Abstract
Rationale:
Occlusive cerebrovascular disease is the most common cause of homonymous hemianopia (HH) with macular sparing.
Patient concerns:
A 61-year-old man came to our ophthalmology clinic complaining of right-side hemianopia. Ophthalmic examination, visual field (VF) examination, and brain magnetic resonance imaging (MRI) were performed.
Diagnoses:
He had right HH without macular sparing on the initial VF test. And brain MRI 6 days after the visual symptoms began revealed a left occipital infarction.
Interventions and Outcomes:
Thirty-seven days after the onset, his follow-up 24-2 VF examination showed HH with bilateral macular sparing, which was not apparent in the initial VF examination. About 4 months after the stroke, his central 10-2 VF examination also showed HH with bilateral macular sparing.
Lessons:
We report a case of HH with a dramatic improvement in central vision several days after an occipital infarction. To our knowledge, this is the first case to show macular sparing developing after several days.
Keywords: homonymous hemianopia, macular sparing, stroke
1. Introduction
Occlusive cerebrovascular disease is the most common cause of homonymous hemianopia (HH) with macular sparing.[1] A paper published in 1951 mentioned that the central visual field (VF) can be bisected and the visual field of the macular area spared.[2] We report a case of right HH with macular sparing that was not seen at the initial examination after a left occipital infarction, and became obvious several days later.
2. Material and methods
The patient received a complete ophthalmologic and neurologic examination, including a review of medical and ocular histories, measurement of best-corrected visual acuity, slit-lamp biomicroscopy, visual field examination and magnetic resonance imaging (MRI).
3. Results
A 61-year-old man came to our ophthalmology clinic complaining of right-side hemianopia. He experienced dizziness and a headache immediately after lifting a heavy object 4 days ago. Subsequently, he could not see the right side of his visual field and had a flashing light sensation on the right side. He had right HH on the initial VF test (Fig. 2A). We referred him to the neurology clinic because an occipital lobe infarction was suspected. MRI 6 days after the visual symptoms began revealed only the patchy acute infarction involving the left occipital cortex (Fig. 1). In MRA, there were no suspicious lesions in large intracranial and cervical arteries. A systemic work-up revealed that the occipital infarction was the result of untreated atrial fibrillation. He began medical treatment including antithrombotic therapy for atrial fibrillation. He experienced a subjective symptomatic improvement in the central visual field over time after the onset of symptoms. Thirty-seven days after the onset, his follow-up 24-2 VF examination showed HH with bilateral macular sparing which was not apparent in the initial VF examination of both the eyes (Fig. 2B). About 4 months after the stroke, his central 10-2 VF examination also showed HH with bilateral macular sparing (Fig. 2C).
Figure 2.
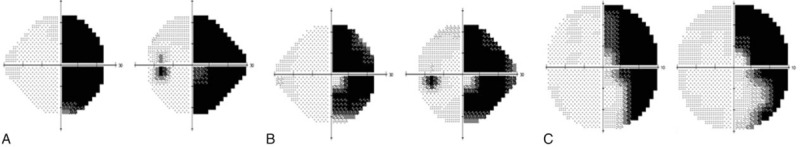
Humphrey visual field examination The Humphrey 24-2 visual field examination showed (A) right homonymous hemianopia on day 4 and (B) right homonymous hemianopia with macular sparing on day 37. C, The Humphrey 10-2 visual field examination 114 days after the occipital infarction showed right homonymous hemianopia with macular sparing.
Figure 1.
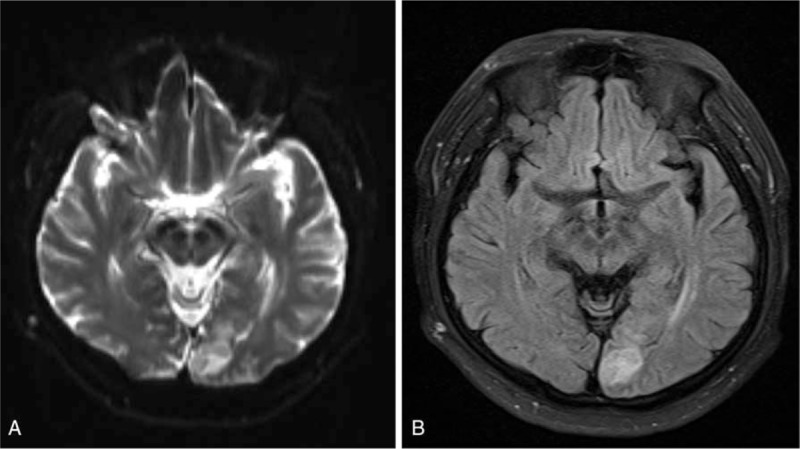
Magnetic resonance imaging brain magnetic resonance imaging performed 6 days after an occipital infarction showed a hyperintense lesion in the left occipital lobe in (A) diffusion-weighted images and (B) fluid-attenuated inversion recovery images.
4. Discussion
Homonymous hemianopia with macular sparing is defined as a homonymous VF defect sparing the central visual field on the affected side. HH with macular sparing has been reported in ischemic stroke patients.[1–4]
However, the mechanism of macular sparing is controversial. One hypothesis is that the visual cortex has a dual blood supply, from the middle (MCA) and posterior (PCA) cerebral arteries or the posterior temporal and calcarine arteries.[3,4] The occlusion of 1 artery might result in macular sparing if another artery still provides blood to the visual cortex that represents macular vision. However, Smith and Richardson[5]reported a variety of patterns by which the 4 branches of the PCA supply the visual cortex. Therefore, another hypothesis, incomplete damage to the visual cortex, might explain this phenomenon.
Our patient noticed improvement in the central VF after seeing flashing light for several days, and his follow-up 24-2 VF examination 37 days after the occipital infarction showed HH with bilateral macular sparing, which was not apparent in the initial 24-2 VF examination. The macular sparing was observed in a subsequent 10-2 VF examination after 114 days. This might result from increased collateral circulation to the PCA territory. We postulate that a PCA infarction caused the temporary HH without macular sparing and resumed blood supply to the tip of occipital lobe led to the improvement in the central VF.
Without knowing the exact mechanism of macular sparing, we report a case of HH with a dramatic improvement in central vision several days after an occipital infarction. This phenomenon might be more common than has been previously thought in HH with macular sparing. As our patient visited the ophthalmology clinic initially, an initial VF examination was performed at an early stage of infarction. If initial VF examinations were performed at an early stage in patients with occipital lobe infarctions, we could determine whether this phenomenon is rare or common. Although we do not understand the mechanism of this phenomenon, to our knowledge, this is the first case to show macular sparing developing after several days.
The patient has consented to the submission of the article to the journal.
Footnotes
Abbreviations: HH = homonymous hemianopia, MCA = middle cerebral arteries, MRA = magnetic resonance angiography, MRI = magnetic resonance imaging, PCA = posterior cerebral arteries, VF = visual field.
The English in this document has been checked by at least 2 professional editors, both native speakers of English. For a certificate, please see: http://www.textcheck.com/certificate/io4mSP.
This study was conducted in accordance with the ethical standards stated in the Declaration of Helsinki and with the approval of the Institutional Review Board of Uijeongbu St. Mary's Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea.
The authors have no conflicts of interest to disclose.
References
- [1].Zhang X, Kedar S, Lynn MJ, et al. Homonymous hemianopias: clinical-anatomic correlations in 904 cases. Neurology 2006;66:906–10. [DOI] [PubMed] [Google Scholar]
- [2].Steiner AA. Homonymous hemianopia, bilateral with macular sparing, of vascular origin. Am J Ophthalmol 1951;34:1170–3. [PubMed] [Google Scholar]
- [3].Dufresne AM, Savard M. A case of bilateral homonymous hemianopsia with macular sparing. Can J Neurol Sci 2011;38:788–90. [DOI] [PubMed] [Google Scholar]
- [4].Leff A. A historical review of the representation of the visual field in primary visual cortex with special reference to the neural mechanisms underlying macular sparing. Brain Lang 2004;88:268–78. [DOI] [PubMed] [Google Scholar]
- [5].Smith CG, Richardson WF. The course and distribution of the arteries supplying the visual (striate) cortex. Am J Ophthalmol 1966;61:1391–6. [DOI] [PubMed] [Google Scholar]


