Abstract
Background
Type II diabetes is a chronic health condition which is associated with skin conditions including chronic foot ulcers and an increased incidence of skin infections. The skin microbiome is thought to play important roles in skin defence and immune functioning. Diabetes affects the skin environment, and this may perturb skin microbiome with possible implications for skin infections and wound healing. This study examines the skin and wound microbiome in type II diabetes.
Methods
Eight type II diabetic subjects with chronic foot ulcers were followed over a time course of 10 weeks, sampling from both foot skin (swabs) and wounds (swabs and debrided tissue) every two weeks. A control group of eight control subjects was also followed over 10 weeks, and skin swabs collected from the foot skin every two weeks. Samples were processed for DNA and subject to 16S rRNA gene PCR and sequencing of the V4 region.
Results
The diabetic skin microbiome was significantly less diverse than control skin. Community composition was also significantly different between diabetic and control skin, however the most abundant taxa were similar between groups, with differences driven by very low abundant members of the skin communities. Chronic wounds tended to be dominated by the most abundant skin Staphylococcus, while other abundant wound taxa differed by patient. No significant correlations were found between wound duration or healing status and the abundance of any particular taxa.
Discussion
The major difference observed in this study of the skin microbiome associated with diabetes was a significant reduction in diversity. The long-term effects of reduced diversity are not yet well understood, but are often associated with disease conditions.
Keywords: Diabetes, Diabetic ulcer, Diversity, Skin microbiome, 16S rRNA gene sequencing
Introduction
Type II diabetes is one the fastest growing chronic diseases in the world today, predicted to rise from 382 million people in 2013 to 592 million in 2035 (Guariguata et al., 2014). The disease is characterised by persistently elevated blood glucose levels as a result of insufficient insulin production or insulin resistance. This leads to many serious complications affecting the heart, kidneys, eyes, blood vessels and nerves (World Health Organisation, 2016). The development of foot ulcers is the culmination of several of these complications, estimated to affect 15 % of diabetes sufferers (Reiber, Boyko & Smith, 1995). These wounds are often slow to heal, difficult to treat, and prone to infection. They have a severe impact on a patient’s quality of life, and are estimated to increase the risk of lower limb amputation by 15 fold (Australian Institute of Health and Welfare, 2008). The cost of treating these chronic wounds is estimated at up to $13 billion annually in the US alone (Rice et al., 2014), and is set to rise with the increasing incidence of diabetes worldwide.
Diabetes is associated with shifts in the gut microbiota (Karlsson et al., 2013; Qin et al., 2012), and these shifts are thought to contribute to the onset of disease (Parekh et al., 2016; Zhang & Zhang, 2013). Dysbiosis of the human microbiome is increasingly recognised to play a role in many diseases, through mechanisms such as altered intestinal barrier function (Kelly et al., 2015), triggering or exacerbating inflammation (Strober, 2013) and regulation of energy metabolism (Samuel et al., 2008). Given the physical changes that occur in the skin as a result of diabetes, such as increased dryness and pH, and glycosylation of structural skin proteins (Behm et al., 2012), it is feasible that diabetes may also affect the microbiome of the skin.
As in the gut, the skin microbiome is thought to protect against infection via both competitive exclusion and direct inhibition (Bomar et al., 2016; Cogen et al., 2010b; Iwase et al., 2010; Shu et al., 2013), and have the potential to regulate skin immune function and wound healing (Kanno et al., 2011; Scales & Huffnagle, 2013). For example, the most common skin isolate, Staphylococcus epidermidis, has been shown to down-regulate inflammation following skin injury (Lai et al., 2009), and to up-regulate the production of antimicrobial peptides in the host (Lai et al., 2010), which work synergistically with antimicrobial peptides from S. epidermidis to inhibit pathogens such as Staphyloccocus aureus and Group A Streptococcus (Cogen et al., 2010a). Another skin commensal, Acinetobacter lwoffii, has been shown to protect against allergic sensitization and inflammation by promoting TH1 and anti-inflammatory responses in the skin (Fyhrquist et al., 2014). Given the importance of the skin microbiome in preventing infection, any shifts to these communities could affect their ability to protect against infection, and may have an effect on wound healing.
The aim of this study was to determine whether there are differences in the skin microbiome between persons with diabetes and healthy controls, and whether any members of the skin microbiome in diabetes are associated with those microbes that colonise chronic wounds during wound healing. We examined a cohort of eight diabetic and eight control individuals at six time points over a 10-week period, by swabbing the skin on the soles of both feet, and collecting swabs and debrided tissue from the chronic foot ulcers of the diabetic patients. The microbial communities associated with these samples were assessed via high-throughput sequencing of the V4 region of the bacterial 16S rRNA gene.
Materials & Methods
Study design, ethics approval, and sample collection
Ethical approval for the study was obtained from both the University of Technology Sydney Human Research Ethics Committee (approval number 2013000170), and the Western Sydney Local Health District Human Research Ethics Committee (approval number HREC2013/9/5.3(3809) AU RED LNR/13/WMEAD/294). Diabetic individuals and control subjects provided written consent for sample collection and all subsequent analyses.
Diabetic adults (n = 8) (Table 1) were selected for inclusion in the study based on medical diagnosis of type II diabetes, the presence of a chronic wound on one foot (chronic wound = present for six or more weeks) and no antibiotic therapy within the previous four weeks. Three swabs were collected for each diabetic subject every two weeks for a 10 week period using sterile rayon tipped swabs (Copan) that had been pre-moistened with a sterile solution of 0.15 M NaCl and 0.1% Tween 20. Two skin swabs were collected from intact foot skin (1) adjacent to the chronic wound (skin adjacent, SA) and (2) contralateral site to the chronic wound (skin contralateral, SC). Skin swabs were collected by firmly rubbing the moistened swab over the base of the foot skin surface for a period of 30 seconds. The whole base of the foot was used to maximise the DNA yield. Skin swab samples were taken prior to any cleaning of the skin surface that routinely took place before debridement of wound tissue. Chronic wounds were cleaned by applying gauze soaked with Prontosan wound irrigation solution (B. Braun Medical, Sheffield, UK) for ten minutes prior to sharp debridement of tissue from the top of the wound (wound debridement, WD). Wound debridement samples were only taken where debridement was deemed to be necessary for the standard wound care. Wound swabs were taken after irrigation of the wound with Prontosan to remove loose tissue, using a dry swab and the Z swab method (wound swab, WS). The Z swab method was the routine method used in the clinic at the time of sampling.
Table 1. Characteristics of diabetic and control cohorts.
| Diabetic | Control | |
|---|---|---|
| Age (years) | 68.9 ± 8.2 (58–81) | 62.8 ± 13.4 (50–81) |
| BMI | 35.4 ± 5.9 (27.2–47.1) | 28.0 ± 6.6 (20.4–37.9) |
| Males:Females | 5:3 | 2:6 |
Notes.
Characteristics are shown for the diabetic and control subjects in the study. Average values with standard deviations are reported, including the range in brackets.
Control subjects (n = 8) (Table 1) were recruited from Sydney, Australia. The criteria for inclusion were not to have been diagnosed as diabetic, between 50–80 years of age, and without the use of antibiotics within the previous four weeks. Skin swabs were collected from the left and right feet of control subjects as described above. Samples were taken from all participants every two weeks for a 10-week period (6 time points in total). All samples were processed for DNA on the day of collection, or stored at 4°C until processing the next day. These storage conditions have been shown to adequately preserve the microbial profile of skin swab samples (Lauber et al., 2010).
Extraction of microbial DNA from skin and wound swabs and wound debridement tissue
Genomic DNA was extracted from all skin and wound samples using the BioStic DNA extraction kit (MO BIO Laboratories, Carlsbad, CA, USA). Swab heads were cut off the plastic applicator using sterile surgical scissors into the bead beating tube from the DNA extraction kit, before addition of buffer CB1. For wound debridement tissue, the tissue was directly placed into the bead beating tube. All subsequent steps were in accordance with the manufacturer’s instructions, and DNA was eluted in 50 µl of solution CB5 (10 mM Tris pH 8). The extracted DNA was quantified on a Qubit® 2.0 Fluorometer (Life Technologies, Carlsbad, CA, USA) with a Qubit® dsDNA HS Assay Kit (Life Technologies, Carlsbad, CA, USA).
Preparation of 16S rRNA gene libraries for Illumina sequencing
A library of the V4 region of the 16S rRNA gene was prepared for Illumina sequencing from the isolated microbial DNA samples. Samples were amplified using primers based on the Caporaso et al. design (Caporaso et al., 2012), which were modified to include eight nt rather than 12 nt barcodes, and include a barcode on both the forward and reverse primer (V4_forward and V4_reverse; Table 2). Different barcoded primers were used for each sample. For skin samples, the V4 region was amplified from 500 pg template DNA; for wound samples template DNA started at 10 ng, but in some cases up to 50 ng was used where a PCR product was not obtained with lower amounts of template DNA. Each sample was subjected to 10 cycles of PCR with 0.5 µM each of V4_forward and V4_reverse barcoded primers in a 50 µl PCR reaction that contained 1 × Taq core PCR buffer (Qiagen, Venlo, Netherlands), 1 × Q solution, 250 µM dNTPs, and 1.25 U Taq DNA polymerase. Thermal cycling was carried out at 95°C for two minutes, followed by 10 cycles of 95°C for 15 s, 50°C for 30 s and 72°C for 90 s, followed by a final extension at 72°C for five minutes. Excess primer was removed via a magnetic bead clean-up using 0.8 volume of Axygen® AxyPrep Mag beads (Corning, NY, USA) and the eluted amplicons were subjected to a further 20 cycles of PCR with 0.25 µM enrichment primers (Illumina_E_1 and Illumina_E_2; Table 2). The PCR reaction and cycling was performed as described above, except that the annealing temperature was increased to 55°C and 20 thermal cycles were performed. Following confirmation of the PCR product on a 1% agarose gel, the amplicons were purified using Axygen® AxyPrep Mag beads (Corning, NY, USA) and quantified on a Qubit® 2.0 Fluorometer (Life Technologies, Carlsbad, CA, USA) with a Qubit® dsDNA HS Assay Kit (Life Technologies, Carlsbad, CA, USA). Equimolar (2 ng) amounts of the 16S amplicons obtained for each skin and wound sample were then pooled and the molarity of the pooled amplicons determined using a Bioanalyser High Sensitivity DNA chip (Agilent Technologies, Santa Clara, CA, USA).
Table 2. Primer sequences used in this study.
| Primer name | Sequence 5′–3′ |
|---|---|
| V4_forward_1 | AATGATACGGCGACCACCGAGATCTACACAACCAGTCTATGGTAATTGTGTGCCAGCMGCCGCGGTAA |
| V4_forward_2 | AATGATACGGCGACCACCGAGATCTACACAACGCTAATATGGTAATTGTGTGCCAGCMGCCGCGGTAA |
| V4_forward_3 | AATGATACGGCGACCACCGAGATCTACACAAGACTACTATGGTAATTGTGTGCCAGCMGCCGCGGTAA |
| V4_forward_4 | AATGATACGGCGACCACCGAGATCTACACAATCGATATATGGTAATTGTGTGCCAGCMGCCGCGGTAA |
| V4_forward_5 | AATGATACGGCGACCACCGAGATCTACACACCAATTGTATGGTAATTGTGTGCCAGCMGCCGCGGTAA |
| V4_forward_6 | AATGATACGGCGACCACCGAGATCTACACACTGAAGTTATGGTAATTGTGTGCCAGCMGCCGCGGTAA |
| V4_forward_7 | AATGATACGGCGACCACCGAGATCTACACATTGCCGCTATGGTAATTGTGTGCCAGCMGCCGCGGTAA |
| V4_forward_8 | AATGATACGGCGACCACCGAGATCTACACCAACCTTATATGGTAATTGTGTGCCAGCMGCCGCGGTAA |
| V4_forward_9 | AATGATACGGCGACCACCGAGATCTACACCCTAATAATATGGTAATTGTGTGCCAGCMGCCGCGGTAA |
| V4_forward_10 | AATGATACGGCGACCACCGAGATCTACACCCTCTGATTATGGTAATTGTGTGCCAGCMGCCGCGGTAA |
| V4_forward_14 | AATGATACGGCGACCACCGAGATCTACACGAACGGAGTATGGTAATTGTGTGCCAGCMGCCGCGGTAA |
| V4_forward_16 | AATGATACGGCGACCACCGAGATCTACACGCGTTACCTATGGTAATTGTGTGCCAGCMGCCGCGGTAA |
| V4_forward_18 | AATGATACGGCGACCACCGAGATCTACACGGATGCCATATGGTAATTGTGTGCCAGCMGCCGCGGTAA |
| V4_forward_20 | AATGATACGGCGACCACCGAGATCTACACGTTGGCCGTATGGTAATTGTGTGCCAGCMGCCGCGGTAA |
| V4_forward_22 | AATGATACGGCGACCACCGAGATCTACACTGACTGCTTATGGTAATTGTGTGCCAGCMGCCGCGGTAA |
| V4_forward_24 | AATGATACGGCGACCACCGAGATCTACACTTCAGCGATATGGTAATTGTGTGCCAGCMGCCGCGGTAA |
| V4_reverse_1 | CAAGCAGAAGACGGCATACGAGATAACCAGTCAGTCAGTCAGCCGGACTACHVGGGTWTCTAAT |
| V4_reverse_7 | CAAGCAGAAGACGGCATACGAGATATTGCCGCAGTCAGTCAGCCGGACTACHVGGGTWTCTAAT |
| V4_reverse_8 | CAAGCAGAAGACGGCATACGAGATCAACCTTAAGTCAGTCAGCCGGACTACHVGGGTWTCTAAT |
| V4_reverse_9 | CAAGCAGAAGACGGCATACGAGATCCTAATAAAGTCAGTCAGCCGGACTACHVGGGTWTCTAAT |
| V4_reverse_15 | CAAGCAGAAGACGGCATACGAGATGCCTACGCAGTCAGTCAGCCGGACTACHVGGGTWTCTAAT |
| V4_reverse_16 | CAAGCAGAAGACGGCATACGAGATGCGTTACCAGTCAGTCAGCCGGACTACHVGGGTWTCTAAT |
| V4_reverse_17 | CAAGCAGAAGACGGCATACGAGATGGAGGCTGAGTCAGTCAGCCGGACTACHVGGGTWTCTAAT |
| V4_reverse_23 | CAAGCAGAAGACGGCATACGAGATTGGCGATTAGTCAGTCAGCCGGACTACHVGGGTWTCTAAT |
| V4_reverse_24 | CAAGCAGAAGACGGCATACGAGATTTCAGCGAAGTCAGTCAGCCGGACTACHVGGGTWTCTAAT |
| V4_reverse_25 | CAAGCAGAAGACGGCATACGAGATTTGGCTATAGTCAGTCAGCCGGACTACHVGGGTWTCTAAT |
| Illumina_E_1 | AATGATACGGCGACCACCGA |
| Illumina_E_2 | CAAGCAGAAGACGGCATACGA |
| V4_read_1 | TATGGTAATTGTGTGCCAGCMGCCGCGGTAA |
| V4_read_2 | AGTCAGTCAGCCGGACTACHVGGGTWTCTAAT |
| V4_index_read | ATTAGAWACCCBDGTAGTCCGGCTGACTGACT |
Illumina sequencing and data analysis
The PCR amplicons from 264 samples (including positive and negative controls) were sequenced over two separate runs on an Illumina Miseq using 500 cycle V2 kits. Sequences were demultiplexed using phylosift (Darling et al., 2014) and read pairs merged using FLASH (Magoc & Salzberg, 2011). Sequences were quality filtered and processed into OTUs using USEARCH v 1.8.1 (Edgar, 2010) (fastq_filter command with the fastq_maxee option set to ‘2’ to remove all sequences with two or more expected errors). Further quality filtering and operational taxonomic unit (OTU) clustering was carried out in QIIME (Caporaso et al., 2010b) version 1.9.0. The split_libraries.py command was used with the –l and –L options set to 240 and 260 respectively, to remove sequences shorter than 240 and longer than 260 base pairs. Sequences were clustered into OTUs at 97% similarity using the pick_open_reference_otus.py script using default settings except that singleton OTUs were removed, and the usearch61 method was used for chimera filtering.
Taxonomy was assigned to OTUs (assign_taxonomy.py) using the UCLUST method (Edgar, 2010) against the Greengenes (DeSantis et al., 2006) database pre-clustered at 97% similarity, accessed from the QIIME website (ftp://greengenes.microbio.me/greengenes_release/gg_13_5/gg_13_8_otus.tar.gz). Representative sequences from each OTU were aligned against the Greengenes alignment using Pynast (Caporaso et al., 2010a) (align_seqs.py), OTUs which failed alignment were filtered from the final OTU table (filter_otus_from_otu_table.py). A phylogenetic tree was built from aligned representative OTU sequences (make_phylogeny.py script) using Fasttree2 (Price, Dehal & Arkin, 2010), with the –r option set to midpoint for tree rooting.
Diabetic skin samples adjacent to wounds were found to be more similar to wound than contralateral skin samples (see Fig. S1), and were removed so as not to confound comparisons between diabetic and non-diabetic skin. To ensure more even sample sizes between the diabetic and non-diabetic groups, only the right foot samples were included from the non-diabetic group for all downstream analyses. Alpha diversity was calculated using Phyloseq (McMurdie & Holmes, 2013) for the observed number of OTUs, Chao 1 and Shannon diversity indices on data rarefied to 30,000 sequences per sample. Significance testing was carried out on alpha diversity estimates using the Wilcoxon rank sum test in R.
Initial beta-diversity analysis was carried out in QIIME on a rarefied OTU table (30K sequences per sample) using the weighted unifrac metric, and the generate_boxplots.py script used to compare unifrac distances between groups of samples. Futher beta diversity analyses, were carried out in Phyloseq, using weighted unifrac distances calculated from an OTU table with raw counts subject to variance stabilising transformation implemented in DEseq2 (Love, Huber & Anders, 2014) as described here (McMurdie & Holmes, 2014). Weighted unifrac distances matrices were also subject to principal coordinates analysis using the Phyloseq package, and significant differences in variance between groups (diabetic and control skin) were determined with PERMANOVA (adonis function) implemented in the Vegan package (Oksanen et al., 2015) in R, using a nested model formula (∼health/subject + subject) and the weighted unifrac distance matrix.
The Wald test for differential abundance was used as implemented in the DESeq2 package in R. Multivariate correlation analysis was carried out against OTUs and wound duration and area using Pearson scores with Bonferroni correction, and p-values were determined via bootstrapping with 100 permutations (implemented in QIIME using the observation_metatdata_correlation.py command). OTU tables were filtered to remove OTUs present in less than 10% of samples for both differential abundance and correlation tests.
A Random forest learning algorithm implemented in R (Liaw & Wiener, 2002) was used to determine if diabetic status could be predicted from the foot skin microbiome. Skin samples were randomly divided into two equal subsets (restricting samples from the same participant to the same subset) for training and testing of learning algorithms. The variance stabilizing transformed OTU table was filtered to include skin samples only, and to remove OTUs observed in less than 10% of samples, and used as the input matrix for the Random forest algorithm. The Random forest fitted on the training subset was created using bootstrapping of one third of the training samples with replacement. As a general practice the rest of the samples were used as a validation set in order to decrease the risk of over-fitting associated with classification algorithms. An optimisation to minimise the out of bag error (classification error on validation data) was used to obtain the optimal number of taxonomic units accessed at each iteration of decision tree creation. Two hundred decision trees consisting of 30 OTUs evaluated at each node of the tree were created. The Random forest model was then used to predict the health status of the subjects in the test subset.
Analysis of the stability of skin microbial communities over time was carried out by comparing intrapersonal weighted unifrac distances between the diabetic and control skin samples, along with intrapersonal distances for all samples. Kruskal–Wallis tests were used to determine significant differences between groups.
Pearson’s Product Moment Correlation was used to test for correlations between wound size or duration and OTU abundance in wound samples as implemented in QIIME (observation_metadata_correlation.py). P-values were calculated using bootstrapping with 100 permutations, and Bonferroni correction for multiple testing. Kruskal-Wallis tests for OTUs that were differentially abundant in healing vs non-healing wounds were implemented in QIIME (group_significance.py). Wounds were classified as healing or non-healing based on a reduction in wound area since the last sampling time (healing) or no change or greater wound size area since the last sampling (non-healing). OTU tables were filtered to remove OTUs present in less than 10% of samples prior to testing.
Inter-visit weighted unifrac distances were compared to the overall degree of healing (1 − (final wound area/initial wound area)) using the lm function of the stats package in R.
Quality filtered sequence data has been deposited in the European Nucleotide Archive under study accession number PRJEB17696. A script containing the code used to process the data in R is provided as supplementary data, along with all the necessary input files, including OTU table and phylogenetic tree.
Results
Cohort characteristics
The diabetic cohort (n = 8) consisted of five males and three females, with an average age of 68.9 ± 8.2 (range 58–81), average BMI of 35.4 ± 5.9 (range 27.2–47.1), and all had at least one foot ulcer which had been present for a average time of 9.1 ± 8.4 months (range 1.5–24 months). All wounds were neuropathic, with the exception of Patient 6 where the wound was ischemic. Two of the eight wounds healed during the course of sampling. Wounds were dressed with either Allevyn foam (Smith and Nephew) to promote moist wound healing, Zetuvit dressing (Hartmann) to remove excess wound exudate, Inadine antimicrobial dressing (10% povidone-iodine) (Johnson and Johnson), or Acticoat flex (antimicrobial silver coated) (Smith and Nephew), as deemed appropriate by the treating podiatrist or wound care nurse. All wounds were located on the plantar aspect of the foot. Details of the specific location of each wound, along with size and treatment over time and are provided in Table S3.
The control cohort (n = 8) consisted of 2 males and 6 females, with an average age of 62.8 ± 13.4 (range 50–81), average BMI of 28.0 ± 6.6 (range 20.4–37.9), and did not have wounds present on the feet.
Sample processing, 16S PCR and sequencing
A total of 242 samples were collected from the diabetic and control cohorts, including 170 skin swabs (85 diabetic and 85 control), 40 wound swabs and 32 wound debridement samples. Full details for samples collected at each time point for each participant can be found in Table S1 (diabetic participants) and Table S2 (control participants).
DNA yields obtained from diabetic skin swabs varied from 0.51 to 600 ng, with a median of 8.5 ng. Three skin samples did not yield enough DNA to be measured by the Qubit assay, however 16S rRNA gene PCR products were still obtained. Control skin sample DNA yields ranged from 0.5 to 41.7 ng (median 5.55), with 20 samples falling below the detection limit of the Qubit assay (<5 pg/µl). Of these 20 samples, PCR products were obtained for all but 3. DNA yields from wound swab samples ranged from 15 ng to 5.6 µg (median 760 ng) and for wound debridement samples ranged from 170 ng to 5.8 µg (median 1.2 µg). One wound swab sample did not yield enough DNA to be detected. Negative control swabs (n =4) did not yield enough DNA to be detected, and also did not yield detectable PCR products.
PCR products from the V4 region of the 16S rRNA gene were obtained for 257 of the 273 samples collected. Repeated attempts were made with increased amounts of template for those samples that did not initially yield a PCR product, however no PCR product was obtained (detailed in Tables S1 and S2). Amplicons from the remaining 257 samples were pooled and paired-end sequenced over two separate MiSeq runs with V2-500 cycle kits. Sample from four diabetic and four control subjects were sequenced in each run (Table S4). A median coverage of 73,599 sequences per sample was obtained (minimum 1,683, maximum 297,817). Negative controls (two blank swab and 2 no DNA PCR controls) had between 1,508 and 27,840 sequences assigned. The final sequencing coverage obtained for each sample can be found in Table S4 . Because negative control samples contained taxa that are similar to those found on skin (e.g., Staphylococcus, Corynebacterium and Acinetobacter) specific taxa were not removed from the data, rather samples with less than 30,000 sequences (n = 5) were removed from the analysis, based on the highest level of sequencing reads obtained from negative controls. A PERMANOVA test was run on a weighted unfrac distance matrix generated from variance stabilising transformed counts to assess the amount of variance attributable to the two different sequencing runs, (run + subject). Sequencing run was a significant factor accounting for 3.0% of the variance (p < 0.001), while inter-individual differences accounted for 34.5% (p < 0.001).
The microbiome of diabetic skin is less diverse than control skin
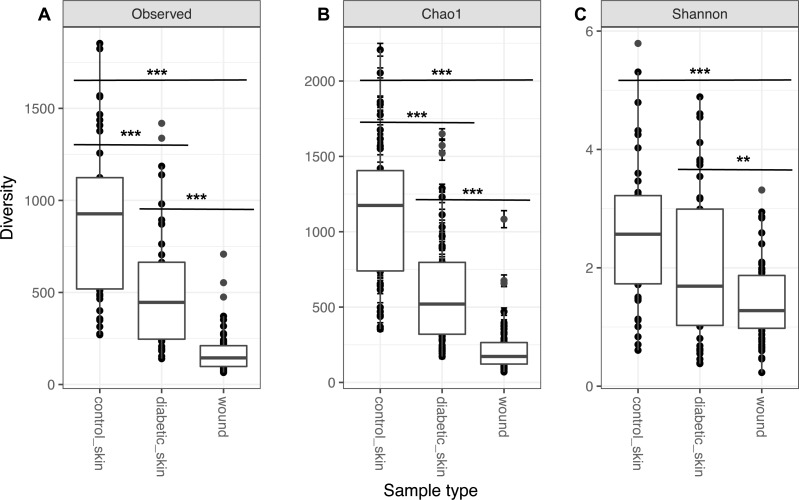
Diversity in all three groups was significantly different for observed richness, Chao1 and Shannon diversity indices (likelihood ratio test, p < 0.01). Diabetic skin was significantly less diverse than control skin for richness and Chao1 indices (Wilcoxon rank sum test, p < 0.01) (Fig. 1). Control skin had a median of 998.5 observed OTUs, compared to 435 for diabetic skin. Wounds were also significantly less diverse than diabetic skin with a median of 145 observed OTUs.
Figure 1. Alpha diversity of skin and wounds.
Box plots of 3 different alpha diversity measures, (A) observed number of OTUs or richness, (B) the Chao I estimator, and (C) the Shannon index, based on OTUs clustered at 97% similarity for control skin, diabetic skin and diabetic wounds. Significant differences are indicated by asterix ∗ = p < 0.05, ∗∗ = p < 0.01 ∗∗∗ = p < 0.001.
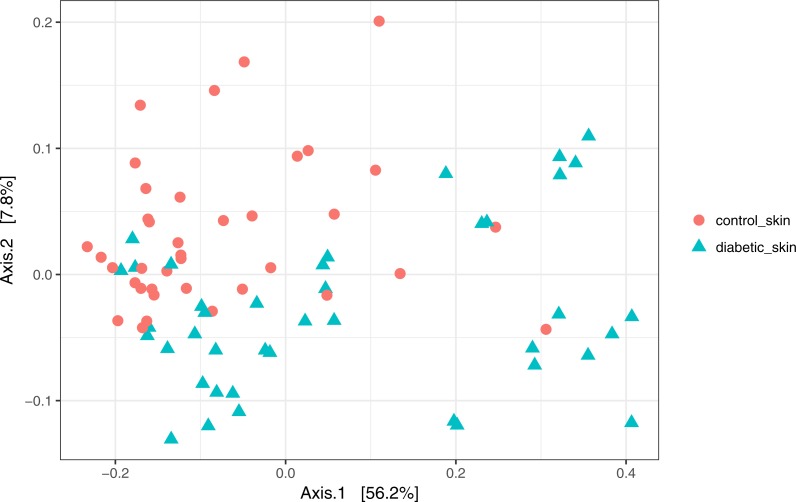
The skin microbiome is significantly different between diabetic and control subjects
Skin microbial communities overall were significantly different between diabetic and control skin (Fig. 2). A clear distinction can be observed between the sample types, and this was confirmed by a PERMANOVA test (∼health/subject + health), where health (diabetes vs control) was a significant factor accounting for 11.7% of the variance (R2 = 0.117, p = 0.001). Subject (inter-individual differences) was the most significant factor accounting for 34.6% of the observed variance (R2 = 0.346, p = 0.001).
Figure 2. Principal coordinates analysis of diabetic and control skin samples.
Distances are based on the weighted unifrac metric, calculated using raw counts subjected to a variance stabilising transformation.
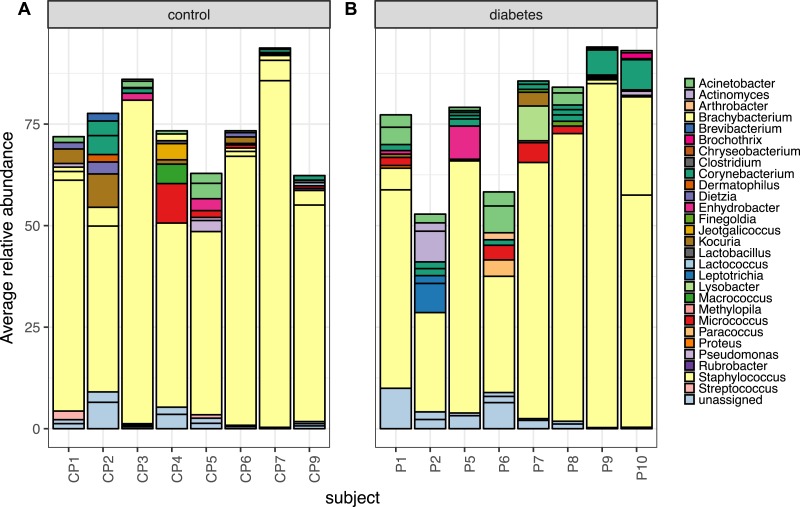
Abundant taxa from skin are similar between persons with diabetes and healthy controls
Despite the clear distinction between diabetic and control skin in the PCoA plot above, the most abundant taxa from both groups were similar. Foot skin communities from diabetic skin were dominated by the genera Staphylococcus, followed by Acinetobacter and Corynebacterium, then unclassified Enterobacteriacea. Control skin was dominated by the genera Staphylococcus, followed by Acinetobacter, Kocuria, Corynebacterium and Micrococcus, (Fig. 3).
Figure 3. The top 10 most abundant OTUs in diabetic and control skin per subject.
The top 10 most abundant OTUs in (A) control and (B) diabetic skin per subject. Average abundances per person were calculated from data rarefied to 30,000 sequences per sample. Genus assigned taxonomy is indicated in the legend, individual OTUs of the same genera are indicated with black lines.
To determine which OTUs were contributing to the significant difference detected in the PERMANOVA analysis, the Wald test as implemented in the DESeq2 package (Love, Huber & Anders, 2014), was carried out. Sixty-nine OTUs were identified as significantly different in abundance (adjusted p < 0.05), all with an average abundance of less than 1%. A full list of the results can be found in Table S5. Similar results were found when re-running the analysis at the Genera level, with 24 genera identified as significantly different, but all at an average relative abundance of less then 1% (Table S6).
The foot skin microbiome may predict diabetic status
Despite only low abundance OTUs showing significant differences between diabetic and non-diabetic skin, a Random Forrest classifier was able to predict diabetic status from the foot skin microbiome. The model achieved an overall accuracy of 85.0%, with a sensitivity of 79.2%, and specificity of 93.8%. The negative predictive value (75.0%) was lower than the positive predictive value (95.0%). The classifier’s Gini index provided a list of 106 OTUs that were important in the classification task (Table S7); the majority were low abundance OTUs (103 OTUs < 1% average relative abundance), and the majority of these were more abundant in control than diabetic skin (75 OTUs).
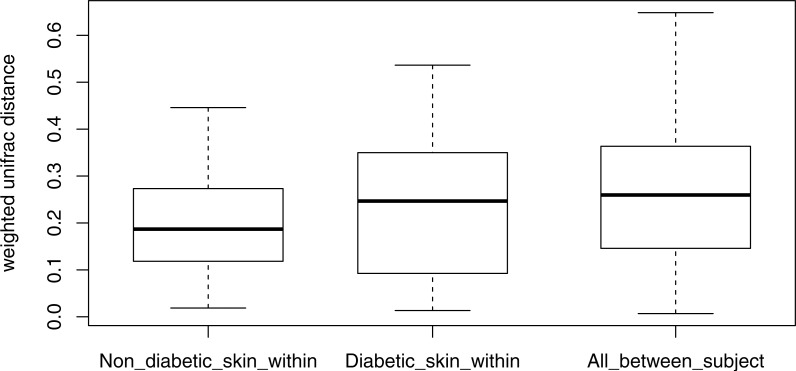
Stability of the diabetic skin microbiome over time
Longitudinal analysis of the skin microbiome over time showed a trend of lower stability for diabetic skin than non-diabetic skin (Fig. 4), however this difference did not reach significance (p = 0.09), while both control and diabetic skin intrapersonal differences over time were significantly smaller (i.e., more stable) than inter-individual differences (p < 0.05).
Figure 4. Boxplots of intra-individual differences over time in diabetic and non-diabetic skin microbial communities.
Inter-individual distances are also shown for comparison. The stability of non-diabetic skin was higher (i.e., lower distances over time) than for diabetic skin, however this difference did not reach significance. (Kolmogorov–Smirnov test, p = 0.09).
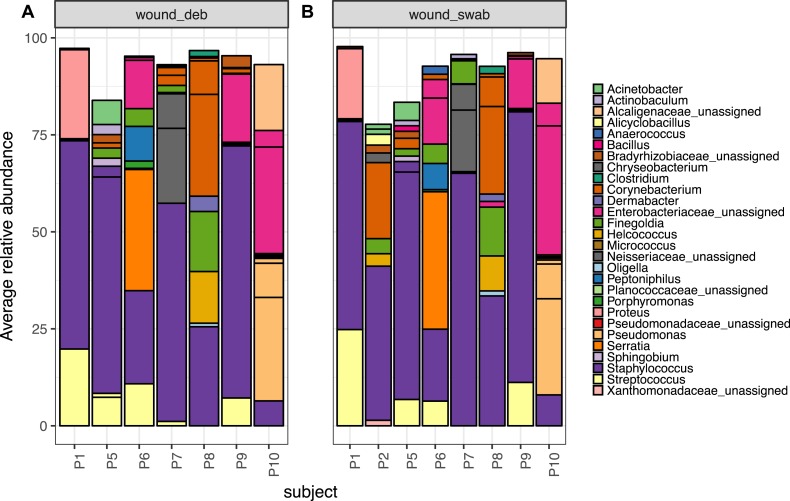
Microbiota of chronic diabetic wounds overlap with skin and differ between patient
Wound swab and debridement samples were similar in taxonomic composition, and the top ten OTUs from all wounds per patient are shown in Fig. 5. The most abundant OTU detected in wounds was also the most abundant OTU found on skin, Staphylococcus sp. (OTU 1084865), and was present in the wounds of all eight patients. Other skin associated OTUs found in wounds included Corynebacterium (OTU 1011712), which was in the top 10 OTUs in six out of eight patient’s wounds.
Figure 5. The top 10 abundant OTUs in wounds per subject.
The top 10 abundant OTUs per subject in diabetic (A) wound debridement and (B) wound swab samples. Average abundances per group were calculated from data rarefied to 30,000 sequences per sample. Genus assigned taxonomy is indicated in the legend, or family level where genus was unassigned. Individual OTUs of the same genera are indicated with black lines.
The Wald test for differential abundance between diabetic skin and wounds identified four OTUs that were significantly more abundant across all wounds (two classified as Enterobactericaeae, one as Serratia and one as Finegoldia). The complete list of results can be found in Table S8.
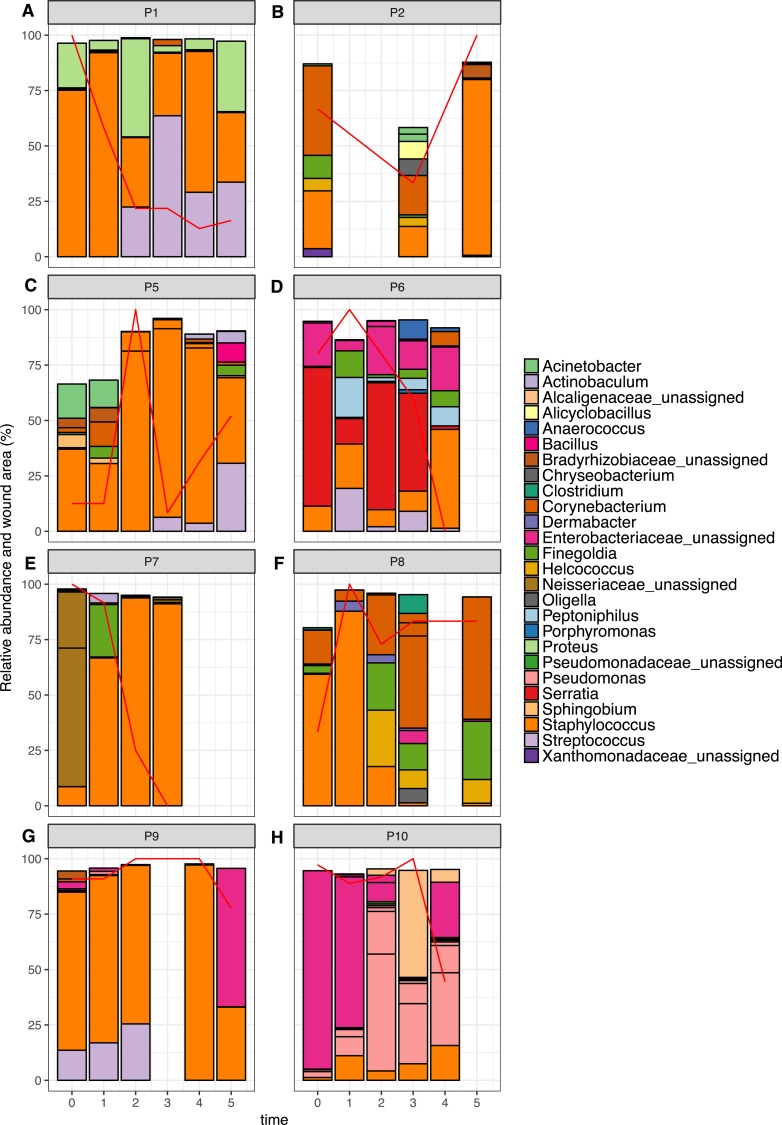
The top 10 OTUs in wounds per patient over time are shown in Fig. 6. Of the eight wounds, six are dominated by the most abundant skin OTU, at the majority of time points measured (Staphylococcus OTU 1084865). Only Patients 6 and 10 showed wound profiles dominated by non-skin associated taxa across the time period surveyed. No significant correlations were found between any abundant OTUs (average abundance > 1%) and wound duration or healing status. No significant correlation was found between the overall degree of wound healing, and inter-visit weighted unifrac distances in individual wounds (Fig. S2, p = 0.29). However, some interesting observations were made that correlated to clinical events. For example, the wound of Patient 6 had been present for 24 months at the start of the study. It was dominated by Enterobacteriacaea and showed little healing until time point 3, which coincided with an angioplasty procedure to improve blood flow to the foot. This was followed by resolution of the wound within two weeks. When Patient 7 presented to the clinic, the wound had been present for 12 months, and was dominated by an OTU from the Neisseriaceae family. Following the standard treatment of debridement and wound dressing, rapid healing was observed, as well as a shift to a community dominated by the most abundant skin OTU.
Figure 6. Relative abundance of the top 10 OTUs per patient over time.
Patients 1–10 are represented individually in (A–H). Wound area is overlaid as a red line and is represented as a percentage of the largest wound area measured over time. Relative abundances were calculated from data rarefied to 30,000 sequences per sample. Genus assigned taxonomy is indicated in the legend, or family level where genus was unassigned. Individual OTUs of the same genera are indicated with black lines.
Discussion
This study aimed to compare the skin microbiome between persons with diabetes and healthy control individuals over time. We additionally sought to characterise the wound microbiota in diabetic foot ulcers over time and determine if any members of the skin microbiome were correlated to the wound microbiome or wound healing.
The microbiome from diabetic skin was significantly different to that of control skin, however this difference was not driven by the most abundant members of the skin community. The top 10 most abundant OTUs per person were similar in abundance and not significantly different between groups. Many low abundance OTUs were identified as significantly different, with the vast majority of these being more abundant in control skin. One limitation of this study is that, although commonly used in microbiome studies (Cope et al., 2017; David et al., 2014; Halfvarson et al., 2017; Smith et al., 2016), the V4 region of the 16S rRNA gene does not allow differentiation between Staphylococcus aureus and other Staphylococcus species found on skin, such as Staphylococcus epidermidis (Conlan, Kong & Segre, 2012). Additionally, the V4 primers have mismatches that prevent detection of Propionibacterium, an important genera in the skin microbiome (Kuczynski et al., 2011). The clinical consequences of these organisms may be important, and this should be taken into consideration for the experimental design of future studies (Gohl et al., 2016; Meisel et al., 2016).
We observed a significant reduction in alpha diversity and a trend of decreased stability (non-significant) of diabetic skin microbiomes compared to non-diabetic skin. This is in contrast to a previous study of diabetic skin (Redel et al., 2013) where the opposite result was observed. It is possible that changes to the skin environment associated with diabetes, such as increased pH (Yosipovitch et al., 1993) advanced glycation end products in the skin matrix (Gkogkolou & Bohm, 2012), or increased levels of skin inflammation (Tellechea et al., 2013) could drive a decrease in diversity. It is also possible that activities associated with diabetes, such as increased exposure to antibiotics (Mor et al., 2016), contribute to the observed effect despite our attempts to control for recent antibiotic exposure as a confounding variable. Another limitation of the current study is the small sample size, and as such this result should be confirmed on a larger cohort.
If skin microbiome diversity is depleted in people with diabetes, what are the implications for the health of diabetic skin? While in some body sites an increase is microbial diversity is associated with disease states, particularly the vagina (Van de Wijgert et al., 2014), decreased diversity of the microbiome has frequently been correlated with disease and inflammation in the skin (Alekseyenko et al., 2013; Ellebrecht et al., 2016; Seite et al., 2014; Williams & Gallo, 2015), gut (Giloteaux et al., 2016; Sze & Schloss, 2016) and airways (Yu et al., 2015). However it is not known whether decreased diversity in these sites is a cause or merely an indicator of inflammation. Diversity is commonly used as an indicator of ecosystem health, with decreased diversity typically signalling a disturbed and less resilient state (Oliver et al., 2015). In the context of the human skin microbiome, decreased diversity could allow potential pathogens to overgrow, and these may be capable of triggering inflammation and triggering or exacerbating a disease state. Alternatively, inflammation could be triggered by genetic and environmental factors, and the inflammation itself could drive down bacterial diversity by creating an inhospitable growth environment.
Patients with diabetes enrolled in this study had no exposure to antibiotics within the previous four weeks, so as not to confound the comparison between diabetic and control skin. This meant that the foot ulcers analysed in this study were considered to be clinically non-infected wounds. No significant correlations were found between any OTU in diabetic skin or wounds with wound size, duration or healing status. This is possibly due to the small sample size, as a previous study found correlations between the relative abundance of specific bacterial taxa and ulcer duration and depth (e.g., Staphylococcus was negatively correlated with wound duration) (Gardner et al., 2013). Another possible limitation of this study is the use of the z-swab method which samples across the entire wound base regardless of size, as this will possibly increase heterogeneity with increasing wound size.
A recent longitudinal study of wounds found a negative correlation between wound microbiota stability and time to heal (Loesche et al., 2017). We did not find any such correlation here when comparing degree of healing to between visit weighted unifrac distances (Fig. S2), although again our sample size was smaller, as was the length of time patients were followed.
The overall composition of the diabetic wound microbiota described here is in agreement with a survey of 910 chronic diabetic foot ulcers, where a dominance of Staphylococcus, as well as Pseudomonas, Corynebacterium, Streptococcus and Finegoldia (among others) was found (Wolcott et al., 2016). Gardner et al. (2013) found that diabetic ulcers clustered into three types, depending on the dominant taxa in the wounds, which were Staphylococcus, Streptococcus, or a mixture of anaerobic bacteria or Proteobacteria. Similar results were found in a later study where two wound clusters were dominated by either Staphylococcus or Streptococcus, and genera such as Corynebacterium and Finegoldia were frequently observed (Loesche et al., 2017). These same genera were observed in most wounds here, while other genera such as Serratia and Proteus were specific to individuals.
Other studies of diabetic foot ulcers have reported contrasting results, such as a dominance of Corynebacterium (Dowd et al., 2008), while a recent study found that Staphylococcus were common in new ulcers, but not in recurring ulcers (Smith et al., 2016). One trend that was consistent across several studies was that the microbial profile from diabetic ulcers was variable, with no one typical diabetic ulcer microbiota apparent.
Conclusions
The major effect associated with diabetes observed here was a significant reduction in the diversity of the skin microbiome. The cohort of this study was small, and these observations should be verified in a larger study. The long-term effects of reduced diversity are not yet well understood, but low diversity continues to be linked to disease and poor health outcomes (Hua et al., 2016; Miller et al., 2016; Rook, 2013). One possible effect is increased infection susceptibility (Seto et al., 2014), and it is intriguing to consider whether decreased skin microbiome diversity could be contributing to the high incidence of skin and wound infections associated with this disease (Peleg et al., 2007). There are, of course, many other well-documented factors such as immune dysfunction that can contribute to an increased rate of infections (Geerlings & Hoepelman, 1999); however, the skin microbiome may be an as yet unconsidered contributor to this phenomenon.
Supplemental Information
Sample types are indicated in the second column: skin swab from an area adjacent to the foot wound (SA), skin swab from the contralateral foot (SC), wound swab (WS) and debrided wound tissue (WD). A tick (x) indicates that a sample was collected, a cross (x) indicates that no samples for that time point were collected because the patient could not make their scheduled appointment, and NC indicates that a sample was not collected because podiatry staff deemed there was not sufficient tissue available for a debridement sample. In the case that a wound healed (indicated by WH) no further samples were collected for that patient. In the case of P4, the contralateral foot had previously been amputated, and the foot containing the wound was amputated after time point 2. Samples for which a 16S rRNA gene PCR product was not obtained are indicated with (x).
Sample types are indicated in the second column: skin swab from the base of the left foot (L), or right foot (F). A tick (x) indicates that a sample was collected, a cross (x) indicates that no samples for that time point were collected because the subject was not available. Samples for which a 16S rRNA gene PCR product was not obtained are indicated with (x). Control subject 8 (CP8) was removed from the study as not enough samples were collected.
Wound size is shown as height × width × depth in mm. All wounds were routinely irrigated with Prontosan solution, followed by dressing with either Allevyn foam for moist wound healing, Zetuvit dressing to remove excess wound exudate, Inadine antimicrobial dressing (10% povidone-iodine), or Acticoat flex (silver coated antimicrobial dressing). Decisions on wound dressing were made by the treating podiatrist or wound care nurse.
Coverage before and after quality filtering for each sample is indicated, along with the sequencing run that each sample was sequenced in.
The Wald test was used as implemented in DESeq2. The model health + subject:health was used, and the OTU table was filtered to remove OTUs with a count of less than 2, and/or present in less than 10% of samples. Log2FC was calculated relative to the control skin samples.
The Wald test was used as implemented in DESeq2. The model health + subject:health was used, and OTUs were collapsed into genera level classifications. The original OTU table was filtered to remove OTUs with a count of less than 2, and/or present in less than 10% of samples. Log2FC was calculated relative to the control skin samples.
OTUs important to the classification in the Random Forrest Model calculated using the GINI index.
The Wald test was used as implemented in DESeq2. The model sampletype + sampletype:health was used, and the OTU table was filtered to remove OTUs present in less than 20% of samples. Log2FC was calculated relative to the diabetic skin samples.
Comparison as adjacent diabetic skin to wound swabs (adj_V_ws), contralateral diabetic skin to wound swabs (con_V_ws), adjacent diabetic skin to wound debridement (adj_V_wd), and contralateral diabetic skin to wound debridement (con_V_ws). Small but statistically significant differences were observed, such that there was greater similarity between adjacent skin and wounds compared to contralateral skin and wounds. Significant differences are indicated with ∗∗∗(p < 0.001).
Inter-visit weighted unifrac distances from wound swabs for individual patients were plotted against the degree of healing, where 1 equals complete healing, 0 equals no change in wound size and negative numbers indicate and increase in wound size. No significant correlation was found using a linear model.
Acknowledgments
We would like to acknowledge Westmead Hospital and the Podiatry Clinic Staff who kindly assisted in the collection of samples. We also acknowledge Professor Mark Morrison and Dr Paraic O. Cuiv for helpful discussions about the study design.
Funding Statement
Funding for this study was provided by internal grants from the University of Technology Sydney. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Additional Information and Declarations
Competing Interests
The authors declare there are no competing interests.
Author Contributions
Melissa Gardiner performed the experiments, analyzed the data, wrote the paper, prepared figures and/or tables, reviewed drafts of the paper.
Mauro Vicaretti, Jill Sparks and Michael Liu performed the experiments, reviewed drafts of the paper.
Sunaina Bansal and Stephen Bush analyzed the data, reviewed drafts of the paper.
Aaron Darling contributed reagents/materials/analysis tools, reviewed drafts of the paper.
Elizabeth Harry conceived and designed the experiments, contributed reagents/materials/analysis tools, reviewed drafts of the paper.
Catherine M. Burke conceived and designed the experiments, performed the experiments, analyzed the data, contributed reagents/materials/analysis tools, wrote the paper, prepared figures and/or tables, reviewed drafts of the paper.
Human Ethics
The following information was supplied relating to ethical approvals (i.e., approving body and any reference numbers):
Ethical approval for the study was obtained from both the University of Technology Sydney Human Research Ethics Committee (approval number 2013000170), and the Western Sydney Local Health District Human Research Ethics Committee (approval number HREC2013/9/5.3(3809) AU RED LNR/13/WMEAD/294). Diabetic individuals and control subjects provided written consent for sample collection and all subsequent analyses.
Data Availability
The following information was supplied regarding data availability:
Quality filtered sequence data has been deposited in the European Nucleotide Archive under study accession number PRJEB17696.
References
- Alekseyenko et al. (2013).Alekseyenko AV, Perez-Perez GI, De Souza A, Strober B, Gao Z, Bihan M, Li K, Methe BA, Blaser MJ. Community differentiation of the cutaneous microbiota in psoriasis. Microbiome. 2013;1:31. doi: 10.1186/2049-2618-1-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Australian Institute of Health and Welfare (2008).Australian Institute of Health and Welfare . Diabetes: Australian Facts 2008. AIHW; Canberra: 2008. [Google Scholar]
- Behm et al. (2012).Behm B, Schreml S, Landthaler M, Babilas P. Skin signs in diabetes mellitus. Journal of the European Academy of Dermatology and Venereology. 2012;26:1203–1211. doi: 10.1111/j.1468-3083.2012.04475.x. [DOI] [PubMed] [Google Scholar]
- Bomar et al. (2016).Bomar L, Brugger SD, Yost BH, Davies SS, Lemon KP. Corynebacterium accolens releases antipneumococcal free fatty acids from human nostril and skin surface triacylglycerols. mBio. 2016;7:e01725–01715. doi: 10.1128/mBio.01725-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caporaso et al. (2010a).Caporaso JG, Bittinger K, Bushman FD, DeSantis TZ, Andersen GL, Knight R. PyNAST: a flexible tool for aligning sequences to a template alignment. Bioinformatics. 2010a;26:266–267. doi: 10.1093/bioinformatics/btp636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caporaso et al. (2010b).Caporaso JG, Kuczynski J, Stombaugh J, Bittinger K, Bushman FD, Costello EK, Fierer N, Pena AG, Goodrich JK, Gordon JI, Huttley GA, Kelley ST, Knights D, Koenig JE, Ley RE, Lozupone CA, McDonald D, Muegge BD, Pirrung M, Reeder J, Sevinsky JR, Turnbaugh PJ, Walters WA, Widmann J, Yatsunenko T, Zaneveld J, Knight R. QIIME allows analysis of high-throughput community sequencing data. Nature Methods. 2010b;7:335–336. doi: 10.1038/nmeth.f.303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caporaso et al. (2012).Caporaso JG, Lauber CL, Walters WA, Berg-Lyons D, Huntley J, Fierer N, Owens SM, Betley J, Fraser L, Bauer M, Gormley N, Gilbert JA, Smith G, Knight R. Ultra-high-throughput microbial community analysis on the Illumina HiSeq and MiSeq platforms. ISME Journal. 2012;6:1621–1624. doi: 10.1038/ismej.2012.8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cogen et al. (2010a).Cogen AL, Yamasaki K, Muto J, Sanchez KM, Crotty Alexander L, Tanios J, Lai Y, Kim JE, Nizet V, Gallo RL. Staphylococcus epidermidis antimicrobial delta-toxin (phenol-soluble modulin-gamma) cooperates with host antimicrobial peptides to kill group A Streptococcus. PLOS ONE. 2010a;5:e8557. doi: 10.1371/journal.pone.0008557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cogen et al. (2010b).Cogen AL, Yamasaki K, Sanchez KM, Dorschner RA, Lai Y, MacLeod DT, Torpey JW, Otto M, Nizet V, Kim JE, Gallo RL. Selective antimicrobial action is provided by phenol-soluble modulins derived from Staphylococcus epidermidis, a normal resident of the skin. Journal of Investigative Dermatology. 2010b;130:192–200. doi: 10.1038/jid.2009.243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conlan, Kong & Segre (2012).Conlan S, Kong HH, Segre JA. Species-level analysis of DNA sequence data from the NIH Human Microbiome Project. PLOS ONE. 2012;7:e47075. doi: 10.1371/journal.pone.0047075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cope et al. (2017).Cope EK, Goldberg AN, Pletcher SD, Lynch SV. Compositionally and functionally distinct sinus microbiota in chronic rhinosinusitis patients have immunological and clinically divergent consequences. Microbiome. 2017;5:53. doi: 10.1186/s40168-017-0266-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Darling et al. (2014).Darling AE, Jospin G, Lowe E, Matsen FAt, Bik HM, Eisen JA. PhyloSift: phylogenetic analysis of genomes and metagenomes. PeerJ. 2014;2:e243. doi: 10.7717/peerj.243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- David et al. (2014).David LA, Maurice CF, Carmody RN, Gootenberg DB, Button JE, Wolfe BE, Ling AV, Devlin AS, Varma Y, Fischbach MA, Biddinger SB, Dutton RJ, Turnbaugh PJ. Diet rapidly and reproducibly alters the human gut microbiome. Nature. 2014;505:559–563. doi: 10.1038/nature12820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DeSantis et al. (2006).DeSantis TZ, Hugenholtz P, Larsen N, Rojas M, Brodie EL, Keller K, Huber T, Dalevi D, Hu P, Andersen GL. Greengenes, a chimera-checked 16S rRNA gene database and workbench compatible with ARB. Applied and Environmental Microbiology. 2006;72:5069–5072. doi: 10.1128/AEM.03006-05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dowd et al. (2008).Dowd SE, Wolcott RD, Sun Y, McKeehan T, Smith E, Rhoads D. Polymicrobial nature of chronic diabetic foot ulcer biofilm infections determined using bacterial tag encoded FLX amplicon pyrosequencing (bTEFAP) PLOS ONE. 2008;3:e3326. doi: 10.1371/journal.pone.0003326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edgar (2010).Edgar RC. Search and clustering orders of magnitude faster than BLAST. Bioinformatics. 2010;26:2460–2461. doi: 10.1093/bioinformatics/btq461. [DOI] [PubMed] [Google Scholar]
- Ellebrecht et al. (2016).Ellebrecht CT, Srinivas G, Bieber K, Banczyk D, Kalies K, Kunzel S, Hammers CM, Baines JF, Zillikens D, Ludwig RJ, Westermann J. Skin microbiota-associated inflammation precedes autoantibody induced tissue damage in experimental epidermolysis bullosa acquisita. Journal of Autoimmunity. 2016;68:14–22. doi: 10.1016/j.jaut.2015.08.007. [DOI] [PubMed] [Google Scholar]
- Fyhrquist et al. (2014).Fyhrquist N, Ruokolainen L, Suomalainen A, Lehtimaki S, Veckman V, Vendelin J, Karisola P, Lehto M, Savinko T, Jarva H, Kosunen TU, Corander J, Auvinen P, Paulin L, Von Hertzen L, Laatikainen T, Makela M, Haahtela T, Greco D, Hanski I, Alenius H. Acinetobacter species in the skin microbiota protect against allergic sensitization and inflammation. Journal of Allergy and Clinical Immunology. 2014;134:1301–1309. doi: 10.1016/j.jaci.2014.07.059. [DOI] [PubMed] [Google Scholar]
- Gardner et al. (2013).Gardner SE, Hillis SL, Heilmann K, Segre JA, Grice EA. The neuropathic diabetic foot ulcer microbiome is associated with clinical factors. Diabetes. 2013;62:923–930. doi: 10.2337/db12-0771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geerlings & Hoepelman (1999).Geerlings SE, Hoepelman AI. Immune dysfunction in patients with diabetes mellitus (DM) FEMS Immunology and Medical Microbiology. 1999;26:259–265. doi: 10.1111/j.1574-695X.1999.tb01397.x. [DOI] [PubMed] [Google Scholar]
- Giloteaux et al. (2016).Giloteaux L, Goodrich JK, Walters WA, Levine SM, Ley RE, Hanson MR. Reduced diversity and altered composition of the gut microbiome in individuals with myalgic encephalomyelitis/chronic fatigue syndrome. Microbiome. 2016;4:30. doi: 10.1186/s40168-016-0171-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gkogkolou & Bohm (2012).Gkogkolou P, Bohm M. Advanced glycation end products: key players in skin aging? Dermato-Endocrinology. 2012;4:259-270. doi: 10.4161/derm.22028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gohl et al. (2016).Gohl DM, Vangay P, Garbe J, MacLean A, Hauge A, Becker A, Gould TJ, Clayton JB, Johnson TJ, Hunter R, Knights D, Beckman KB. Systematic improvement of amplicon marker gene methods for increased accuracy in microbiome studies. Nature Biotechnology. 2016;34:942–949. doi: 10.1038/nbt.3601. [DOI] [PubMed] [Google Scholar]
- Guariguata et al. (2014).Guariguata L, Whiting DR, Hambleton I, Beagley J, Linnenkamp U, Shaw JE. Global estimates of diabetes prevalence for 2013 and projections for 2035. Diabetes Research and Clinical Practice. 2014;103:137–149. doi: 10.1016/j.diabres.2013.11.002. [DOI] [PubMed] [Google Scholar]
- Halfvarson et al. (2017).Halfvarson J, Brislawn CJ, Lamendella R, Vazquez-Baeza Y, Walters WA, Bramer LM, D’Amato M, Bonfiglio F, McDonald D, Gonzalez A, McClure EE, Dunklebarger MF, Knight R, Jansson JK. Dynamics of the human gut microbiome in inflammatory bowel disease. Nature Microbiology. 2017;2:17004. doi: 10.1038/nmicrobiol.2017.4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hua et al. (2016).Hua X, Goedert JJ, Pu A, Yu G, Shi J. Allergy associations with the adult fecal microbiota: analysis of the American Gut Project. EBioMedicine. 2016;3:172–179. doi: 10.1016/j.ebiom.2015.11.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iwase et al. (2010).Iwase T, Uehara Y, Shinji H, Tajima A, Seo H, Takada K, Agata T, Mizunoe Y. Staphylococcus epidermidis Esp inhibits Staphylococcus aureus biofilm formation and nasal colonization. Nature. 2010;465:346–349. doi: 10.1038/nature09074. [DOI] [PubMed] [Google Scholar]
- Kanno et al. (2011).Kanno E, Kawakami K, Ritsu M, Ishii K, Tanno H, Toriyabe S, Imai Y, Maruyama R, Tachi M. Wound healing in skin promoted by inoculation with Pseudomonas aeruginosa PAO1: the critical role of tumor necrosis factor-alpha secreted from infiltrating neutrophils. Wound Repair and Regeneration. 2011;19:608–621. doi: 10.1111/j.1524-475X.2011.00721.x. [DOI] [PubMed] [Google Scholar]
- Karlsson et al. (2013).Karlsson FH, Tremaroli V, Nookaew I, Bergstrom G, Behre CJ, Fagerberg B, Nielsen J, Backhed F. Gut metagenome in European women with normal, impaired and diabetic glucose control. Nature. 2013;498:99–103. doi: 10.1038/nature12198. [DOI] [PubMed] [Google Scholar]
- Kelly et al. (2015).Kelly CJ, Zheng L, Campbell EL, Saeedi B, Scholz CC, Bayless AJ, Wilson KE, Glover LE, Kominsky DJ, Magnuson A, Weir TL, Ehrentraut SF, Pickel C, Kuhn KA, Lanis JM, Nguyen V, Taylor CT, Colgan SP. Crosstalk between microbiota-derived short-chain fatty acids and intestinal epithelial HIF augments tissue barrier function. Cell Host & Microbe. 2015;17:662–671. doi: 10.1016/j.chom.2015.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuczynski et al. (2011).Kuczynski J, Lauber CL, Walters WA, Parfrey LW, Clemente JC, Gevers D, Knight R. Experimental and analytical tools for studying the human microbiome. Nature Reviews Genetics. 2011;13:47–58. doi: 10.1038/nrg3129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lai et al. (2010).Lai Y, Cogen AL, Radek KA, Park HJ, Macleod DT, Leichtle A, Ryan AF, Di Nardo A, Gallo RL. Activation of TLR2 by a small molecule produced by Staphylococcus epidermidis increases antimicrobial defense against bacterial skin infections. Journal of Investigative Dermatology. 2010;130:2211–2221. doi: 10.1038/jid.2010.123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lai et al. (2009).Lai Y, Di Nardo A, Nakatsuji T, Leichtle A, Yang Y, Cogen AL, Wu ZR, Hooper LV, Schmidt RR, Von Aulock S, Radek KA, Huang CM, Ryan AF, Gallo RL. Commensal bacteria regulate Toll-like receptor 3-dependent inflammation after skin injury. Nature Medicine. 2009;15:1377–1382. doi: 10.1038/nm.2062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lauber et al. (2010).Lauber CL, Zhou N, Gordon JI, Knight R, Fierer N. Effect of storage conditions on the assessment of bacterial community structure in soil and human-associated samples. FEMS Microbiology Letters. 2010;307:80–86. doi: 10.1111/j.1574-6968.2010.01965.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liaw & Wiener (2002).Liaw A, Wiener M. Classification and Regression by randomForest. R News. 2002;2:18–22. [Google Scholar]
- Loesche et al. (2017).Loesche M, Gardner SE, Kalan L, Horwinski J, Zheng Q, Hodkinson BP, Tyldsley AS, Franciscus CL, Hillis SL, Mehta S, Margolis DJ, Grice EA. Temporal stability in chronic wound microbiota is associated with poor healing. Journal of Investigative Dermatology. 2017;137:237–244. doi: 10.1016/j.jid.2016.08.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Love, Huber & Anders (2014).Love MI, Huber W, Anders S. Moderated estimation of fold change and dispersion for RNA-seq data with DESeq2. Genome Biology. 2014;15:550. doi: 10.1186/s13059-014-0550-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Magoc & Salzberg (2011).Magoc T, Salzberg SL. FLASH: fast length adjustment of short reads to improve genome assemblies. Bioinformatics. 2011;27:2957–2963. doi: 10.1093/bioinformatics/btr507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McMurdie & Holmes (2013).McMurdie PJ, Holmes S. phyloseq: an R package for reproducible interactive analysis and graphics of microbiome census data. PLOS ONE. 2013;8:e61217. doi: 10.1371/journal.pone.0061217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McMurdie & Holmes (2014).McMurdie PJ, Holmes S. Waste not, want not: why rarefying microbiome data is inadmissible. PLOS Computational Biology. 2014;10:e1003531. doi: 10.1371/journal.pcbi.1003531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meisel et al. (2016).Meisel JS, Hannigan GD, Tyldsley AS, SanMiguel AJ, Hodkinson BP, Zheng Q, Grice EA. Skin microbiome surveys are strongly influenced by experimental design. Journal of Investigative Dermatology. 2016;136:947–956. doi: 10.1016/j.jid.2016.01.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller et al. (2016).Miller GE, Engen PA, Gillevet PM, Shaikh M, Sikaroodi M, Forsyth CB, Mutlu E, Keshavarzian A. Lower neighborhood socioeconomic status associated with reduced diversity of the colonic microbiota in healthy adults. PLOS ONE. 2016;11:e0148952. doi: 10.1371/journal.pone.0148952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mor et al. (2016).Mor A, Berencsi K, Nielsen JS, Rungby J, Friborg S, Brandslund I, Christiansen JS, Vaag A, Beck-Nielsen H, Sorensen HT, Thomsen RW. Rates of community-based antibiotic prescriptions and hospital-treated infections in individuals with and without type 2 diabetes: a Danish nationwide cohort study, 2004–2012. Clinical Infectious Diseases. 2016;63:501–511. doi: 10.1093/cid/ciw345. [DOI] [PubMed] [Google Scholar]
- Oksanen et al. (2015).vegan: community Ecology Package. https://cran.r-project.org/web/packages/vegan/index.html. Oksanen J, Blanchet FG, Kindt R, Legendre P, Minchin PR, O’Hara RB, Simpson GL, Solymos P, Henry M, Stevens H, Wagner H. 2005
- Oliver et al. (2015).Oliver TH, Heard MS, Isaac NJ, Roy DB, Procter D, Eigenbrod F, Freckleton R, Hector A, Orme CD, Petchey OL, Proenca V, Raffaelli D, Suttle KB, Mace GM, Martin-Lopez B, Woodcock BA, Bullock JM. Biodiversity and resilience of ecosystem functions. Trends in Ecology & Evolution. 2015;30:673–684. doi: 10.1016/j.tree.2015.08.009. [DOI] [PubMed] [Google Scholar]
- Parekh et al. (2016).Parekh PJ, Nayi VR, Johnson DA, Vinik AI. The role of gut microflora and the cholinergic anti-inflammatory neuroendocrine system in diabetes mellitus. Frontiers in Endocrinology. 2016;7:55. doi: 10.3389/fendo.2016.00055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peleg et al. (2007).Peleg AY, Weerarathna T, McCarthy JS, Davis TM. Common infections in diabetes: pathogenesis, management and relationship to glycaemic control. Diabetes/Metabolism Research and Reviews. 2007;23:3–13. doi: 10.1002/dmrr.682. [DOI] [PubMed] [Google Scholar]
- Price, Dehal & Arkin (2010).Price MN, Dehal PS, Arkin AP. FastTree 2–approximately maximum-likelihood trees for large alignments. PLOS ONE. 2010;5:e9490. doi: 10.1371/journal.pone.0009490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qin et al. (2012).Qin J, Li Y, Cai Z, Li S, Zhu J, Zhang F, Liang S, Zhang W, Guan Y, Shen D, Peng Y, Zhang D, Jie Z, Wu W, Qin Y, Xue W, Li J, Han L, Lu D, Wu P, Dai Y, Sun X, Li Z, Tang A, Zhong S, Li X, Chen W, Xu R, Wang M, Feng Q, Gong M, Yu J, Zhang Y, Zhang M, Hansen T, Sanchez G, Raes J, Falony G, Okuda S, Almeida M, LeChatelier E, Renault P, Pons N, Batto JM, Zhang Z, Chen H, Yang R, Zheng W, Li S, Yang H, Wang J, Ehrlich SD, Nielsen R, Pedersen O, Kristiansen K, Wang J. A metagenome-wide association study of gut microbiota in type 2 diabetes. Nature. 2012;490:55–60. doi: 10.1038/nature11450. [DOI] [PubMed] [Google Scholar]
- Redel et al. (2013).Redel H, Gao Z, Li H, Alekseyenko AV, Zhou Y, Perez-Perez GI, Weinstock G, Sodergren E, Blaser MJ. Quantitation and composition of cutaneous microbiota in diabetic and nondiabetic men. Journal of Infectious Diseases. 2013;207:1105–1114. doi: 10.1093/infdis/jit005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reiber, Boyko & Smith (1995).Reiber GE, Boyko EJ, Smith DG. Lower extremity foot ulcers and amputations in diabetes. In: NDDG, editor. Diabetes in America. 2nd edition. Bethsada: National Institutes of Health; 1995. [Google Scholar]
- Rice et al. (2014).Rice JB, Desai U, Cummings AK, Birnbaum HG, Skornicki M, Parsons NB. Burden of diabetic foot ulcers for medicare and private insurers. Diabetes Care. 2014;37:651–658. doi: 10.2337/dc13-2176. [DOI] [PubMed] [Google Scholar]
- Rook (2013).Rook GA. Regulation of the immune system by biodiversity from the natural environment: an ecosystem service essential to health. Proceedings of the National Academy of Sciences of the United States of America. 2013;110:18360–18367. doi: 10.1073/pnas.1313731110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Samuel et al. (2008).Samuel BS, Shaito A, Motoike T, Rey FE, Backhed F, Manchester JK, Hammer RE, Williams SC, Crowley J, Yanagisawa M, Gordon JI. Effects of the gut microbiota on host adiposity are modulated by the short-chain fatty-acid binding G protein-coupled receptor, Gpr41. Proceedings of the National Academy of Sciences of the United States of America. 2008;105:16767–16772. doi: 10.1073/pnas.0808567105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scales & Huffnagle (2013).Scales BS, Huffnagle GB. The microbiome in wound repair and tissue fibrosis. Journal of Pathology. 2013;229:323–331. doi: 10.1002/path.4118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seite et al. (2014).Seite S, Flores GE, Henley JB, Martin R, Zelenkova H, Aguilar L, Fierer N. Microbiome of affected and unaffected skin of patients with atopic dermatitis before and after emollient treatment. Journal of Drugs in Dermatology. 2014;13:1365–1372. [PubMed] [Google Scholar]
- Seto et al. (2014).Seto CT, Jeraldo P, Orenstein R, Chia N, DiBaise JK. Prolonged use of a proton pump inhibitor reduces microbial diversity: implications for Clostridium difficile susceptibility. Microbiome. 2014;2:42. doi: 10.1186/2049-2618-2-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shu et al. (2013).Shu M, Wang Y, Yu J, Kuo S, Coda A, Jiang Y, Gallo RL, Huang CM. Fermentation of Propionibacterium acnes, a commensal bacterium in the human skin microbiome, as skin probiotics against methicillin-resistant Staphylococcus aureus. PLOS ONE. 2013;8:e55380. doi: 10.1371/journal.pone.0055380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith et al. (2016).Smith K, Collier A, Townsend EM, O’Donnell LE, Bal AM, Butcher J, Mackay WG, Ramage G, Williams C. One step closer to understanding the role of bacteria in diabetic foot ulcers: characterising the microbiome of ulcers. BMC Microbiology. 2016;16:54. doi: 10.1186/s12866-016-0665-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strober (2013).Strober W. Impact of the gut microbiome on mucosal inflammation. Trends in Immunology. 2013;34:423–430. doi: 10.1016/j.it.2013.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sze & Schloss (2016).Sze MA, Schloss PD. Looking for a signal in the noise: revisiting obesity and the microbiome. mBio. 2016;7:e01018–01016. doi: 10.1128/mBio.01018-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tellechea et al. (2013).Tellechea A, Kafanas A, Leal EC, Tecilazich F, Kuchibhotla S, Auster ME, Kontoes I, Paolino J, Carvalho E, Nabzdyk LP, Veves A. Increased skin inflammation and blood vessel density in human and experimental diabetes. International Journal of Lower Extremity Wounds. 2013;12:4–11. doi: 10.1177/1534734612474303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van de Wijgert et al. (2014).Van de Wijgert JH, Borgdorff H, Verhelst R, Crucitti T, Francis S, Verstraelen H, Jespers V. The vaginal microbiota: what have we learned after a decade of molecular characterization? PLOS ONE. 2014;9:e105998. doi: 10.1371/journal.pone.0105998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams & Gallo (2015).Williams MR, Gallo RL. The role of the skin microbiome in atopic dermatitis. Current Allergy and Asthma Reports. 2015;15:65. doi: 10.1007/s11882-015-0567-4. [DOI] [PubMed] [Google Scholar]
- Wolcott et al. (2016).Wolcott RD, Hanson JD, Rees EJ, Koenig LD, Phillips CD, Wolcott RA, Cox SB, White JS. Analysis of the chronic wound microbiota of 2,963 patients by 16S rDNA pyrosequencing. Wound Repair and Regeneration. 2016;24:163–174. doi: 10.1111/wrr.12370. [DOI] [PubMed] [Google Scholar]
- World Health Organisation (2016).World Health Organisation Diabetes mellitus. 2016. http://www.who.int/mediacentre/factsheets/fs138/en/ http://www.who.int/mediacentre/factsheets/fs138/en/
- Yosipovitch et al. (1993).Yosipovitch G, Tur E, Cohen O, Rusecki Y. Skin surface pH in intertriginous areas in NIDDM patients. Possible correlation to candidal intertrigo. Diabetes Care. 1993;16:560–563. doi: 10.2337/diacare.16.4.560. [DOI] [PubMed] [Google Scholar]
- Yu et al. (2015).Yu W, Yuan X, Xu X, Ding R, Pang L, Liu Y, Guo Y, Li H, Li M, Yuan J, Tang L, Wen S. Reduced airway microbiota diversity is associated with elevated allergic respiratory inflammation. Annals of Allergy, Asthma & Immunology. 2015;115:63–68. doi: 10.1016/j.anai.2015.04.025. [DOI] [PubMed] [Google Scholar]
- Zhang & Zhang (2013).Zhang Y, Zhang H. Microbiota associated with type 2 diabetes and its related complications. Food Science and Human Wellness. 2013;2:167–172. doi: 10.1016/j.fshw.2013.09.002. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Sample types are indicated in the second column: skin swab from an area adjacent to the foot wound (SA), skin swab from the contralateral foot (SC), wound swab (WS) and debrided wound tissue (WD). A tick (x) indicates that a sample was collected, a cross (x) indicates that no samples for that time point were collected because the patient could not make their scheduled appointment, and NC indicates that a sample was not collected because podiatry staff deemed there was not sufficient tissue available for a debridement sample. In the case that a wound healed (indicated by WH) no further samples were collected for that patient. In the case of P4, the contralateral foot had previously been amputated, and the foot containing the wound was amputated after time point 2. Samples for which a 16S rRNA gene PCR product was not obtained are indicated with (x).
Sample types are indicated in the second column: skin swab from the base of the left foot (L), or right foot (F). A tick (x) indicates that a sample was collected, a cross (x) indicates that no samples for that time point were collected because the subject was not available. Samples for which a 16S rRNA gene PCR product was not obtained are indicated with (x). Control subject 8 (CP8) was removed from the study as not enough samples were collected.
Wound size is shown as height × width × depth in mm. All wounds were routinely irrigated with Prontosan solution, followed by dressing with either Allevyn foam for moist wound healing, Zetuvit dressing to remove excess wound exudate, Inadine antimicrobial dressing (10% povidone-iodine), or Acticoat flex (silver coated antimicrobial dressing). Decisions on wound dressing were made by the treating podiatrist or wound care nurse.
Coverage before and after quality filtering for each sample is indicated, along with the sequencing run that each sample was sequenced in.
The Wald test was used as implemented in DESeq2. The model health + subject:health was used, and the OTU table was filtered to remove OTUs with a count of less than 2, and/or present in less than 10% of samples. Log2FC was calculated relative to the control skin samples.
The Wald test was used as implemented in DESeq2. The model health + subject:health was used, and OTUs were collapsed into genera level classifications. The original OTU table was filtered to remove OTUs with a count of less than 2, and/or present in less than 10% of samples. Log2FC was calculated relative to the control skin samples.
OTUs important to the classification in the Random Forrest Model calculated using the GINI index.
The Wald test was used as implemented in DESeq2. The model sampletype + sampletype:health was used, and the OTU table was filtered to remove OTUs present in less than 20% of samples. Log2FC was calculated relative to the diabetic skin samples.
Comparison as adjacent diabetic skin to wound swabs (adj_V_ws), contralateral diabetic skin to wound swabs (con_V_ws), adjacent diabetic skin to wound debridement (adj_V_wd), and contralateral diabetic skin to wound debridement (con_V_ws). Small but statistically significant differences were observed, such that there was greater similarity between adjacent skin and wounds compared to contralateral skin and wounds. Significant differences are indicated with ∗∗∗(p < 0.001).
Inter-visit weighted unifrac distances from wound swabs for individual patients were plotted against the degree of healing, where 1 equals complete healing, 0 equals no change in wound size and negative numbers indicate and increase in wound size. No significant correlation was found using a linear model.
Data Availability Statement
The following information was supplied regarding data availability:
Quality filtered sequence data has been deposited in the European Nucleotide Archive under study accession number PRJEB17696.