Abstract
Self-efficacy is a commonly included cognitive variable in weight-loss trials, but there is little uniformity in its measurement. Weight-loss trials frequently focus on physical activity (PA) and eating behavior, as well as weight loss, but no survey is available that offers reliable measurement of self-efficacy as it relates to each of these targeted outcomes. The purpose of this study was to test the psychometric properties of brief, pragmatic self-efficacy scales specific to PA, healthful eating and weight-loss (4 items each). An adult sample (n=1790) from 28 worksites enrolled in a worksite weight-loss program completed the self-efficacy scale, as well as measures of PA, dietary fat intake, and weight, at baseline, 6-, and 12-months. The hypothesized factor structure was tested through confirmatory factor analysis, which supported the expected factor structure for three latent self-efficacy factors, specific to PA, healthful eating, and weight-loss. Measurement equivalence/invariance between relevant demographic groups, and over time was also supported. Parallel growth processes in self-efficacy factors and outcomes (PA, fat intake, and weight) support the predictive validity of score interpretations. Overall, this initial series of psychometric analyses supports the interpretation that scores on these scales reflect self-efficacy for PA, healthful eating, and weight-loss. The use of this instrument in large-scale weight-loss trials is encouraged.
Introduction
In response to the worldwide increase in body mass index (BMI) over the last three decades (World Health Organization, 2011), the development of translatable weight-loss programs is a public health priority (Wadden, Brownell, & Foster, 2002). Much work has been done to identify efficacious methods of weight-loss (Berkel, Carlos Poston, Reeves, & Foreyt, 2005; Curioni & Lourenco, 2005; Franz et al., 2007; Haddock, Poston, Dill, Foreyt, & Ericsson, 2002; Jakicic et al., 2001; Tang, Abraham, Greaves, & Yates, 2014; Wing & Phelan, 2005). One promising approach involves developing interventions based on behavioral theories that target social cognitions and self-regulation strategies (Bandura, 1986; Michie, van Stralen, & West, 2011; Prochaska & Velicer, 1997; Schwarzer, 1992). An early review on the role of self-efficacy in health behavior change supported the inclusion of self-efficacy enhancing strategies in behavioral interventions (Strecher, DeVellis, Becker, & Rosenstock, 1986). Frequent consideration for self-efficacy in weight-loss trials in the recent decades (e.g. Byrne, Barry, & Petry, 2012; Fontaine & Cheskin, 1997; Hays, Finch, Saha, Marrero, & Ackermann, 2014; Linde, Rothman, Baldwin, & Jeffery, 2006; Plotnikoff, McCargar, Wilson, & Loucaides, 2005; Prochaska, Norcross, Fowler, Follick, & Abrams, 1992; Richman, Loughnan, Droulers, Steinbeck, & Caterson, 2001; Shin et al., 2011; Warziski, Sereika, Styn, Music, & Burke, 2008; White et al., 2004), suggests that this recommendation was well-received among weight-loss researchers, and demonstrates a clear desire to move toward behavioral interventions in which self-efficacy is expected to play an important role. Progress and comparison across trials is limited, however, by inconsistency in the use, conceptualization, and measurement of self-efficacy.
Self-efficacy is defined as an individual's belief in their ability to perform a task or reach a goal successfully (Bandura, 1977, 1997). Individuals with higher self-efficacy are more likely to persist in their efforts until success is achieved, compared to those with lower self-efficacy. Self-efficacy is domain specific, such that a high sense of efficacy in one domain (e.g., healthful eating) is not necessarily accompanied by high efficacy in other domains (e.g., physical activity). Self-efficacy judgments for independent behavioral domains governed by similar sub-skills are expected to be related (e.g. self-efficacy to lose weight and self-efficacy to eat healthfully). Through this postulate of generalizability, self-efficacy is conceptualized as a hierarchical construct (e.g. Bong, 1997; Skaalvik & Skaalvik, 2010), though such a structure has not yet been examined for self-efficacy as it relates to typical targeted outcomes of weight-loss trials (i.e. physical activity, healthful eating, and weight-loss).
Some evidence suggests that self-efficacy is particularly important as a predictor of initial success, and maintenance of weight-loss (Elfhag & Rössner, 2005) and related behavior changes (Maes & Karoly, 2005) in obese samples (Clark, Cargill, Medeiros, & Pera, 1996; Trost, Kerr, Ward, & Pate, 2001). Significant positive effects of self-efficacy have been reported for weight-loss (Byrne et al., 2012; Hays et al., 2014; Palmeira et al., 2007; Shin et al., 2011; Warziski et al., 2008), physical activity (Linde et al., 2006; McAuley & Blissmer, 2000), and healthful eating (Hagler, 2007; Henry, Reimer, Smith, & Reicks, 2006; Steptoe, Doherty, Kerry, Rink, & Hilton, 2000; Stotland & Zuroff, 1991). Other studies, however, have not found these relationships (Annesi, 2007; Linde et al., 2004; Teixeira et al., 2002; Teixeira et al., 2004). Heterogeneity of effects across studies may result from the lack of uniformity in which self-efficacy has been included in weight-loss trials. In some cases, measures of self-efficacy for physical activity or exercise (Plotnikoff et al., 2005; Teixeira et al., 2004), diet or eating habits (e.g. Shin et al., 2011; Warziski et al., 2008), or both (e.g. Linde et al., 2006; Palmeira et al., 2007) are measured. Most report on relationships between self-efficacy and overall weight-loss (e.g. Annesi, 2007; Byrne et al., 2012; Palmeira et al., 2007), though some focus on self-efficacy domains and behavior with congruent focal points (e.g. the relationship between diet self-efficacy and change in fruit and vegetable consumption; Van Duyn et al., 2001), or incongruent focal points (e.g. the relationship between self-efficacy for exercise and change in dietary behaviors; Linde et al., 2006). Furthermore, self-efficacy has been included as a predictor (e.g. Linde et al., 2006), outcome (e.g. Plotnikoff et al., 2005) or mediator (e.g. White et al., 2004) in weight-loss trials.
Despite differences in the behavioral domain of interest and the range of applications of self-efficacy in relation to various behavioral outcomes observed in the literature, no surveys are currently available that measure self-efficacy for more than one behavioral domain related to weight-loss (e.g. physical activity, healthful eating). Additionally, the concern of participant burden in the application of behavioral interventions typically results in the assessment of self-efficacy within a large battery of survey items (e.g. Plotnikoff et al., 2005; Shin et al., 2011). Taken together, these observations highlight the need to assess self-efficacy related to physical activity, eating, and weight loss with brief measures that can be embedded within larger surveys. The brief measures of self-efficacy used previously (e.g. Annesi, 2007; Steptoe et al., 2000; Van Duyn et al., 2001), however, have little or no supporting evidence of construct validity. Tests of factorial validity have been reserved for surveys with greater numbers of items (i.e. 20-25), though they reflect factors presumed to contribute to a single behavioral domain of self-efficacy (e.g. Clark, Abrams, Niaura, Eaton, & Rossi, 1991; Glynn & Ruderman, 1986). Furthermore, reports of measurement equivalence/invariance of those scales are infrequent, even though differences in effects between self-efficacy and weight-loss-related behaviors (i.e. weight-loss, physical activity, or healthful eating) have been reported according to gender (Forster & Jeffrey, 1986; Linde et al., 2004), BMI status (Richman et al., 2001), and race (Annesi, 2007). Lastly, the frequent use of author developed or adapted scales (e.g. Dennis & Goldberg, 1996; Hagler, 2007; Henry et al., 2006; Schwarzer & Renner, 2000; Steptoe et al., 2000) suggests dissatisfaction with available measures, and has contributed to the accumulation of evidence that is difficult to interpret.
The development and validation of brief pragmatic measures1 of key theoretical constructs specified as important mechanisms of behavior change, which may be proximal indicators of intervention effects, is of importance to facilitate research translation (Glasgow, 2013). The purpose of the current investigation was to provide a survey to measure self-efficacy for weight-loss-related behaviors that is brief, comprehensive, and pragmatic. Here we report on initial tests of the psychometric quality of a brief survey targeting self-efficacy for weight-loss-related behaviors. Tests of factorial and predictive validity, measurement equivalence/invariance according to gender, age, race education level, and BMI status, and stability across time were conducted using a representative sample of overweight and obese individuals participating in a large-scale worksite weight-loss intervention (citation removed for author masking in the review process).
Methods
Participants
The sample (N=1790) consisted of overweight or obese adults (73.3% female; 73.4% white; 33.7% college grad) with a mean (sd) age 46.61(10.978), and BMI 33.32(6.54), from 28 worksites in Southwestern Virginia enrolled in a 2-condition cluster randomized weight-loss trial. Eligibility for the worksite weight-loss program extended to worksites with 100-600 employees and Internet access at work. Included worksites agreed to distribute a brief health survey to the entire employee population. Participant inclusion for the worksite weight-loss program extended to individuals with a BMI >24.5 kg/m2. All participants provided informed consent.
Procedure
Procedures for the current study were embedded in those of the worksite weight-loss trial. Worksites were randomly assigned to one of two intervention programs: 1) IncentaHealth and 2) Livin' My Weigh (LMW). Both programs provided healthy eating and physical activity strategies for weight-loss, were based on Social Cognitive Theory (Bandura, 1997), and were delivered over 12 months. The nutrition component targeted consumption of fruits and vegetables and dietary fat intake, and the physical activity component encouraged participants to work their way up to regular bouts of moderate-to-vigorous physical activity for 150 minutes per week (Garber, Blissmer, Deschenes, & et al., 2011). Both programs offered health promotion e-newsletters and quarterly weigh-ins. Primary differences between conditions included the frequency of e-newsletter delivery and access to weigh-in stations, and the presence/absence of a moderate monetary incentive which was offered in the IncentaHealth condition only. More details on each program can be found elsewhere (citation removed for author masking in the review process). Participants completed several surveys, including the scale measuring self-efficacy for weight-loss-related behaviors, on three occasions each spaced 6 months apart.
Measures
All measures, with the exception of body weight, were self-reported and completed via either web-based or paper-and-pencil format. Demographic information (i.e. height, gender, age, race, education level) was gathered using a brief health survey prior to random assignment of the worksites to intervention conditions.
Self-efficacy
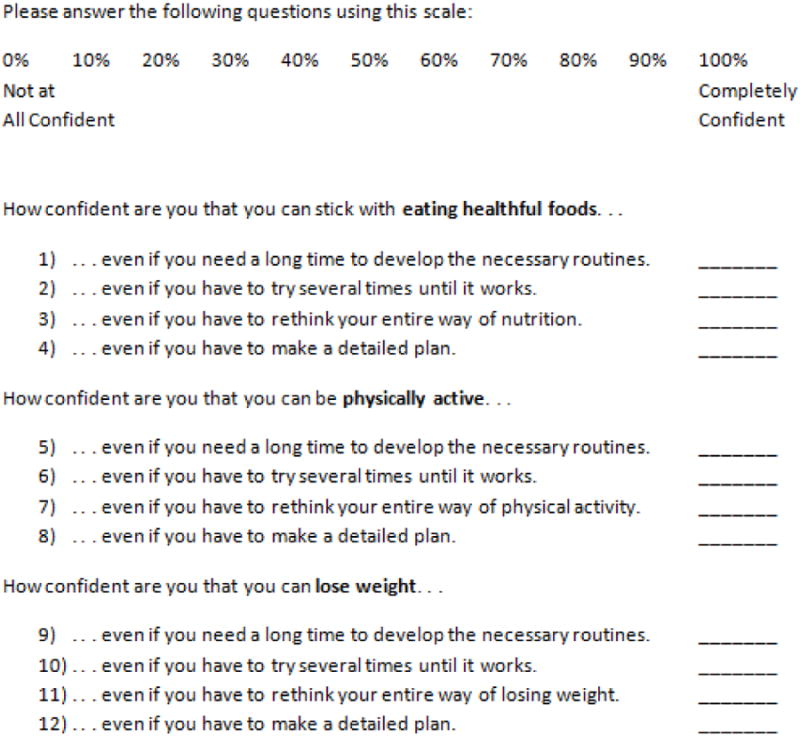
Self-efficacy for physical activity (PASE), healthful eating (HESE), and weight-loss (WLSE), were each measured using four items modeled after those used by Schwarzer & Renner (2000) to include items designed to measure self-efficacy that align with many social cognitive theories (e.g., Social Cognitive Theory, Bandura, 1997; Health Action Process Approach, Schwarzer, 1992; Transtheoretical Model, Prochaska & Velicer, 1997). Two items each were selected from those specified by Schwarzer and Renner as ‘action self-efficacy’ (e.g. I can manage to stick to healthful food even if I have to rethink my entire way of nutrition.) and ‘coping self-efficacy’ (e.g. I can manage to stick to healthful food even if I need a long time to develop the necessary routines.). Item stems were altered to reflect the targeted outcome (e.g. “How confident are you that you can remain physically active even if you have to make a detailed plan?). Participants were asked to rate how confident they were that they could stick with a specific behavior under certain circumstances using an 11-point scale ranging from 0% to 100%. The measure is displayed in Figure 1.
Figure 1. Weight-loss-related behavior self-efficacy scales.
Weight
Body weight was assessed objectively using a calibrated scale at each worksite (citation removed for author masking in the review process). For each measure of body weight, participants logged-in to their online account and stepped onto the scale. Data was automatically uploaded and de-identified for use by the research team.
Physical activity
Items from the behavioral risk factor surveillance survey (BRFSS; Brownson, Jones, Pratt, Blanton, & Heath, 2000) (i.e. “how many [days per week/minutes per day] of [moderate/vigorous] physical activity in the last seven days”) were used to estimate weekly minutes of moderate-to-vigorous physical activity at all three time points.
Fat intake
The Block Dietary Fat Screener (Block, Gillespie, Rosenbaum, & Jenson, 2000; Flood et al., 2002; Michels et al., 2000; Thompson et al., 1999) was used to quantify fat intake. Frequency of fatty food consumption per day, ranging from 1 to 51 times per day, was measure using 17 items with response options that ranged from “once a month or less” to “5+ times a week”. Higher scores represent greater consumption of fatty foods.
Statistical analysis
Robust maximum likelihood estimation was used to adjust for systematic differences between worksites in Mplus 7.11 (Muthén & Muthén, 2012). Critical z-scores (parameter estimate/SE) were used to test significance of relations between variables (p < .05). There was 22.1% missingness for all measures (49,446 of 223,750 responses/measurements) across all three measurement time points. Preliminary analyses confirmed that covariance matrices of self-efficacy scale items did not differ between intervention conditions (χ2(df)=71.372(55), RMSEA(90% CI)=.018(.000, .030), CFI=998, SRMR=.026). Further, changes in weight, physical activity, and fat consumption from baseline to 6- and 12-months did not differ between groups (Wald statistic ≥.076, p≥.1038). Therefore, the sample was collapsed and analyses were run on the full sample for this psychometric assessment.
Confirmatory factor analysis
The factor structure of the scale was examined iteratively using confirmatory factor analysis (CFA). Using the entire sample, model fit was compared across a number of alternative model specifications that gradually grew more complex until we reached a model reflective of the expected hierarchical factor structure. The model with the best fit was retained for further analysis.
Model specifications
The simplest model specification was the null model which reflected the absence of systematic relationships between item responses, and would suggest that any observed covariance was a result of random influences if supported. It was expected that the null model would demonstrate the worst model fit compared to all other models tested, as at face value the items are clearly related and could reflect a number of underlying factor structures. Specification of the single factor model reflected the possibility that a single underlying factor is responsible for all item covariances, which would suggest the scale measures self-efficacy for weight-loss-related behaviors without distinguishing between the targeted behavioral domains (i.e. healthful eating, physical activity, and weight-loss). Support for the single factor model would support the use of a composite score of all scale items, and would suggest that items targeting physical activity self-efficacy covary as strongly with items targeting healthful eating or weight-loss self-efficacy as they do with each other, in opposition of the theoretical postulate that self-efficacy is domain specific (Bandura, 1977, 1997). A two factor model was specified to test the possibility that items designed to assess self-efficacy in the planning phases of behavior change (i.e. action self-efficacy) correlate more strongly with each other than they do with items designed to assess self-efficacy in the post-intentional, or action phase of behavior change (i.e. coping self-efficacy), and vice versa, regardless of behavioral domain.2 Next, an orthogonal three factor model was specified as the first model distinguishing between behavioral domains (PASE, EHSE, and WLSE). This model was aligned with the theoretical postulate of domain specificity, but opposed to the postulate of generalizability across similar sub-skills (Bandura, 1977, 1997). Finally, the hierarchical model was specified to align more fully with self-efficacy theory such that items loaded onto first-order factors HESE, PASE, and WLSE, reflective of the expected behavioral domain specificity of self-efficacy, and those first-order factors loaded onto a single second-order factor for weight-loss-related behavior self-efficacy (WLRBSE) reflective of the generalizability of self-efficacy across behavioral domains with similar sub-skills (Bandura, 1977, 1997). An alternative model to the hierarchical model is a correlated, three-factor model in which first-order factors for HESE, PASE, and WLSE are allowed to correlate, but do not load onto a second-order factor. This alternative model is statistically equivalent to the hierarchical model, making the choice of factor structure between these two models a matter of investigator preference.
Measurement equivalence/invariance
Measurement equivalence/invariance was examined using an omnibus test of equal covariances between groups classified according to gender, age, race, education level, and BMI status, and across the three measurement time points. Age groups were specified as 1) those ≥ 1 SD below the sample mean, 2) those < 1 SD from the mean, and 3) those ≥ 1 SD above the mean. Racial comparisons were limited to ‘White/Caucasian’ compared with ‘Black/African American’ due to the small number of Asian (n=12), American Indian/Alaskan Native (n=9), Native Hawaiian or Other Pacific Islander (n=2) participants. Categories for education level included 1) those with a high school education or less, 2) those with some college experience, 3) college graduates, and 4) those with postgraduate education. Participants were also classified as ‘overweight’ (BMI of 24.5-29.9), ‘obese class 1’ (BMI of 30.0-34.9), ‘obese class 2’ (BMI of 35.0-39.9), or ‘obese class 3’ (BMI≥40). Finally, stability of the measure was tested across the three measurement times spanning one year. In the case that equivalence of covariance matrices had not been supported, tests of decreasingly restrictive levels of equivalence were planned to identify the highest level of measurement equivalence/invariance reflected in these data (Vandenberg & Lance, 2000).
Latent growth models
Mean-level conditional latent growth models were specified that predicted change in the outcomes by change in each respective self-efficacy scale (e.g. change in physical activity predicted by change in PASE), as well as by change in the second-order factor, WLRBSE. A two-step approach was used to judge model fit of self-efficacy change predicting outcome change (Kline, 2011). Unconditional models were first specified to test for significant change in each factor and outcome variable independently. Conditional models then tested relationships between change in self-efficacy and change in behavioral outcomes, with the expectation that as self-efficacy increased, the target outcome would change in a desirable direction (i.e. increases in physical activity, and decreases in weight and dietary fat intake). Model 1 tested the relationship between change in WLSE and change in weight. Model 2 tested the relationship between change in PASE and change in moderate-to-vigorous physical activity minutes per week, Model 3 tested the relationship between change in HESE and change in dietary fat consumption, and Models 4-6 tested the relationship between change in WLRBSE and change in each outcome behavior, separately.
Model fit
Model fit was evaluated using the chi-square (χ2) statistic, comparative fit index (CFI), root mean square error of approximation (RMSEA) and its 90% confidence interval, and standardized root mean square residual (SRMR) (Bollen, 1989; Hu & Bentler, 1999). Commonly, values of CFI approximating 0.90 are judged to be acceptable, while values > 0.95 indicate good fit. Close and acceptable fit are indicated by values of the RMSEA ≤ 0.06 and ≤ 0.08, respectively. Optimal protection from type I and type II error rates is provided by concurrent values ≥0.95 for CFI and ≤0.08 for SRMR (Hu & Bentler, 1999). Models were compared using the Bayesian Information Criterion (BIC), a relative fit statistic which approximates the Bayes factor and is conservative for comparing complex models (Bollen, Harden, Ray, & Zavisca, 2014).
Results
Baseline means, standard deviations, and bivariate correlations of the self-efficacy scales and outcome measures are reported in Table 1. Model fit statistics for all confirmatory factor analyses are displayed in Table 2.
Table 1. Baseline values and bivariate correlations between self-efficacy factors and outcome variables.
| M(sd) | PASE | HESE | WLSE | Weight | MVPA | |
|---|---|---|---|---|---|---|
| Physical activity self-efficacy | 71.55(20.94) | |||||
| Healthful eating self-efficacy | 68.38(20.78) | .740** | ||||
| Weight-loss self-efficacy | 72.30(21.44) | .758** | .770** | |||
| Weight (lbs.) | 207.5(45.9) | -.050* | -.050* | -.004 | ||
| Moderate-to-vigorous PA mini/wk. | 61.67(112.26) | .309** | .154** | .145** | -.129** | |
| Fat intake summary score | 22.32(8.61) | -.143** | -.222** | -.102** | .163** | -.175** |
p<.05,
p<.01.
Table 2. Model fit statistics for all models.
| N | χ2 (df) | RMSEA (90% CI) | CFI | SRMR | BIC | |
|---|---|---|---|---|---|---|
| Confirmatory Factor Analyses | ||||||
| Null Model | 1751 | 9284.006(66) | 0.282(0.278, 0.287) | <0.001 | 0.637 | 189438.178 |
| Single Factor | 1751 | 3679.493(54) | 0.196(0.190, 0.201) | 0.607 | 0.081 | 167394.792 |
| Two Phasic Factors | 1751 | 4880.738(54) | 0.226(0.221, 0.231) | 0.476 | 0.473 | 171235.824 |
| Three Orthogonal Factors | 1751 | 2292.053(54) | 0.154(0.149, 0.159) | 0.757 | 0.502 | 161062.479 |
| Three Correlated Factors | 1751 | 1135.759(51) | 0.110(0.105, 0.116) | 0.882 | 0.038 | 157909.409 |
| Hierarchical Model | 1751 | 1135.759(51) | 0.110(0.105, 0.116) | 0.882 | 0.038 | 157909.409 |
| Trimmed Hierarchical Model | 1751 | 280.877(32) | 0.067(0.060, 0.074) | 0.964 | 0.011 | 130547.798 |
Confirmatory factor analysis
Generally, model fit for the confirmatory factor analyses improved with increasing complexity, though the two-factor model reflecting phasic factors of action and coping self-efficacy demonstrated worse fit than the less complex single-factor model. The hierarchical model demonstrated improved fit compared to the orthogonal three-factor model, the two-factor model, the single-factor model, and the null model. Composite factor reliabilities for the first-order factors were .985 for PASE, .997 for HESE, and .985 for WLSE. Modification indices specified significant item collinearity. Model fit was acceptable for this sample after trimming a total of two items from the hierarchical model (items 4 and 12, from HESE and WLSE, respectively). Composite factor reliabilities of the trimmed factors were .972 for PASE, .964 for HESE, and .976 for WLSE. The hierarchical model is displayed in Figure 2. Interested readers are encouraged to contact the corresponding author for detailed results of the remaining confirmatory factor analyses.
Figure 2. Hierarchical model reflecting the hypothesized factor structure of the scale.
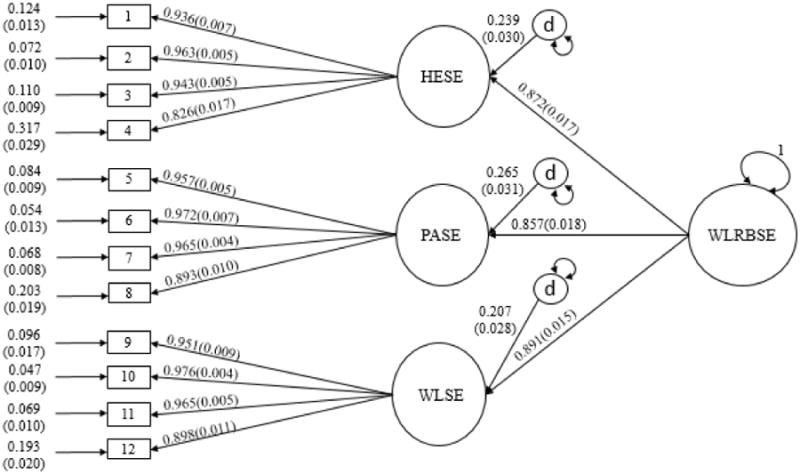
WLSE: Weight-loss self-efficacy; PASE: Physical activity self-efficacy; HESE: Healthful eating self-efficacy; WLRBSE: Weight-loss-related behavior self-efficacy; d: Disturbance term for endogenous latent factors.
Measurement equivalence/invariance
Equivalence of the covariance matrices was supported between genders (χ2(df)=59.63(55), RMSEA(90%CI)=0.01(<0.001,0.02), CFI=0.99, SRMR=0.07), age groups (χ2(df)=462.17(100), RMSEA(90%CI)=0.03 (0.02,0.04), CFI=0.99, SRMR=0.046), race (χ2(df)=65.53(55), RMSEA(90%CI)=0.02 (<0.001,0.03), CFI=0.99, SRMR=0.03), education (χ2(df)=270.49(165), RMSEA(90%CI)= 0.04(0.03,0.05), CFI=0.99, SRMR=0.050), BMI status (χ2(df)=234.85(165), RMSEA (90%CI)=0.03(0.02,0.04), CFI=0.99, SRMR=0.05), and across time (χ2(df)=398.02(310), RMSEA(90%CI)=0.01 (0.01,0.02), CFI=0.99, SRMR=0.07).
Latent growth models
Unstandardized and standardized parameter estimates for change over each 6-month interval in the unconditional models, and the relationships between rates change over time for the specified self-efficacy factor and outcome variable in the conditional models are listed in Table 3. Unconditional latent growth models demonstrated acceptable model fit (χ2(df)<21.16(1), RMSEA≤0.10, CFI≥0.95, SRMR<0.03), with exception of the model for change in fat intake (χ2(df)=46.89(1), RMSEA(90%CI)=0.16(0.12,0.20), CFI=0.89, SRMR=0.04), for which relative (CFI) and absolute (RMSEA) fit indices demonstrate only marginal fit. Parameter estimates supported significant linear change over time for all variables (p≤.01). With each 6-month increment, a reduction was seen for WLRBSE (M= -3.00,sd=0.35), WLSE (M= -3.25, sd=0.34), PASE (M= -3.13, sd=0.41), HESE (M= -2.53, sd=0.43), objectively measured weight (M= -1.56, sd=0.29), and fat consumption (M= -1.90, sd=0.10), whereas moderate-to-vigorous physical activity increased over time (M= 19.44, sd=3.48). Change over time for all variables was heterogeneous (p≤.048), with exception change in fat consumption (p=.183). All conditional models demonstrated acceptable-to-good model fit (χ2(df)< 103.784(9), RMSEA<0.07, CFI>0.93, SRMR<0.03), and parameter estimates supported positive change in self-efficacy significantly predicting desirable health behavior change. The relationships between the rates of changes in self-efficacy and behavior were heterogeneous in all conditional models (p<001).
Table 3. Standardized path coefficients for change over time in the unconditional models and the relationship between change in outcome and change in self-efficacy in the conditional models.
| B(95% CI) | Zβ (95% CI) | P | |
|---|---|---|---|
|
|
|||
| Unconditional Models | |||
|
|
|||
| WLSE | -3.253 (-3.920, -2.586) | -0.560 (-0.823, -0.297) | <.001 |
| HESE | -2.525 (-3.364, -1.686) | -0.396 (-0.653, -0.139) | .002 |
| PASE | -3.131 (-3.939, -2.323) | -0.447 (-0.618, -0.276) | <.001 |
| WLRBSE | -3.000 (-3.690, -2.310) | -0.483 (-0.687, -0.279) | <.001 |
| Weight | -1.559 (-2.128, -0.990) | -0.231 (-0.321, -0.141) | <.001 |
| Fat intake | -1.901 (-2.103, -1.699) | -1.141 (-2.010, -0.272) | .010 |
| MVPA | 19.440 (12.679, 26.201) | 0.594 (0.176, 1.012) | .005 |
| Conditional Models | |||
|
|
|||
| Model 1: Weight on WLSE | -0.762 (-1.001, -0.523) | -0.672 (-0.846, -0.480) | <.001 |
| Model 2: Fat intake on HESE | -0.136 (-0.191, -0.081) | -0.630 (-1.111, -0.129) | .010 |
| Model 3: MVPA on PASE | 4.506 (2.649, 6.363) | 0.978 (0.268, 1.688) | .007 |
| Model 4: Weight on WLRBSE | -0.766 (-0.999, -0.533) | -0.647 (-0.845, -0.449) | <.001 |
| Model 5: Fat intake on WLRBSE | -0.158 (-0.029, -0.107) | -0.683 (-1.211, -0.155) | .011 |
| Model 6: MVPA on WLRBSE | 4.280 (2.831, 5.729) | 0.865 (0.181, 1.549) | .013 |
Unconditional models indicate change in the respective variable over each 6-month interval. Conditional models indicate the relationship between change in self-efficacy and change in outcome over each 6-month interval. WLSE: Weight-loss self-efficacy; PASE: Physical activity self-efficacy; HESE: Healthful eating self-efficacy; WLRBSE: Weight-loss-related behavior self-efficacy; MVPA: Moderate-to-vigorous physical activity. B represents the unstandardized solution, whereas Zβ reflects the standardized solution.
Discussion
This study provides evidence of strong psychometric quality of this survey targeting self-efficacy for weight-loss-related behaviors, supporting the continued use of this brief, comprehensive, and pragmatic survey in weight-loss trials. The self-efficacy scales presented here are the first to systematically measure PASE, HESE, and WLSE within a single tool, and should promote uniformity of measurement across weight-loss interventions with the goal of enhancing progress in the development of translatable weight-loss programs. Adapted from a brief scale capturing self-efficacy for healthful eating (Schwarzer & Renner, 2000), this new survey incorporates the phasic nature of behavior change outlined in theory (Bandura, 1997; Prochaska & Velicer, 1997; Schwarzer, 1992) by including items framed towards self-efficacy for starting a behavior, as well as for continuing or maintaining a behavior, in relation to three behavioral domains: 1) healthful eating, 2) physical activity, and 3) weight-loss. Results support the expected factor structure, measurement equivalence/invariance across a range of relevant sample characteristics, stability of the item covariances across time, scale sensitivity to change over time, and the expected predictive ability of each self-efficacy factor for relevant behavioral outcomes in a large, representative sample of overweight and obese adults participating in a worksite weight-loss program.
The extent to which the factor structure of this measure aligns with underlying theory (Bandura, 1977, 1997) was illustrated by comparing model fit across increasingly complex models. The first model distinguishing between behavioral domains in testing the structure of this scale was the orthogonal three-factor model. Though still poor, this model demonstrated improved model fit compared to all less complex models, supporting the expectation that the scale would reflect the postulated domain specificity of self-efficacy (Bandura, 1977, 1997). Model fit was best, compared to all other models tested, in the hierarchical model demonstrating scale alignment with theoretical postulates of domain specificity, and generalizability of self-efficacy across domains with similar sub-skills. An equivalent model, the correlated three-factor model supports the theoretical postulate of domain specificity, but does not go so far as to attribute relations between first-order factors to a common underlying factor for WLRBSE. Performance of the alternative model is not expected to differ from that of the hierarchical model in the analyses for measurement invariance and predictive validity. Modification indices specified cross-loading and extreme collinearity of two items. Removal of these two items revealed acceptable model fit for the hierarchical model. It should be noted that this observation does not imply that the two removed items perform poorly. Rather, in this sample, items from two different behavioral domains covaried so strongly that the model specification restricting them to load only on their respective factor degraded the fit of the specified model, as model test statistics indicate the degree to which the model-implied covariance matrix matches that of the obtained data (Kline, 2011). Factor loadings of these two items on their respective factors were both large (β= 0.826, β= 0.898) and significant (p<.001). More work would be required to determine if this extreme collinearity generalizes to other samples before recommending that items be restricted from future use. Analyses therefore provided strong support for the intended factor structure of the measure.
The structure of the survey was further supported through analysis of measurement equivalence/invariance, and stability over time. Generally, these tests indicated that respondents of different genders, ages, races, education levels, or BMI statuses interpret the survey in a conceptually similar way, and there did not appear to be any differences according to relevant sample characteristics that precluded responding to the scales in a similar manner. Further, the factor structure was stable across time, indicating that the conceptual frame of reference against which the sample responded to the measure did not change over time. These results provide confidence for researchers interested in using the scale, that any between group effects according to gender, age, race, education level, or BMI status are not biased by systematic differences in the interpretation of and responses to the self-efficacy measures. Moreover, these results support the interpretation that change over time in the scores reflects true changes in the construct of interest, as the stability of the scale's structure has been established across three measurements spanning a year.
In addition to stability of the factor structure over time, the scale scores demonstrated sensitivity to change over time for all self-efficacy factors, indicating a reduction in self-efficacy for all weight-loss-related behavioral domains with each 6-month increment. The scores were also sensitive to between subject variability in the rate of change in all self-efficacy factors, including WLRBSE, as was indicated by significant heterogeneity of change over time in the respective unconditional latent growth models. The reason for the reduction in self-efficacy over time is unclear. It is plausible that the drop in self-efficacy over time was reflective of participants changing perceptions of their ability to stick with healthful eating and physical activity over a long period of time. This is not the first trial to report a reduction in self-efficacy for weight-loss-related behavior (Linde et al., 2006). These observations align with the theoretical postulate that as participants become more experienced with the difficulty of losing weight as well as maintaining healthful eating and physical activity, their perceptions become more realistic (Bandura, 1977, 1997). This preliminary evidence for score sensitivity to change, and the aforementioned evidence for factorial validity and measurement equivalence/invariance, provide strong initial support for the application of this survey in studies focused on weight-loss or related behaviors in overweight or obese samples.
Tests of predictive validity further supported the interpretation of scores from the new survey as reflective of self-efficacy for weight-loss-related behaviors. Analyses confirmed the expected relationships between change in self-efficacy and change in target outcomes, such that increases in self-efficacy were related to more desirable outcomes (i.e. increases in physical activity and decreases in fat intake and weight). Unstandardized results of the conditional latent growth models indicated that for every 1% increase in WLSE, HESE, and PASE, participants lost about three quarters of a pound, consumed less fat (reflected in a reduction of .14 in fat intake score), and participated in about four and a half more minutes of moderate-to-vigorous physical activity per week, respectively. Not surprisingly these changes were nearly identical when considering WLRBSE. Results from the standardized solutions indicate that a one standard deviation change in WLSE, HESE, or WLRBSE was associated with a change of over a half of a standard deviation in weight and fat intake. Effects were larger for moderate-to-vigorous physical activity, as a one standard deviation change in PASE, or WLRBSE was associated with a change of about a full standard deviation in physical activity level.
Relationships between change in self-efficacy, which declined over time in this sample, and change in target outcomes were heterogeneous, indicating that those participants who experienced increases or less decline in self-efficacy also had superior weight loss and behavioral outcomes. Specifically, greater weight-loss, reduction in fat intake, and increases in moderate-to-vigorous physical activity were observed for those who had more gradual decline, and less overall decline, in WLSE, HESE, and PASE, respectively. A practical recommendation from this psychometric investigation, then, is that weight loss interventions may benefit from strategies to reduce the likelihood of declines in WLSE, HESE, and PASE similar to those used in acceptance based cognitive behavioral therapy (Hayes, 2004). Overall, results of the conditional latent growth models provide additional support for the validity of score interpretation from this survey as reflecting underlying self-efficacy for weight-loss-related behaviors, as relationships between change in survey scores and outcome measures are in the expected direction based on theory (Bandura, 1977, 1997) and empirical evidence (Byrne et al., 2012; Hagler, 2007; Hays et al., 2014; Henry et al., 2006; Linde et al., 2006; McAuley, Elavsky, Motl, & Konopack, 2005; Palmeira et al., 2007; Steptoe et al., 2000; Warziski et al., 2008).
Additional research will be needed to test the construct validity of the measurements obtained with this survey. Tests of convergent and discriminant validity, and evidence for predictive validity using more comprehensive, as well as objective, measures of physical activity and dietary habits are recommended. Also, continued use of this survey in trials of varying size and diversity are encouraged as assessment of psychometric performance of this survey under varying conditions is necessary to determine its applicability to weight-loss programs across the translational spectrum. It is recommended that scores be summed for items measuring HESE, PASE, and WLSE for further use. A composite score is not recommended to measure WLRBSE, as the single-factor model demonstrated poor model fit. More evidence will need to be generated before a proper weighting coefficient can be added so that we may appropriately assess WLRBSE, if possible.
Conclusion
Overall, evidence provided here supports the validity of score interpretations from this survey targeting self-efficacy for weight-loss-related behaviors in overweight or obese individuals participating in a large-scale worksite weight-loss trial. The expected factor structure was supported, and the strictest form of measurement equivalence/invariance was observed according to gender, age, race, education level, and BMI status. The scale scores also demonstrated stability and sensitivity to change over time. Conditional latent growth models revealed the expected relationships between change in self-efficacy and change in targeted outcomes. The performance of these scales in a large, representative sample supports the use of this survey in similar trials. Additional support for this survey could be provided by tests of convergent and discriminant validity, as well as reports on applied hypothesis testing based on self-efficacy theory in randomized controlled trials. Future studies might also test the quality of the survey using physical activity and diet constructs not present in the current investigation. Continued use of this measure in trials and longitudinal observations examining self-efficacy and weight-loss-related behaviors is encouraged to further test validity, and explore the relationships between self-efficacy, eating and physical activity behaviors, and weight loss.
Footnotes
Pragmatic measures and metrics are defined as those that are reliable, valid, sensitive to change, feasible, important to practitioners, actionable, user friendly, broadly applicable, low cost, harmless, and relevant to public health while enhancing patient engagement (Glasgow, 2013). The current study aims to provide evidence of pragmatism for the presented measure.
Though this scale was modeled after the scale presented by Schwarzer and Renner (2000) in a desire to maintain alignment with phasic theories of behavior change, items on the scale presented here were administered together at all measurement time points, whereas Schwarzer and Renner administered the action self-efficacy items at baseline, and the coping self-efficacy items 6 months later. This lagged administration, coupled with the limitation of the action self-efficacy scale to 2 items prohibited a test of factor structure according to phasic alignment of the items in the previous version of the scale, justifying a test of factor structure alignment with this theoretically derived item classification.
References
- Annesi JJ. Relations of changes in exercise self-efficacy, physical self-concept, and body satisfaction with weight changes in obese white and African American women initiating a physical activity program. Ethnicity and Disease. 2007;17(1):19. [PubMed] [Google Scholar]
- Bandura A. Self-efficacy: toward a unifying theory of behavioral change. Psychological Review. 1977;84(2):191. doi: 10.1037//0033-295x.84.2.191. [DOI] [PubMed] [Google Scholar]
- Bandura A. Social foundations of thought and action. Vol. 1986 Englewood Cliffs, NJ: 1986. [Google Scholar]
- Bandura A. Self-Efficacy: The Exercise of Control. New York: W.H. Freeman and Company; 1997. [Google Scholar]
- Berkel LA, Carlos Poston WS, Reeves RS, Foreyt JP. Behavioral Interventions for Obesity. Journal of the American Dietetic Association. 2005;105(5, Supplement):35–43. doi: 10.1016/j.jada.2005.02.031. doi: http://dx.doi.org/10.1016/j.jada.2005.02.031. [DOI] [PubMed] [Google Scholar]
- Block G, Gillespie C, Rosenbaum E, Jenson C. A rapid food screener to assess fat and fruit and vegetable intake. Am J Prev Med. 2000;18(4):284–288. doi: 10.1016/s0749-3797(00)00119-7. [DOI] [PubMed] [Google Scholar]
- Bollen KA. A new incremental fit index for general structural equation models. Sociological Methods & Research. 1989;17(3):303–316. [Google Scholar]
- Bollen KA, Harden JJ, Ray S, Zavisca J. BIC and alternative Bayesian information criteria in the selection of structural equation models. Structural Equation Modeling: A Multidisciplinary Journal. 2014;21(1):1–19. doi: 10.1080/10705511.2014.856691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bong M. Generality of academic self-efficacy judgments: Evidence of hierarchical relations. Journal of Educational Psychology. 1997;89(4):696–709. doi: 10.1037/0022-0663.89.4.696. [DOI] [Google Scholar]
- Brownson R, Jones D, Pratt M, Blanton C, Heath G. Measuring physical activity with the behavioral risk factor surveillance system. Medicine & Science in Sports & Exercise. 2000;32(11):1913–1918. doi: 10.1097/00005768-200011000-00015. [DOI] [PubMed] [Google Scholar]
- Byrne S, Barry D, Petry NM. Predictors of weight loss success. Exercise vs. dietary self-efficacy and treatment attendance. Appetite. 2012;58(2):695–698. doi: 10.1016/j.appet.2012.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clark MM, Abrams DB, Niaura RS, Eaton CA, Rossi JS. Self-efficacy in weight management. Journal of Consulting and Clinical Psychology. 1991;59(5):739–744. doi: 10.1037/0022-006X.59.5.739. [DOI] [PubMed] [Google Scholar]
- Clark MM, Cargill BR, Medeiros ML, Pera V. Changes in Self-Efficacy Following Obesity Treatment. Obesity Research. 1996;4(2):179–181. doi: 10.1002/j.1550-8528.1996.tb00531.x. [DOI] [PubMed] [Google Scholar]
- Curioni CC, Lourenco PM. Long-term weight loss after diet and exercise: a systematic review. Int J Obes Relat Metab Disord. 2005;29(10):1168–1174. doi: 10.1038/sj.ijo.0803015. Retrieved from http://dx.doi.org/10.1038/sj.ijo.0803015. [DOI] [PubMed] [Google Scholar]
- Dennis KE, Goldberg AP. Weight control self-efficacy types and transitions affect weight-loss outcomes in obese women. Addictive Behaviors. 1996;21(1):103–116. doi: 10.1016/0306-4603(95)00042-9. [DOI] [PubMed] [Google Scholar]
- Elfhag K, Rössner S. Who succeeds in maintaining weight loss? A conceptual review of factors associated with weight loss maintenance and weight regain. Obesity Reviews. 2005;6(1):67–85. doi: 10.1111/j.1467-789X.2005.00170.x. [DOI] [PubMed] [Google Scholar]
- Flood A, Velie E, Chaterjee N, Subar A, Thompson F, Lacey J. Fruit and vegetable intakes and the risk of colorectal cancer inthe Breast Cancer Detection Demonstration Project follow-up cohort. Americanl Journal of Clinical Nutrition. 2002;75:936–943. doi: 10.1093/ajcn/75.5.936. [DOI] [PubMed] [Google Scholar]
- Fontaine KR, Cheskin LJ. Self-efficacy, attendance, and weight loss in obesity treatment. Addictive Behaviors. 1997;22(4):567–570. doi: 10.1016/s0306-4603(96)00068-8. doi: http://dx.doi.org/10.1016/S0306-4603(96)00068-8. [DOI] [PubMed] [Google Scholar]
- Forster JL, Jeffrey RW. Gender differences related to weight history, eating patterns, efficacy expectations, self-esteem, and weight loss among participants in a weight reduction program. Addictive Behaviors. 1986;11(2):141–147. doi: 10.1016/0306-4603(86)90039-0. doi: http://dx.doi.org/10.1016/0306-4603(86)90039-0. [DOI] [PubMed] [Google Scholar]
- Franz MJ, VanWormer JJ, Crain AL, Boucher JL, Histon T, Caplan W, et al. Pronk NP. Weight-loss outcomes: a systematic review and meta-analysis of weight-loss clinical trials with a minimum 1-year follow-up. Journal of the American Dietetic Association. 2007;107(10):1755–1767. doi: 10.1016/j.jada.2007.07.017. [DOI] [PubMed] [Google Scholar]
- Garber C, Blissmer B, Deschenes M, et al. American College of Sports Medicine position stand. Quantity and quality of exercise for developing and maintaining cardiorespiratory, musculoskeletal, and neuromotor fitness in apparently healthy adults: guidance for prescribing exercise. Medicine & Science in Sports & Exercise. 2011;43(7):1334–1359. doi: 10.1249/MSS.0b013e318213fefb. [DOI] [PubMed] [Google Scholar]
- Glasgow RE. What does it mean to be pragmatic? Pragmatic methods, measures, and models to facilitate research translation. Health Education & Behavior. 2013;40(3):257–265. doi: 10.1177/1090198113486805. [DOI] [PubMed] [Google Scholar]
- Glynn SM, Ruderman AJ. The development and validation of an eating self-efficacy scale. Cognitive Therapy and Research. 1986;10(4):403–420. [Google Scholar]
- Haddock CK, Poston WSC, Dill PL, Foreyt JP, Ericsson M. Pharmacotherapy for obesity: a quantitative analysis of four decades of published randomized clinical trials. International Journal of Obesity and Related Disorders. 2002;26(2):262–273. doi: 10.1038/sj.ijo.0801889. doi: http://dx.doi.org/10.1038/sj.ijo.0801889. [DOI] [PubMed] [Google Scholar]
- Hagler AS. Psychosocial Correlates of Dietary Intake Among Overweight and Obese Men. American Journal of Health Behavior. 2007;31(1):3–12. doi: 10.5993/AJHB.31.1.1. [DOI] [PubMed] [Google Scholar]
- Hayes SC. Acceptance and commitment therapy, relational frame theory, and the third wave of behavioral and cognitive therapies. Behavior Therapy. 2004;35(4):639–665. doi: 10.1016/j.beth.2016.11.006. doi: http://dx.doi.org/10.1016/S0005-7894(04)80013-3. [DOI] [PubMed] [Google Scholar]
- Hays LM, Finch EA, Saha C, Marrero DG, Ackermann RT. Effect of Self-Efficacy on Weight Loss: A Psychosocial Analysis of a Community-Based Adaptation of the Diabetes Prevention Program Lifestyle Intervention. Diabetes Spectrum. 2014;27(4):270–275. doi: 10.2337/diaspect.27.4.270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Henry H, Reimer K, Smith C, Reicks M. Associations of Decisional Balance, Processes of Change, and Self-Efficacy with Stages of Change for Increased Fruit and Vegetable Intake among Low-Income, African-American Mothers. Journal of the American Dietetic Association. 2006;106(6):841–849. doi: 10.1016/j.jada.2006.03.012. doi: http://dx.doi.org/10.1016/j.jada.2006.03.012. [DOI] [PubMed] [Google Scholar]
- Hu Lt, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling: A Multidisciplinary Journal. 1999;6(1):1–55. [Google Scholar]
- Jakicic JM, Clark K, Coleman E, Donnelly JE, Foreyt J, Melanson E, et al. Volpe SL. American College of Sports Medicine position stand. Appropriate intervention strategies for weight loss and prevention of weight regain for adults. Medicine and Science in Sports and Exercise. 2001;33(12):2145–2156. doi: 10.1097/00005768-200112000-00026. [DOI] [PubMed] [Google Scholar]
- Kline RB. Principles and practice of structural equation modeling. third. New York: The Guilford Press; 2011. [Google Scholar]
- Linde J, Jeffery R, Levy R, Sherwood N, Utter J, Pronk N, Boyle R. Binge eating disorder, weight control self-efficacy, and depression in overweight men and women. International Journal of Obesity. 2004;28(3):418–425. doi: 10.1038/sj.ijo.0802570. [DOI] [PubMed] [Google Scholar]
- Linde J, Rothman A, Baldwin A, Jeffery R. The impact of self-efficacy on behavior change and weight change among overweight participants in a weight loss trial. Health Psychology. 2006;25(3):282. doi: 10.1037/0278-6133.25.3.282. [DOI] [PubMed] [Google Scholar]
- Maes S, Karoly P. Self-Regulation Assessment and Intervention in Physical Health and Illness: A Review. Applied Psychology. 2005;54(2):267–299. [Google Scholar]
- McAuley E, Blissmer B. Self-efficacy determinants and consequences of physical activity. Exercise and Sport Sciences Reviews. 2000;28(2):85–88. [PubMed] [Google Scholar]
- McAuley E, Elavsky S, Motl RW, Konopack JF. Physical activity, self-efficacy, and self-esteem: longitudinal relationships in older adults. Journal of Gerontology. 2005;60B(5):P268–P275. doi: 10.1093/geronb/60.5.p268. [DOI] [PubMed] [Google Scholar]
- Michels K, Giovannucci E, Joshipura K, Rosner B, Stampher M, Fuchs C. Prospective study of fruit and vegetable consumption and incidence of colon and rectal cancers. Journal of the National Cancer Institute. 2000;91:1740–1752. doi: 10.1093/jnci/92.21.1740. [DOI] [PubMed] [Google Scholar]
- Michie S, van Stralen M, West R. The behaviour change wheel: A new method for characterising and designing behaviour change interventions. Implementation Science. 2011;6(1):1–12. doi: 10.1186/1748-5908-6-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthén L, Muthén B. Mplus. Statistical analysis with latent variables Version, 7 2012 [Google Scholar]
- Palmeira AL, Teixeira PJ, Branco TL, Martins SS, Minderico CS, Barata JT, et al. Sardinha LB. Predicting short-term weight loss using four leading health behavior change theories. International Journal of Behavioral Nutrition and Physical Activity. 2007;4(1):14. doi: 10.1186/1479-5868-4-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Plotnikoff RC, McCargar LJ, Wilson PM, Loucaides CA. Efficacy of an E-mail intervention for the promotion of physical activity and nutrition behavior in the workplace context. American Journal of Health Promotion. 2005;19(6):422–439. doi: 10.4278/0890-1171-19.6.422. [DOI] [PubMed] [Google Scholar]
- Prochaska JO, Norcross JC, Fowler JL, Follick MJ, Abrams DB. Attendance and outcome in a work site weight control program: Processes and stages of change as process and predictor variables. Addictive Behaviors. 1992;17(1):35–45. doi: 10.1016/0306-4603(92)90051-v. doi: http://dx.doi.org/10.1016/0306-4603(92)90051-V. [DOI] [PubMed] [Google Scholar]
- Prochaska JO, Velicer WF. The transtheoretical model of health behavior change. American Journal of Health Promotion. 1997;12(1):38–48. doi: 10.4278/0890-1171-12.1.38. [DOI] [PubMed] [Google Scholar]
- Richman RM, Loughnan GT, Droulers AM, Steinbeck KS, Caterson ID. Self-efficacy in relation to eating behaviour among obese and non-obese women. International Journal of Obesity and Related Disorders. 2001;25(6):907–913. doi: 10.1038/sj.ijo.0801606. doi: http://dx.doi.org/10.1038/sj.ijo.0801606. [DOI] [PubMed] [Google Scholar]
- Schwarzer R. Self-Efficacy: Thought Control of Action. Washington, DC: Hemisphere; 1992. Self-efficacy in the adoption and maintenance of health behaviours: Theoretical approaches and a new model; pp. 217–243. [Google Scholar]
- Schwarzer R, Renner B. Social-cognitive predictors of health behavior: action self-efficacy and coping self-efficacy. Health Psychology. 2000;19(5):487. [PubMed] [Google Scholar]
- Shin H, Shin J, Liu PY, Dutton GR, Abood DA, Ilich JZ. Self-efficacy improves weight loss in overweight/obese postmenopausal women during a 6-month weight loss intervention. Nutrition Research. 2011;31(11):822–828. doi: 10.1016/j.nutres.2011.09.022. doi: http://dx.doi.org/10.1016/j.nutres.2011.09.022. [DOI] [PubMed] [Google Scholar]
- Skaalvik EM, Skaalvik S. Teacher self-efficacy and teacher burnout: A study of relations. Teaching and Teacher Education. 2010;26(4):1059–1069. doi: http://dx.doi.org/10.1016/j.tate.2009.11.001. [Google Scholar]
- Steptoe A, Doherty S, Kerry S, Rink E, Hilton S. Sociodemographic and psychological predictors of changes in dietary fat consumption in adults with high blood cholesterol following counseling in primary care. Health Psychology. 2000;19(5):411–419. doi: 10.1037/0278-6133.19.5.411. [DOI] [PubMed] [Google Scholar]
- Stotland S, Zuroff DC. Relations between multiple measures of dieting self-efficacy and weight change in a behavioral weight control program. Behavior Therapy. 1991;22(1):47–59. doi: http://dx.doi.org/10.1016/S0005-7894(05)80243-6. [Google Scholar]
- Strecher VJ, DeVellis BM, Becker MH, Rosenstock IM. The role of self-efficacy in achieving health behavior change. Health Education & Behavior. 1986;13(1):73–92. doi: 10.1177/109019818601300108. [DOI] [PubMed] [Google Scholar]
- Tang J, Abraham C, Greaves C, Yates T. Self-directed interventions to promote weight loss: a systematic review of reviews. Journal of medical Internet research. 2014;16(2) doi: 10.2196/jmir.2857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Teixeira PJ, Going SB, Houtkooper LB, Cussler EC, Martin CJ, Metcalfe LL, et al. Lohman TG. Weight loss readiness in middle-aged women: psychosocial predictors of success for behavioral weight reduction. Journal of Behavioral Medicine. 2002;25(6):499–523. doi: 10.1023/a:1020687832448. [DOI] [PubMed] [Google Scholar]
- Teixeira PJ, Palmeira AL, Branco TL, Martins SS, Minderico CS, Barata JT, et al. Sardinha LB. Who will lose weight? A reexamination of predictors of weight loss in women. International Journal of Behavioral Nutrition and Physical Activity. 2004;1(1):12. doi: 10.1186/1479-5868-1-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thompson B, Denmark-Wahnefried W, WTaylor G, McClelland J, Stables G, Havas S. Basleine fruit and vegetable intake among adults in seven 5 A Day study centers located in diverse geographic areas. Journal of the American Dietetic Association. 1999;99:1241–1248. doi: 10.1016/S0002-8223(99)00306-5. [DOI] [PubMed] [Google Scholar]
- Trost SG, Kerr LM, Ward DS, Pate RR. Physical activity and determinants of physical activity in obese and non-obese children. International Journal of Obesity and Related Disorders. 2001;25(6):822–829. doi: 10.1038/sj.ijo.0801621. doi: http://dx.doi.org/10.1038/sj.ijo.0801621. [DOI] [PubMed] [Google Scholar]
- Van Duyn MAS, Kristal AR, Dodd K, Campbell MK, Subar AF, Stables G, et al. Glanz K. Association of awareness, intrapersonal and interpersonal factors, and stage of dietary change with fruit and vegetable consumption: a national survey. American Journal of Health Promotion. 2001;16(2):69–78. doi: 10.4278/0890-1171-16.2.69. [DOI] [PubMed] [Google Scholar]
- Vandenberg RJ, Lance CE. A Review and Synthesis of the Measurement Invariance Literature: Suggestions, Practices, and Recommendations for Organizational Research. Organizational Research Methods. 2000;3(1):4–69. Retrieved from http://ejournals.ebsco.com/direct.asp?ArticleID=MPHED21WCGM0LC6C87P1. [Google Scholar]
- Wadden TA, Brownell KD, Foster GD. Obesity: responding to the global epidemic. Journal of Consulting and Clinical Psychology. 2002;70(3):510. doi: 10.1037//0022-006x.70.3.510. [DOI] [PubMed] [Google Scholar]
- Warziski M, Sereika S, Styn M, Music E, Burke L. Changes in self-efficacy and dietary adherence: the impact on weight loss in the PREFER study. Journal of Behavioral Medicine. 2008;31(1):81–92. doi: 10.1007/s10865-007-9135-2. [DOI] [PubMed] [Google Scholar]
- White MA, Martin PD, Newton RL, Walden HM, York-Crowe EE, Gordon ST, et al. Williamson DA. Mediators of Weight Loss in a Family-Based Intervention Presented over the Internet. Obesity Research. 2004;12(7):1050–1059. doi: 10.1038/oby.2004.132. [DOI] [PubMed] [Google Scholar]
- Wing RR, Phelan S. Long-term weight loss maintenance. The American Journal of Clinical Nutrition. 2005;82(1):222S–225S. doi: 10.1093/ajcn/82.1.222S. [DOI] [PubMed] [Google Scholar]
- World Health Organization. Global status report on noncommunicable diseases 2010. World Health Organization; 2011. [Google Scholar]


