Abstract
OBJECTIVE
In this study, we aimed to explore the mechanism by which TCF7L2 rs7903146 risk allele confers susceptibility to impaired glucose tolerance (IGT) or type 2 diabetes (T2D) in obese adolescents.
RESEARCH DESIGN AND METHODS
The rs7903146 variant in the TCF7L2 gene was genotyped in a multiethnic cohort of 955 youths. All subjects underwent an oral glucose tolerance test with the use of the Oral Minimal Model to assess insulin secretion, and 33 subjects underwent a hyperinsulinemic-euglycemic clamp. In 307 subjects, a follow-up oral glucose tolerance test was repeated after 3.11 ± 2.36 years.
RESULTS
The TCF7L2 rs7903146 risk allele was associated with higher 2-h glucose levels in Caucasians (P = 0.006) and African Americans (P = 0.009), and a trend was seen also in Hispanics (P = 0.072). Also, the T allele was associated with decreased β-cell responsivity and IGT (P < 0.05). Suppression of endogenous hepatic glucose production was lower in subjects with the risk variant (P = 0.006). Finally, the odds of showing IGT/T2D at follow-up were higher in subjects carrying the minor allele (odds ratio 2.224; 95% CI 1.370–3.612; P = 0.0012).
CONCLUSIONS
The rs7903146 variant in the TCF7L2 gene increases the risk of IGT/T2D in obese adolescents by impairing β-cell function, and hepatic insulin sensitivity predicts the development of IGT/T2D over time.
Introduction
The landscape of childhood diabetes is changing, as an unprecedented phenomenon of type 2 diabetes (T2D) rarely seen in pediatrics before is unfolding. Looking ahead, projected incidence rates of T2D in youth are expected to triple over the next 40 years in the U.S. (1,2). Even more concerning is the ever-increasing number of those with impaired glucose tolerance (IGT) among obese adolescents (3,4). Youth-onset T2D heralds many years of disease with an increased risk of both micro- and macrovascular complications that will occur when affected individuals are still young (5–8). Therefore, it is imperative to identify adolescents at increased risk for T2D when they are in the prediabetic state, particularly because the tempo of progression from IGT to full-blown diabetes seems to be faster in youth than in adults (9,10).
β-Cell dysfunction and hepatic insulin resistance are key defects contributing to the development of T2D. Therefore, understanding the mechanisms associated with the decline of β-cell function and changes in hepatic insulin sensitivity (SI) is essential in combating the disease, particularly at a younger age. There is substantial evidence in adults for a relevant genetic determination of β-cell failure (11–17). Indeed, the discovery in 2006 by Grant et al. (18) that a common single nucleotide polymorphism (SNP) in the TCF7L2 gene region was associated with T2D in an Icelandic case-control study has launched a new direction in diabetes research. Soon after, these results were replicated in other ethnic groups (19,20), with few cross-sectional studies in children (21,22). Notably, the T risk allele of the rs7903146 confers the strongest risk of T2D known to date in Caucasians (16,17,23). However, the molecular mechanisms by which variants in TCF7L2 increase the risk of T2D remain unclear. TCF7L2 encodes a transcription factor that is a member of the Wnt signaling pathway known to be active not only in the β-cells but also in other cell lineages and glucose-metabolizing tissues, including the liver (24–27). Studies in adults showed that the variant impairs β-cell function and had elevated rates of hepatic glucose production (HGP) (23,28,29). It should be noted, however, that most of the evidence linking TCF7L2 variants to diabetes-related phenotypes in humans has been obtained in adults (23,29,30). There are no studies in adolescents that have yet combined detailed genetic/metabolic studies to help define the mechanisms by which genetic variations in TCF7L2 may increase the risk of IGT/T2D. The pathogenesis of β-cell failure and its genetic underpinnings in youth remain elusive. Results from metabolic studies performed in adults cannot be extrapolated to pediatrics, as they are influenced greatly by the aging effects per se on both insulin secretion and sensitivity. Further, the advantage of studying pediatric subjects is that they lack the potential confounding effects of long-term obesity-associated chronic complications. There is thus a compelling rationale to conduct studies focused on these unique age groups to understand disease etiology to better tailor prevention and treatment approaches to these groups. In this study, in a large multiethnic cohort of obese adolescents, we tested the hypothesis that the risk allele at rs7903146 locus favors the maintenance of IGT or its progression to T2D in youth because of 1) reduced β-cell function; 2) altered efficiency of proinsulin processing; and 3) increased hepatic insulin resistance during adolescence, a sensitive/critical time for youth-onset T2D.
Research Design and Methods
Study Cohort
We recruited 955 obese children and adolescents (394 boys and 561 girls; mean ± SD age 13.3 ± 3.4 years; and mean ± SD z score BMI 2.15 ± 0.70) from a multiethnic cohort participating in the Yale Pathogenesis of Youth Onset Type 2 Diabetes (PYOD) study (NCT01967849), a long-term project aimed at studying early alterations in β-cell function and SI in obese youths. The subjects were not taking any medications that affect glucose metabolism when enrolled. All of them underwent a 3-h oral glucose tolerance test (OGTT), and 705 (74%) subjects showed normal glucose tolerance (NGT) and 250 (26%) IGT.
To evaluate the effect of the genotype on the risk of developing IGT, or progressing to T2D over time, 307 subjects underwent a second OGTT after a follow-up of 3.11 ± 2.36 years. During the follow-up, all participants received standard nutritional guidance and recommendations for physical activity and were not on any medications affecting glucose metabolism. The longitudinal cohort was constituted of 114 Caucasians, 90 African Americans, and 103 Hispanics (113 boys and 194 girls; mean ± SD age 12.4 ± 3.0 years; and mean ± SD z score BMI 2.28 ± 0.55). Of them, at baseline, 202 (66%) were NGT and 105 (34%) IGT. The time interval for the follow-up was based on our previous study suggesting that changes in categories of glucose tolerance in obese adolescents are likely to occur over a relatively short period of time (10,31).
OGTT
A 3-h OGTT (1.75 g/kg body weight, up to 75 g) was performed in all 955 patients, as previously reported (4,10,32). Two baseline samples were obtained at −15 and 0 min for measurements of plasma glucose, insulin, and C-peptide. Subjects were studied at the Hospital Research Unit of the Yale New Haven Hospital at 8 a.m. after a 12-h overnight fast. Thereafter, flavored glucose (Orangedex; Custom Laboratories, Baltimore, MD) was given orally, and blood samples were obtained at 10, 20, and 30 min and every 30 min thereafter for 180 min for the measurements of plasma glucose, insulin, and C-peptide. Proinsulin was available in 82 subjects with NGT and 38 with IGT. Glucose tolerance status was defined according to the American Diabetes Association guidelines.
Assessment of Insulin Secretion and Action: Oral Minimal Model Method
Out of the 955 patients, the data usable to perform the oral minimal model analysis were available for 664 subjects (290 Caucasians, 176 African Americans, and 198 Hispanics). The SI was estimated from plasma glucose and insulin concentrations measured during the 3-h OGTT using the Oral Glucose Minimal Model (31,33–36). β-Cell responsivity was estimated from the C-peptide data measured during the 3-h OGTT using the Oral C-peptide Minimal Model (31,33–36). The model assumes that insulin secretion is made up of two components. The dynamic component is likely to represent secretion of promptly releasable insulin and is proportional to the rate of increase of glucose concentration through a parameter, Φd (10−9), which defines the dynamic responsivity index. The static component derives from provision of new insulin to the releasable pool and is characterized by a static index, Φs (10−9 min−1), and by a delay time constant, T (min). From Φd and Φs, one can also calculate a single, overall β-cell responsivity index, Φtotal (10−9 min−1). Finally, a basal β-cell responsivity index, Φb (10−9 min−1) can also be calculated from basal C-peptide and glucose concentrations. To determine whether β-cell function is appropriate for the degree of insulin resistance, Φtotal can be expressed in relation to SI through the total disposition index (DI) = Φtotal · SI.
Direct Measurement of Hepatic and Peripheral SI
The hyperinsulinemic-euglycemic clamp was performed in a subgroup of 33 subjects (20 male and 13 female; 9 CC, 19 CT, and 5 TT genotypes; mean ± SD age 15.02 ± 2.77 years; and mean ± SD BMI z score 2.19 ± 0.54). Twenty were NGT, and 13 were IGT. This subgroup did not differ from the main cohort for age, sex, race, BMI z score, glucose tolerance, hepatic fat fraction, and body fat.
Two intravenous catheters, one for blood sampling and one for infusion of glucose, insulin, and stable isotopes, were inserted in the antecubital vein of each arm after local lidocaine infiltration. The sampling arm was kept in a heated box for arterialization of blood. Hepatic and peripheral SI were measured by a hyperinsulinemic-euglycemic clamp by infusing insulin as a primed continuous infusion at a low insulin dose of 8 mU · m−2 · min−1 and a high insulin dose of 80 mU · m−2 · min−1, each step lasting 120 min. A primed continuous infusion of 6.6-deuterium–labeled glucose was used to quantify insulin’s effects on glucose turnover (37). To maintain the plasma enrichment of 2d-glucose constant at baseline value throughout the clamp, we used the hot glucose infusion method (37). Arterialized blood samples were collected every 10 min during the last 30 min of the baseline period and end of each step of the clamp for measurement of glucose enrichments, hormones, and substrates.
The glucose infusion rates were calculated during the last 30 min of each step of the clamp and expressed as milligrams of glucose per minute per meter squared. Endogenous HGP baseline and during the insulin clamp, along with the clamped glucose disposal rates, were calculated as previously reported (37).
Genotyping
Genomic DNA was extracted from peripheral blood leukocytes. Genotyping was performed with the use of a matrix-assisted–based laser desorption-ionization time-of-flight mass spectrometry on the MassARRAY platform (Sequenom) through the Yale Center for Genome Analysis (38).
Biochemical Analyses
Plasma glucose was determined using the YSI 2700 Analyzer (YSI, Yellow Springs, OH). Plasma insulin was measured by the Linco radioimmunoassay (Linco Research, Inc., St. Charles, MO), which has <1% cross-reactivity with C-peptide and proinsulin. Plasma C-peptide was assayed with an assay made by Diagnostic Products (Los Angeles, CA). Plasma proinsulin was measured using a radioimmunoassay (Linco Research, Inc.).
Statistical Analyses
Distribution of continuous variables was examined for skewness and when appropriate data were log-transformed to approximate univariate normality before association analyses by inverse normal scores. A χ2 test was used to assess the Hardy-Weinberg equilibrium for each of the studied SNPs and to compare proportions.
The primary outcome of the study was IGT. At baseline, the odds ratio (OR) of showing prediabetes according to the genotypes was evaluated by a logistic regression analysis, and age, sex, and z score BMI were used as covariates. The risk of subjects with NGT to progress to prediabetes or T2D at follow-up was calculated by running a logistic regression analysis and including as covariates age, sex, ethnicity, z score BMI at baseline, delta z score BMI, and follow-up time. The association between the genotypes and quantitative traits was evaluated by a regression model after coding the genotype with an additive model of inheritance (i.e., the genotype is coded with 0, 1, or 2 corresponding to the number of minor alleles carried by each individual), and age, sex, z score BMI, and glucose tolerance status were used as covariates when appropriate. Statistical analyses were performed with SPSS (19.0 for Windows; SPSS Inc., Chicago, IL).
Results
Clinical Phenotypes of the Subjects According to TCF7L2 rs7903146 Genotype and Ethnicity
The frequency of the TCF7L2 rs7903146 minor allele (T) was 0.336 in Caucasians, 0.286 in African Americans, and 0.286 in Hispanics. The allele frequencies were comparable with those demonstrated in similar ethnic groups according to Ensembl (http://useast.ensembl.org). The genotype distribution within each ethnic group was in Hardy-Weinberg equilibrium (P > 0.05). The clinical and anthropometric characteristics of the study population according to the TCF7L2 rs7903146 genotype are shown in Table 1. Age, sex distribution, and BMI z score were similar by TCF7L2 rs7903146 genotype and by ethnicity. Fasting glucose was significantly higher only in Caucasians carriers of the minor risk allele showed significantly higher 2-h glucose levels (Table 1). Indeed, the rs7903146 risk allele was associated with IGT in the three ethnic groups, in Caucasians (OR 1.573; 95% CI 1.100–2.250; P = 0.0131), African Americans (OR 2.011; 95% CI 1.265–3.196; P = 0.003), and Hispanics (OR 1.897; 95% CI 1.204–2.989; P = 0.006).
Table 1.
Clinical features of the study population according to the TCF7L2 rs7903146 genotype
| Caucasians |
African Americans |
Hispanics |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| CC | CT | TT | P value | CC | CT | TT | P value | CC | CT | TT | P value | |
| N | 174 | 187 | 42 | 140 | 107 | 24 | 141 | 119 | 21 | |||
| Age (years) | 14.2 ± 3.9 | 13.6 ± 3.3 | 13.2 ± 2.9 | 0.118 | 13.3 ± 3.4 | 13.3 ± 3.2 | 14.3 ± 4.3 | 0.367 | 12.3 ± 3.1 | 13.1 ± 3.1 | 11.8 ± 3.1 | 0.186 |
| Sex (male/female), % | 32/68 | 44/55 | 43/57 | 0.041 | 42/58 | 38/62 | 38/62 | 0.800 | 48/52 | 39/61 | 62/38 | 0.085 |
| BMI z score | 2.0 ± 0.81 | 2.2 ± 0.58 | 2.1 ± 0.64 | 0.055 | 2.3 ± 0.51 | 2.2 ± 0.71 | 2.1 ± 0.55 | 0.297 | 2.1 ± 0.76 | 2.2 ± 0.65 | 1.9 ± 1.4 | 0.374 |
| Tanner 1/2–3/4–5, % | 7/25/68 | 5/37/58 | 12/26/62 | 0.061 | 13/36/51 | 7/43/50 | 4/33/63 | 0.308 | 11/45/44 | 8/38/54 | 14/48/38 | 0.429 |
| Fasting glucose (mg/dL) | 90.2 ± 8.3 | 91.2 ± 8.3 | 93.9 ± 10.3 | 0.036 | 91.5 ± 8.6 | 92.1 ± 8.6 | 93.3 ± 7.1 | 0.466 | 91.6 ± 7.7 | 92.7 ± 8.6 | 96.6 ± 12.0 | 0.082 |
| 2-h glucose (mg/dL) | 118.4 ± 26.3 | 123.2 ± 27.4 | 137.1 ± 34.9 | 0.006 | 117.7 ± 28.5 | 129.5 ± 31.5 | 122.0 ± 26.4 | 0.009 | 117.8 ± 20.7 | 124.3 ± 24.4 | 129.0 ± 31.0 | 0.072 |
| HbA1c (%) | 5.4 ± 0.30 | 5.4 ± 0.30 | 5.5 ± 0.34 | 0.057 | 5.5 ± 0.35 | 5.6 ± 0.37 | 5.7 ± 0.45 | 0.094 | 5.5 ± 0.27 | 5.5 ± 0.36 | 5.5 ± 0.37 | 0.990 |
| HbA1c (mmol/mol) | 36 ± 2.3 | 36 ± 2.3 | 37 ± 2.39 | 0.057 | 37 ± 2.4 | 38 ± 2.4 | 39 ± 2.9 | 0.094 | 37 ± 1.98 | 37 ± 2.3 | 37 ± 2.4 | 0.990 |
| Insulin (μU/mL) | 30.3 ± 17.2 | 34.2 ± 19.7 | 33.2 ± 15.8 | 0.225 | 34.5 ± 18.2 | 37.4 ± 29.4 | 34.4 ± 13.7 | 0.320 | 30.3 ± 17.2 | 35.7 ± 18.0 | 42.7 ± 32.0 | 0.038 |
| WBISI (I2/mg/μU) | 2.1 ± 1.3 | 1.9 ± 1.1 | 1.8 ± 1.2 | 0.267 | 1.8 ± 1.2 | 2.0 ± 1.6 | 1.6 ± 0.61 | 0.322 | 2.0 ± 1.1 | 1.6 ± 0.94 | 2.1 ± 1.7 | 0.062 |
| IGI (μU/mg) | 4.2 ± 4.0 | 4.2 ± 3.3 | 3.8 ± 3.4 | 0.769 | 6.2 ± 4.8 | 6.6 ± 9.7 | 6.4 ± 5.0 | 0.072 | 4.6 ± 3.8 | 4.6 ± 3.0 | 3.7 ± 3.5 | 0.266 |
| DI (I2/mg2) | 6.9 ± 6.8 | 6.0 ± 4.3 | 5.5 ± 3.0 | 0.090 | 9.2 ± 5.7 | 7.9 ± 7.8 | 8.6 ± 6.0 | 0.010 | 7.6 ± 5.9 | 6.6 ± 4.7 | 6.0 ± 5.9 | 0.051 |
| OMM | ||||||||||||
| N | 138 | 127 | 25 | 89 | 71 | 16 | 110 | 73 | 15 | |||
| Φb (10−9 min−1) | 14.7 ± 6.3 | 14.9 ± 6.1 | 13.3 ± 7.2 | 0.490 | 13.8 ± 5.5 | 12.6 ± 6.7 | 12.2 ± 5.5 | 0.347 | 13.7 ± 4.5 | 15.7 ± 6.5 | 12.1 ± 6.0 | 0.839 |
| Φd (10−9 min−1) | 1,395.9 ± 765.6 | 1,431.5 ± 929.7 | 1,386.7 ± 996.2 | 0.880 | 1,963.7 ± 1,064.0 | 1,788.8 ± 1,270.1 | 1,431.6 ± 926.5 | 0.127 | 1,649.0 ± 1,007.9 | 1,679.4 ± 907.9 | 1,209.2 ± 525.6 | 0.626 |
| Φs (10−9 min−1) | 81.6 ± 49.8 | 76.4 ± 43.0 | 52.2 ± 23.0 | 0.010 | 87.4 ± 63.2 | 62.0 ± 36.3 | 75.1 ± 33.2 | 0.039 | 85.7 ± 62.7 | 78.2 ± 34.3 | 50.8 ± 19.8 | 0.858 |
| Φtotal (10−9 min−1) | 96.4 ± 55.0 | 97.1 ± 54.7 | 64.2 ± 27.8 | 0.003 | 111.347 ± 66.2 | 80.2 ± 40.8 | 88.1 ± 44.0 | 0.002 | 106.8 ± 70.9 | 92.8 ± 42.5 | 66.8 ± 26.2 | 0.035 |
| SI (10−5 dL · kg −1 · min−1/pmol · L−1) | 26.1 ± 23.4 | 25.0 ± 20.2 | 30.6 ± 27.7 | 0.841 | 24.9 ± 18.4 | 26.9 ± 21.8 | 20.4 ± 15.1 | 0.742 | 27.1 ± 18.5 | 17.0 ± 12.1 | 24.3 ± 15.0 | 0.003 |
Data are mean ± SD unless otherwise indicated.
IGI, insulinogenic index; WBISI, whole-body insulin sensitivity index.
The rs7903146 Variant in the TCF7L2 Gene Is Associated With Decreased β-Cell Responsivity (Φtotal) and a Low DI in Obese Adolescents
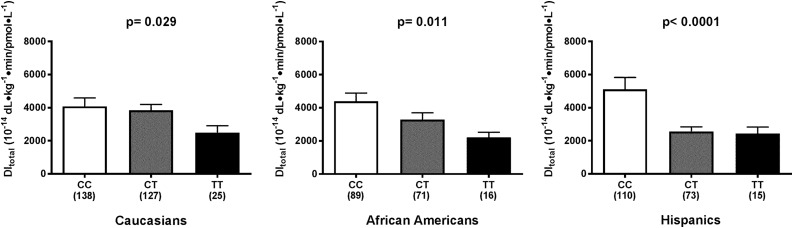
The evaluation of insulin secretion using the Oral Minimal Model (OMM) showed that subjects carrying the risk allele have a decreased β-cell responsivity (Φtotal) (in Caucasians, P = 0.003; in African Americans, P = 0.002; and in Hispanics, P = 0.035) (Table 1). Peripheral SI was, however, not affected significantly. To better express β-cell function in the context of ambient peripheral whole-body SI, we used the DI, which was significantly reduced in Caucasians (P = 0.029), African Americans (P = 0.011), and Hispanics (P < 0.0001), carriers of the risk genotype in TCF7L2 (Fig. 1).
Figure 1.
Association between the TCF7L2 rs7903146 gene and the total DI as calculated by the OMM. The results showed that the variant is associated with a lower total DI in Caucasians, African Americans, and Hispanics.
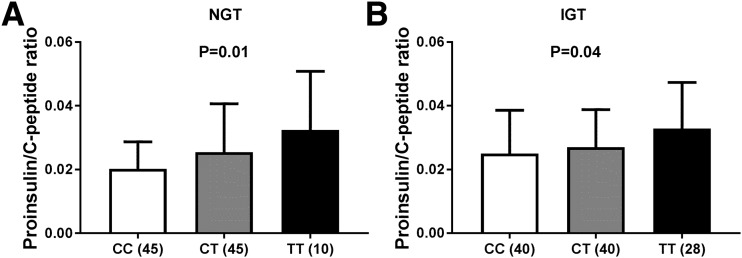
The rs7903146 Variant in the TCF7L2 Gene Is Associated With Impaired Proinsulin Processing in Obese Adolescents
Out of the 955 study subjects, in a subgroup of 208 subjects (mean ± SD age 13.2 ± 2.5 years; and mean ± SD BMI 33.4 ± 2.8), the proinsulin levels were measured to determine whether the rs7903146 variant in the TCF7L2 gene might affect the efficiency of proinsulin processing. Of them, 100 had NGT (45 CC, 45 CT, and 10 TT) and 108 IGT (40 CC, 40 CT, and 28 TT). The proinsulin to C-peptide ratio was calculated from the fasting proinsulin and C-peptide levels. The rs7903146 variant was associated with a higher proinsulin to C-peptide ratio than heterozygous in both the NGT (P = 0.01) and IGT groups (P = 0.04) (Fig. 2), even after adjusting for the effect of obesity and insulin resistance.
Figure 2.
Association between the TCF7L2 rs7903146 gene and proinsulin to C-peptide ratio. The variant is associated with a higher proinsulin to C-peptide ratio, which demonstrates that the variant impairs proinsulin processing.
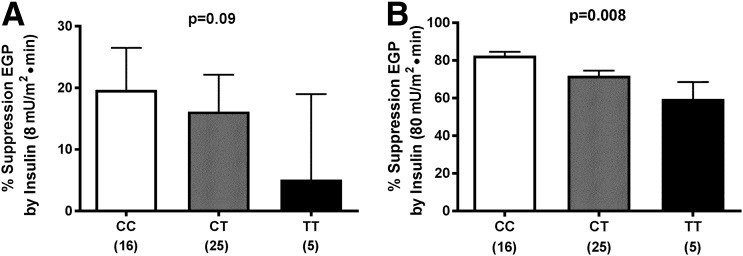
The rs7903146 Variant Is Associated With Hepatic but Not Peripheral Insulin Resistance
We explored the effect of the risk genotype of TCF7L2 on hepatic SI during a hyperinsulinemic-euglycemic clamp in 33 obese adolescents with similar BMI, fasting insulin, and glucagon (Supplementary Table 1). Of note, despite similar clamp insulin steady state in each genotype group and during each step of the clamp, homozygous carriers of the TT risk allele showed a significantly reduced suppression of HGP compared with those with the CC genotype, particularly during the high insulin dose of 80 mU/m2 · min, suggesting the presence of hepatic insulin resistance (Fig. 3).
Figure 3.
Association between the TCF7L2 rs7903146 gene and percent suppression of endogenous glucose production (EGP) by low-dose (8 mU/m2 · min) (A) and high-dose (80 mU/m2 · min) (B) insulin infusion during a hyperinsulinemic-euglycemic clamp.
The rs7903146 Variant in the TCF7L2 Gene Predisposes to Transition From IGT to T2D in Obese Adolescents: Lessons From the Longitudinal Cohort
To assess the effect of the rs7903146 variant on changes in glucose tolerance 307 subjects underwent a second OGTT after 3.11 ± 2.36 years. Two hundred two subjects (66%) were NGT at baseline (112 CC, 75 CT, and 15 TT), whereas 105 subjects (34%) were IGT at baseline (39 CC, 56 CT, and 10 TT). Compared with NGT, subjects with the diagnosis of IGT tended to show a shorter follow-up time (3.27 ± 2.43 vs. 2.28 ± 2.20; P = 0.084), but the years of follow-up did not differ across genotypes neither in the baseline NGT nor in the baseline IGT group (all P > 0.10)
In the whole population, the odds of showing IGT/T2D at follow-up were higher in subjects carrying the minor allele (OR 2.224; 95% CI 1.370–3.612; P = 0.0012). Analysis using Kaplan-Meier curves in the whole population indicated that the carriers of rs7903146 CT/TT genotypes had greater risk of IGT/T2D than CC genotype carriers (Supplementary Fig. 1). The log-rank test comparing the plots of the complement of the Kaplan-Meier estimates between risk allele carriers (CT or TT) and noncarriers (CC) showed that this relationship was statistically significant (P = 0.001) (Supplementary Fig. 1).
To assess the odds of showing IGT/T2D at follow-up according to the glucose tolerance status at baseline, the study population was divided in two groups of glucose tolerance: NGT and IGT/T2D. In the group of subjects with NGT carrying the minor allele showed a higher risk to develop IGT/T2D as compared with the group of individuals carrying the major allele (OR 2.648; 95% CI 1.326–5.291; P = 0.005) independent of age, sex, BMI, changes in BMI, follow-up time, 2-h glucose at baseline, and ethnicity. In subjects with IGT at baseline, the rs7903146 minor allele was associated with a higher risk of remaining IGT or transitioning to T2D at follow-up (OR 2.221; 95% CI 1.046–4.718; P = 0.0379) independent of age, sex, BMI, changes in BMI, follow-up time, 2-h glucose at baseline, and ethnicity.
Conclusions
In the current study, we combined detailed genetic/metabolic studies to help define how genetic variations in the TCF7L2 gene may increase the risk of T2D, particularly during the critical developmental stage of adolescence. Remarkably, we found in this very young cohort that each copy of the T allele (rs7903146) is associated with almost twofold increased odds for IGT (P = 0.0001). Additionally, our longitudinal follow-up data from the cohort suggest that the TCF7L2 risk genotype is associated with a high OR of maintaining IGT or progressing to T2D (OR 2.419; 95% CI 1.291–4.532; P = 0.006). To unravel the mechanisms that might explain the genotype/phenotype correlations, we used the OMM in a large multiethnic cohort of youths and assessed the proinsulin processing by measuring the circulating fasting proinsulin/C-peptide ratio and the clamp techniques coupled with tracer methodologies (in a subset of adolescents) to more accurately assess hepatic and peripheral SI. We found that the T allele of TCF7L2 rs7903146 has profound effects on β-cell function as reflected by a reduced DI and an altered proinsulin secretory efficiency. Moreover, its effects seem to extend to the liver by reducing insulin ability to suppress hepatic endogenous glucose production. These effects seem to occur in parallel, thus playing a critical role in two of the major defects that are key to the development of hyperglycemia.
The pathogenesis of the rapid β-cell failure and its genetic underpinnings in youth-onset IGT/T2D is poorly understood. Our study provides for the first time the evidence that the rs7903146 variant in the TCF7L2 affects functional β-cell capacity early in the course of T2D development in obese adolescents. Longitudinal follow-up of these obese adolescents suggest the mechanisms by which homozygosity for the high-risk allele at rs7903146 favors the maintenance of IGT or progression from IGT to T2D in youth.
TCF7L2, the gene with the largest effect on disease susceptibility discovered to date, was identified pre–genome-wide association by Grant et al. (18) in 2006, with rapid replication of its consequence on diabetes susceptibility in multiple populations (19,20). In the Diabetes Prevention Program (DPP) study (39), participants who were homozygous for the T allele at rs7903146 were more likely to have progression to diabetes than were those who were homozygous for the C allele (hazard ratio 1.55; 95% CI 1.20–2.01; P < 0.001). The genotypic relative risk reported in this study in our obese adolescents might differ slightly from the OR documented by Grant et al. (18) and Florez et al. (39), owing to the younger age of our cohort. Our study is consistent with data reported in a population of young adults without diabetes participating in the Young Finns Study (40), indicating that the TCF7L2 variant predicts the incidence of impaired fasting glucose.
Despite the evidence provided in this study in a very young cohort and by previous studies in adults of an effect of the rs7903146 variant on insulin secretion, resolving the functional mechanisms underlying these associations has been, so far, extremely challenging. The molecular mechanisms by which variants in TCF7L2 increase the risk of T2D have not been fully elucidated. TCF7L2 encodes a transcription factor that is a member of the Wnt signaling pathway known to be active not only in the β-cells (27) but also in other organs, including liver. Both increased and decreased TCF7L2 expression in β-cells has been associated with altered insulin secretion and apoptosis in human islets (27) and altered proinsulin processing (27). Notably, rs7903146 in TCF7L2, which shows consistent T2D association in samples across diverse ethnic groups, is located in an islet-selective open chromatin site (41,42). Thus, in human islet cells, the chromatin state at rs7903146 is more open in chromosomes carrying the T allele, which is associated with increased T2D risk. Furthermore, there is also previous experimental support for the finding of elevated proinsulin/insulin ration in carriers of the T allele, showing that a number of genes involved in proinsulin processing is altered in animals with knockdown of TCF7L2 or human carriers of the T allele (43).
Although the genetic association with T2D seems to arise from TCF7L2’s function in pancreatic β-cells, emerging studies provide evidence of the role of TCF7L2 in the liver as well (30,44). Reports of functional studies in humans comparing hepatic SI between carriers of the risk SNP and control subjects are inconsistent. Human carriers of the TCF7L2 rs7903146 risk T allele have been reported to have elevated HGP (29). Florez et al. (39) reported impaired insulin secretion accompanied by higher hepatic SI in carriers of the T allele. In contrast, Schäfer et al. (29) could not confirm an association of the risk allele with clamp-measured SI. More recently, Varghese et al. (45) in a small group of overweight, adult subjects without diabetes did not find that genetic variation at TCF7L2 alters either hepatic or extrahepatic insulin action. The contrasting differences on the effect of the TCF7L2 variant between our study and that of Varghese et al. (45) are likely because of the younger age and greater severity of obesity of our subjects and the fact that we used a higher insulin to completely suppress HGP.
In the liver, the WNT–β-catenin pathway is involved in metabolic zonations (i.e., hepatocytes exhibit different metabolic profiles [glycolysis vs. gluconeogenesis] depending on their localization along the portocentral axis) (46). TCF7L2 expression is highest in pericentral hepatocytes, in which gluconeogenesis is low. Recently, Neve et al. (46) reported a significant correlation between increased expression of alternative TCF7L2 liver transcripts and the T2D-associated rs7901346 risk allele in obese normoglycemic individuals. These results underscore the importance of characterizing the role of TCF7L2 in the pathogenic mechanisms leading to T2D. In light of the key role of the liver and the strong association found with the common noncoding TCF7L2 SNP with prediabetes/T2D in adolescents, we explored if TCF7L2 variant rs7903146 affects hepatic SI in obese adolescents and found that subjects with the TT risk genotype had a significantly impaired suppression in HGP during the hyperinsulinemic clamp. Although these results should be replicated in a larger number of subjects with the T risk allele, they do suggest that the risk variant is not only confined to the β-cell but also involves the liver. Additional studies aimed at deciphering the impact of this key gene variant on hepatic glucose fluxes and determining whether gluconeogenesis is increased according to the TCF7L2 genotype are needed.
Despite this evidence, it cannot be excluded that the effect on the liver might be somehow mediated by the pancreas. In other words, the insufficient insulin levels, because of an impaired β-cell response in subjects carrying the TCF7L2 risk allele, might be responsible for the increase in glucose production in the liver.
Evidence today would indicate that the T2D seems to be more aggressive and deteriorating at a faster pace than what usually seen in adults (10,47). Of note, our data suggest that obese adolescents homozygous for the “risk” TCF7L2 genotype followed over a 2-year window showed a greater risk of remaining IGT or developing T2D compared with those with the nonrisk TCF7L2 genotype.
Our study has some limitations. We acknowledge the small sample size of the longitudinal cohort and of those undergoing the hyperinsulinemic-euglycemic clamp. The strengths of our study are the young age of our patients and the assessment of insulin secretion by the OMM and in a subgroup by the hyperinsulinemiceuglycemic clamp and the longitudinal component.
In conclusion, this is the first study showing in obese adolescents the association between the TCF7L2 rs7903146 and β-cell dysfunction, with impaired proinsulin processing and decreased hepatic SI. The TCF7L2 variant is implicated in the progression of prediabetes to T2D in the pediatric population.
Supplementary Material
Article Information
Acknowledgments. The authors thank the patients and families as well as the Yale Center for Genome Analysis and the Yale Center for Clinical Investigation and Hospital Research Unit personnel.
Funding. This work has been made possible by National Institute of Diabetes and Digestive and Kidney Diseases grants R01-DK-111038 and R01-HD-028016 (to S.C.). C.C. was supported by “Progetti di Ricerca di Ateneo 2014” grant CPDA145405/14. N.S. is supported by the American Heart Association through grants 13SDG14640038 and 16IRG27390002 and by the Allen Foundation award. A.G. received a Research Fellowship from the International Society for Pediatric and Adolescent Diabetes. This work was also made possible by Eunice Kennedy Shriver National Institute of Child Health and Human Development and National Institute of Diabetes and Digestive and Kidney Diseases grant DK-045735 to the Yale Diabetes Research Center and by the National Center for Advancing Translational Sciences, a component of the National Institutes of Health, and National Institutes of Health Roadmap for Medical Research Clinical and Translational Science Awards grant UL1-RR-024139.
This article's contents are solely the responsibility of the authors and do not necessarily represent the official view of the National Institutes of Health.
Duality of Interest. No potential conflicts of interest relevant to this article were reported.
Author Contributions. C.C., N.S., and S.C. analyzed and reviewed the data and wrote and edited the manuscript. L.G. genotyped the TCF7L2 SNP. C.C. and C.D.M. analyzed the data on insulin secretion using the OMM. A.G., R.K., B.P., and M.G. performed the clamps and RT-PCR of the liver. N.S. and S.C. are the guarantors of this work and, as such, had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Footnotes
This article contains Supplementary Data online at http://care.diabetesjournals.org/lookup/suppl/doi:10.2337/dc17-0290/-/DC1.
References
- 1.Imperatore G, Boyle JP, Thompson TJ, et al.; SEARCH for Diabetes in Youth Study Group . Projections of type 1 and type 2 diabetes burden in the U.S. population aged <20 years through 2050: dynamic modeling of incidence, mortality, and population growth. Diabetes Care 2012;35:2515–2520 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Dabelea D, Mayer-Davis EJ, Saydah S, et al.; SEARCH for Diabetes in Youth Study . Prevalence of type 1 and type 2 diabetes among children and adolescents from 2001 to 2009. JAMA 2014;311:1778–1786 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Demmer RT, Zuk AM, Rosenbaum M, Desvarieux M. Prevalence of diagnosed and undiagnosed type 2 diabetes mellitus among US adolescents: results from the continuous NHANES, 1999-2010. Am J Epidemiol 2013;178:1106–1113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sinha R, Fisch G, Teague B, et al. Prevalence of impaired glucose tolerance among children and adolescents with marked obesity [published correction appears in N Engl J Med 2002;346:1756]. N Engl J Med 2002;346:802–810 [DOI] [PubMed] [Google Scholar]
- 5.Constantino MI, Molyneaux L, Limacher-Gisler F, et al. Long-term complications and mortality in young-onset diabetes: type 2 diabetes is more hazardous and lethal than type 1 diabetes. Diabetes Care 2013;36:3863–3869 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dean HJ, Sellers EA. Comorbidities and microvascular complications of type 2 diabetes in children and adolescents. Pediatr Diabetes 2007;8(Suppl. 9):35–41 [DOI] [PubMed] [Google Scholar]
- 7.Orchard TJ. The changing face of young-onset diabetes: type 1 optimism mellowed by type 2 concerns. Diabetes Care 2013;36:3857–3859 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rhodes ET, Prosser LA, Hoerger TJ, Lieu T, Ludwig DS, Laffel LM. Estimated morbidity and mortality in adolescents and young adults diagnosed with type 2 diabetes mellitus. Diabet Med 2012;29:453–463 [DOI] [PubMed] [Google Scholar]
- 9.Gungor N, Arslanian S. Progressive beta cell failure in type 2 diabetes mellitus of youth. J Pediatr 2004;144:656–659 [DOI] [PubMed] [Google Scholar]
- 10.Weiss R, Taksali SE, Tamborlane WV, Burgert TS, Savoye M, Caprio S. Predictors of changes in glucose tolerance status in obese youth. Diabetes Care 2005;28:902–909 [DOI] [PubMed] [Google Scholar]
- 11.Sladek R, Rocheleau G, Rung J, et al. A genome-wide association study identifies novel risk loci for type 2 diabetes. Nature 2007;445:881–885 [DOI] [PubMed] [Google Scholar]
- 12.Saxena R, Voight BF, Lyssenko V, et al.; Diabetes Genetics Initiative of Broad Institute of Harvard and MIT, Lund University, and Novartis Institutes of BioMedical Research . Genome-wide association analysis identifies loci for type 2 diabetes and triglyceride levels. Science 2007;316:1331–1336 [DOI] [PubMed] [Google Scholar]
- 13.Florez JC. Newly identified loci highlight beta cell dysfunction as a key cause of type 2 diabetes: where are the insulin resistance genes? Diabetologia 2008;51:1100–1110 [DOI] [PubMed] [Google Scholar]
- 14.O’Rahilly S, Barroso I, Wareham NJ. Genetic factors in type 2 diabetes: the end of the beginning? Science 2005;307:370–373 [DOI] [PubMed] [Google Scholar]
- 15.McCarthy MI. Genomics, type 2 diabetes, and obesity. N Engl J Med 2010;363:2339–2350 [DOI] [PubMed] [Google Scholar]
- 16.Zeggini E, Weedon MN, Lindgren CM, et al.; Wellcome Trust Case Control Consortium (WTCCC) . Replication of genome-wide association signals in UK samples reveals risk loci for type 2 diabetes. Science 2007;316:1336–1341 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Zeggini E, Scott LJ, Saxena R, et al.; Wellcome Trust Case Control Consortium . Meta-analysis of genome-wide association data and large-scale replication identifies additional susceptibility loci for type 2 diabetes. Nat Genet 2008;40:638–645 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Grant SF, Thorleifsson G, Reynisdottir I, et al. Variant of transcription factor 7-like 2 (TCF7L2) gene confers risk of type 2 diabetes. Nat Genet 2006;38:320–323 [DOI] [PubMed] [Google Scholar]
- 19.Saxena R, Gianniny L, Burtt NP, et al. Common single nucleotide polymorphisms in TCF7L2 are reproducibly associated with type 2 diabetes and reduce the insulin response to glucose in nondiabetic individuals. Diabetes 2006;55:2890–2895 [DOI] [PubMed] [Google Scholar]
- 20.Cauchi S, El Achhab Y, Choquet H, et al. TCF7L2 is reproducibly associated with type 2 diabetes in various ethnic groups: a global meta-analysis. J Mol Med (Berl) 2007;85:777–782 [DOI] [PubMed] [Google Scholar]
- 21.Körner A, Berndt J, Stumvoll M, Kiess W, Kovacs P. TCF7L2 gene polymorphisms confer an increased risk for early impairment of glucose metabolism and increased height in obese children. J Clin Endocrinol Metab 2007;92:1956–1960 [DOI] [PubMed] [Google Scholar]
- 22.Roth CL, Hinney A, Reinehr T, et al. TCF7L2 polymorphism rs7903146 and predisposition for type 2 diabetes mellitus in obese children. Horm Metab Res 2008;40:713–717 [DOI] [PubMed] [Google Scholar]
- 23.Lyssenko V, Lupi R, Marchetti P, et al. Mechanisms by which common variants in the TCF7L2 gene increase risk of type 2 diabetes. J Clin Invest 2007;117:2155–2163 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Smith U. TCF7L2 and type 2 diabetes--we WNT to know. Diabetologia 2007;50:5–7 [DOI] [PubMed] [Google Scholar]
- 25.Hansson O, Zhou Y, Renström E, Osmark P. Molecular function of TCF7L2: consequences of TCF7L2 splicing for molecular function and risk for type 2 diabetes. Curr Diab Rep 2010;10:444–451 [DOI] [PubMed] [Google Scholar]
- 26.Jin T, Liu L. The Wnt signaling pathway effector TCF7L2 and type 2 diabetes mellitus. Mol Endocrinol 2008;22:2383–2392 [DOI] [PubMed] [Google Scholar]
- 27.Shu L, Sauter NS, Schulthess FT, Matveyenko AV, Oberholzer J, Maedler K. Transcription factor 7-like 2 regulates beta-cell survival and function in human pancreatic islets [retracted in: Diabetes 2014;63:3974]. Diabetes 2008;57:645–653 [DOI] [PubMed] [Google Scholar]
- 28.Pilgaard K, Jensen CB, Schou JH, et al. The T allele of rs7903146 TCF7L2 is associated with impaired insulinotropic action of incretin hormones, reduced 24 h profiles of plasma insulin and glucagon, and increased hepatic glucose production in young healthy men. Diabetologia 2009;52:1298–1307 [DOI] [PubMed] [Google Scholar]
- 29.Schäfer SA, Tschritter O, Machicao F, et al. Impaired glucagon-like peptide-1-induced insulin secretion in carriers of transcription factor 7-like 2 (TCF7L2) gene polymorphisms [published correction appears in Diabetologia 2008;51:208 and 2009;52:557]. Diabetologia 2007;50:2443–2450 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Boj SF, van Es JH, Huch M, et al. Diabetes risk gene and Wnt effector Tcf7l2/TCF4 controls hepatic response to perinatal and adult metabolic demand. Cell 2012;151:1595–1607 [DOI] [PubMed] [Google Scholar]
- 31.Breda E, Cavaghan MK, Toffolo G, Polonsky KS, Cobelli C. Oral glucose tolerance test minimal model indexes of beta-cell function and insulin sensitivity. Diabetes 2001;50:150–158 [DOI] [PubMed] [Google Scholar]
- 32.O’Malley G, Santoro N, Northrup V, et al. High normal fasting glucose level in obese youth: a marker for insulin resistance and beta cell dysregulation. Diabetologia 2010;53:1199–1209 [DOI] [PubMed] [Google Scholar]
- 33.Cobelli C, Dalla Man C, Toffolo G, Basu R, Vella A, Rizza R. The oral minimal model method. Diabetes 2014;63:1203–1213 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Dalla Man C, Caumo A, Basu R, Rizza R, Toffolo G, Cobelli C. Minimal model estimation of glucose absorption and insulin sensitivity from oral test: validation with a tracer method. Am J Physiol Endocrinol Metab 2004;287:E637–E643 [DOI] [PubMed] [Google Scholar]
- 35.Dalla Man C, Caumo A, Basu R, Rizza R, Toffolo G, Cobelli C. Measurement of selective effect of insulin on glucose disposal from labeled glucose oral test minimal model. Am J Physiol Endocrinol Metab 2005;289:E909–E914 [DOI] [PubMed] [Google Scholar]
- 36.Dalla Man C, Yarasheski KE, Caumo A, et al. Insulin sensitivity by oral glucose minimal models: validation against clamp. Am J Physiol Endocrinol Metab 2005;289:E954–E959 [DOI] [PubMed] [Google Scholar]
- 37.Weiss R, Dufour S, Taksali SE, et al. Prediabetes in obese youth: a syndrome of impaired glucose tolerance, severe insulin resistance, and altered myocellular and abdominal fat partitioning. Lancet 2003;362:951–957 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Giannini C, Dalla Man C, Groop L, et al. Co-occurrence of risk alleles in or near genes modulating insulin secretion predisposes obese youth to prediabetes. Diabetes Care 2014;37:475–482 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Florez JC, Jablonski KA, Bayley N, et al.; Diabetes Prevention Program Research Group . TCF7L2 polymorphisms and progression to diabetes in the Diabetes Prevention Program. N Engl J Med 2006;355:241–250 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Raitakari OT, Rönnemaa T, Huupponen R, et al. Variation of the transcription factor 7-like 2 (TCF7L2) gene predicts impaired fasting glucose in healthy young adults: the Cardiovascular Risk in Young Finns Study [published correction appears in Diabetes Care 2007;30:3154]. Diabetes Care 2007;30:2299–2301 [DOI] [PubMed] [Google Scholar]
- 41.Gaulton KJ, Nammo T, Pasquali L, et al. A map of open chromatin in human pancreatic islets. Nat Genet 2010;42:255–259 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Savic D, Park SY, Bailey KA, Bell GI, Nobrega MA. In vitro scan for enhancers at the TCF7L2 locus. Diabetologia 2013;56:121–125 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Zhou Y, Zhang E, Berggreen C, et al. Survival of pancreatic beta cells is partly controlled by a TCF7L2-p53-p53INP1-dependent pathway. Hum Mol Genet 2012;21:196–207 [DOI] [PubMed] [Google Scholar]
- 44.Jin T. Current understanding on role of the Wnt signaling pathway effector TCF7L2 in glucose homeostasis. Endocr Rev 2016;37:254–277 [DOI] [PubMed] [Google Scholar]
- 45.Varghese RT, Viegas I, Barosa C, et al. Diabetes-associated variation in TCF7L2 is not associated with hepatic or extrahepatic insulin resistance. Diabetes 2016;65:887–892 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Neve B, Le Bacquer O, Caron S, et al. Alternative human liver transcripts of TCF7L2 bind to the gluconeogenesis regulator HNF4α at the protein level. Diabetologia 2014;57:785–796 [DOI] [PubMed] [Google Scholar]
- 47.Giannini C, Weiss R, Cali A, et al. Evidence for early defects in insulin sensitivity and secretion before the onset of glucose dysregulation in obese youths: a longitudinal study. Diabetes 2012;61:606–614 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.