Abstract
Little work has examined how individuals’ social affiliations-- the venues in which they meet friends and engage in informal social interaction– influence their engagement with public health services. We investigate how links to these local places shape access to information and exposure to health-seeking behavior. Using longitudinal data from a respondent-driven sample of 618 young black men who have sex with men (YBMSM) in Chicago, we identify different sets of social venues that connect YBMSM. We then examine how YBMSM’s connections within this network influence their receipt of HIV prevention and treatment services and knowledge of pre-exposure prophylaxis (PrEP). Our results show that YBMSM’s positions within Chicago’s venue network shape the types of health-related services they access, net of demographic, structural, and community covariates. Men with affiliations that are linked to the city’s gay enclave are most likely to know about PrEP, while men with affiliations that are predominately in the black community demonstrate improved HIV treatment outcomes. Outreach engaging MSM beyond venues in gay enclaves is needed.
Keywords: social networks, public health, HIV, minority health, affiliations, health disparities, neighborhoods, men who have sex with men
1. INTRODUCTION
Young black men who have sex with men (MSM) are at particularly high risk for HIV infection in the United States, and current estimates predict that 1 in 2 black MSM will be diagnosed with HIV in his lifetime, compared to 1 in 11 white MSM.1 Recent research suggests that Black MSM’s higher rates of HIV infection are due to a combination of increased exposure to HIV risk and diminished access to HIV care, rather than differences in risky sexual behavior.2 In predicting access to HIV services, extant research has pointed to issues related to spatial availability (e.g., distance to service providers), structural barriers (e.g., poverty, unemployment) and social “resiliency” or support-related factors.3–5 Greater healthcare access and utilization are associated with better health outcomes for HIV (sero)positive individuals, including lower viral load 6 and lower likelihood of transmission to HIV-negative sex partners.7 However, compared to white MSM, black MSM are less likely to be aware that they are HIV seropositive, and also have less access to the health care resources that are needed to achieve viral suppression.2 To this end, black MSM are also more likely to be diagnosed in the later stages of HIV8 and are less likely to be taking anti-retroviral medications.9,10
These trends underscore the urgent need to understand black MSM’s access to and engagement with the public health system. We advance research on the role local community venues play for HIV transmission11,12 by examining how the informal social institutions in which MSM spend their time in everyday life influence their public health engagement. Informal social institutions and venues – such as schools, cafes, and bars – are key sites of social interaction, support, and informal social control.13,14 These are also places where MSM socialize and meet their friends and sex partners and, as we argue in this paper, are incidentally exposed to information about important public health services, such as testing opportunites.15–17
It is partly in recognition of the important role that is played by informal social networks that non-clinical venues – such as parks, bars, and other community spaces – have become a focus of community-based HIV outreach efforts.18–20 Previous research has leveraged the importance of social and sexual venues to track the flow of infectious diseases21,22 and research on the HIV epidemic in the United States has identified commercial sex venues (e.g., bathhouses) as ongoing risk environments for transmission.23,24 This work underscores that venues represent important sites to reduce risk among vulnerable populations, such as minority MSM who may be otherwise difficult to test and recruit into HIV prevention and treatment programs.25–27 However, there has been limited research on how at-risk individuals’ informal affiliations with such venues shape their receipt of HIV-related health services. It is possible that individuals’ healthcare knowledge and behavior are affected by the patterns of informal social connections they have with these community institutions-- net of their geographic locations, their formal connections to clinics, and their other network ties.
In this particular context, an analysis of MSM’s informal and indirect affiliations to each other via community venues may provide important insight into how local spaces influence access to and utilization of health services. Affiliation network analysis is frequently utilized to examine how individuals are tied to social events and venues.11,13,28 Recent analyses have documented how the set of recreational venues MSM visit influences their sexual behavior29 and the substantial correlation that exists between black MSM’s HIV status and the clinics they visit for healthcare.30 These studies emphasize the important role that local social affiliations play in shaping at-risk individuals’ exposure to sexual environments and access to HIV services. Our analysis extends this work by exploring the role of social affiliations with local venues for the utilization of HIV services and HIV treatment outcomes. Utilizing new longitudinal data from UConnect (2013–2016), a respondent-driven sample of 618 young, black MSM in Chicago, we examine how young black MSMs’ informal social affiliations are related to their receipt of HIV-related public health services, including receipt of treatment and prevention services and knowledge of pre-exposure prophylaxis (PrEP).31,32
2. METHODS
Between June 2013 and May 2014, 618 young black MSM in Chicago were recruited into the UConnect study using respondent driven sampling (RDS).33 RDS chains of up to 13 waves in length, with a mean of 2.3 recruits per participant, were generated by a diverse group of seeds. We provide additional detail on seed recruitment in Appendix A. Respondents were eligible for the study if they identified as black or African American, were born male, were between 16 and 29 years old inclusive, reported at least one male sex partner within the last 24 months, resided or spent most of their time in the Black community area, and gave informed consent at the time of the interview. Wave 2, administered 9 months later in 2014–2015, had an 84% retention rate, with 525 of the original respondents completing the Wave 2 survey. IRB approval from the University of Chicago and National Opinion Research Center was granted prior to data collection in 2013.
2.1. Venue affiliation network position
The key variable in this analysis is the respondent’s position within a network of local social venues in Chicago. Individuals are usually affiliated with multiple types of venues (e.g., bars), that link them to overlapping sets of MSM. The assumption we test here is that individuals who have similar (overlapping) affiliations also have similar exposures to healthcare information because they spend time in similar venue environments that contain similar sets of men, who themselves can serve as important sources of information about healthcare resources. Little work has investigated which types of venue affiliations are the most salient for young black MSM’s access to health services. Therefore, one of our first tasks is to understand the topology of affiliations within black MSM communities. We then investigate how these classes of affiliations are tied to health service utilization.
We begin with a set of questions that asked respondents (at the baseline interview) where they had gone in Chicago to “meet or socialize with other men” during the last 12 months. Respondents were asked if they frequented each of the following venues types: 1) bars and clubs, 2) gyms, 3) “public spaces” (e.g., parks, shopping malls), 4) bath houses or bookstores, and/or 5) House/Ball events. If the respondent answered affirmatively and indicated that he goes to the venue type at least once per year, he was then asked to identify whether the venues were located on the North Side, South Side, and/or West Side of Chicago. The North Side of Chicago is predominately composed of white residents and houses the city’s gay enclave (“Boystown”), while the South Side of Chicago is home to the largest contiguous black community in the U.S. and contains a high concentration of underserved neighborhoods.34,35 The West Side of Chicago is ethnically mixed and contains adjacent concentrated black and Latino/a neighborhoods. A given respondent could indicate multiple regions per venue type (e.g., clubs on both the North Side and South Side) and was coded as being tied to a space if he indicated during the interview that it was a place he visited to meet other men.
Based on the combination of general venue types and geographic regions, we then identify 15 regional venue types (e.g., “Black Community” gyms, “Gay Enclave” bars), and construct a m x n matrix of 481 respondents who provided valid affiliations (m) and their affiliations with the 15 (n) venue-region spaces. To identify the respondent’s position within the city’s venue affiliation network, we transform the two-mode respondent-to-venue network into a one-mode respondent-to-respondent network using UCINET.36 We weight the ties connecting respondents to venues by Bonacich’s (1972) normalization rule to adjust for differential levels of venue attendance across respondents, such that individuals who overlap in a greater proportion of their venue affiliations are weighted as more strongly tied to one another. The resulting one-mode projection yields a m x m matrix wherein each cell contains the degree of overlapping affiliations a respondent shares with each of the other respondents. We then submit this matrix to a hierarchical cluster analysis in Stata 13 using Ward’s linkage criteria to identify distinct groups of MSM with similar affiliation patterns.37 Visual assessment of the dendrogram in combination with goodness of fit tests (Calinski–Harabasz pseudo-F and Duda-Hart statistics) suggest that a three-cluster solution is the strongest, most parsimonious representation of venue affiliation patterns. Supplemental analyses (available upon request) demonstrate that the clusters that are identified here do not depend on our use of Wards linkage or other clustering criteria.
2.2. HIV-related public health engagement
Our main interest is in how MSM’s venue affiliations are associated with their patterns of public health service engagement. To examine this, we consider several different measures.
Receipt of HIV services
Respondents are asked at baseline, “Have you been to a health service provider in the last 24 months?” At the nine-month follow-up, respondents were asked if they have been to a health service provider in the time since the baseline interview. If the respondent answered affirmatively, he was then asked if he received HIV prevention or treatment services from this service provider (1 = yes).
Continuum of care
HIV-positive respondents were asked at both waves how many times they had visited an HIV provider in the last twelve months. Respondents who had attended at least two appointments in the past year were coded as retained in care (1 = retained). HIV-positive respondents were asked if they had ever taken medication to treat their HIV. Respondents who had taken medication and had missed fewer than four doses in the past 30 days (>85% adherence) were coded as adherent to antiretrovirals (1 = adherent).38 We also measured whether respondents were virally suppressed based upon their recorded viral load. Viral suppression was defined as having an HIV RNA <2000 nucleic acid (NA) copies/mL in whole blood. Blood was drawn via finger stick during the interview and viral load testing (Abbott ReaLTime HIV-1 assay) was applied to samples from dry blood spots. For medication adherent HIV-positive individuals with missing viral load testing (< 3% of HIV-positives), we impute suppression status based on self-report.
PrEP knowledge
For respondents who were HIV-negative at baseline, we examine how affiliations influence knowledge of pre-exposure prophylaxis (PrEP). At both the baseline and follow up interviews, respondents are asked, “Before today, have you heard of PrEP?”
2.3. Covariates
At baseline, respondents were asked their age (years), whether they had previously been diagnosed with HIV, and how they classified their sexual identity. Due to the small number of respondents who neither identified as gay or bisexual. we collapse sexual orientation to a gay vs. non-gay-identified indicator. Respondents were also asked their yearly income, which we collapsed to a binary variable for low income status (less than $20,000 per year), and whether they had previously participated in other HIV programming. Finally, respondents were asked to assess their closeness to the gay and black communities (4 = very close). Our substantive results are robust to the inclusion of educational attainment and neighborhood residence adjustments.
2.4. Analytic strategy
Longitudinal logistic regression models adjust for the original RDS sampling structure and standard errors clustered by seed recruiter. To adjust for selection into Wave 2, we weight the longitudinal models by multiplying the inverse probability of being retained in the follow up by the RDS sample weights, such that the follow up respondents who most closely resemble those who dropped out of the study are weighted more heavily.39 All models utilize social affiliations and control variables measured at baseline to predict the dependent variables measured at follow-up. We calculate pseudo-R2 values for each logistic regression according to Fleiss, Williams and Dubro’s specification.40
3. RESULTS
3.1. Sample description
At the baseline interview, the average age was 22.47 years-old and the majority (85%) of sample had incomes below $20,000. With regard to sexual orientation, 62% of the sample identified as gay. 88% of respondents had visited a healthcare provider in the last two years, and 66% of respondents received HIV care from that provider (Table 1). 20% of the analytic sample reports having been diagnosed with HIV prior to the baseline interview. Among HIV-seropositive respondents at the nine-month follow up, 44% were retained in care, 40% were adherent to antiretrovirals, and 32% were virally suppressed. These trends are in line with levels of care engagement across the HIV care continuum in Chicago.
Table 1.
Baseline and Follow-Up Characteristics of Young Black MSM in the uConnect Cohort (n=618), UConnect, 2013–2016.
| Bridges | Gay Enclave | Black Community | Outsiders | All | Pearson’s Uncorrected Chi-Squared |
||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean | (SE) | Mean | (SE) | Mean | (SE) | Mean | (SE) | Mean | (SE) | ||
| Demographics (baseline) | |||||||||||
| Age (years) | 23.61 | (.34) | 23.70 | (.28) | 21.31 | (.58) | 22.12 | (.34) | 22.47 | (.37) | 15.36** b |
| Low income (1 = yes) | .83 | (.04) | .77 | (.05) | .94 | (.02) | .82 | (.05) | .85 | (.03) | 20.04** |
| Health (baseline) | |||||||||||
| Previously diagnosed HIV positive (1 = yes) | .23 | (.05) | .30 | (.05) | .14 | (.03) | .17 | (.05) | .20 | (.03) | 13.98* |
| Has health service provider (1 = yes) | .84 | (.05) | .92 | (.03) | .88 | (.02) | .85 | (.04) | .88 | (.02) | 4.70 |
| Participation in HIV prevention program or research study (1 = yes) | .28 | (.05) | .29 | (.07) | .21 | (.05) | .31 | (.05) | .27 | (.03) | 4.44 |
| Sexual Orientation (baseline) | |||||||||||
| Gay (1 = yes) | .63 | (.06) | .78 | (.05) | .53 | (.05) | .55 | (.04) | .62 | (.03) | 29.89** |
| Community Closeness (baseline) | |||||||||||
| Closeness to gay community (1 = not at all close, 4 = very close) | 2.87 | (.09) | 2.75 | (.07) | 2.71 | (.11) | 2.26 | (.10) | 2.62 | (.05) | 11.30** b |
| Closeness to black community (1 = not at all close, 4 = very close) | 3.35 | (.09) | 3.27 | (.07) | 3.26 | (.06) | 3.27 | (.11) | 3.28 | (.05) | 0.31 b |
| Health services (baseline) | |||||||||||
| Received HIV prevention or treatment services from provider | .74 | (.06) | .70 | (.03) | .58 | (.07) | .69 | (.04) | .66 | (.03) | 9.90 |
| PrEP aware | .38 | (.07) | .33 | (.07) | .30 | (.04) | .33 | (.06) | .32 | (.03) | 1.32 |
| Retained in care | .45 | (.07) | .50 | (.07) | .31 | (.08) | .34 | (.09) | .41 | (.05) | 5.72 |
| Adherent to ARVs | .35 | (.08) | .42 | (.08) | .23 | (.07) | .29 | (.09) | .34 | (.05) | 5.10 |
| Virally Suppressed | .31 | (.08) | .37 | (.08) | .19 | (.07) | .25 | (.08) | .30 | (.04) | 4.98 |
| Health services (follow up) | |||||||||||
| Received HIV prevention or treatment services from provider | .66 | (.05) | .66 | (.08) | .46 | (.04) | .63 | (.06) | .59 | (.03) | 15.99† |
| PrEP aware | .58 | (.08) | .81 | (.04) | .59 | (.06) | .61 | (.06) | .65 | (.04) | 14.66* |
| Retained in care | .64 | (.08) | .46 | (.09) | .56 | (.08) | .26 | (.07) | .44 | (.04) | 12.97* |
| Adherent to ARVs | .59 | (.09) | .40 | (.09) | .55 | (.08) | .23 | (.08) | .40 | (.04) | 12.89* |
| Virally suppressed | .53 | (.09) | .38 | (.08) | .31 | (.09) | .18 | (.07) | .32 | (.05) | 10.48† |
p < .10
p < .05,
p < .01
Significance based on corrected F-test, corrected F-statistics
Estimates are weighted
Bivariate model F statistic utilized for continuous and ordinal variables
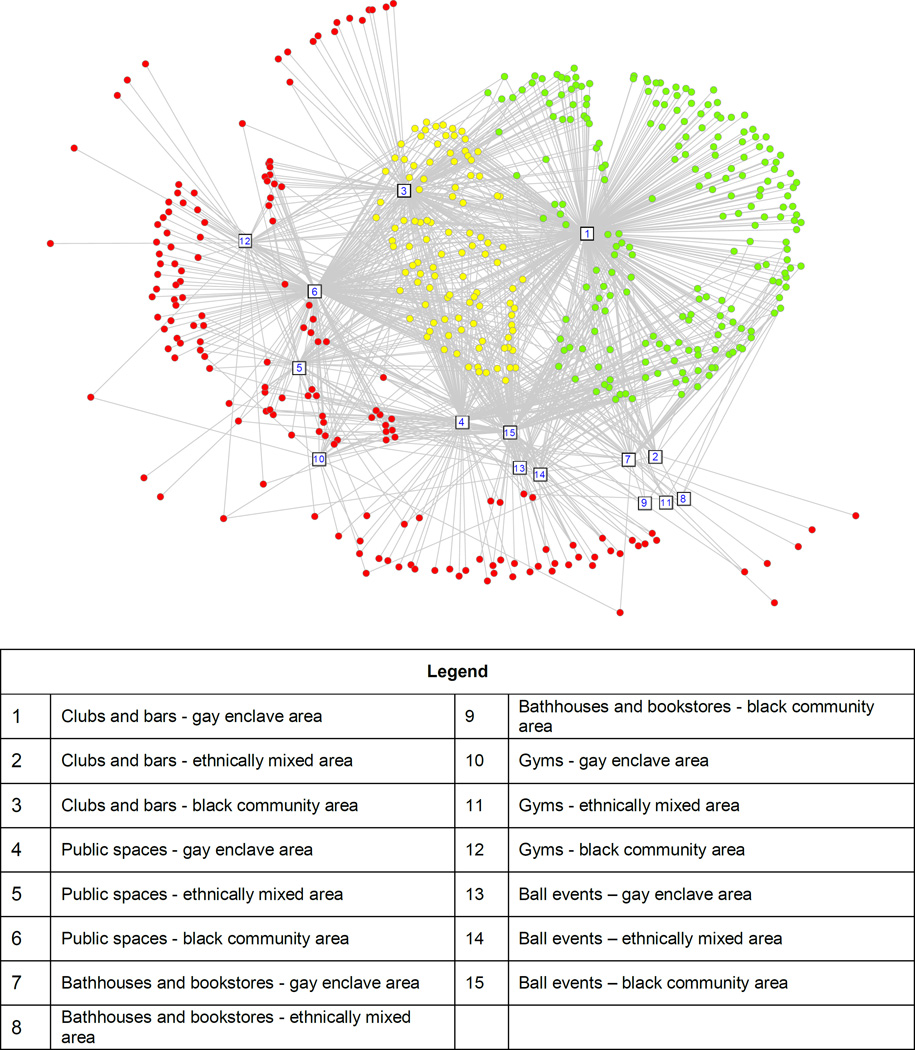
The network that is formed via respondents’ shared affiliations at baseline breaks into clusters that correspond to MSM’s affiliations with different sets of venues: “Black Community,” “Gay Enclave,” and “Bridging.” These cluster names are mnemonics based on the predominant region(s) in which MSM in each affiliation cluster tend to meet others. Figure 1 depicts the respondents, shaded by venue affiliation cluster, within the network. On average, “Gay Enclave” MSM (n = 211, colored green in Figure 1) visit venues that are predominately in Chicago’s gay enclave (North Side), and who have limited interactions with venues and MSM in other parts of the city. In contrast, MSM in the “Black Community” cluster (n = 165, colored red in Figure 1) visit a wide array of venues, but not bars and clubs in the gay enclave region (North Side) (square #1). On average, MSM in the Black Community cluster visit only .36 venues in the gay enclave, almost five times fewer than the 1.4 venues visited on average by the Gay Enclave cluster. The venues frequented by members of this cluster are concentrated in Chicago’s major black community area, as well as in the ethnically diverse neighborhoods on the West Side. The “Bridging” cluster (n = 105) captures respondents who visit both bars in the gay enclave as well as venues beyond the gay enclave (yellow in Figure 1), which they share in common with the Black Community cluster. In this way, respondents in the Bridging cluster serve as bridges connecting respondents who are in the Gay Enclave cluster to those who are in the Black Community cluster. Finally, we create a fourth cluster that contains the remaining “Outsiders” – that is, those respondents who visited zero venues or who frequented only those venues that were in “other” locations (n = 136).
Figure 1.
Respondents (circles) shaded according to cluster membership in a two-mode network visualized using spring embedding layout in UCINET 6. Respondents with Gay Enclave cluster affiliations are green, with Bridges affiliations are yellow, and with Black Community affiliations are red. The venues to which individuals are tied are designated as numbered white squares, labeled below. Outsiders-- respondents without venue affiliations-- are not visualized.
We observe important variation between clusters both in terms of the characteristics and healthcare utilization of their members. On average, 94% of respondents in the Black Community cluster are low-income whereas only 77% respondents in the Gay Enclave, 83% in the Bridging and 82% in the Outsider clusters are low-income. Interestingly, although feelings of connectedness to the gay community vary significantly by affiliation clusters (2.87 among respondents in the Bridging cluster versus 2.26 among respondents in the Outsiders cluster), connectedness to the black community does not vary significantly by affiliation network position. Respondents in the Gay Enclave and Bridging clusters are more likely to identify as gay (78% and 63% of respondents respectively, vs. 53% of respondents in the Black Community cluster and 55% of respondents in the Outsiders cluster). Respondents with Gay Enclave affiliations are also the most likely to have been previously diagnosed with HIV (30%), especially relative to respondents in the Black Community cluster (14%). In the Bridging cluster, HIV diagnosis rates are higher than in the Black Community (14%) and Outsiders (17%) clusters but lower than in the Gay Enclave cluster (30%). Men with Black Community affiliations are also the youngest (21.31 years-old), over two years younger on average than men with Bridging affiliations (23.61 years-old) and Gay Enclave affiliations (23.70 years-old), and slightly less than a year younger than men with Outsider affiliations (22.12 years-old).
Differential healthcare access and utilization by affiliation network position appears to be exacerbated over time. Although we observe substantive differences in HIV care receipt, PrEP awareness, and continuum of care position, these estimates are not significantly different from one another at baseline; however, we do observe significant variation across affiliation network positions at the nine-month follow up. One interpretation of these differences is that individuals are not selecting into certain patterns of afffiliations based on healthcare factors, but that the affiliations at baseline impact access to health services over time. For example, while we observe a general increase in PrEP awareness between the baseline and follow up surveys (32% vs. 65% aware of PrEP), this increase is especially strong among respondents with Gay Enclave affiliations (33% at baseline vs. 81% at follow up). At follow up, with regard to HIV prevention, HIV-negative respondents in the Gay Enclave cluster are most likely to know about PrEP (81% vs. 58% of individuals with Briding affiliations, 59% of individuals with Black Community Affiliations and 61% of respondents with Outsider affiliations).
Although Black Community respondents are the least likely to have received HIV services from a healthcare provider at follow-up (46% for Black Community MSM vs. 59% on average), HIV-seropositive respondents in this group are more likely than respondents with Outsider or Gay Enclave affiliations to be retained in care and adherent to antiretrovirals. Whereas 56% of HIV-positive respondents with Black Community affiliations are retained in care the follow up, only 26% of Outsiders and 46% of individuals with Gay Enclave affiliations are retained in care. A similar pattern is observed for ARV adherence at follow up, at which point 55% of individuals with Black Community respondents report ARV adherence, compared to 23% and 40% of individuals with Outsider and Gay Enclave affiliations respectively. Trends in being retained in care and adherence to ARVs at the follow up are most similar between individuals with Bridging and Black Community (64% vs. 56% and 59% vs. 55%). With regard to viral suppression, individuals with Bridging network positions have the highest rate of suppression (53%), followed by individuals with Gay Enclave (38%), Black Community (31%), and Outsider affiliations (18%).
3.2. Longitudinal multivariate findings
The multivariate models in Table 2 reinforce the descriptive statistics in that, despite their greater participation in the prevention community, Bridging respondents do not exhibit a greater likelihood of receiving of HIV services than Outsiders (Table 2, Model 1). Rather, HIV program participation (AOR: 2.94; 95% CI: 1.64 – 5.28) and HIV-positive status (AOR: 4.44; 95% CI: 2.11 – 9.38) are independently, positively associated with HIV service receipt (Model 3). Rates of HIV service receipt are similar between individuals with Bridging, Gay Enclave, and Outsider patterns of affiliation. However, respondents in the “Black Community” network position have a significantly lower likelihood of receiving HIV treatment or prevention services from a health service provider than Outsiders (AOR = .46; 95% CI: 0.24 – 0.88). A supplemental analysis of trends in HIV service receipt illustrates that while HIV-negative individuals are less likely to receive HIV services, HIV-negative individuals in the Black Community cluster are substantially less likely to access this type of care than are their HIV-positive counterparts within the same cluster (available upon request).
Table 2.
Nested Logistic Regression Models Predicting the Adjusted Odds Ratio (AOR) of Receiving HIV Prevention or Treatment Services from a Healthcare Provider (n = 525), UConnect, 2013–2016.
| WAVE 1 VARIABLES | Receipt of HIV prevention or treatment services from healthcare provider | ||||||
|---|---|---|---|---|---|---|---|
| Model 1 Affiliation cluster |
Model 2 Respondent characteristics controls |
Model 3 Healthcare engagement controls |
|||||
| AOR | 95% CI | AOR | 95% CI | AOR | 95% CI | ||
| Affiliation Cluster | |||||||
| Bridges | 1.11 | (0.59 – 2.10) | 0.89 | (0.43 – 1.82) | 0.95 | (0.48 – 1.89) | |
| Gay Enclave | 1.20 | (0.43 – 3.31) | 0.87 | (0.31 – 2.40) | 0.91 | (0.33 – 2.51) | |
| Black Community | 0.52* | (0.29 – 0.95) | 0.42** | (0.23 – 0.79) | 0.46* | (0.24 – 0.88) | |
| Outsiders | -- | -- | -- | -- | -- | -- | |
| Demographics | |||||||
| HIV positive | 4.41*** | (2.09 – 9.32) | 4.44*** | (2.11 – 9.38) | |||
| Health service provider | 1.63 | (0.72 – 3.70) | 1.45 | (0.64 – 3.26) | |||
| Age (years) | 1.09+ | (0.99 – 1.20) | 1.08+ | (1.00 – 1.18) | |||
| Low income | 1.49 | (0.83 – 2.68) | 1.45 | (0.82 – 2.56) | |||
| Sexual Orientation | |||||||
| Gay | 1.20 | (0.70 – 2.05) | 1.13 | (0.64 – 2.01) | |||
| Community Closeness | |||||||
| Closeness to gay community | 1.09 | (0.82 – 1.44) | 1.04 | (0.77 – 1.41) | |||
| Closeness to black community | 0.99 | (0.66 – 1.50) | 0.99 | (0.64 – 1.52) | |||
| Healthcare Engagement | |||||||
| Clinical HIV service receipt | 2.27* | (1.20 – 4.27) | 1.21 | (0.60 – 2.47) | 1.11 | (0.56 – 2.19) | |
| HIV program participation | 2.94*** | (1.64 – 5.28) | |||||
| PrEP aware | 0.78 | (0.55 – 1.10) | |||||
| Constant | 0.96 | (0.45 – 2.04) | 0.06* | (0.00 – 0.94) | 0.08+ | (0.00 – 1.34) | |
| N | 496 | 494 | 491 | ||||
| F-statistic | 5.37** | 6.01** | 6.63** | ||||
| Pseudo R2 | .04 | 0.10 | 0.12 | ||||
p < .10,
p < .05,
p < .01
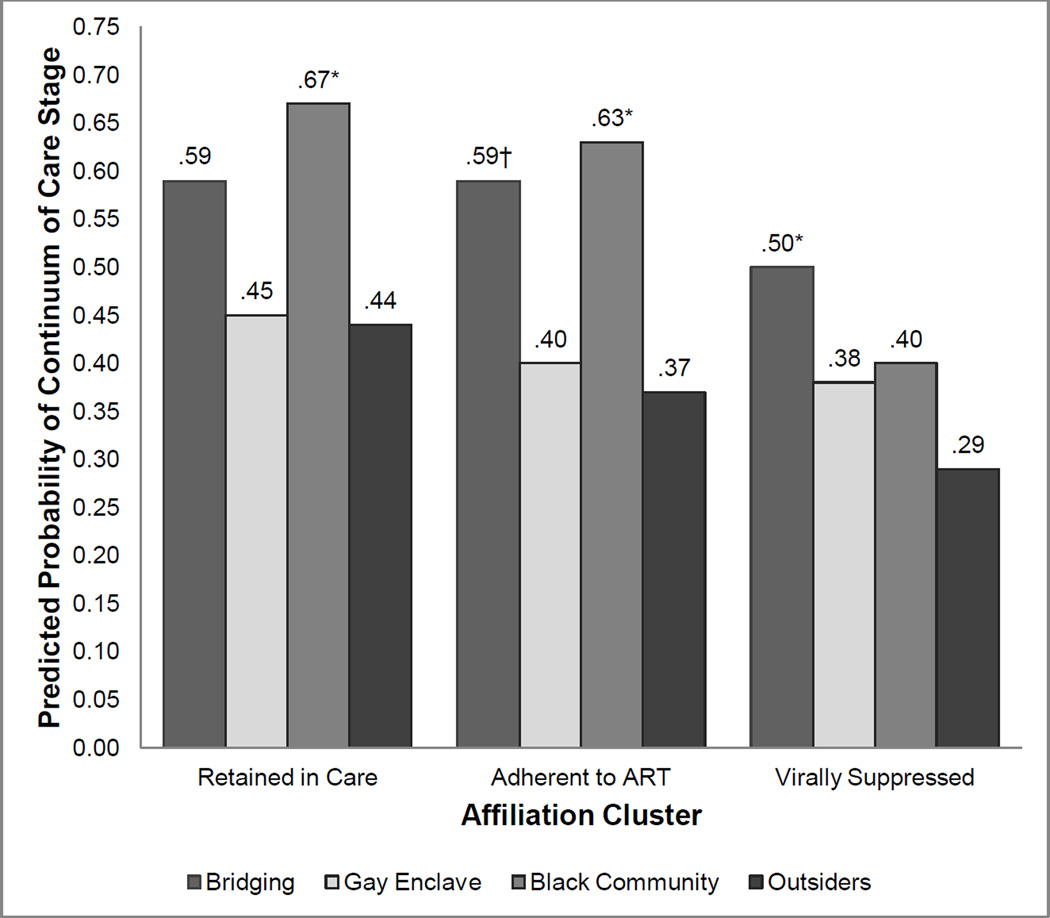
In Table 3, we examine how HIV-positive individuals’ affiliations at baseline are related to their HIV treatment outcomes at follow-up, adjusting for the continuum of care stage at baseline. Although respondents in the Black Community cluster – regardless of their HIV status – are significantly less likely than Outsiders to receive HIV services from a clinical provider, HIV-positive individuals who are in this cluster have significantly improved likelihood of being retained in care and adherent to ARVs (Table 3; Figure 2). Adjusting for whether individuals were retained in care at baseline, Black Community respondents are 3.79 times more likely to be retained in care (AOR =3.79; 95% CI: 1.15 – 12.49) than individuals with Outsiders affiliations, while respondents who are classified in the Bridging (AOR = 2.34; 95% CI: 0.81 – 6.80) and Gay Enclave (AOR: 1.05; 95% CI: 0.34 −3.28) clusters are not significantly more likely than Outsiders to be retained in care. We observe similar patterns in adherence to ARVs: Individuals with Black Community affiliations are 4.39 times more likely to be adherent to antiretrovirals than Outsiders (AOR = 4.39; 95% CI = 1.25 – 15.41) after adjusting for adherence at baseline. Meanwhile, individuals with Bridging (AOR= 3.46; 95% CI: 0.90–13.24) and Gay Enclave (AOR=1.17; 95% CI: 0.33 – 4.16) affiliations do not differ significantly from Outsiders in predicted adherence to ARVs at the 95% confidence level. Taken together, these results suggest that affiliations in the Black Community may have an especially protective relationship with early continuum of care outcomes for HIV-positive individuals.
Table 3.
Nested Logistic Regression Models Predicting the Adjusted Odds Ratio (AOR) of Continuum of Care Stage for HIV-Positive Respondents at Follow Up (n = 188), UConnect, 2013–2016.
| WAVE 1 VARIABLES | Retained in Care |
Adherent to ARVs |
Viral Suppression |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Model 1 Affiliation cluster |
Model 2 Respondent characteristics |
Model 1 Affiliation cluster |
Model 2 Respondent characteristics |
Model 1 Affiliation cluster |
Model 2 Respondent characteristics |
|||||||
| AOR | 95% CI | AOR | 95% CI | AOR | 95% CI | AOR | 95% CI | AOR | 95% CI | AOR | 95% CI | |
| Affiliation Cluster | ||||||||||||
| Bridges | 2.71+ | (0.83 – 8.90) | 2.34 | (0.81 – 6.80) | 3.63+ | (0.95 – 13.85) | 3.46+ | (0.90 – 13.24) | 3.84* | (1.02 – 14.45) | 3.58* | (1.05 – 12.26) |
| Gay Enclave | 1.52 | (0.54 – 4.24) | 1.05 | (0.34 – 3.28) | 1.44 | (0.50 – 4.15) | 1.17 | (0.33 – 4.16) | 1.98 | (0.58 – 6.74) | 1.76 | (0.48 – 6.51) |
| Black Community | 4.35* | (1.27 – 14.91) | 3.79* | (1.15 – 12.49) | 4.88* | (1.31 – 18.15) | 4.39* | (1.25 – 15.41) | 2.27 | (0.72 – 7.13) | 2.08 | (0.62 – 6.93) |
| Outsiders | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- |
| Demographics | ||||||||||||
| Age (years) | 1.13 | (0.94 – 1.36) | 1.05 | (0.88 – 1.26) | 1.02 | (0.83 – 1.25) | ||||||
| Low income | 1.11 | (0.51 – 2.40) | 1.62 | (0.78 – 3.37) | 1.27 | (0.55 – 2.93) | ||||||
| Sexual Orientation | ||||||||||||
| Gay | 5.01** | (1.83 – 13.74) | 7.04*** | (2.41 – 20.59) | 3.33* | (1.18 – 9.42) | ||||||
| Continuum of Care Stage | ||||||||||||
| Retained in care | 7.92*** | (3.07 – 20.42) | 8.03*** | (3.30 – 19.52) | ||||||||
| Adherent to ARVs | 9.04*** | (3.23 – 25.32) | 10.86*** | (4.01 – 29.41) | ||||||||
| Virally suppressed | 12.13*** | (4.51 – 32.64) | 13.17*** | (5.01 – 34.63) | ||||||||
| Constant | 0.22*** | (0.10 – 0.50) | 0.00* | (0.00 – 0.40) | 0.20*** | (0.08 – 0.45) | 0.01* | (0.00 – 0.70) | 0.12*** | (0.05 – 0.27) | 0.02 | (0.00 – 4.62) |
| N | 164 | 164 | 160 | 160 | 164 | 164 | ||||||
| Model F-statistic | 5.15** | 5.61** | 5.39** | 5.26** | 8.76** | 4.81** | ||||||
| Pseudo R2 | .21 | .21 | .18 | .18 | .23 | .25 | ||||||
p < .10,
p < .05,
p < .01
Figure 2.
Predicted probability of continuum care stage for HIV-positive respondents at the nine-month follow-up by venue affiliation cluster based on Model 2, Table 3, UConnect (2013 – 2016).
Note: Statistical significance denoted based on cluster coefficient significance relative to baseline category (Outsiders) in Model 2, Table 3.
Turning to trends in viral suppression, our results suggest that individuals with Bridging affiliations are significantly more likely than individuals who do not frequent Chicago venues (Outsiders) to be virally suppressed, even after adjusting for viral suppression status at baseline (AOR = 3.58; 95% CI: 1.05 – 12.26). However, the likelihood of viral suppression does not differ significantly between indivdiuals with Gay Enclave (AOR = 1.76; 95% CI: 0.48 – 6.51) or Black Community (AOR = 2.08; 95% CI: 0.62 – 6.93) affiliations, relative to Outsiders. These results suggest that individuals with Bridging affiliations may experience health benefits from the increased social capital related to their bridging network position.41 We graph the predicted probabilities of attaining each continuum of care stage based on the multivariate models of Table 3 in Figure 2.
In Table 4, we shift focus to PrEP awareness among HIV-negative respondents. We find that social affiliations play a similarly strong role in prediciting PrEP awareness, as individuals with Gay Enclave position are 2.28 times more likely know about PrEP than are respondents who have no affiliations (AOR = 2.28; 95% CI: 1.14 – 4.57). However, we also find that men with Bridging (AOR = 0.46; 95% CI: 0.19 – 1.10; and Black Community (AOR = 0.99; 95% CI: 0.44 – 2.25) affiliations are not significantly more likely than men who have no affiliations to know about PrEP. Net of PrEP awareness at baseline, these results suggest that men whose affiliations are primarily focused in the gay enclave have experienced the greatest gains in knowledge of new preventative treatment approaches.
Table 4.
Nested Logistic Regression Models Predicting the Adjusted Odds Ratio (AOR) of Knowledge of Pre-Exposure Prophylaxis (PrEP) at Follow Up Among Respondents Who Self-Reported Being HIV-Negative at Baseline (n = 384), UConnect, 2013–2016.
| WAVE 1 VARIABLES | PrEP Awareness |
|||||
|---|---|---|---|---|---|---|
| Model 1 Affiliation cluster |
Model 2 Respondent characteristics controls |
Model 3 Healthcare engagement controls |
||||
| AOR | 95% CI | AOR | 95% CI | AOR | 95% CI | |
| Affiliation Cluster | ||||||
| Bridges | 0.55 | (0.23 – 1.32) | 0.48+ | (0.21 – 1.10) | 0.46+ | (0.19 – 1.10) |
| Gay Enclave | 3.01*** | (1.70 – 5.32) | 2.37* | (1.18 – 4.75) | 2.28* | (1.14 – 4.57) |
| Black Community | 1.06 | (0.46 – 2.43) | 1.05 | (0.44 – 2.48) | 0.99 | (0.44 – 2.25) |
| Outsiders | -- | -- | -- | -- | -- | -- |
| Demographics | ||||||
| Health service provider | 1.24 | (0.69 – 2.23) | 2.13+ | (0.92 – 4.92) | ||
| Age (years) | 1.10* | (1.00 – 1.20) | 1.10* | (1.00 – 1.21) | ||
| Low income | 1.04 | (0.35 – 3.09) | 1.05 | (0.39 – 2.85) | ||
| Sexual Orientation | ||||||
| Gay | 1.91 | (0.81 – 4.50) | 1.96 | (0.83 – 4.64) | ||
| Community Closeness | ||||||
| Closeness to gay community | 0.84 | (0.56 – 1.25) | 0.86 | (0.58 – 1.28) | ||
| Closeness to black community | 0.94 | (0.61 – 1.45) | 0.96 | (0.60 – 1.53) | ||
| Healthcare Engagement | ||||||
| PrEP aware | 13.74** | * (5.83 – 32.43) | 12.97*** | (4.71 – 35.70) | 14.91*** | (4.53 – 49.14) |
| Clinical HIV service receipt | 0.46+ | (0.21 – 1.01) | ||||
| HIV program participation | 1.03 | (0.47 – 2.26) | ||||
| Constant | 0.89 | (0.50 – 1.56) | 0.13 | (0.00 – 5.57) | 0.11 | (0.00 – 4.77) |
| N | 361 | 357 | 356 | |||
| F-statistic | 13.21** | 4.31** | 4.22** | |||
| Pseudo R2 | .18 | .20 | .20 | |||
p < .10,
p < .05,
p < .01
4. DISCUSSION
Despite formal public health initiatives that stress the importance of expanded outreach for HIV prevention, few studies have examined how the informal social venues in which the most at-risk individuals spend their time influence their access to public health services. This paper demonstrates that young, black MSM’s informal affiliations with local social venues are related to their utilization of public-health-related HIV services. Even after adjusting for their use of HIV services at baseline, young black MSM’s positions within the local community venue affiliation network are strongly and significantly associated with the types of HIV-related care they access and their outcomes across the continuum of care.
Social affiliations are related to substantial variation in black MSM’s healthcare engagement. However, there is no single set of affiliations that is universally associated with greater public health service utilization. MSM who have affiliations primarily in the “Black Community” were the least likely to access HIV services from a healthcare provider. This is likely due to limited healthcare providers in the Black community region, a perception that the services in the community are of low quality, or that the majority of HIV testing and outreach resources that link these men to services are located in the gay enclave. Young men in this affiliation cluster may also be less likely to identify as gay, and thus may feel less comfortable disclosing their sexual orientations to local providers.42 We also find that HIV-seropositive respondents with Black Community affiliations were more likely to be retained in care and to adhere to antiretrovirals. This may indicate that receiving healthcare close to where one lives is advantageous for health outcomes, especially given the considerable travel distance between the Black community and gay enclave. Men in this cluster were more likely to have low incomes than other men, and may therefore have faced greater financial barriers to care.2,3 The institutional support offered by these informal programs may thus have a more pronounced impact on these men’s healthcare access and well-being.43 To speculate further regarding the role of social networks – there may be aspects of the personal ties (including family and friends) of members of the Black Community cluster (e.g., density, kin composition) that affect levels of informal scrutiny and enforcement with respect to prescribed medical treatment. Additional research is needed to assess this idea.
Alternatively, research has suggested that while resources located in one’s neighborhood may increase accessibility, black MSM may avoid HIV programming in their area in order to maintain the privacy of their sexual orientation and health status.25 Although our work cannot test this question directly, our results suggest that HIV-positive men whose affiliations geographically overlap with their residential neighborhoods are more likely to be retained in care and more likely to be adherent to ARVs (“Black Community” cluster), and men whose affiliations bridged between their geographic neighborhoods and other neighobrhoods in the city (“Bridges” cluster) were more likely to be virally suppressed than individuals with no affiliations. The vast majority of UConnect sample respondents live in Chicago’s major black community on the South Side and there are no significant differences in residential neighborhood region across affiliation network position. This suggests that the affiliation network effects we observe are not proxying differences across residential neighborhood contexts. If black MSM are indeed likely to access public health services within their residential neighborhood, then social affiliations concentrated within their neighborhoods may serve as “vital places” for these men to maintain supportive ties with others and learn about health resources within their communities.14 At least among HIV-positive individuals, this geographic overlap appears to offer health benefits as continuum of care outcomes are best among individuals who spend more time in venues within the black community.
The social networks that black MSM form and maintain via their venue affliliations also likely play a role in their patterns of healthcare engagement and greater geographic overlap between men’s residential neighborhoods and local social affiliations may increase their access to social support after becoming HIV-positive. Although venues within gay enclaves are frequent targets for expanded HIV outreach44, black MSM may be less likely to benefit from outreach efforts there given their greater risk of experiencing countervailing stigma within them.45,46 Black MSM may also experience greater minority stress spending time in the gay enclave.47 In Chicago—as in many other cities-- the gay enclave is located in a whiter, more affluent region of the city than where most black MSM live and black MSM may be more likely to experience racial discrimination by both gay community members, as well as by neighborhood residents, in this area. Indeed, we find that individuals whose affilaitions are predominately based in the gay enclave are more likely to know about PrEP, but neither more likely to receive HIV services nor report improved HIV outcomes relative to individuals with no affiliations. Social relationships with others whom MSM feel they can rely on, who reaffirm self-worth, and who promote social integration help to buffer the effects of structural barriers on decreased mental health and healthcare utilization48 and improve medication adherence for HIV-positive individuals.49 Our finding that viral suppression is highest among sero-positive men whose affiliations bridge the black and gay communities suggests that these men may benefit from the increased social capital their network position engenders.41 Individuals who are embedded in supportive social networks may be directly encouraged and/or more motivated to engage with healthcare services48,50 and these networks may be formed most readily among men who spend more time in venues located in the black community (i.e. among individuals with Bridging and Black Community affiliations).
The UConnect data offer a unique opportunity to examine how the informal social venues in which black MSM meet their friends and sex partners are linked to intra-population disparities in healthcare access and HIV treatment outcomes. However, there are several important limitations to this study. First, our sample of YBMSM is drawn exclusively from Chicago, so the results of our study are not necessarily generalizable. However, trends in both residential segregation and segregation within the gay community in Chicago mirror those of other large urban areas. Secondly, our construction of the affiliation network clusters relies on respondents’ affiliations with venue types within different regions of the city. In regions with a high density of venues, it is unlikely that all venues of a given type feature identical social environments.
Nonetheless, the geographically-specific venue types we utilize are important. Given the dynamic nature of venue formation and dissolution, a typology of venues remains constant and provides a framework for public health engagement and intervention. Finally, because our sample consists entirely of young, black MSM, we are unable to test whether their particular social affiliations account for their higher HIV incidence rates compared to white MSM. Thus, while we cannot address disparities between populations2, this next generation analysis moves beyond a disparities framework and begins to illuminate the factors and processes that are most amenable to intervention within Black MSM networks. Such an approach recognizes BMSM as a diverse group, and in particular younger Black MSM, for whom prevention interventions are largely absent.51
5. PUBLIC HEALTH IMPLICATIONS
Greater intervention efforts are needed in venues beyond gay enclave communities to address the prevention and treatment needs of young, black MSM. Adherence to PrEP may most effectively engage young, black MSM who frequent venues in the “Black Community” cluster due to this group’s greater adherence to HIV antiretrovirals, which require a similar pattern of engagementas PrEP care. Although we find that PrEP awareness is currently highest among MSM with “Gay Enclave” affiliations, PrEP’s efficacy as biomedical prevention is contingent on consistent usage, and patterns of adherence behaviors which are substantially greater among men with “Black Community” affiliations. Positioning PrEP outreach in the “Black Community,” where the vast majority of young, black MSM live if not also socialize, may thus improve broader prevention efforts by increasing young black MSM’s geographic access and adherence to PrEP.
Our findings emphasize the broader role of local social affiliations for health inequalities. At-risk men’s affiliations can increase healthcare utilization, knowledge of preventative services, and HIV treatment outcomes. However the patterns in which types of public health services these affiliations privilege are complex and reveal important heterogeneity in healthcare engagement within this vulnerable population. Informal social affiliations, particularly those beyond gay enclaves, represent promising sites for future interventions that strategically engage at-risk individuals within the population most affected by HIV. Moving toward a framework of health equity, future research is needed to better understand intra-population dynamics and disparities to formulate impactful interventions that improve minority health.
Supplementary Material
Acknowledgments
Data from this project were collected with financial support from the National Institutes of Health (R01 DA033875). Support for this research was also provided by the Agency for Healthcare Research and Quality (R36 HS024167-01) and the National Institutes of Health (R01 MH100021). The content of this paper is the responsibility of the authors and does not reflect the official views of the AHRQ or the NIH. We thank all study respondents for participating. We also thank Alexander Currit, Adam Jonas, Aditya Khanna, Keith Green, Nicola Lancki and other members of the UConnect study team for their advice throughout the research process.
Footnotes
CONFLICTS OF INTEREST: The authors do not have any conflicts of interest to report. The writing and content of this paper is the sole responsibility of the authors.
HUMAN SUBJECTS: IRB approval from the University of Chicago and National Opinion Research Center was granted prior to the first wave of UConnect data collection in 2013.
INFORMED CONSENT: Informed consent was obtained from all study participants and was a criterion for participation in the UConnect study. Participants were only eligible if they were able to provide informed consent at the time of the study visit.
REFERENCES
- 1.Centers for Disease Control and Prevention. Lifetime Risk of HIV Diagnosis. [Accessed June 5, 2016];NCHHSTP. 2016 http://www.cdc.gov/nchhstp/newsroom/2016/croi-press-release-risk.html.
- 2.Millett GA, Peterson JL, Flores SA, et al. Comparisons of disparities and risks of HIV infection in black and other men who have sex with men in Canada, UK, and USA: A meta-analysis. The Lancet. 2012;380(9839):341–348. doi: 10.1016/S0140-6736(12)60899-X. [DOI] [PubMed] [Google Scholar]
- 3.Levy ME, Wilton L, Phillips G, et al. Understanding structural barriers to accessing HIV testing and prevention services among black men who have sex with men (BMSM) in the United States. AIDS Behav. 2014;18(5):972–996. doi: 10.1007/s10461-014-0719-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pierce SJ, Miller RL, Morales MM, Forney J. Identifying HIV prevention service needs of African American men who have sex with men: an application of spatial analysis techniques to service planning. J Public Health Manag Pract. 2007;(Suppl):S72–S79. doi: 10.1097/00124784-200701001-00012. [DOI] [PubMed] [Google Scholar]
- 5.Scott HM, Pollack L, Rebchook GM, Huebner DM, Peterson J, Kegeles SM. Peer social support is associated with recent HIV testing among young black men who have sex with men. AIDS Behav. 2014;18(5):913–920. doi: 10.1007/s10461-013-0608-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zinski A, Westfall AO, Gardner LI, et al. The Contribution of Missed Clinic Visits to Disparities in HIV Viral Load Outcomes. Am J Public Health. 2015;105(10):2068–2075. doi: 10.2105/AJPH.2015.302695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Attia S, Egger M, Muller M, Zwahlen M, Low N. Sexual transmission of HIV according to viral load and antiretroviral therapy: systematic review and meta-analysis. AIDS. 2009;23(11):1397–14044. doi: 10.1097/QAD.0b013e32832b7dca. [DOI] [PubMed] [Google Scholar]
- 8.Millett GA, Peterson JL, Wolitski RJ, Stall R. Greater risk for HIV infection of black men who have sex with men: a critical literature review. Am J Public Health. 2006;96(6):1007–1019. doi: 10.2105/AJPH.2005.066720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Millett GA, Flores SA, Peterson JL, Bakeman R. Explaining disparities in HIV infection among black and white men who have sex with men: a meta-analysis of HIV risk behaviors. AIDS. 2007;21(15):2083–2091. doi: 10.1097/QAD.0b013e3282e9a64b. [DOI] [PubMed] [Google Scholar]
- 10.Oster AM, Wiegand RE, Sionean C, et al. Understanding disparities in HIV infection between black and white MSM in the United States. AIDS. 2011 Mar;25:1103–1112. doi: 10.1097/QAD.0b013e3283471efa. [DOI] [PubMed] [Google Scholar]
- 11.Frost SDW. Using sexual affiliation networks to describe the sexual structure of a population. Sex Transm Infect. 2007;83(Suppl 1(suppl_1)):37–i42. doi: 10.1136/sti.2006.023580. [DOI] [PubMed] [Google Scholar]
- 12.Laumann EO, Ellingson S, Mahay J, Paik A, Youm Y. The Sexual Organization of the City. Chicago: University of Chicago Press; 2004. [Google Scholar]
- 13.Browning CR, Soller B, Jackson AL. Neighborhoods and adolescent health-risk behavior: An ecological network approach. Soc Sci Med. 2014:1–10. doi: 10.1016/j.socscimed.2014.06.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Walton E. Vital places: Facilitators of behavioral and social health mechanisms in low-income neighborhoods. Soc Sci Med. 2014;122:1–12. doi: 10.1016/j.socscimed.2014.10.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Delgado M. The role of Latina-owned beauty parlors in a Latino Community. Soc Work. 1997;42:445–453. [Google Scholar]
- 16.Linnan L, Thomas S, D’Angelo H, Owens Ferguson Y. African American Barbershops adn Beauty Salons: An Innovative Approach to Reducing Health Disparities through Community Building and Health Education. Community Organizing and Community Buidilng for Health and Welfare. 2012:229–245. [Google Scholar]
- 17.Small ML. Unanticipated Gains: Origins of Network Inequality in Everyday Life. New York: Oxford University Press; 2009. [Google Scholar]
- 18.Bowles KE, Clark HA, Tai E, et al. Implementing rapid HIV testing in outreach and community settings: results from an advancing HIV prevention demonstration project conducted in seven U.S. cities. Public Health Rep. 2008;(Suppl 3(123)):78–85. doi: 10.1177/00333549081230S310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Centers for Disease Control. HIV Testing in Non-Clinical Settings. [Accessed December 4, 2015];Div HIV/AIDS Prev Natl Cent HIV/AIDS, Viral Hepatitis, Sex Transm Dis Tuberc Prev Centers Dis Control Prev. 2015 http://www.cdc.gov/msmhealth/msm-programs.htm.
- 20.White House Office of National AIDS Policy. A National HIV/AIDS Strategy for the United States. Washington, DC: 2010. [Google Scholar]
- 21.De P, Singh AE, Wong T, Yacoub W, Jolly AM. Sexual network analysis of a gonorrhoea outbreak. Sex Transm Infect. 2004;80(4):280–285. doi: 10.1136/sti.2003.007187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Klovdahl A, Graviss E, Yaganehdoost A, et al. Networks and tuberculosis: an undetected community outbreak involving public places. Soc Sci Med. 2001;52(5):681–694. doi: 10.1016/s0277-9536(00)00170-2. [DOI] [PubMed] [Google Scholar]
- 23.Binson D, Woods WJ, Pollack L, Paul J, Stall R, Catania JA. Differential HIV risk in bathhouses and public cruising areas. Am J Public Health. 2001;91(9):1482–1486. doi: 10.2105/ajph.91.9.1482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Thiede H, Jenkins RA, Carey JW, et al. Determinants of Recent HIV Infection Among Seattle-Area Men Who Have Sex with Men. Am J Public Health. 2009;99(S1):S157–S164. doi: 10.2105/AJPH.2006.098582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Seal DW, Kelly JA, Bloom FR, et al. HIV prevention with young men who have sex with men: What young men themselves say is needed. AIDS Care. 2000;12(1):5–26. doi: 10.1080/09540120047431. [DOI] [PubMed] [Google Scholar]
- 26.MacKellar DA, Gallagher KM, Finlayson T, Sanchez T, Lansky A, Sullivan P. Surveillance of HIV Risk and Prevention Behaviors of Men Who Have Sex with Men: A National Application of Venue-Based, Time-Space Sampling. Public Health Rep. 2007;122(Supplement 1):39–47. doi: 10.1177/00333549071220S107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kelly JA, St Lawrence JS, Diaz YE, et al. HIV risk behavior reduction following intervention with key opinion leaders of population: an experimental analysis. Am J Public Health. 1991;81(2):168–171. doi: 10.2105/ajph.81.2.168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Borgatti SP, Everett MG. Network analysis of 2-mode data. Soc Networks. 1997;19:243–269. [Google Scholar]
- 29.Fujimoto K, Williams ML, Ross MW. Venue-based affiliation networks and HIV risk-taking behavior among male sex workers. Sex Transm Dis. 2013;40(6):453–458. doi: 10.1097/OLQ.0b013e31829186e5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Schneider JA, Walsh T, Cornwell B, Ostrow D, Michaels S, Laumann EO. HIV health center affiliation networks of black men who have sex with men: disentangling fragmented patterns of HIV prevention service utilization. Sex Transm Dis. 2012;39(8):598–604. doi: 10.1097/OLQ.0b013e3182515cee. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Gardner EM, McLees MP, Steiner JF, Del Rio C, Burman WJ. The spectrum of engagement in HIV care and its relevance to test-and-treat strategies for prevention of HIV infection. Clin Infect Dis. 2011;52(6):793–800. doi: 10.1093/cid/ciq243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Mugavero MJ, Amico KR, Horn T, Thompson MA. The state of engagement in HIV care in the United States: from cascade to continuum to control. Clin Infect Dis. 2013;57(8):1164–1171. doi: 10.1093/cid/cit420. [DOI] [PubMed] [Google Scholar]
- 33.Khanna AS, Michaels S, Skaathun B, et al. Preexposure Prophylaxis Awareness and Use in a Population-Based Sample of Young Black Men Who Have Sex With Men. JAMA Intern Med. 2015:1–3. doi: 10.1001/jamainternmed.2015.6536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Wacquant L. Urban Outcasts: A Comparative Sociology of Advanced Marginality. Cambridge, UK: Polity; 2008. [Google Scholar]
- 35.Wilson WJ. The Truly Disadvantaged: The Inner City, the Underclass, and Public Policy. Chicago: University of Chicago Press; 1987. [Google Scholar]
- 36.Borgatti SP, Everett MG, Freeman LC. UCINET for Windows: Software for Social Network Analysis. 2002. [Google Scholar]
- 37.Everitt BS, Landau S, Leese M, Stahl D. Cluster Analysis. 5th. London: Wiley; 2011. [Google Scholar]
- 38.Paterson DL, Swindells S, Mohr J, et al. Adherence to protease inhibitor therapy and outcomes in patients with HIV infection. Ann Intern Med. 2000;133(1):21–30. doi: 10.7326/0003-4819-133-1-200007040-00004. [DOI] [PubMed] [Google Scholar]
- 39.Morgan SL, Todd JJ. A diagnostic routine for the detection of consequential heterogeneity of causal effects. Sociol Methodol. 2008;38(1):231–281. [Google Scholar]
- 40.Fleiss JL, Williams JB, Dubro AF. The logistic regression analysis of psychiatric data. J Psychiatr Res. 1986;20(3):195–209. doi: 10.1016/0022-3956(86)90003-8. [DOI] [PubMed] [Google Scholar]
- 41.Burt RS. The Network Structure of Social Capital. Research in Organizational Behavior. 2000:345–423. [Google Scholar]
- 42.Petroll AE, Mosack KE. Physician awareness of sexual orientation and preventive health recommendations to men who have sex with men. Sex Transm Dis. 2011;38(1):63–67. doi: 10.1097/OLQ.0b013e3181ebd50f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Watkins-Hayes C. The micro dynamics of support seeking: The social and economic utility of institutional ties for HIV-positive women. Ann Am Acad Pol Soc Sci. 2013;647:83–101. [Google Scholar]
- 44.Voisin DR, Bird JDP, Shiu C-S, Krieger C. “It’s crazy being a Black, gay youth.” Getting information about HIV prevention: a pilot study. J Adolesc. 2013;36(1):111–119. doi: 10.1016/j.adolescence.2012.09.009. [DOI] [PubMed] [Google Scholar]
- 45.Choi K-H, Han C, Paul J, Ayala G. Strategies for managing racism and homophobia among U.S. ethnic and racial minority men who have sex with men. AIDS Educ Prev. 2011;23(2):145–158. doi: 10.1521/aeap.2011.23.2.145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Han C. They Don’t Want To Cruise Your Type: Gay Men of Color and the Racial Politics of Exclusion. Soc Identities. 2007;13(1):51–67. [Google Scholar]
- 47.Meyer IH. Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations: conceptual issues and research evidence. Psychol Bull. 2003;129(5):674–697. doi: 10.1037/0033-2909.129.5.674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Lauby JL, Marks G, Bingham T, et al. Having supportive social relationships is associated with reduced risk of unrecognized HIV infection among black and Latino men who have sex with men. AIDS Behav. 2012;16(3):508–515. doi: 10.1007/s10461-011-0002-3. [DOI] [PubMed] [Google Scholar]
- 49.Gonzalez JS, Penedo FJ, Antoni MH, et al. Social support, positive states of mind, and HIV treatment adherence in men and women living with HIV/AIDS. Health Psychol. 2004;23(4):413–418. doi: 10.1037/0278-6133.23.4.413. [DOI] [PubMed] [Google Scholar]
- 50.Bouris A, Hill BJ, Fisher K, et al. Mother-Son Communication About Sex and Routine Human Immunodeficiency Virus Testing Among Younger Men of Color Who Have Sex With Men. J Adolesc Heal. 2015;57(5):515–522. doi: 10.1016/j.jadohealth.2015.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Hemmige V, McFadden R, Cook S, Tang H, Schneider JA. HIV prevention interventions to reduce racial disparities in the United States: a systematic review. J Gen Intern Med. 2012;27(8):1047–1067. doi: 10.1007/s11606-012-2036-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.