Abstract
Out-of-hospital cardiac arrest (OHCA) can be used to evaluate the overall performance of the emergency medical services’ (EMS) system. This study assessed the impact of EMS on OHCA survival rates in a setting where the prehospital system is underdeveloped.
A retrospective chart review was carried out over a 5-year period of all adult OHCA patients admitted to the emergency department (ED) of a tertiary care center in Lebanon.
A total of 271 patients with OHCA (179 [66.1%] men, mean age of 69.9 [standard deviation = 15.0 years] were enrolled. The most common OHCA location was residence/home (58.7%). The majority of arrests were witnessed (51.7%) with 6.1% witnessed by EMS; 211 patients (75.6%) were transported to the ED by EMS. Prehospital cardiopulmonary resuscitation (CPR) was done by EMS for 43.2% of the patients, whereas only 4.4% received CPR from a family member/bystander. Prehospital automated external defibrillator use was documented in 1.5% of cases in the prehospital setting. Only 2 patients had return of spontaneous circulation prior to ED arrival. Most patients (96.7%) were resuscitated in the ED. Patients presented to the ED mostly in asystole (79.3%). Forty-three patients (15.9%) survived to hospital admission and 13 (4.8%) were discharged alive with over half of them (53.8%) had a good neurological outcome upon discharge (cerebral performance category 1 or 2).
Survival of EMS-treated OHCA victims in Lebanon is not as expected. Medical oversight of EMS activities is needed to link EMS activities to clinical outcomes and improve survival from cardiac arrest in Lebanon.
Keywords: cardiac arrest, developing country, emergency medical services
1. Introduction
Out-of-hospital cardiac arrest (OHCA) survival rates remain low despite major advances in resuscitation.[1] Around 250,000 Americans die each year from sudden cardiac arrest, and the majority occurs outside of the hospital.[2] Approximately 60% of OHCA are treated by emergency medical services (EMS).[3] The estimated incidence of EMS assessed OHCA is around 10.8 individuals per 100,000 population in the United States.[4] The Utstein guidelines for reporting of survival rates from OHCA allow for comparing outcomes between different communities.[5,6] The reported survival rates for patients with witnessed cardiac arrest with an initial rhythm of ventricular fibrillation vary from 4% to 45%.[5,7] During the past 30 years, and despite major initiatives to reduce mortality from OHCA, the reported survival to hospital discharge in the United States was only 10.4%.[8]
The mortality rate of victims of OHCA increases by 7% to 10% for every minute of delay in receiving basic life support (BLS).[9] The American Heart Association (AHA) “chain of survival” aims at improving outcomes and decreasing mortality through a bundle of measures that can be implemented in any setting.[10] The chain of survival consists of immediate recognition of OHCA symptoms and activation of EMS, early chest compression, rapid defibrillation, effective advanced life support (ALS), and integrated postcardiac arrest care.
OHCA survival to hospital discharge can also be used as a performance measure of the overall EMS system.[11] It allows the evaluation of the different components of the OHCA bundle of care to improve each link in the cardiac arrest “chain of survival.”[10] An effective EMS response can lead to higher survival rates through dispatcher assisted cardiopulmonary resuscitation (CPR) instructions, early and good quality CPR, early defibrillation and transport to appropriate hospitals. Community-level variation remains a significant factor affecting EMS treatment and survival from OHCA with reported survival to hospital discharge ranging from 3.0% to 16.2% of EMS-treated patients from 10 resuscitation outcome consortium communities.[1]
Internationally, additional variation in OHCA management exists depending on the type of existing EMS system. In developed countries, termination of resuscitation (TOR) rules exists. The clinical criteria to predict survival from OHCA include arrest witnessed by a bystander, arrest witnessed by EMS, provision of bystander CPR, shockable cardiac rhythm, and return of spontaneous circulation (ROSC) in the field. Nevertheless, the impact of the type of EMS system on OHCA survival has not been systematically evaluated across populations.
Several AHA chain of survival components are missing in Lebanon like other developing countries. The EMS system in Lebanon is underdeveloped and fragmented. Prehospital EMS are based on volunteer systems with multiple agencies.[11] Rapid transport to hospitals and minimal prehospital medical care are the norms for management of OHCA.[11] Patients are often transported by private cars to local hospitals, which may cause delayed treatment and poor outcomes.
The objective of this study was to describe the impact of EMS on OHCA survival rates in a setting where the prehospital system is underdeveloped by comparing patient survival by mode of transport (private vs EMS) and by evaluating survival by initial rhythm.
2. Methods
2.1. Study setting and design
This retrospective chart review study was conducted in the emergency department (ED) at the American University of Beirut Medical Center (AUBMC), which is the largest and most advanced academic tertiary care center in Lebanon, and a major referral center for Lebanon and the region with more than 50,000 ED patient visits per year.
Lebanon has a largely volunteer EMS system that is fragmented with multiple agencies providing prehospital emergency services. There is absence of national EMS plan or lead governmental EMS authority, with absence of an EMS law or regulations for operating EMS agencies.[11] There is no national curriculum or scope of practice for prehospital providers. All agencies operate at the BLS with variable training provided within the different agencies. The prehospital care that is provided usually consists of first aid intervention and rapid transport. CPR is not uniformly provided for cardiac arrest patients and automated external defibrillators (AEDs) are not present in all ambulances. There are also no official public access defibrillators programs for community use.[11]
The charts of all adult patients (age 18 years and older) who were treated in the ED at AUBMC for OHCA during the period between July 1, 2009 and December 31, 2013 were reviewed.
The Institutional Review Board (IRB) of the American University of Beirut approved this study.
2.2. Inclusion/exclusion criteria
Victims of OHCA were identified using the ED database (n = 333). The database search was done by chief complaint and ED admission diagnosis for the following terms: “cardiac,” “arrest,” “unconsciousness,” “unresponsive,” “dead,” “death,” “collapse,” “seizure,” and “loss of consciousness.”
All eligible patients who were found to have absent signs of circulation in the prehospital setting or on arrival to ED were included in the study. Patients with presumed noncardiac etiology of arrest including drug overdose, suicide, drowning, hypoxia, exsanguination, cerebrovascular accident, subarachnoid hemorrhage, and trauma were excluded (n = 58).
Patients were also excluded if they met one of the following exclusion criteria: age <18 years, patient transferred from other hospitals for further management of cardiac arrest (n = 4), patients who were immediately pronounced dead on scene and for whom resuscitation was not attempted, including those with decapitation, rigor mortis, and dependent lividity. Patients with missing charts were also excluded. Two reviewers independently reviewed the final list and complete agreement was reached over the included and excluded results.
2.3. Data collection
The data collection was carried out by 2 research assistants who were trained on data abstraction. The prehospital, the ED, and the hospital data elements were collected from the electronic health records of corresponding patients. Prehospital data were collected from the description of arrest in the ED chart.
The Utstein guidelines templates were used for data collection and analysis.[4,12] The 2 main outcomes reported were survival to hospital discharge and neurologic outcome in the form of cerebral performance category (CPC) score. The CPC score was determined from the last inpatient neurologic examination documented prior to patient discharge. Scores of 1 (good recovery) and 2 (minimal disability) indicate good outcome. On the other hand, scores of 3 (severe disability, dependent on others), 4 (persistent vegetative state), and 5 (death) indicate a poor neurologic outcome.[13,14]
2.4. Statistical analysis
The Statistical Package for Social Sciences (IBM Corp. Released 2011. IBM SPSS Statistics for Windows, Version 20.0. Armonk, NY), was used for data entry, management, and analyses. Descriptive analyses were carried out by calculating the number and percent for categorical variables, whereas the mean and standard deviation (SD) were calculated for continuous variables. Bivariate analysis was conducted to compare outcomes by mode of arrival (EMS vs Private) and by ED presenting rhythm. This was followed by a multivariate analysis to adjust for variables which were found to be statistically significant at the bivariate level in addition to the following confounding variables: ED presenting rhythm (shockable vs unshockable or asystole), location of arrest (ref: home/residence), whether the arrest was witnessed (witnessed vs unwitnessed), ED shock (yes vs no) in addition to the duration of prehospital time interval from collapse to ED arrival. Differences were considered significant for a P < .05.
2.5. Ethical review
The study was approved by the IRB of the American University of Beirut.
3. Results
A total of 271 patients with OHCA were enrolled during the study period between July 1, 2009 and December 31, 2013. These consisted of 179 (66.1%) male patients and 92 (33.9%) female patients, with a mean age of 69.93 (SD = 15.03). The most common location of the arrest was residence/home (58.7%). The majority of arrests were witnessed (51.7%) with 6.1% witnessed by EMS. Two hundred eleven patients (75.6%) were transported to the ED by EMS and the rest by private mode of transport. Prehospital CPR was documented in 48% (131/271) of the victims. Prehospital CPR was done by EMS for 43.2% (117/271) of the patients, whereas only 4.4% (12/271) received CPR from a family member or a bystander. Prehospital AED use was documented in 1.5% (4/271) of the cases in the prehospital setting by EMS providers with shocks delivered. Only 2 patients (0.7%) had ROSC prior to arrival to the ED. Most patients (96.7%) were resuscitated in the ED. Patients presented to the ED mostly in asystole (79.3%). Forty-three patients (15.9%) survived to hospital admission and 13 (4.8%) were discharged alive with a mean Glasgow Coma Score of 11 (SD = 5). Over half of them (7 out of 13, 53.8%) had a good neurological outcome upon discharge (CPC 1 or 2).
3.1. OHCA outcome stratified by mode of arrival to the ED
A significantly higher percentage of patients who presented by private transport survived to hospital admission as compared to those transferred by EMS (33.3% vs 10.9%, respectively) (P < .0001) and to hospital discharge (11.7% vs 2.8%, respectively) (P = .01) (Table 1).
Table 1.
Association between all the variables and the prearrival mode.
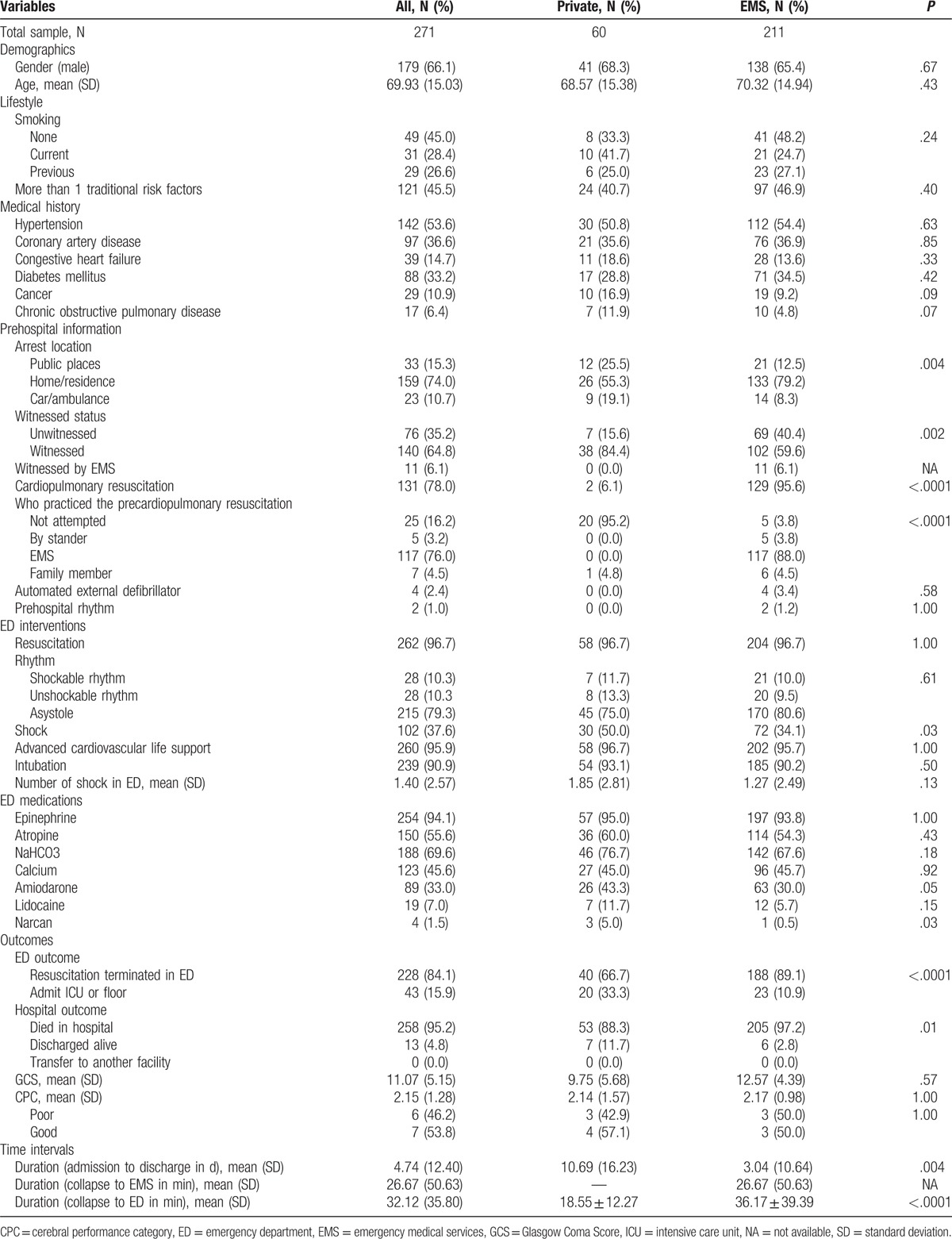
Patients arriving by means of private transport had a significantly higher rate of witnessed arrests (84.4% vs 59.6%) (P = .002), and a significantly higher arrest occurrence during transport (19.1% vs 8.3%) (P = .004), as compared to those transferred by EMS. The private group had, however, lower documented prehospital CPR rate as compared to the EMS transport group (6.1% vs 95.6%) (P < .0001).
The presenting rhythm on arrival to ED was similar for both groups (private vs EMS) (P = .61), with the majority of patients presenting in asystole.
Duration from collapse to ED arrival (in minutes) was almost double for the EMS group (36.17, SD = 39.39 min) as compared to the private transport group (18.55, SD = 12.27 min) (P < .0001).
3.2. OHCA outcome stratified by presenting rhythm to ED
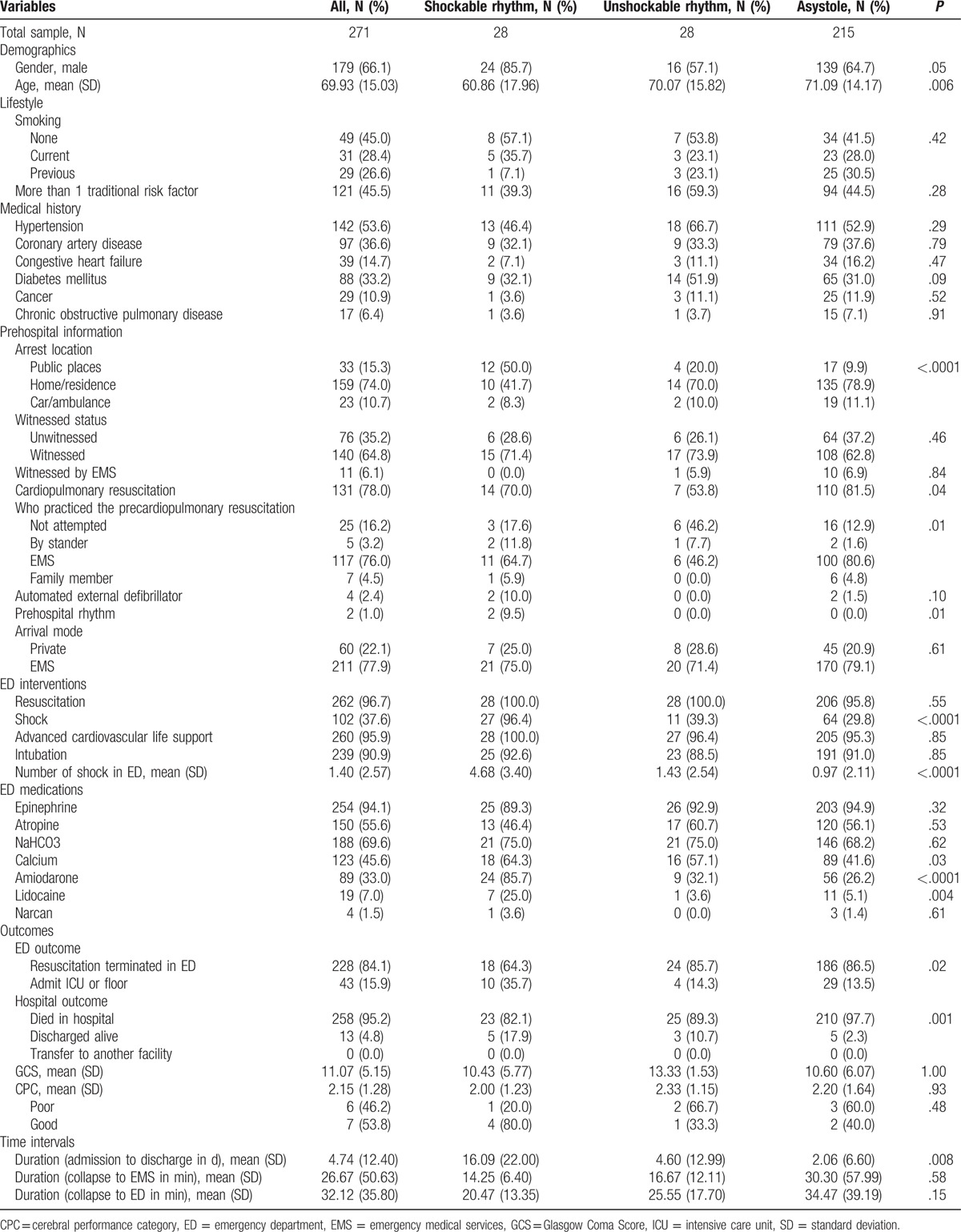
The majority of patients presented to ED in asystole (79.3%). Survival to hospital discharge varied significantly by rhythm with highest survival for shockable rhythm (17.9%) followed by nonshockable rhythm (10.7%) and by asystole (2.3%) (P = .001). The neurologic outcome of survivors was comparable among the 3 groups. Although there was a trend toward increased prehospital time interval (collapse to ED arrival) from shockable to nonshockable to asystole, this increase was not statistically significant (Table 2).
Table 2.
Association between all the variables and the rhythm at ED.
3.3. Mode of arrival and ED and hospital outcomes
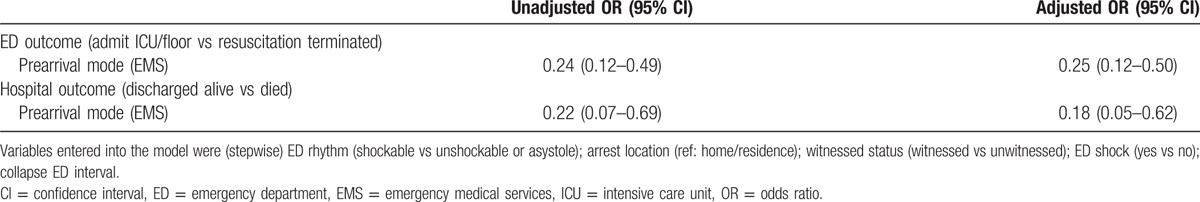
After adjusting for significant and confounding variables using multivariate regression analysis the survival to hospital admission (odds ratio [OR] = 0.25, 95% confidence interval [CI]: 0.12–0.50) and to hospital discharge (OR = 0.18, 95% CI: 0.05–0.62) remained significantly lower in the EMS group compared with the private transport group (Table 3).
Table 3.
Multivariate regression analysis for the association between prearrival mode and the outcomes (ED and hospital).
4. Discussion
This study examined OHCA survival in a setting with limited prehospital emergency resources. Cardiac arrest is a tracer condition that can reflect how the overall system is performing. This study shows that OHCA survival rates are negatively affected when EMS is used in this setting. Patients transported by EMS had lower survival to hospital discharge than those transported by private car (OR = 0.18, 95% CI: 0.05–0.62). However, this is not equivalent to saying that EMS has no benefit but rather highlights that the EMS system the way it is operating is not linked to what EMS is all about which is patient care and delivering good clinical outcomes. The lack of AED use by the EMS might have contributed to the lower survival rate.
Survival from OHCA is multifactorial and is dependent on essential elements across the different phases of care from the prehospital to ED to in-hospital phase. A previously proposed evidence-based measure for OHCA for EMS systems consists of a response interval <5 min for basic CPR and AEDs.[15] This measure, if implemented correctly, is linked to an NNT of 8 with 1 death avoided.[15] There are several ways; this can be achieved using a combination of the following community elements and EMS elements; immediate initiation of CPR by bystanders, dispatcher-assisted CPR instructions, community CPR training programs, availability of public access defibrillators, response intervals for BLS initiation, and AEDs use and quality assurance protocols for first responders.[16,17]
The absence of almost all of these elements in our setting, with the exception of community CPR programs, contributes to the poor survival rate to hospital discharge in OHCA victims (4.8%).
Essential community elements such as recognition and activation of emergency response, immediate high-quality CPR, and rapid defibrillation are deficient. Only 1.5% of patients had AED use in the prehospital setting. Prehospital CPR, mainly by EMS, was documented in only 47.6% of patients. Despite activation of the EMS response, the mean time interval from collapse to EMS arrival was 26.67 min (SD = 50.63), which is approximately 5 times the recommended time.
ALS care delay is another factor contributing to poor outcomes. Only basic level of care is provided in the prehospital field in Lebanon with ALS care usually starting in the ED. Patients transported by EMS had much longer collapse to ED arrival interval when compared to those in the private group (36.17, SD = 39.39 min vs 18.55, SD = 12.27 min). This may have resulted in lower incidence of shockable rhythm with only 10.3% of patients having a shockable rhythm in the ED. This contrasts with the higher incidence of ventricular fibrillation in other prehospital studies.[18] A previous study showed that almost 85% of individuals with ambulatory, out-of-hospital, primary cardiac arrest experience ventricular tachy-arrhythmias during the early minutes after collapse.[19]
Poor survival rates might also be related to futile transports in our system. OHCA victims are usually treated by EMS in more developed countries.[3] TOR rules in the prehospital field exist for providers to reduce unnecessary transports. One example is the “BLS termination of resuscitation rule.” The following 3 criteria must be present to consider terminating BLS resuscitative attempts for adult victims of OHCA: arrest was not witnessed by EMS provider or first responder; no ROSC after 3 full rounds of CPR and AED analysis; and no AED shocks were delivered.[20] This rule can reduce the rate of transport of cardiac arrests without affecting outcomes[21] and can also reduce the costs of care and improve resources availability.[22–24] It can also reduce hazard risk to EMS personnel who are engaged in performing interventions in a moving vehicle or conducting resuscitative efforts[25] while preventing risks associated with emergency lights and sirens transport.[26] For more advanced EMS systems that provide ALS care for OHCA victims in the field, the following criteria constitute a reasonable rule for stopping further resuscitation attempts: asystole for more than 20 min in the absence of a reversible cause and with ongoing ALS without ROSC.[27]
Such termination rules, however, require robust quality management programs and would not be possible in the absence of full compliance with standards of care related to OHCA management mainly CPR and defibrillation.
4.1. Limitations
The results of our study have to be evaluated in light of its limitations. The first limitation is linked to the retrospective nature of the study with prehospital data collected from the ED records of the patients. Another limitation is related to data collection from only 1 urban medical center in Beirut. AUBMC is, however, the largest tertiary care center in Beirut and the patients it serves are representative of the population in Beirut. The impact of the in-hospital phase of treatment on OHCA outcomes, mainly survival, was not assessed by our study since treatment received in the prehospital phase was considered to be the most important predictor for OHCA outcomes. This study, however, uses standardized outcomes of patients with a specific EMS priority condition (OHCA) to describe the EMS system's performance and can serve as a model study of focusing on tracer conditions to highlight potential areas for improvement of prehospital care in a developing country and to improve patients’ outcomes. Our study findings echo those of other studies in resource-limited settings.[28] Cardiac arrest research should be used to improve the EMS system. The findings of this study were used to drive system changes in Beirut. This started with the launch of a pilot registry for OHCA in Beirut in 2014 out of the AUBMC collecting standardized data elements using the Utstein guidelines. The registry currently collects information from a single center and is planned to involve different EMS agencies and other hospitals. Additional initiatives consisted of engaging stakeholders (EMS and policy makers) to work on a national EMS office and a national EMS response plan with the focus on EMS priority conditions including but not limited to OHCA. This plan will involve providing dispatch assisted instructions for callers, ensuring reliability in EMS response, revamping EMS treatment protocols, implementation of public access defibrillation programs, and increasing community awareness for more involvement in bystander CPR and AED use.
5. Conclusion
OHCA can be used to evaluate the overall performance of an EMS system. Survival of OHCA victims in Lebanon seems to be negatively affected by EMS. Several areas of improvement in the emergency response to OHCA victims were identified. Medical oversight of EMS activities is needed to link EMS activities to clinical outcomes and improve survival from cardiac arrest in Lebanon.
Acknowledgments
The authors would like to acknowledge the University Research Board at the American University of Beirut, which helped provide support for conducting this study and for providing the resources to establish the Lebanese Cardiac Arrest Registry.
Footnotes
Abbreviations: AEDs = automated external defibrillators, ALS = advanced life support, AHA = American Heart Association, AUBMC = American University of Beirut Medical Center, CI = confidence interval, CPC = cerebral performance category, ED = emergency department, EMS = emergency medical services, IRB = institutional review board, NNT = number needed to treat, OHCA = out-of-hospital cardiac arrest, OR = odds ratio, ROSC = return of spontaneous circulation, SD = standard deviation, TOR = termination of resuscitation.
MMR and HT have contributed equally to this work.
The authors have no funding and conflicts of interest to disclose.
References
- [1].Nichols G, Thomas E, Callaway CW. Resuscitation outcomes consortium investigators regional variation in out-of-hospital cardiac arrest incidence and outcome. JAMA 2008;300:1423–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].American Heart Association. 2002 Heart and Stroke Statistical Update. Dallas, TX: American Heart Association; 2002. [Google Scholar]
- [3].Rosamond W, Flegal K, Furie K, et al. Heart disease and stroke statistics-2008 update: a report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation 2008;117:e25–146. [DOI] [PubMed] [Google Scholar]
- [4].Mozaffarian D, Benjamin EJ, et al. Writing Group Members. Heart disease and stroke statistics-2016 update: a report from the American Heart Association. Circulation 2016;133:e38–60. [DOI] [PubMed] [Google Scholar]
- [5].Cummins RO, Chamberlain DA, Abramson NS, et al. Recommended guidelines for uniform reporting of data from out-of-hospital cardiac arrest: the Utstein style. Circulation 1991;84:960–75. [DOI] [PubMed] [Google Scholar]
- [6].Perkins GD, Jacobs IG, Nadkarni VM, et al. Cardiac arrest and cardiopulmonary resuscitation outcome reports: update of the Utstein Resuscitation Registry Templates for Out-of-Hospital Cardiac Arrest: a statement for healthcare professionals from a task force of the International Liaison Committee on Resuscitation (American Heart Association, European Resuscitation Council, Australian and New Zealand Council on Resuscitation, Heart and Stroke Foundation of Canada, InterAmerican Heart Foundation, Resuscitation Council of Southern Africa, Resuscitation Council of Asia); and the American Heart Association Emergency Cardiovascular Care Committee and the Council on Cardiopulmonary, Critical Care, Perioperative and Resuscitation. Circulation 2015;132:1286–300. [DOI] [PubMed] [Google Scholar]
- [7].Kellermann AL, Hackman BB, Somes G, et al. Impact of first responder defibrillation in an urban emergency medical services system. JAMA 1993;270:1708–13. [DOI] [PubMed] [Google Scholar]
- [8].Go AS, Mozaffarian D, Roger VL, et al. Heart disease and stroke statistics-2014 update: a report from the American Heart Association. Circulation 2014;129:e28–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Brooks SC, Anderson ML, Bruder E, et al. Part 6: alternative techniques and ancillary devices for cardiopulmonary resuscitation. 2015 American Heart Association Guidelines update for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation 2015;132:S436–43. [DOI] [PubMed] [Google Scholar]
- [10].Cummins RO, Ornato JP, Thies WH, et al. Improving survival from sudden cardiac arrest: the “chain of survival” concept. A statement for health professionals from the Advanced Cardiac Life Support Subcommittee and the Emergency Cardiac Care Committee, American Heart Association. Circulation 1991;83:1832–47. [DOI] [PubMed] [Google Scholar]
- [11].El Sayed M, Bayram JD. Prehospital emergency medical services in Lebanon: overview and prospects. Prehosp Disaster Med 2013;28:163–5. [DOI] [PubMed] [Google Scholar]
- [12].European Resuscitation Council, American Heart Association, Heart and Strike Foundation of Canada, and Australian Resuscitation Council. Recommended guidelines for uniform reporting of data from out-of-hospital cardiac arrest (new abridged version). The “Utstein Style”. Br Heart J 1992;67:325–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Jennett B, Bond M. Assessment of outcome after severe brain damage. Lancet 1975;1:480–4. [DOI] [PubMed] [Google Scholar]
- [14].Rittenberger JC, Raina K, Holm MB, et al. Association between cerebral performance category, modified Rankin scale, and discharge disposition after cardiac arrest. Resuscitation 2011;82:1036–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Myers JB, Slovis CM, Eckstein M, et al. Evidence-based performance measures for emergency medical services systems: a model for expanded EMS benchmarking. Prehosp Emerg Care 2008;12:141–51. [DOI] [PubMed] [Google Scholar]
- [16].Eisenberg MS, Horwood BT, Cummins RO, et al. Cardiac arrest and resuscitation: a tale of 29 cities. Ann Emerg Med 1990;19:179–86. [DOI] [PubMed] [Google Scholar]
- [17].Nichol G, Stiell IG, Laupacis A, et al. A cumulative meta-analysis of the effectiveness of defibrillator capable emergency medical services for victims of out-of-hospital cardiac arrest. Ann Emerg Med 1999;34:517–25. [PubMed] [Google Scholar]
- [18].Herlitz J, Ekström L, Wennerblom B, et al. Predictors of early and late survival after out-of-hospital cardiac arrest in which asystole was the first recorded arrhythmia on scene. Resuscitation 1994;28:27–36. [DOI] [PubMed] [Google Scholar]
- [19].Bayes de Luna A, Coumel P, Leclercq JF. Ambulatory sudden cardiac death: mechanisms of production of fatal arrhythmia on the basis of data from 157 cases. Am Heart J 1989;117:151–9. [DOI] [PubMed] [Google Scholar]
- [20].Morrison LJ, Kierzek G, Diekema DS, et al. Part 3: ethics 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation 2010;122(18 Suppl 3):S665–75. [DOI] [PubMed] [Google Scholar]
- [21].Morrison LJ, Visentin LM, Kiss A, et al. Validation of a rule for termination of resuscitation in out-of-hospital cardiac arrest. N Engl J Med 2006;355:478–87. [DOI] [PubMed] [Google Scholar]
- [22].Gray WA, Capone RJ, Most AS. Unsuccessful emergency medical resuscitation are continued efforts in the emergency department justified? N Engl J Med 1991;325:1393–8. [DOI] [PubMed] [Google Scholar]
- [23].Suchard JR, Fenton FR, Powers RD. Medicare expenditures on unsuccessful out-of-hospital resuscitations. J Emerg Med 1999;17:801–5. [DOI] [PubMed] [Google Scholar]
- [24].Cheung MC, Morrison LJ, Verbeek PR. Prehospital vs. emergency department pronouncement of death: a cost analysis. Can J Emerg Med 2001;3:19–25. [DOI] [PubMed] [Google Scholar]
- [25].Kelen GD, DiGiovanna T, Bisson L, et al. Human immunodeficiency virus infection in emergency patients: epidemiology, clinical presentations, and risk to health care workers: the Johns Hopkins experience. JAMA 1989;262:516–22. [DOI] [PubMed] [Google Scholar]
- [26].Clawson JJ, Martin RL, Cady GA, et al. The wake-effect emergency vehicle related collisions. Prehosp Disast Med 1997;12:274–7. [PubMed] [Google Scholar]
- [27].Soar J, Nolan JP, Böttiger BW, et al. European Resuscitation Council Guidelines for resuscitation 2015: section 3. Adult advanced life support. Resuscitation 2015;95:100–47. [DOI] [PubMed] [Google Scholar]
- [28].Mawani M, Kadir MM, Azam I, et al. Epidemiology and outcomes of out-of-hospital cardiac arrest in a developing country—a multicenter cohort study. BMC Emerg Med 2016;16:28. [DOI] [PMC free article] [PubMed] [Google Scholar]


