OR bypass OR graft OR intervention OR endovascular” AND “stent OR ballooning OR angioplasty.” During the search, we did not limit the language to identify as many studies as possible. We also performed a manual search of references in previously published studies and review articles. This meta-analysis collected data from published articles; thus, no ethical approval was necessary.
2.2. Inclusion and exclusion criteria
Eligible studies were selected on the basis of the following criteria: comparison of endovascular balloon angioplasty to stent insertion; patients diagnosed with TA; and sufficient data on the number of patients, lesions, and outcome data. In cases of multiple reports from the same institution, only the most detailed published report was used to avoid duplication of data. Studies were excluded on the basis of the following criteria: overlapping data; studies without reliable data; case reports or review articles; and only abstract available. No restrictions were placed on race, ethnicity, or geographic area.
2.3. Data extraction
The baseline information was extracted, including the first author, year of publication, country of the study population, number of patients in each group, number of lesions in each group, location of involved vascular lesions, and method used (balloon angioplasty or stenting). In cases of duplicated publications from the same study group, the study with the larger sample size was retained. This meta-analysis was conducted on the basis of the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines.[6]
2.4. Statistical analysis
We measured odds ratios (ORs) for dichotomous data and reported 95% confidence intervals (CIs). We performed meta-analyses on restenosis in all artery and renal artery interventions, clinical efficacy of the renal artery intervention, other complications, including progressive renal insufficiency, transient ischemic attack, stroke, congestive heart failure, myocardial infarction, emergency surgery, or death, and acute vascular complications, excluding restenosis in the renal artery intervention. Restenosis and vascular complications were analyzed on the basis of the number of lesions and other complications of the patients.
Heterogeneity between studies was assessed using the Cochran Q test (in which a P < .10 was considered a statistically significant heterogeneity), and the heterogeneity among the studies was tested using the I2 statistic (in which I2 > 50% was considered a statistically significant heterogeneity).[7] If there was no significance in the study heterogeneity, a fixed-effects model was used: otherwise, a random-effects model was used.[8,9] Forest plots were drawn to visualize the overall effect. This meta-analysis was performed using the Review Manager (RevMan) version 5.3 (The Nordic Cochrane Center, The Cochrane Collaboration, 2014).
3. Results
3.1. Study identification and characteristics
The online database queries and manual reference searches identified 369 studies, of which 42 were selected for a full-text review on the basis of the screening of their title and abstract. One study was excluded because it contained overlapping data, 6 because they had only published abstracts, and 19 because they were case reports or review articles. In addition, three were excluded because they lacked the exact number of involved lesions and 6 because they included only data on endovascular interventions not divided into balloon angioplasty and stenting. Finally, 7 studies met the inclusion criteria and were used in the meta-analysis.[10–16] A flow chart detailing the inclusion and exclusion process is shown in Fig. 1. The included studies involved a total of 266 patients and 316 lesions, with 186 lesions treated with balloon angioplasty and 130 lesions treated with stenting. Table 1 summarizes the characteristics of the included studies.
Figure 1.
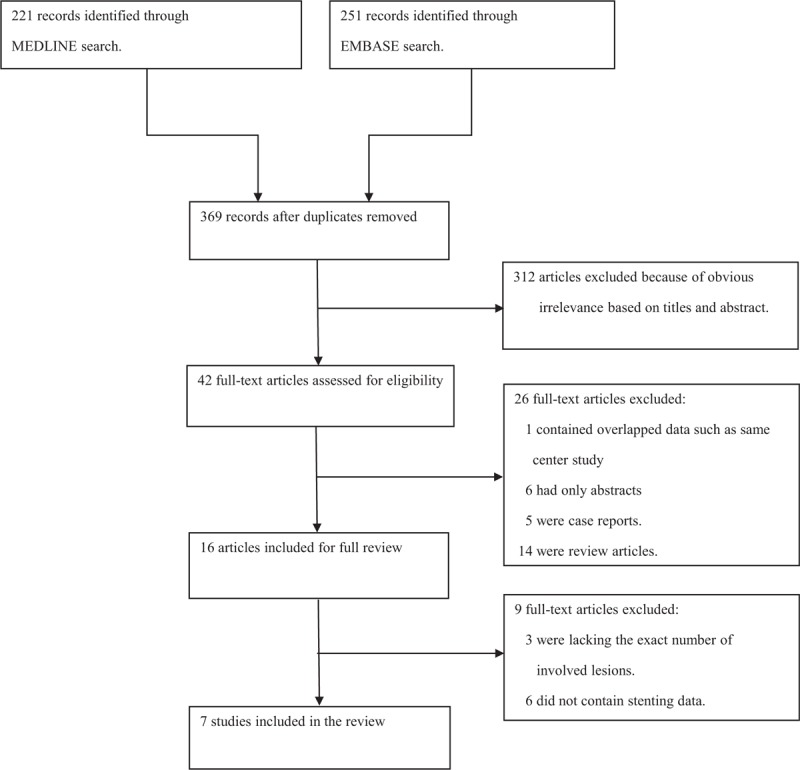
Flow chart of the inclusion/exclusion criteria. A total of 7 studies met the inclusion criteria and are used in the meta-analysis. The included studies involve a total of 266 patients and 316 lesions, with 186 lesions treated with balloon angioplasty and 130 lesions treated with stenting.
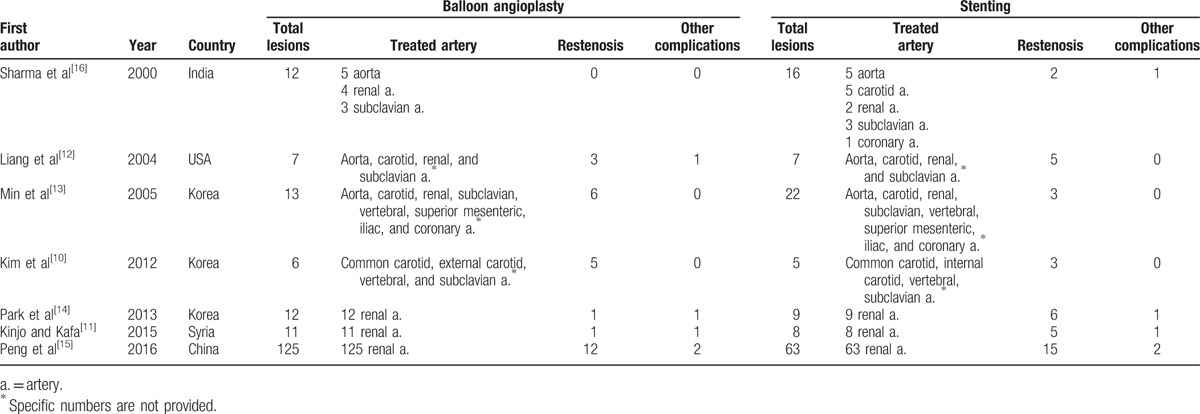
Table 1.
Characteristics of the individual studies included in the systematic review and meta-analysis.
3.2. Comparison between balloon angioplasty and stenting for restenosis in the overall artery interventions and renal artery intervention
We performed a meta-analysis of 186 lesions treated with balloon angioplasty and 130 lesions treated with stenting in 7 studies and found that the incidence of restenosis was not significantly different between balloon angioplasty and stenting in the overall artery interventions (OR = 2.39, 95% CI = 0.66–8.66, P = .18; Fig. 2). We also performed a meta-analysis of the renal artery interventions in 4 studies. This meta-analysis included 152 lesions treated with balloon angioplasty and 82 lesions treated with stenting. Stenting in the renal artery showed a significantly higher incidence of restenosis than balloon angioplasty (OR = 4.40, 95% CI = 2.14–9.02, P < .001; Fig. 3).
Figure 2.
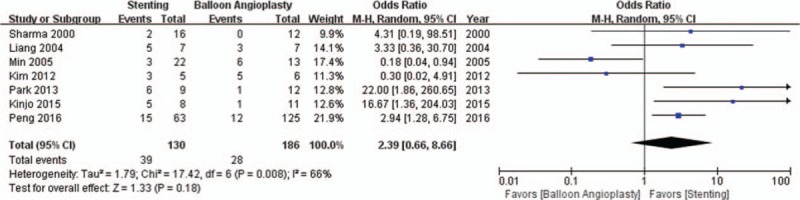
Comparison between balloon angioplasty and stenting for restenosis in the overall artery interventions. A meta-analysis of 186 lesions treated with balloon angioplasty and 130 lesions treated with stenting in 7 studies.
Figure 3.
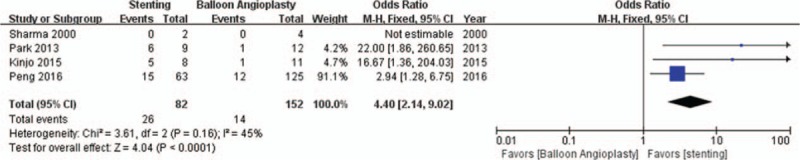
Comparison between balloon angioplasty and stenting for restenosis in the renal artery intervention. A meta-analysis of 152 lesions treated with balloon angioplasty and 82 lesions treated with stenting in 4 studies.
3.3. Comparison between balloon angioplasty and stenting for their clinical efficacy in the renal artery intervention
We performed a meta-analysis of 111 patients treated with balloon angioplasty and 75 patients treated with stenting in 4 studies. The clinical efficacy of improving renal hypertension between balloon angioplasty and stenting was similar (OR = 0.65, 95% CI = 0.28–1.51, P = .31; Fig. 4).
Figure 4.
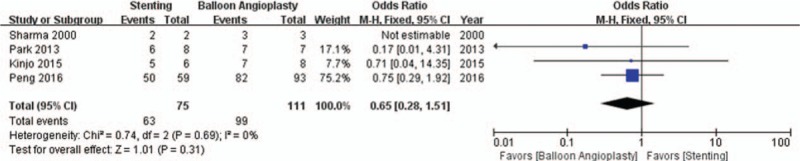
Comparison between balloon angioplasty and stenting for clinical efficacy in the renal artery intervention. A meta-analysis of 111 patients treated with balloon angioplasty and 75 patients treated with stenting in 4 studies.
3.4. Comparison between balloon angioplasty and stenting for other complications in the overall artery interventions and acute vascular complications in the renal artery intervention
A total of 7 studies reported other complications from balloon angioplasty and stenting. However, there were no other complications in either group in 3 studies, and the meta-analysis did not evaluate these. There were no significant differences in the incidence of other complications between balloon angioplasty and stenting in the overall artery interventions (OR = 1.80, 95% CI = 0.49–6.65, P = .38; Fig. 5). Other complications included 6 cases of progressive renal insufficiency, 1 case of transient ischemic attack, 1 case of stroke, and 1 case of congestive heart failure.
Figure 5.
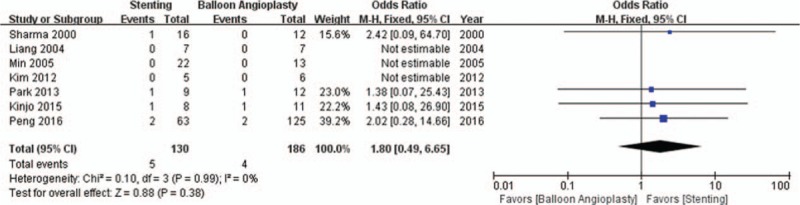
Comparison between balloon angioplasty and stenting for other complications in the overall artery interventions. There are no significant differences in the incidence of other complications between balloon angioplasty and stenting in the overall artery interventions.
Further, we conducted a meta-analysis of acute vascular complications in the renal artery intervention and found significantly fewer complications in stenting than in balloon angioplasty (OR = 0.07, 95% CI = 0.02–0.29, P < .001; Fig. 6). Majority of the acute vascular complications were vessel dissections.
Figure 6.
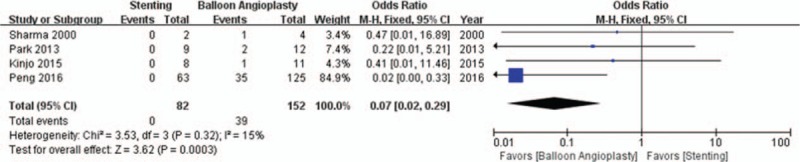
Comparison between balloon angioplasty and stenting for acute vascular complications in the renal artery intervention. A meta-analysis of acute vascular complications in the renal artery intervention and found significantly fewer complications in stenting than in balloon angioplasty.
3.5. Heterogeneity and publication bias
The meta-analysis of restenosis in all the arteries showed a significant heterogeneity and used the random-effects model. However, in the other meta-analyses, the fixed-effects model was used because a significant heterogeneity was not observed. Publication bias was examined using a funnel plot. Funnel plot was not symmetric. We attempted to reduce heterogeneity using a subgroup analysis.
4. Discussion
This study is the first meta-analysis to compare the outcomes of balloon angioplasty and stenting. Although there have been many reports on endovascular interventions and some comparative studies, the numbers of patients included in previous studies were limited, and most reports have only assessed 1 group, rather than comparing balloon angioplasty and stenting. In this meta-analysis including 7 studies, stenting in all the arteries showed equivocal rates of restenosis with balloon angioplasty; however, stenting in the renal arteries presented a significantly higher incidence of restenosis than balloon angioplasty. The efficacy of improving renal hypertension was similar between the 2 interventions, and the rates of other complications without restenosis were also similar.
The principal treatments of symptomatic TA are revascularizations of the affected vessels. In the active stage of TA, preemptive medical therapies with steroids or immunosuppressants before revascularization should be considered, as panarteritis characterized by degeneration of elastic fibers and formation of aneurysms could be improved.[17,18] It was known that pre-treatment with steroids improved inflammations within few weeks. Conversely, revascularization during the active phase could increase the risk of procedure-related complications, including restenosis and dissection.[19] In 6 studies in this meta-analysis, the patients in the active phase or the progression of the symptoms were administered with anti-inflammatory agents, such as steroids, methotrexate, or azathioprine before and/or after the interventions. One study did not clarify how the patients were treated with anti-inflammatory agents.[12] Although the treatment protocols were different among the studies, the interventions in the included studies were performed after active inflammation was controlled. Consequently, we assumed that the restenosis rates were not magnified and that the analyses were performed with fewer biases.
In the chronic phase, the affected vessels can be revascularized via either surgery or endovascular treatment. Bypass surgery had disadvantages, such as graft stenosis, aneurysmal change in the anastomosis site, and morbidity. Hence, percutaneous angioplasty was introduced for the treatment of TA. Balloon angioplasty was considered as a cost-effective, less invasive, and safe method for relieving stenosis.[20] Percutaneous angioplasty yielded excellent results ranging from 81% to 100% and low morbidity and mortality.[21,22] Balloon angioplasty is relatively simple and cost-effective. It avoids the risks of anesthesia and shortens the hospital stay. However, the success rate and outcome of balloon angioplasty varied in accordance with the stenosis degree, lesion length, and target vessel. A flow-limiting dissection and vessel rupture could develop, and a restenosis rate up to ∼80% was also problematic.[23] Thus, the introduction of stent implantation in TA was anticipated to solve these problems. Chronically fibrosed and thick arterial walls of TA could be efficiently dilated with stenting. Deployment of stents attained a better luminal diameter, and the in-stent restenosis rate in the large vessels was low. Some studies reported improved results in stenting; however, stenting was reserved for dissections or persisting stenoses after balloon angioplasty.[12,22,24] In the previous studies, restenosis rate of balloon angioplasty in patients with TA was about 17% to 32% in overall arteries,[13,25] 10% to 15% in subclavian artery,[26] and 21% in renal artery.[27] Restenosis rate of stenting was 12% to 66% in overall arteries,[14,16] and 62.5% in renal artery.[11] Although restenosis rates of stenting and balloon angioplasty were approximately 30% and 15%, respectively, the overall restenosis rate of stenting in TA was not significantly different compared with that of balloon angioplasty in this meta-analysis. As a result, either balloon angioplasty or stenting could be recommended to treat overall stenoses in TA.
Among the involved arteries in TA, renal artery stenosis accounting for up to 60% in TA caused renal failure and renovascular hypertension. However, interventions in the renal artery showed a different result in this study. Although both balloon angioplasty and stenting in the renal artery showed a good efficacy, stenting in the renal artery in TA had a significantly higher incidence of restenosis than balloon angioplasty. With the involvements with reactive fibrosis, intimal thickening, thrombus formation, and neo-vascularization, stent-related exaggeration in neointimal tissue proliferation could be associated.[28] Considering the fact that the diameter of the renal artery was relatively smaller than that of other involved arteries and as the lower minimal lumen diameter was related to the in-stent restenosis, stenting in the renal artery could be related to a higher incidence of restenosis.[29] Proximal, long, and complicated lesions in TA might also contribute to the occurrence of restenosis. Nonetheless, overall patency rate of ballooning angioplasty in TA showed good efficacy in this study, considering that 30% to 40% restenosis rate of coronary balloon angioplasty in patients without TA. Because TA develops at younger age than atherosclerotic diseases, long-term patency rate is more critical in these patient populations. In consideration of the current practice, which deploys stents in cases of dissection or persistent stenosis, avoidance of balloon angioplasty resulting in vessel dissections was desirable in the renal artery. Further investigations on whether to treat persistent stenosis using balloon angioplasty alone or with stenting are needed.
There were some limitations in this meta-analysis. First, the included studies lacked large sample sizes. TA is a disease with a very low prevalence; thus, conducting large-scale and multicenter prospective randomized studies is difficult. Second, the locations of the interventions varied. The outcome may vary depending on the locations of the interventions; however, the small sample sizes were investigated in detail. Third, the follow-up period differed between each study. Fourth, additional comparisons of variables, such as lumen diameter, could not be performed. Finally, publication bias is an important factor in meta-analyses, which we attempted to mitigate by including studies in all languages.
5. Conclusion
TA provokes symptomatic or significant vascular lesions, and interventions are eventually needed. In circumstances in which less invasive treatments are preferred, superiority between balloon angioplasty and stenting has not been conclusive. In this meta-analysis, there was a lower incidence of restenosis in balloon angioplasty than in stenting in the renal artery intervention. Although other complications were similar, it is desirable to avoid vessel dissections during balloon angioplasty, which can eventually require stent implantations. However, as large-scale studies have not yet been conducted, there are limitations in the result interpretation, and further research studies are needed in the future.
Footnotes
Abbreviations: CI = confidence interval, OR = odds ratio, PRISMA = Preferred Reporting Items for Systematic Reviews and Meta-Analyses, TA = Takayasu arteritis.
HSJ and JHJ contributed equally to this work.
No grants or other supports were received for this study.
The authors declare no conflict of interest.
References
- [1].Mason JC. Takayasu arteritis: advances in diagnosis and management. Nat Rev Rheumatol 2010;6:406–15. [DOI] [PubMed] [Google Scholar]
- [2].Phillip R, Luqmani R. Mortality in systemic vasculitis: a systematic review. Clin Exp Rheumatol 2008;26(5 Suppl 51):S94–104. [PubMed] [Google Scholar]
- [3].Johnston SL, Lock RJ, Gompels MM. Takayasu arteritis: a review. J Clin Pathol 2002;55:481–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Perera AH, Youngstein T, Gibbs RG, et al. Optimizing the outcome of vascular intervention for Takayasu arteritis. Br J Surg 2014;101:43–50. [DOI] [PubMed] [Google Scholar]
- [5].Sharma S, Gupta H, Saxena A, et al. Results of renal angioplasty in nonspecific aortoarteritis (Takayasu disease). J Vasc Interv Radiol 1998;9:429–35. [DOI] [PubMed] [Google Scholar]
- [6].Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ 2009;339:b2535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med 2002;21:1539–58. [DOI] [PubMed] [Google Scholar]
- [8].DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials 1986;7:177–88. [DOI] [PubMed] [Google Scholar]
- [9].Egger M, Smith GD, Phillips AN. Meta-analysis: principles and procedures. BMJ 1997;315:1533–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Kim YW, Kim DI, Park YJ, et al. Surgical bypass vs endovascular treatment for patients with supra-aortic arterial occlusive disease due to Takayasu arteritis. J Vasc Surg 2012;55:693–700. [DOI] [PubMed] [Google Scholar]
- [11].Kinjo H, Kafa A. The results of treatment in renal artery stenosis due to Takayasu disease: comparison between surgery, angioplasty, and stenting. A monocentrique retrospective study. G Chir 2015;36:161–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Liang P, Tan-Ong M, Hoffman GS. Takayasu's arteritis: vascular interventions and outcomes. J Rheumatol 2004;31:102–6. [PubMed] [Google Scholar]
- [13].Min PK, Park S, Jung JH, et al. Endovascular therapy combined with immunosuppressive treatment for occlusive arterial disease in patients with Takayasu's arteritis. J Endovasc Ther 2005;12:28–34. [DOI] [PubMed] [Google Scholar]
- [14].Park HS, Do YS, Park KB, et al. Long term results of endovascular treatment in renal arterial stenosis from Takayasu arteritis: angioplasty versus stent placement. Eur J Radiol 2013;82:1913–8. [DOI] [PubMed] [Google Scholar]
- [15].Peng M, Ji W, Jiang X, et al. Selective stent placement versus balloon angioplasty for renovascular hypertension caused by Takayasu arteritis: two-year results. Int J Cardiol 2016;205:117–23. [DOI] [PubMed] [Google Scholar]
- [16].Sharma BK, Jain S, Bali HK, et al. A follow-up study of balloon angioplasty and de-novo stenting in Takayasu arteritis. Int J Cardiol 2000;75(Suppl 1):S147–52. [DOI] [PubMed] [Google Scholar]
- [17].Andrews J, Mason JC. Takayasu's arteritis: recent advances in imaging offer promise. Rheumatology 2007;46:6–15. [DOI] [PubMed] [Google Scholar]
- [18].Hotchi M. Pathological studies on Takayasu arteritis. Heart Vessels Suppl 1992;7:11–7. [DOI] [PubMed] [Google Scholar]
- [19].Keser G, Direskeneli H, Aksu K. Management of Takayasu arteritis: a systematic review. Rheumatology 2014;53:793–801. [DOI] [PubMed] [Google Scholar]
- [20].Fava MP, Foradori GB, Garcia CB, et al. Percutaneous transluminal angioplasty in patients with Takayasu arteritis: five-year experience. J Vasc Interv Radiol 1993;4:649–52. [DOI] [PubMed] [Google Scholar]
- [21].Dev V, Shrivastava S, Rajani M. Percutaneous transluminal balloon angioplasty in Takayasu's aortitis: persistent benefit over two years. Am Heart J 1990;120:222–4. [DOI] [PubMed] [Google Scholar]
- [22].Lee BB, Laredo J, Neville R, et al. Endovascular management of Takayasu arteritis: is it a durable option? Vascular 2009;17:138–46. [DOI] [PubMed] [Google Scholar]
- [23].Qureshi MA, Martin Z, Greenberg RK. Endovascular management of patients with Takayasu arteritis: stents versus stent grafts. Semin Vasc Surg 2011;24:44–52. [DOI] [PubMed] [Google Scholar]
- [24].Isobe M. Takayasu arteritis revisited: current diagnosis and treatment. Int J Cardiol 2013;168:3–10. [DOI] [PubMed] [Google Scholar]
- [25].Park MC, Lee SW, Park YB, et al. Post-interventional immunosuppressive treatment and vascular restenosis in Takayasu's arteritis. Rheumatology 2006;45:600–5. [DOI] [PubMed] [Google Scholar]
- [26].Tyagi S, Verma PK, Gambhir DS, et al. Early and long-term results of subclavian angioplasty in aortoarteritis (Takayasu disease): comparison with atherosclerosis. Cardiovasc Intervent Radiol 1998;21:219–24. [DOI] [PubMed] [Google Scholar]
- [27].Sharma S, Saxena A, Talwar KK, et al. Renal artery stenosis caused by nonspecific arteritis (Takayasu disease): results of treatment with percutaneous transluminal angioplasty. AJR Am J Roentgenol 1992;158:417–22. [DOI] [PubMed] [Google Scholar]
- [28].Vaideeswar P, Deshpande JR. Pathology of Takayasu arteritis: a brief review. Ann Pediatr Cardiol 2013;6:52–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Kastrati A, Schomig A, Elezi S, et al. Predictive factors of restenosis after coronary stent placement. J Am Coll Cardiol 1997;30:1428–36. [DOI] [PubMed] [Google Scholar]


