Abstract
Sexual debut experience may influence HIV/sexual risks among men who have sex with men (MSM). We assessed associations between age of sexual debut and sex of debut partner with recent (past-3-month) sexual/HIV/syphilis risks among 3588 community-based Chinese MSM. Sexual debut with women was associated with more recent (condomless) insertive anal sex with men, more recent (condomless) vaginal sex, and more lifetime female partners. Sexual debut with men was associated with more recent (condomless) receptive anal sex with men and more lifetime male partners. All associations were strongest among those having first sex ≤18 years in both groups. Earlier sexual debut was associated with higher HIV/syphilis risk; HIV risk was higher with first sex with a man, but syphilis was higher with first sex with a woman. Earlier age of sexual debut is associated with greater HIV/syphilis and sexual risks, but MSM risk differs with first sex with women versus men.
Keywords: HIV, Syphilis, Sexual debut, Chinese men who have sex with men, Sexual risk
Introduction
Despite the national efforts in scaling up prevention interventions, men who have sex with men (MSM) in China continue to represent the most affected population by HIV [1, 2]. While HIV epidemics have stabilized or declined among other high-risk populations (e.g., female sex workers, people who inject drugs), HIV prevalence among Chinese MSM had increased from 0.9% in 2003 to 7.7% in 2014 [3]. In 2014, MSM accounted for 25.8% of the newly diagnosed HIV cases in China [3]. Personal, social, and structural barriers have resulted in the under-representation of Chinese MSM in HIV testing, post-diagnosis linkage-to-care, and treatment initiation/retention [4, 5], which limits the success of “test-and-treat” and “treatment as prevention” strategies to tackle the HIV epidemic among this high-risk subgroup [6].
Most Chinese MSM do not disclose their sexual identity to their family members, relatives and friend as a result of homosexuality-related stigma [7, 8]. Chinese men are also influenced by the traditional norms and cultural pressure to marry a woman (all “women/woman” in this paper are referred to cisgender women/woman unless specified), not only to carry their family line, but also to avoid bringing shame or disappointment to their parents by remaining single [9–11]. Therefore, practice of bisexual behaviors is common among Chinese MSM as well as in other culturally conservative Asian countries [12]. A recent meta-analysis showed that 31.2% of the 28,739 MSM in China had ever had sex with a woman [13]. Men who have sex with men and women (MSMW) are less likely to be infected with HIV than MSM-only (MSMO), probably because MSMW are more likely to practice insertive anal (with a man) and virginal intercourse with a woman, which is associated with lower HIV risk compared to receptive anal intercourse with a man [12, 14–16]. On the other hand, MSMW are shown not to use condom consistently with female sexual partners [17], which may bridge HIV/STIs to their average-risk female sexual partners [18].
The first sexual experience is an important part of one’s life and human development [19]. Partner characteristics and age at sexual debut may influence future mental/sexual health and set risky behavior patterns [20]. Studies show that MSM who have sexual debut at a younger age are more likely to sell sex for money/drugs, have more sexual partners, practice condomless sex and encounter psychological/emotional problems [19, 21]. Another study also shows that MSM who have their first sex with an older partner may be at elevated risk of HIV and STIs [22]. In the context of sexual debut and bisexual behavior among MSM, it is likely that some men have their sexual debuts with women, but later initiate sex with men; some men continue bisexual behaviors with varying gender-specific frequencies. These MSM subgroups may carry different sociodemographic and sexual risk profiles that should be understood for designing specific HIV risk reduction strategies.
We have not identified any study that has assessed the influence of sex of first partner and age of sexual debut on subsequent sexual behaviors and HIV risk among MSM, despite its important implications for targeting prevention interventions. In a community-based sample of MSM in Beijing, China, we compared the sociodemographic and behavioral characteristics by sex of first partner, assessed the associations of sex of first partner with subsequent sexual/HIV/syphilis risk, examining whether associations are modified by their age of sexual debut.
Methods
Study Design and Population
We used the baseline data among a convenient sample of MSM from a randomized controlled trial: Multi-component HIV Intervention Packages for Chinese MSM—Test, Link and Care (China-MP3 trial; ClinicalTrials.gov Identifier: NCT01904877). Details of the parent trial design and study setting are described elsewhere [23, 24]. In short, we recruited 3760 self-reported HIV-uninfected or status unknown men between March 2013 and March 2014 via short message services, gay website-based advertisement, peer referral, outreach to gay-frequented venues and recruitment during their visit at our participating HIV hospitals/clinics. Men who self-reported to be (1) ≥18 years old, (2) having anal sex with men or transgender women in the past 12 months, (3) currently living in Beijing and not planning to leave in the next 12 months, and (4) willing/able to provide written informed consent, were eligible for study participation. The institutional review boards of Vanderbilt University and the National Center for AIDS/STD Control and Prevention of the China Center for Disease Control and Prevention reviewed and approved the study protocol.
Data Collection
A face-to-face questionnaire interview was administered by trained medical staff to survey: (1) sociodemographic information, including age, age of sexual debut, ethnicity, current marital status, education, employment, monthly income, health insurance, perception of HIV risk (self-report perception of “likely/very likely” or “low/no” risk to contract HIV), venues of seeking male sexual partners, house-hold registration status (Hukou), years of living in Beijing, residence of origin, and HIV testing history; (2) high-risk behaviors, including recent (in the past 3 months pre-survey) hazardous alcohol drinking (assessed with Alcohol Use Disorder Identification Test-Consumption, AUDIT-C, score ranges between 0 and 12, with a score ≥4 indicating hazardous alcohol drinking) [25], recent binge drinking (having 6 or more standard drinks on one occasion) [25], recent illicit drug use (self-report intake of methamphetamine, MDMA, rush, magu, ketamine, cannabis/marijuana, cocaine, opium, or heroin, morphine), recent pattern/frequency of insertive/ receptive anal sex with men, recent anal sex with HIV-infected men, recent sex with male commercial sex workers, recent pattern/frequency of vaginal sex with women (all “women/woman” in the analyses were confined to cisgender women/woman), year of sexual activity, and lifetime number of male/female sexual partners. We also tested participants for rapid HIV and syphilis tests after the questionnaire survey. For those with positive HIV or syphilis rapid test results, a 5-ml blood specimen was drawn for further laboratory screening and confirmatory tests. Each participant was provided pre-test and post-test counselling and compensated 50 Yuan (≈US$8.) for transportation costs. Detailed measures of the variables and laboratory techniques are documented elsewhere [23, 24, 26].
Statistical Analysis
We used median with interquartile range (IQR; for continuous measures) and frequency distribution with percentage (for categorical measures) to describe the sociodemographic and high-risk behaviors among the participants. A predictive logistic regression model was built to evaluate sociodemographic predictors of having sexual debut with a woman. Factors (p < 0.05) associated with having sexual debut with a woman from the Chi square test or Wilcoxon Rank-Sum test were entered into a preliminary multivariable model, followed by a stepwise backward selection procedure to retain significant predictors (p < 0.05) for multivariable adjustment. Collinearity between included variables was assessed before fitting the final model.
To assess the association between sex of first partner and sexual risk among the participants, we first used a Chi square test to compare the high-risk behaviors (categorical variables) between those having sexual debut with a man versus with a woman. We further used separate multi-variable ordinal logistic regression to assess the association between sex of first partner and the likelihood of attaining a higher frequency category of selected risky sexual behaviors (continuous variables). We categorized these continuous variables into quartiles, and merged adjacent categories for some variables when necessary to avoid sparse data. These risky behaviors include: (1) total number of lifetime male sexual partners (1–4, 5–9, 10–19, ≥20), (2) total number of receptive anal sex with men in the past 3 months (0, 1, 2, ≥3), (3) total number of condomless receptive anal sex with men in the past 3 months (0, 1, 2, ≥3), (4) total number of insertive anal sex with men in the past 3 months (0, 1–2, 3–4, ≥5), (5) total number of condomless insertive anal sex with men in the past 3 months (0, 1, 2, ≥3), (6) total number of lifetime female sexual partners (0, 1, ≥2), (7) total number of vaginal sex with women in the past 3 months (0,1–2, ≥3), and (8) total number of condomless vaginal sex with women in the past 3 months (0,1–2, ≥3). We adjusted each model for age, education, perception of HIV risk, sex-finding venue, residence of origin, and migration status. The proportional odds assumption was tested and fulfilled for each of the multivariable models. We stratified the analyses to assess if their sexual risk may vary by age of sexual debut (≤18, 19–22 and ≥23 years).
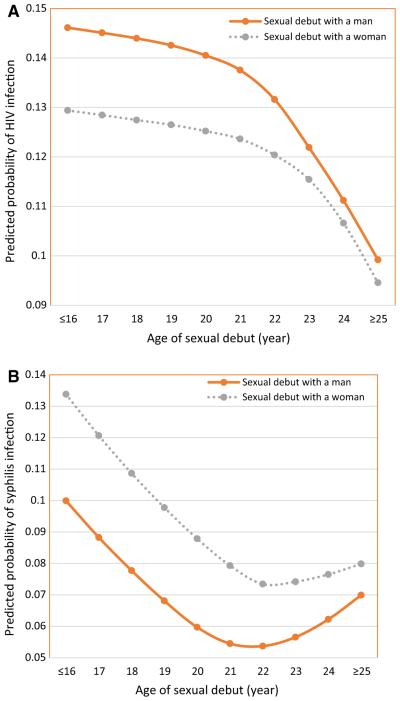
Last, we used logit models and applied restricted cubic splines with four knots to model the non-linear relationship between age of sexual debut (≤16, 17, 18, 19, 20, 21, 22, 23, 24 and ≥25) and the predicted probability of being HIV or syphilis infection, by sex of first partner, adjusting for age, education, perception of HIV risk, sex-finding venue, residence of origin and migration status. All youth with sexual debut ≤16 years (cumulative %: 3.7%) were merged into a ≤16 year category; similarly, persons with sexual debuts at any age ≥25 years (cumulative %: 4.8%) were merged, to avoid sparse data. Data analyses were conducted using Stata 12.0™ (StataCorp LP, College Station, Texas, USA).
Results
Population Characteristics
Among the 3760 recruited participants, 172 men were excluded due to duplicate participation (126), confirmed prior HIV infection (30), no blood specimen collected (5), non-MSM (5), invalid identification numbers (4), and lack of a questionnaire (2), resulting in a final analytical sample of 3588 (95.4%). Of these 3588 men (transgender women were eligible, but none were recruited), the median age was 28 years (IQR: 24–33) and the median age of sexual debut was 20 years (IQR: 18–23). A majority of the participants were of Han-ethnicity (93.7%), single (85.0%), college-educated (71.9%), employed (82.5%), health-insured (61.1%), migrants (75.2%), previously residing in a city (67.9%), and finding sex via the Internet (79.1%). Confirmed HIV prevalence was 12.7%, and syphilis prevalence was 7.5%.
Thirty percent of our participants reported ever engaging in bisexual behavior, and 29.6% had their first sex with a woman. Compared to MSM who had their sexual debut with a man, MSM who had sexual debut with a woman were significantly (p < 0.05) more likely to be older, older at age of sexual debut, currently married, having education below college, not current students, self-perceiving low/no HIV risk, not health-insured, finding sex via non-Internet venues, migrants, having residence of origin in township/ village areas, living in Beijing for a longer duration, and syphilis-infected (Table 1).
Table 1.
Characteristics of Chinese MSM who had sexual debut with a male or female sexual partner (N = 3588)
| Characteristics | Total N = 3588 n (%) |
Sexual debut |
χ2 or z-statistics | p value | |
|---|---|---|---|---|---|
| With a man N = 2538 n (%) |
With a woman N = 1050 n (%) |
||||
| Age (year) | 352.654 (χ2) –18.349 (z) |
<0.001* | |||
| Median (IQR) | 28 (24–33) | 27 (24–31) | 32 (27–40) | ||
| <25 | 914 (25.5) | 764 (30.1) | 150 (14.3) | ||
| 25–34 | 1927 (53.7) | 1440 (56.7) | 487 (46.4) | ||
| 35–44 | 536 (14.9) | 265 (10.5) | 271 (25.8) | ||
| ≥45 | 211 (5.9) | 69 (2.7) | 142 (13.5) | ||
| Age of sexual debut (year) | 36.355 (χ2) –6.203 (z) |
<0.001* | |||
| Median (IQR) | 20 (18–23) | 20 (18–22) | 21 (19–24) | ||
| ≤18 | 995 (27.7) | 749 (29.5) | 246 (23.4) | ||
| 19–22 | 1642 (45.8) | 1186 (46.7) | 456 (45.8) | ||
| ≤23 | 951 (26.5) | 603 (23.8) | 951 (26.5) | ||
| Ethnicity | 1.254 | 0.263 | |||
| Han | 3361 (93.7) | 2370 (93.4) | 991 (94.4) | ||
| Non-Han | 227 (6.3) | 168 (6.6) | 59 (5.6) | ||
| Current marital status | 559.229 | <0.001 | |||
| Single | 3049 (85.0) | 2387 (94.0) | 662 (63.0) | ||
| Married | 539 (15.0) | 151 (6.0) | 388 (37.0) | ||
| Education (year of schooling) | 235.261 | <0.001 | |||
| College and above (>12) | 2579 (71.9) | 2010 (79.2) | 569 (54.2) | ||
| Senior high (10–12) | 593 (16.5) | 327 (12.9) | 266 (25.3) | ||
| Junior middle school and less (≤9) |
416 (11.6) | 201 (7.9) | 215 (20.5) | ||
| Employment | 117.416 | <0.001 | |||
| Employed | 2960 (82.5) | 2031 (80.0) | 929 (88.5) | ||
| Unemployed/retired | 182 (5.1) | 109 (4.3) | 73 (6.9) | ||
| Student | 388 (10.8) | 363 (14.3) | 25 (2.4) | ||
| Other | 58 (1.6) | 35 (1.4) | 23 (2.2) | ||
| Personal monthly income, Chinese yuan | 0.258 | 0.612 | |||
| <5000 | 1698 (47.3) | 1208 (47.6) | 490 (46.7) | ||
| ≥5000 | 1890 (52.7) | 1330 (52.4) | 560 (53.3) | ||
| Health insurance | 36.048 | <0.001 | |||
| No | 1395 (38.9) | 907 (35.7) | 488 (46.5) | ||
| Yes | 2193 (61.1) | 1631 (64.3) | 562 (53.5) | ||
| Perception of HIV risk prior to HIV diagnosis | 7.570 | 0.006 | |||
| Likely/very likely | 1462 (40.7) | 1071 (42.2) | 391 (37.2) | ||
| Low/no risk | 2126 (59.3) | 1467 (57.8) | 659 (62.8) | ||
| Sex-finding venue | 160.794 | <0.001 | |||
| Internet | 2838 (79.1) | 2148 (84.6) | 690 (65.7) | ||
| Non-Internet** | 750 (20.9) | 390 (15.4) | 360 (34.3) | ||
| Migrant (No Beijing Hukou) | 27.021 | <0.001 | |||
| No | 889 (24.8) | 690 (27.2) | 199 (18.9) | ||
| Yes | 2699 (75.2) | 1848 (72.8) | 851 (81.1) | ||
| Year of living in Beijing | 18.267 | <0.001 | |||
| ≤5 | 1533 (42.7) | 1142 (45.0) | 391 (37.2) | ||
| >5 | 2055 (57.3) | 1396 (55.0) | 659 (62.8) | ||
| Residence of origin | 39.715 | <0.001 | |||
| City | 2437 (67.9) | 1804 (71.1) | 633 (60.3) | ||
| Township/village | 1151 (32.1) | 734 (28.9) | 417 (39.7) | ||
| HIV infection | 1.019 | 0.313 | |||
| No | 3133 (87.3) | 2207 (87.0) | 926 (88.2) | ||
| Yes | 455 (12.7) | 331 (13.0) | 124 (11.8) | ||
| Syphilis infection | 5.145 | 0.023 | |||
| No | 3319 (92.5) | 2364 (93.1) | 955 (90.9) | ||
| Yes | 269 (7.5) | 174 (6.9) | 95 (9.1) | ||
p < 0.001 for both Chi square Test (categorical age and age of sexual debut) and Wilcoxon Rank-Sum Test (continuous age and age of sexual debut)
Park, bar or night/dance club, public bathroom, fitness center/gym, public restroom, college dormitory, beach, woods, street, theater, public transportation, hotel and private homes
IQR interquartile rage; Hukou household registration; 1 Chinese yuan ≈ 0.15 US dollar
Predictors of Having Sexual Debut with a Woman
Table 2 shows the significant predictors of having sexual debut with a woman. These included (after multivariable adjustment): older current age [e.g., ≥45 years vs. 25 years, adjusted odds ratio (AOR): 3.03; 95% confidence interval (CI) 2.03–4.52; p < 0.001], being currently married (AOR: 4.93; 95% CI 3.89–6.23; p < 0.001), being less educated (e.g., junior middle school and less vs. college and above, AOR: 1.75; 95% CI 1.42–2.17; p < 0.001), self-perceiving low/no risk of HIV (AOR: 1.23; 95% CI 1.06–1.42; p = 0.008), finding sexual partners via non-Internet venues (AOR: 1.69; 95% CI 1.39–2.06; p < 0.001), being migrants (AOR: 1.57; 95% CI 1.28–1.93; p < 0.001), and having township/village residence of origin (AOR: 1.40; 95% CI 1.19–1.65; p < 0.001).
Table 2.
Sociodemographic predictors of Chinese men who have sex with men experiencing sexual debut with a woman (N = 3588)
| Characteristics | AOR (95% CI)† | p-value |
|---|---|---|
| Age, year | ||
| <25 | Reference | |
| 25–34 | 1.48 (1.20, 1.83) | <0.001 |
| 35–44 | 2.53 (1.92, 3.34) | <0.001 |
| ≥45 | 3.03 (2.03, 4.52) | <0.001 |
| Current marital status | ||
| Single | Reference | |
| Married | 4.93 (3.89, 6.23) | <0.001 |
| Education (year of schooling) | ||
| College and above (>12) | Reference | |
| Senior high (10–12) | 1.51 (1.16, 1.96) | 0.002 |
| Junior middle school and less (≤9) | 1.75 (1.42, 2.17) | <0.001 |
| Perception of HIV risk prior to HIV diagnosis | ||
| Likely/very likely | Reference | |
| Low/no risk | 1.23 (1.06, 1.42) | 0.008 |
| Sex-finding venue | ||
| Internet | Reference | |
| Non-Internet** | 1.69 (1.39, 2.06) | <0.001 |
| Migrant (No Beijing Hukou) | ||
| No | Reference | |
| Yes | 1.57 (1.28, 1.93) | <0.001 |
| Residence of origin | ||
| City | Reference | |
| Township/village | 1.40 (1.19, 1.65) | <0.001 |
AOR adjusted odds ratio; CI confidence interval; Hukou household registration
Only significant predictors (p < 0.05) after stepwise backward selection are presented in the current table and are adjusted in the final multivariable predictive model
Park, bar or night/dance club, public bathroom, fitness center/gym, public restroom, college dormitory, beach, woods, street, theater, public transportation, hotel and private homes
Comparison of High-Risk Behaviors
Compared to MSM having sexual debut with a man (Table 3), those having sexual debut with a woman were more likely to have recent (in the past 3 months) hazardous alcohol drinking (21.2% vs. 11.6%; χ2 = 56.13; p < 0.001), have recent binge drinking (21.4% vs. 14.9%; χ2 = 22.69; p < 0.001), have recent alcohol drinking before sex (26.3% vs. 18.2%; χ2 = 29.70; p < 0.001), practice exclusively insertive anal sex roles (41.6% vs. 29.9%; χ2 = 115.17; p < 0.001), have recent insertive (69.5% vs. 56.9%; χ2 = 49.61; p < 0.001) or condomless insertive anal sex (27.9% vs. 19.5%; χ2 = 30.90; p < 0.001), have recent sex (26.1% vs. 4.1%; χ2 = 383.58; p < 0.001) or condomless vaginal sex (15.9% vs. 2.8%; χ2 = 208.09; p < 0.001) with women, have been sexually active for ≥7 years (67.6% vs. 41.2%; χ2 = 207.86; p < 0.001), and have ≥2 lifetime female sexual partners (45.2% vs. 5.1%; χ2 = 852.63; p < 0.001). Conversely, MSM having sexual debuts with men were more likely to recently use illicit drugs (29.9% vs. 21.9%; χ2 = 23.59; p < 0.001), have recent receptive sex with men (56.4% vs. 42.3%; χ2 = 59.16; p < 0.001) or condomless receptive anal sex (21.5% vs. 17.7%; χ2 = 6.73; p = 0.009) with men, and have ≥10 lifetime male sexual partners (52.4% vs. 42.2%; χ2 = 30.99; p < 0.001).
Table 3.
Comparison of high-risk behaviors between Chinese MSM who had sexual debut with a male versus female sexual partner (N = 3588)
| High-risk behaviors | Total N = 3588 n (%) | Sexual debut |
χ2 statistics | p-value | |
|---|---|---|---|---|---|
| With a man N = 2538 n (%) | With a woman N = 1050 n (%) | ||||
| Had hazardous alcohol drinking in the past 3 months (AUDIT-C score ≥4) | 56.129 | <0.001 | |||
| No | 3071 (85.6) | 2244 (88.4) | 827 (78.8) | ||
| Yes | 517 (14.4) | 294 (11.6) | 223 (21.2) | ||
| Had binge drinking in the past 3 months† | 22.686 | <0.001 | |||
| No | 2985 (83.2) | 2160 (85.1) | 825 (78.6) | ||
| Yes | 603 (16.8) | 378 (14.9) | 225 (21.4) | ||
| Alcohol drinking before sex in the past 3 months | 29.697 | <0.001 | |||
| No | 2850 (79.4) | 2076 (81.8) | 774 (73.7) | ||
| Yes | 738 (20.6) | 462 (18.2) | 276 (26.3) | ||
| Drug use in the past 3 months | 23.592 | <0.001 | |||
| No | 2600 (72.5) | 1780 (70.1) | 820 (78.1) | ||
| Yes | 988 (27.5) | 758 (29.9) | 230 (21.9) | ||
| Predominant anal role* | 115.169 | <0.001 | |||
| Exclusively insertive | 1131 (33.3) | 723 (29.9) | 408 (41.6) | ||
| Versatile | 1434 (42.2) | 982 (40.7) | 452 (46.0) | ||
| Exclusively receptive | 832 (24.5) | 710 (29.4) | 122 (12.4) | ||
| Had insertive anal sex with men in the past 3 months | 49.606 | <0.001 | |||
| No | 1414 (39.4) | 1094 (43.1) | 320 (30.5) | ||
| Yes | 2174 (60.6) | 1444 (56.9) | 730 (69.5) | ||
| Had condomless insertive anal sex with men in the past 3 months | 30.903 | <0.001 | |||
| No | 2801 (78.1) | 2044 (80.5) | 757 (72.1) | ||
| Yes | 787 (21.9) | 494 (19.5) | 293 (27.9) | ||
| Had receptive anal sex with men in the past 3 months | 59.162 | <0.001 | |||
| No | 1713 (47.7) | 1107 (43.6) | 606 (57.7) | ||
| Yes | 1875 (52.3) | 1431 (56.4) | 444 (42.3) | ||
| Had condomless receptive anal sex with men in the past 3 months | 6.731 | 0.009 | |||
| No | 2855 (79.6) | 1991 (78.5) | 864 (82.3) | ||
| Yes | 733 (20.4) | 547 (21.5) | 186 (17.7) | ||
| Had anal sex with HIV-infected men in the past 3 months | 0.199 | 0.655 | |||
| No | 3946 (97.4) | 2471 (97.4) | 1025 (97.6) | ||
| Yes | 92 (2.6) | 67 (2.6) | 25 (2.4) | ||
| Buying sex from male commercial sex worker in the past 3 months | 1.115 | 0.291 | |||
| No | 3488 (97.2) | 2472 (97.4) | 1016 (96.8) | ||
| Yes | 100 (2.3) | 66 (2.6) | 34 (3.2) | ||
| Had sex with women in the past 3 months | 383.578 | <0.001 | |||
| No | 3211 (89.5) | 2435 (95.9) | 776 (73.9) | ||
| Yes | 377 (10.5) | 103 (4.1) | 274 (26.1) | ||
| Had condomless vaginal sex with women in the past 3 months | 208.086 | <0.001 | |||
| No | 3351 (93.4) | 2468 (97.2) | 883 (84.1) | ||
| Yes | 237 (6.6) | 70 (2.8) | 167 (15.9) | ||
| Year of sexual activity | 207.863 | <0.001 | |||
| <7 | 1833 (51.1) | 1493 (58.8) | 340 (32.4) | ||
| ≥7 | 1755 (48.9) | 1045 (41.2) | 710 (67.6) | ||
| Lifetime number of male sexual partners | 30.992 | <0.001 | |||
| <10 | 1815 (50.6) | 1208 (47.6) | 607 (57.8) | ||
| ≤10 | 1773 (49.4) | 1330 (52.4) | 443 (42.2) | ||
| Lifetime number of female sexual partners | 852.627 | <0.001 | |||
| ≤1 | 2983 (83.1) | 2408 (94.9) | 575 (54.8) | ||
| ≥2 | 605 (16.9) | 130 (5.1) | 475 (45.2) | ||
| Ever tested for HIV | 0.475 | 0.491 | |||
| No | 1054 (29.4) | 737 (29.0) | 317 (30.2) | ||
| Yes | 2534 (70.6) | 1801 (71.0) | 733 (69.8) | ||
AUDIT-C alcohol use disorders identification test
Sample size reduces to 3397 due to 191 participants self-reported no anal sex with men in the past 3 months
Having 6 or more standard drinks on one occasion; a standard drink is defined as any drink that contains about 10 grams of pure alcohol [50 ml of spirits; or 40 ml (one small cup) of rice wine; or one can of beer; or 140 ml (one cup) of red wine]
Table 4 presents the associations of sex of first partner with the odds of attaining a higher frequency category of risky sex/partnership, stratified by their age of sexual debuts. Men who had sexual debut with a man at early age (≤18 years) had the highest odds (vs. 19–22 and ≥23 years) of having a higher total number of lifetime male sexual partners (AOR: 2.38; 95% CI 1.74–3.25; ptrend < 0.001), a greater number of recent receptive sexual encounters (AOR: 1.82; 95% CI 1.36–2.43; ptrend < 0.001), and condomless receptive anal sexual encounters (AOR: 1.68; 95% CI 1.05–2.69; ptrend < 0.001) with men. Men who had their sexual debut with a woman at an early age (≤18 years) had the highest odds (vs. 19–22 and ≥23 years) of having had a higher frequency of total number of recent insertive sexual encounters (AOR: 1.99; 95% CI 1.52–2.61; ptrend < 0.001) or condomless insertive anal sexual encounters (AOR: 2.32; 95% CI 1.67–3.23; ptrend = 0.03) with men, total lifetime female sexual partners (AOR: 66.35; 95% CI 43.08–102.22; ptrend = 0.04), and total number of recent vaginal sexual encounters (AOR: 5.90; 95% CI 3.61–9.64; ptrend = 0.21) or condomless vaginal sexual encounters (AOR: 3.68; 95% CI 1.58 –8.58; ptrend = 0.75) with women.
Table 4.
Multivariable ordinal logistic regression of association between sex of first sexual partner and high-risk behaviors among Chinese men who have sex with men (N = 3588)
| Partner’s gender at sexual debut | Age of sexual debut |
p for trend | |||||
|---|---|---|---|---|---|---|---|
| ≤18 years, age |
19–22 years, age |
≥23 year, age |
|||||
| AOR† (95% CI) |
p- value |
AOR† (95% CI) |
p- value |
AOR† (95% CI) | p-value | ||
| Total number of lifetime male sexual partnersa | |||||||
| With a woman | Reference | Reference | Reference | ||||
| With a man | 2.38 (1.74, 3.25) | <0.001 | 2.28 (1.83, 2.85) | <0.001 | 1.85 (1.39, 2.45) | <0.001 | <0.001 |
| Total number of receptive anal sex with men in the past 3 monthsb | |||||||
| With a woman | Reference | Reference | Reference | ||||
| With a man | 1.82 (1.36, 2.43) | <0.001 | 1.54 (1.23, 1.94) | <0.001 | 1.64 (1.18, 2.28) | 0.003 | <0.001 |
| Total number of condomless receptive anal sex with men in the past 3 monthsc | |||||||
| With a woman | Reference | Reference | Reference | ||||
| With a man | 1.68 (1.05, 2.69) | 0.03 | 1.28 (0.94, 1.73) | 0.112 | 1.04 (0.73, 1.49) | 0.817 | <0.001 |
| Total number of insertive anal sex with men in the past 3 monthsd | |||||||
| With a man | Reference | Reference | Reference | ||||
| With a woman | 1.99 (1.52, 2.61) | <0.001 | 1.46 (1.19, 1.82) | <0.001 | 1.22 (0.91, 1.65) | 0.186 | <0.001 |
| Total number of condomless insertive anal sex with men in the past 3 monthse | |||||||
| With a man | Reference | Reference | Reference | ||||
| With a woman | 2.32 (1.67, 3.23) | <0.001 | 1.41 (1.07, 1.86) | 0.015 | 1.05 (0.71, 1.55) | 0.801 | 0.031 |
| Total number of lifetime female sexual partnersf | |||||||
| With a man | Reference | Reference | Reference | ||||
| With a woman | 66.35 (43.08, 102.22) | <0.001 | 31.31 (23.29,42.09) | <0.001 | 30.06 (19.66,45.97) | <0.001 | 0.042 |
| Total number of vaginal sex with women in the past 3 monthsg | |||||||
| With a man | Reference | Reference | Reference | ||||
| With a woman | 5.90 (3.61,9.64) | <0.001 | 3.71 (2.43, 5.66) | <0.001 | 3.84 (2.11, 6.99) | <0.001 | 0.211 |
| Total number of condomless vaginal sex with women in the past 3 monthsh | |||||||
| With a man | Reference | Reference | Reference | ||||
| With a woman | 3.68 (1.58, 8.58) | 0.002 | 2.44 (1.48, 4.03) | <0.001 | 2.94 (1.65, 5.24) | <0.001 | 0.747 |
Odds ratios represent the odds of attaining a higher category of the specific high-risk behavior outcome; p for trend denotes the trend of attaining higher frequency category of the specific high-risk behaviors across increased order of age groups
Category (number of lifetime male sexual partners): 1–4, 5–9, 10–19, ≥20
Category (Total number of receptive anal sex with men in the past 3 months): 0, 1, 2, ≥3
Category (Total number of condomless receptive anal sex with men in the past 3 months): 0, 1, 2, ≥3
Category (Total number of insertive anal sex with men in the past 3 months): 0, 1–2, 3–4, ≥5
Category (Total number of condomless insertive anal sex with men in the past 3 months): 0, 1, 2, ≥3
Category (Total number of lifetime female sexual partners): 0, 1, ≥2
Category (Total number of vaginal sex with women in the past 3 months): 0, 1–2, ≥3
Category (Total number of condomless vaginal sex with women in the past 3 months): 0, 1–2, ≥3
Predicted Probability of HIV and Syphilis
Figure 1a shows a non-linear relationship between the age of sexual debut and the predicted probability of being diagnosed positive with HIV, stratified by sex of first partner. The probability of HIV infection was slightly higher among men having sexual debut with a man than those with a woman across all ages of sexual debut. The older the age of sexual debut, the lower the probability of HIV infection, with this association being even more dramatic when age of sexual debut was >22 years.
Fig. 1.
a Predicted probability of HIV infection by age of sexual debut among men who have sex with men in Beijing, China (N = 3588). b Predicted probability of syphilis infection by age of sexual debut among men who have sex with men in Beijing, China (N = 3588)
In contrast, the predicted probability of being diagnosed positive with syphilis was higher among men having sexual debut with a woman than those with a man (Fig. 1b). A stronger negative relationship between the probability of syphilis and age of sexual debut ≤22 years was seen among both groups, with a nadir of risk noted at sexual debut at age 22 years, but then there was a gradual increase in risk with later year of sexual debut.
Discussion
We found that men having sexual debut with a woman were more likely to predominantly practice an insertive anal role, have more lifetime female sex partners, have more recent condomless insertive anal sex with men, and have more recent condomless vaginal sex with women. Conversely, men having their first sex with a man were more likely to take a receptive anal role, report more lifetime male sex partners, and have had more recent condomless receptive anal sex with a man. Regardless of sex of first partner, we also found that earlier age of sexual debut was associated with an increased likelihood of having more frequent condomless sex, having more lifetime sexual partners and being infected with HIV or syphilis. Our observation of the associations between earlier age of sexual debut and later risky sexual behaviors are consistent with other studies among both MSM and general populations [19, 21, 27, 28].
A person’s first sexual intercourse experience may have possible effects on sexual attitude, belief, subsequent sexual preference, development and adjustment [29]. The self-labeling and anal sex role preference is an important identity among both MSM and MSMW; early patterns and preferences may be influenced by early partner characteristics (e.g., first sexual encounter with a male or a female), and be associated with psychosexual preferences of specific male-to-male anal sex roles, influencing different HIV/STI risk exposures (e.g., receptive anal sex riskier than insertive) [30–32]. Complex prospective studies of youth and young adults would be needed to assess whether the sex of the first partner has a predisposing influence on subsequent sexual positioning and practice preference, or in turn, whether this choice merely reflects these early preferences without influencing them. Qualitative assessments would be essential components of such studies, and even then a “chicken and egg” element would be hard to tease out.
In this study, 39.6% of our Beijing MSM reported ever having sex with a woman, higher than the findings from recent meta-analyses among both Chinese MSM (31.2%) and Asian MSM (32.8%) [12, 13]. Studies in the U.S. also reported high prevalence of bisexuality, particularly among black MSM [33, 34]. As the capital of China, Beijing attracts migrants, including MSM, for better employment opportunity and living condition [35]. Previous studies have shown a higher marriage rate among migrant MSM than local MSM [11, 36], explaining why higher prevalence of bisexual behaviors is seen in our study, as well as other Beijing studies (45.6–46.2%) [25, 37, 38].
We found that a high proportion of Chinese MSM had their sexual debuts with women (29.6%), while Mao et al. reported this at 41.3% [39]. Among this subgroup, 37% eventually married a woman (compared to 6.0% among men who had their sexual debuts with men; p < 0.001), and 87% were migrants. In western countries, the prevalence of MSM marrying a woman is lower than in China, below 6% [40–42]. This might due to the existence of more open social/family norms and cultural acceptability towards homosexuality. In China, as in other culturally conservative countries, MSM may experience family/social isolation once they are discovered to be homosexual, especially MSM originated from rural/village areas [11]. These geographical and cultural constructs may influence some MSM to use marriage as a disguise [9]. These men may endure pressures of gay-related stigma, fear of sexual orientation disclosure, as well as carrying a heavy responsibility to support their families [16]. These pressures may partially explain our finding of a higher likelihood of hazardous or binge drinking problems among this subgroup [43]. Older MSM were more likely to have sexual debut with a woman, perhaps reflecting the birth cohort effect that those were born before the mid-1970s in China who were exposed to more conservative cultural values. Initiating sex with a man was a stronger past taboo than it is at present. Similar to our findings, a 7-city Chinese study conducted from 2008 to 2009 suggested that older MSM were more likely to be married and to practice condomless vaginal intercourse [44]. It is a challenging, high priority public health intervention to help married MSM who do not use condoms with their wives to use condoms, both with their typically clandestine male partners and with their wives [11].
Men having their sexual debut with a man were more likely to practice condomless receptive or condomless receptive intercourse with men and also to have more male sexual partners. These biologically and epidemiologically established high risk behaviors are suggested to be associated with increased risk of HIV, supporting our findings that men who had their first sex with a man showing higher predicted probability of HIV, confirmed with our sero-diagnostics. In contrast, men having their first sex with a woman presents higher predicted probability of syphilis across all ages of sexual debut. Compared to MSM having first sex with a man, these subgroups were more likely to seek sex via non-Internet venues and have increased recent or lifetime female sex partners, which might include syphilis-at-risk female sex workers, increasing their exposure to contract syphilis through unprotected virginal sex [24, 45, 46].
Strengths of our study include the exploration of the association of sex of first partner on sexual and HIV/ syphilis risk among a large community-based sample of Chinese MSM, and the application of rigorous multivariable modeling as well as restricted cubic spline methods. We think that recall of the sex of a first lifetime sexual partner and age of sexual debut are less biases than for less memorable life experiences. Limitations include our lack of an Audio Computer-Assisted Self-Interview which might have reduced social desirability bias in our sensitive questions regarding sexual and substance use behaviors. Second, the study was conducted among a convenient sample of Beijing MSM and the findings may have limited generalizability to other settings. Third, the cross-sectional nature of the study may not infer causality. Finally, we were limited in assessing detailed partner characteristics at sexual debut and possible intermediate psychological constructs that may further elucidate the mechanism underlying the observed associations.
Bisexual behavior is common among Chinese MSM, exacerbating the spread of HIV to lower-risk persons. The sex of one’s first partner and the exact age of sexual debut may both play a role in shaping subsequent risky sexual behaviors among Chinese MSM. Patterns differed for HIV versus syphilis risk, reminding us that risk assessments for one STI is not necessarily a strong surrogate for another. Further exploration of the social, psychological, and behavioral contexts of early sexual experiences and latter STI risks can help design of targeted risk reduction programs among Chinese MSM.
Acknowledgements
This research was supported by the National Institute of Allergy and Infectious Diseases of the National Institutes of Health under Award Numbers R01AI094562 and R34AI091446, and National Natural Science Foundation of China (11471336). We thank volunteers from Chaoyang Chinese AIDS Volunteer Group, staff from Xicheng and Chaoyang District Center for Disease Control and Prevention, for their assistance in recruiting the participants, collecting data, and conducting focus group discussions.
Footnotes
Compliance with Ethical Standards
Conflict of interest The authors declare that they have no conflict of interest.
Ethical Approval All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent Informed consent was obtained from all individual participants included in the study.
References
- 1.Jia Z, Huang X, Wu H, et al. HIV burden in men who have sex with men: a prospective cohort study 2007-2012. Sci Rep. 2015;5:11205. doi: 10.1038/srep11205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zhang W, Xu JJ, Zou H, Zhang J, Wang N, Shang H. HIV incidence and associated risk factors in men who have sex with men in Mainland China: an updated systematic review and meta-analysis. Sex Health. 2016 doi: 10.1071/SH16001. doi:10.1071/SH16001. [DOI] [PubMed] [Google Scholar]
- 3.State Council AIDS Working Committee Office (SCAWCO): China 2015 UNGASS Country Progress Report, Beijing. http://www.unaids.org/sites/default/files/country/documents/CHN_narrative_report_2015.pdf.
- 4.Liu Y, Osborn CY, Qian HZ, et al. Barriers and facilitators of linkage to and engagement in HIV care among HIV-positive men who have sex with men in China: a qualitative study. AIDS Patient Care STDS. 2016;30(2):70–7. doi: 10.1089/apc.2015.0296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Liu Y, Sun X, Qian HZ, et al. Qualitative assessment of barriers and facilitators of access to HIV testing among men who have sex with men in China. AIDS Patient Care STDS. 2015;29(9):481–9. doi: 10.1089/apc.2015.0083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wei C, Yan H, Yang C, et al. Accessing HIV testing and treatment among men who have sex with men in China: a qualitative study. AIDS Care. 2014;26(3):372–8. doi: 10.1080/09540121.2013.824538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Choi KH, Hudes ES, Steward WT. Social discrimination, concurrent sexual partnerships, and HIV risk among men who have sex with men in Shanghai, China. AIDS Behav. 2008;12(4 Suppl):S71–7. doi: 10.1007/s10461-008-9394-0. [DOI] [PubMed] [Google Scholar]
- 8.Liao M, Kang D, Tao X, et al. Alcohol use, stigmatizing/discriminatory attitudes, and HIV high-risk sexual behaviors among men who have sex with men in China. Biomed Res Int. 2014;2014:143738. doi: 10.1155/2014/143738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Steward WT, Miege P, Choi KH. Charting a moral life: the influence of stigma and filial duties on marital decisions among Chinese men who have sex with men. PLoS ONE. 2013;8(8):e71778. doi: 10.1371/journal.pone.0071778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wang S, Song D, Huang W, et al. Heterosexual partnerships and the need for HIV prevention and testing for men who have sex with men and women in China: a qualitative study. AIDS Educ Prev. 2015;27(2):126–38. doi: 10.1521/aeap.2015.27.2.126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Liu Y, Li D, Vermund SH, et al. Associations of current marital status and living arrangements with HIV and syphilis risk: findings from a community-based sample of men who have sex with men in China. AIDS Care. 2016;28:1–6. doi: 10.1080/09540121.2016.1189502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bowring AL, Veronese V, Doyle JS, Stoove M, Hellard M. HIV and sexual risk among men who have sex with men and women in Asia: a systematic review and meta-analysis. AIDS Behav. 2016;20(10):2243–65. doi: 10.1007/s10461-015-1281-x. [DOI] [PubMed] [Google Scholar]
- 13.Yun K, Xu JJ, Reilly KH, et al. Prevalence of bisexual behaviour among bridge population of men who have sex with men in China: a meta-analysis of observational studies. Sex Transm Infect. 2011;87(7):563–70. doi: 10.1136/sextrans-2011-050079. [DOI] [PubMed] [Google Scholar]
- 14.Wang HY, Xu JJ, Zou HC, et al. Sexual risk behaviors and HIV infection among men who have sex with men and women in China: evidence from a systematic review and meta-analysis. Biomed Res Int. 2015;2015:850132. doi: 10.1155/2015/850132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wu Z, Xu J, Liu E, et al. HIV and syphilis prevalence among men who have sex with men: a cross-sectional survey of 61 cities in China. Clin Infect Dis. 2013;57(2):298–309. doi: 10.1093/cid/cit210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chen JP, Han MM, Liao ZJ, et al. HIV-related behaviors, social support and health-related quality of life among men who have sex with men and women (MSMW): a cross-sectional study in Chongqing, China. PLoS ONE. 2015;10(2):e0118651. doi: 10.1371/journal.pone.0118651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cai R, Zhao J, Cai W, Chen L, Richardus JH, de Vlas SJ. HIV risk and prevention behaviors in men who have sex with men and women: a respondent-driven sampling study in Shenzhen, China. AIDS Behav. 2014;18(8):1560–8. doi: 10.1007/s10461-014-0735-x. [DOI] [PubMed] [Google Scholar]
- 18.He Q, Wang Y, Lin P, et al. Potential bridges for HIV infection to men who have sex with men in Guangzhou, China. AIDS Behav. 2006;10(4 Suppl):S17–23. doi: 10.1007/s10461-006-9125-3. [DOI] [PubMed] [Google Scholar]
- 19.Outlaw AY, Phillips G, 2nd, Hightow-Weidman LB, et al. Age of MSM sexual debut and risk factors: results from a multisite study of racial/ethnic minority YMSM living with HIV. AIDS Patient Care STDS. 2011;25(Suppl 1):S23–9. doi: 10.1089/apc.2011.9879. [DOI] [PubMed] [Google Scholar]
- 20.Shrestha R, Karki P, Copenhaver M. Early sexual debut: a risk factor for STIs/HIV acquisition among a nationally representative sample of adults in Nepal. J Community Health. 2016;41(1):70–7. doi: 10.1007/s10900-015-0065-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Nelson KM, Gamarel KE, Pantalone DW, Carey MP, Simoni JM. Sexual debut and HIV-related sexual risk-taking by birth cohort among men who have sex with men in the United States. AIDS Behav. 2016;20(10):2286–95. doi: 10.1007/s10461-016-1330-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Coburn BJ, Blower S. A major HIV risk factor for young men who have sex with men is sex with older partners. J Acquir Immune Defic Syndr. 2010;54(2):113–4. doi: 10.1097/QAI.0b013e3181d43999. [DOI] [PubMed] [Google Scholar]
- 23.Liu Y, Qian HZ, Ruan Y, et al. Frequent HIV testing: impact on HIV risk among Chinese men who have sex with men. J Acquir Immune Defic Syndr. 2016;72(4):452–61. doi: 10.1097/QAI.0000000000001001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Liu Y, Wang J, Qian HZ, et al. Seeking male sexual partners via internet and traditional venues among Chinese men who have sex with men: implications for HIV risk reduction interventions. AIDS Behav. 2016 doi: 10.1007/s10461-016-1371-4. doi:10.1007/s10461-016-1371-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lu H, Han Y, He X, et al. Alcohol use and HIV risk taking among Chinese MSM in Beijing. Drug Alcohol Depend. 2013;133(2):317–23. doi: 10.1016/j.drugalcdep.2013.06.013. [DOI] [PubMed] [Google Scholar]
- 26.Zhang H, Teng T, Lu H, et al. Poppers use and risky sexual behaviors among men who have sex with men in Beijing, China. Drug Alcohol Depend. 2016;160:42–8. doi: 10.1016/j.drugalcdep.2015.11.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Baldwin P, Shrestha R, Potrepka J, Copenhaver M. The age of initiation of drug use and sexual behavior may influence subsequent HIV risk behavior: a systematic review. ISRN AIDS. 2013;2013:976035. doi: 10.1155/2013/976035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wang N, Wu G, Lu R, et al. Investigating HIV infection and HIV incidence among Chinese men who have sex with men with recent sexual debut, Chongqing, China, 2011. AIDS Behav. 2016;20(12):2976–82. doi: 10.1007/s10461-016-1356-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Reissing ED, Andruff HL, Wentland JJ. Looking back: the experience of first sexual intercourse and current sexual adjustment in young heterosexual adults. J Sex Res. 2012;49(1):27–35. doi: 10.1080/00224499.2010.538951. [DOI] [PubMed] [Google Scholar]
- 30.Dangerfield DT, 2nd, Smith LR, Williams J, Unger J, Bluthenthal R. Sexual positioning among men who have sex with men: a narrative review. Arch Sex Behav. 2016 doi: 10.1007/s10508-016-0738-y. doi:10.1007/s10508-016-0738-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wei C, Raymond HF. Preference for and maintenance of anal sex roles among men who have sex with men: sociodemographic and behavioral correlates. Arch Sex Behav. 2011;40(4):829–34. doi: 10.1007/s10508-010-9623-2. [DOI] [PubMed] [Google Scholar]
- 32.Zhou C, Raymond HF, Ding X, et al. Anal sex role, circumcision status, and HIV infection among men who have sex with men in Chongqing, China. Arch Sex Behav. 2013;42(7):1275–83. doi: 10.1007/s10508-012-0008-6. [DOI] [PubMed] [Google Scholar]
- 33.Asare Bempong G, Ramamurthi HC, McCuller J, Williams JK, Harawa NT. Recruiting black men who have sex with men and women (BMSMW) in an urban setting for HIV prevention research. J AIDS Clin Res. 2014 doi: 10.4172/2155-6113.1000408. doi:10.4172/2155-6113. 1000408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ellen JM, Greenberg L, Willard N, Stines S, Korelitz J, Boyer CB. Cross-sectional survey comparing HIV risk behaviours of adolescent and young adult men who have sex with men only and men who have sex with men and women in the U.S. and Puerto Rico. Sex Transm Infect. 2015;91(6):458–61. doi: 10.1136/sextrans-2014-051712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Guo Y, Li X, Song Y, Liu Y. Bisexual behavior among Chinese young migrant men who have sex with men: implications for HIV prevention and intervention. AIDS Care. 2012;24(4):451–8. doi: 10.1080/09540121.2011.613914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Liu Y, Li X, Zhang L, Li S, Jiang S, Stanton B. Correlates of consistent condom use among young migrant men who have sex with men (MSM) in Beijing, China. Eur J Contracept Reprod Health Care. 2012;17(3):219–28. doi: 10.3109/13625187.2012.662544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Tao J, Ruan Y, Yin L, et al. Sex with women among men who have sex with men in China: prevalence and sexual practices. AIDS Patient Care STDS. 2013;27(9):524–8. doi: 10.1089/apc.2013.0161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Qian HZ, Ruan Y, Liu Y, et al. Lower HIV risk among circumcised men who have sex with men in China: interaction with anal sex role in a cross-sectional study. J Acquir Immune Defic Syndr. 2016;71(4):444–51. doi: 10.1097/QAI.0000000000000856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Mao H, Ma W, Lu H, et al. High incidence of HIV and syphilis among migrant men who have sex with men in Beijing, China: a prospective cohort study. BMJ Open. 2014;4(9):e005351. doi: 10.1136/bmjopen-2014-005351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Weinhardt LS, Kelly JA, Brondino MJ, et al. HIV transmission risk behavior among men and women living with HIV in 4 cities in the United States. J Acquir Immune Defic Syndr. 2004;36(5):1057–66. doi: 10.1097/00126334-200408150-00009. [DOI] [PubMed] [Google Scholar]
- 41.Jeffries WLT. Sociodemographic, sexual, and HIV and other sexually transmitted disease risk profiles of nonhomosexual-identified men who have sex with men. Am J Public Health. 2009;99(6):1042–5. doi: 10.2105/AJPH.2007.125674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Yang HT, Tang W, Xiao ZP, et al. Worsening epidemic of HIV and syphilis among men who have sex with men in Jiangsu Province, China. Clin Infect Dis. 2014;58(12):1753–9. doi: 10.1093/cid/ciu175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Fan W, Lu R, Wu G, et al. Alcohol drinking and HIV-related risk among men who have sex with men in Chongqing, China. Alcohol. 2016;50:1–7. doi: 10.1016/j.alcohol.2015.09.004. [DOI] [PubMed] [Google Scholar]
- 44.Shen H, Tang S, Mahapatra T, et al. Condomless vaginal inter-course and its associates among men who have sex with men in China. PLoS ONE. 2016;11(4):e0154132. doi: 10.1371/journal.pone.0154132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Zheng C, Xu JJ, Hu QH, et al. Commercial sex and risk of HIV, syphilis, and herpes simplex virus-2 among men who have sex with men in six Chinese cities. BMC Infect Dis. 2016;16(1):765. doi: 10.1186/s12879-016-2130-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Tang S, Tang W, Meyers K, Chan P, Chen Z, Tucker JD. HIV and syphilis among men who have sex with men and transgender individuals in China: a scoping review. Lancet. 2016;388(Suppl 1):S74. doi: 10.1186/s12879-016-1904-5. [DOI] [PMC free article] [PubMed] [Google Scholar]